Simponi
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use SIMPONI safely and effectively. See full prescribing information for SIMPONI. SIMPONI (golimumab) injection, for subcutaneous use Initial U.S. Approval: 2009BOXED WARNINGWARNING: SERIOUS INFECTIONS AND MALIGNANCY See full prescribing information for complete boxed warning. Serious infections leading to hospitalization or death including tuberculosis (TB), bacterial sepsis, invasive fungal (such as histoplasmosis), and other opportunistic infections have occurred in patients receiving SIMPONI (5.1) Discontinue SIMPONI if a patient develops a serious infection or sepsis (5.1) Perform test for latent TB; if positive, start treatment for TB prior to starting SIMPONI (5.1) Monitor all patients for active TB during treatment, even if initial latent TB test is negative (5.1) Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers, of which SIMPONI is a member (5.2) RECENT MAJOR CHANGES Indications and Usage, Ulcerative Colitis (1.4) 5/2013 Dosage and Administration (2.2, 2.4) 5/2013 Warnings and Precautions (5.1, 5.2, 5.9) 11/2013 INDICATIONS AND USAGESIMPONI is a tumor necrosis factor (TNF) blocker indicated for the treatment of adult patients with: Moderately to severely active rheumatoid arthritis (RA) in combination with methotrexate (1.1) Active psoriatic arthritis (PsA) alone, or in combination with methotrexate (1.2) Active ankylosing spondylitis (AS) (1.3) Moderate to severe Ulcerative colitis (UC) with an inadequate response or intolerant to prior treatment or requiring continuous steroid therapy (1.4) inducing and maintaining clinical response improving endoscopic appearance of the mucosa during induction inducing clinical remission achieving and sustaining clinical remission in induction responders DOSAGE AND ADMINISTRATION RA, PsA, and AS: 50 mg administered by subcutaneous injection once a month (2.1) UC: 200 mg initially administered by subcutaneous injection at Week 0, followed by 100 mg at Week 2 and then 100 mg every 4 weeks (2.2) DOSAGE FORMS AND STRENGTHSInjection (3): 50 mg/0.5 mL in a single dose prefilled SmartJect® autoinjector 50 mg/0.5 mL in a single dose prefilled syringe 100 mg/1 mL in a single dose prefilled SmartJect® autoinjector 100 mg/1 mL in a single dose prefilled syringe CONTRAINDICATIONSNone (4)WARNINGS AND PRECAUTIONS Serious Infections: Do not start SIMPONI during an active infection. If an infection develops, monitor carefully, and stop SIMPONI if infection becomes serious (5.1) Invasive Fungal Infections: For patients who develop a systemic illness on SIMPONI, consider empiric antifungal therapy for those who reside in or travel to regions where mycoses are endemic (5.1) Hepatitis B Reactivation: Monitor HBV carriers during and several months after therapy. If reactivation occurs, stop SIMPONI and begin anti-viral therapy (5.1) Malignancies: Incidence of lymphoma was greater than in the general U.S. population. Cases of other malignancies have been observed among patients receiving TNF-blockers (5.2) Heart Failure: Worsening, or new onset, may occur. Stop SIMPONI if new or worsening symptoms occur (5.3) Demyelinating Disease: Exacerbation or new onset, may occur (5.4) Hypersensitivity Reactions: Serious systemic hypersensitivity reactions including anaphylaxis may occur (5.10) Side EffectsMost common adverse reactions (incidence > 5%) are upper respiratory tract infection, nasopharyngitis, injection site reactions (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Janssen Biotech, Inc. at 1-800-JANSSEN (1-800-526-7736) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Abatacept: Increased risk of serious infection (5.1, 5.5, 7.2) Anakinra: Increased risk of serious infection (5.1, 5.6, 7.2). Live vaccines/therapeutic infectious agents: Avoid use with SIMPONI (5.9, 7.3).
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 SIMPONI INDICATIONS AND USAGE
- 2 SIMPONI DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 SIMPONI CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Serious Infections
- 5.2 Malignancies
- 5.3 Congestive Heart Failure
- 5.4 Demyelinating Disorders
- 5.5 Use with Abatacept
- 5.6 Use with Anakinra
- 5.7 Switching Between Biological Disease Modifying Antirheumatic Drugs
- 5.8 Hematologic Cytopenias
- 5.9 Vaccinations/Therapeutic Infectious Agents
- 5.10 Hypersensitivity Reactions
- 6 SIMPONI ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 SIMPONI DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
SERIOUS INFECTIONS
Patients treated with SIMPONI® are at increased risk for developing serious infections that may lead to hospitalization or death [see Warnings and Precautions (5.1)]. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.
Discontinue SIMPONI if a patient develops a serious infection.
Reported infections with TNF-blockers, of which SIMPONI is a member, include:
- Active tuberculosis, including reactivation of latent tuberculosis. Patients with tuberculosis have frequently presented with disseminated or extrapulmonary disease. Test patients for latent tuberculosis before SIMPONI use and during therapy. Initiate treatment for latent TB prior to SIMPONI use.
- Invasive fungal infections including histoplasmosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis and pneumocystosis. Patients with histoplasmosis or other invasive fungal infections may present with disseminated, rather than localized, disease. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. Consider empiric anti-fungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness.
- Bacterial, viral and other infections due to opportunistic pathogens, including Legionella and Listeria.
Consider the risks and benefits of treatment with SIMPONI prior to initiating therapy in patients with chronic or recurrent infection.
Monitor patients closely for the development of signs and symptoms of infection during and after treatment with SIMPONI, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis infection prior to initiating therapy [see Warnings and Precautions (5.1)].
MALIGNANCY
Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers, of which SIMPONI is a member [see Warnings and Precautions (5.2)] .
1 INDICATIONS AND USAGE
1.1 Rheumatoid Arthritis
SIMPONI, in combination with methotrexate, is indicated for the treatment of adult patients with moderately to severely active rheumatoid arthritis.
1.2 Psoriatic Arthritis
SIMPONI, alone or in combination with methotrexate, is indicated for the treatment of adult patients with active psoriatic arthritis.
1.3 Ankylosing Spondylitis
SIMPONI is indicated for the treatment of adult patients with active ankylosing spondylitis.
1.4 Ulcerative Colitis
SIMPONI is indicated in adult patients with moderately to severely active ulcerative colitis who have demonstrated corticosteroid dependence or who have had an inadequate response to or failed to tolerate oral aminosalicylates, oral corticosteroids, azathioprine, or 6-mercaptopurine for:
- inducing and maintaining clinical response
- improving endoscopic appearance of the mucosa during induction
- inducing clinical remission
- achieving and sustaining clinical remission in induction responders [see Clinical Studies (14.4)].
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Rheumatoid Arthritis, Psoriatic Arthritis, Ankylosing Spondylitis
The SIMPONI dose regimen is 50 mg administered by subcutaneous injection once a month.
For patients with rheumatoid arthritis (RA), SIMPONI should be given in combination with methotrexate and for patients with psoriatic arthritis (PsA) or ankylosing spondylitis (AS), SIMPONI may be given with or without methotrexate or other non-biologic Disease Modifying Antirheumatic Drugs (DMARDs). For patients with RA, PsA, or AS, corticosteroids, non-biologic DMARDs, and/or NSAIDs may be continued during treatment with SIMPONI.
2.2 Dosage in Moderately to Severely Active Ulcerative Colitis
The recommended SIMPONI induction dosage regimen is a 200 mg subcutaneous injection at Week 0, followed by 100 mg at Week 2 and then maintenance therapy with 100 mg every 4 weeks.
2.3 Monitoring to Assess Safety
Prior to initiating SIMPONI and periodically during therapy, evaluate patients for active tuberculosis and tested for latent infection [see Warnings and Precautions (5.1)]. Prior to initiating SIMPONI, patients should be tested for hepatitis B viral infection [see Warnings and Precautions (5.1)].
2.4 Important Administration Instructions
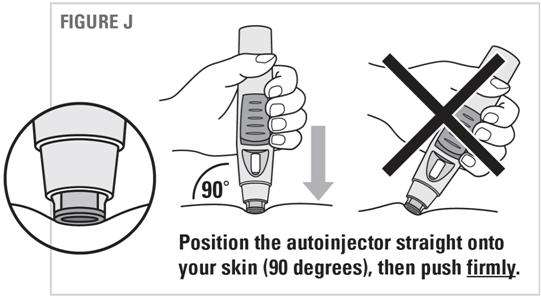
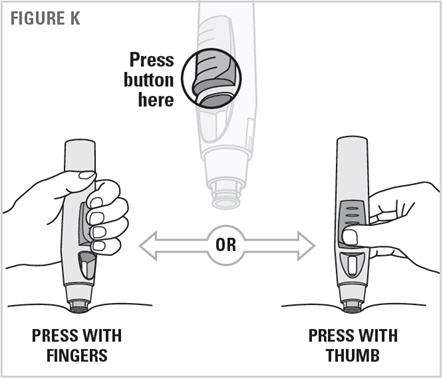
SIMPONI is intended for use under the guidance and supervision of a healthcare provider. After proper training in subcutaneous injection technique, a patient may self inject with SIMPONI if a physician determines that it is appropriate. Instruct patients to follow the directions provided below [see Instructions for Use]:
- To ensure proper use, allow the prefilled syringe or autoinjector to sit at room temperature outside the carton for 30 minutes prior to subcutaneous injection. Do not warm SIMPONI in any other way.
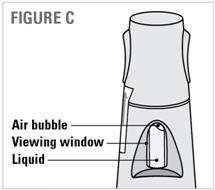
- Prior to administration, visually inspect the solution for particles and discoloration through the viewing window. SIMPONI is clear to slightly opalescent and colorless to light yellow. Do not use SIMPONI, if the solution is discolored, or cloudy, or if foreign particles are present.
- Do not use any leftover product remaining in the prefilled syringe or prefilled autoinjector.
- Instruct patients sensitive to latex, to not handle the needle cover on the prefilled syringe as well as the needle cover of the prefilled syringe within the autoinjector cap because it contains dry natural rubber (a derivative of latex).
- At the time of dosing, if multiple injections are required, administer the injections at different sites on the body.
- Rotate injection sites and never give injections into areas where the skin is tender, bruised, red, or hard.
3 DOSAGE FORMS AND STRENGTHS
The SIMPONI dosage form is for subcutaneous injection. SIMPONI is available in 50 mg and 100 mg strengths.
SmartJect® Autoinjector
- Each 50 mg single dose SmartJect autoinjector contains a prefilled glass syringe (27 gauge ½ inch) providing 50 mg of SIMPONI per 0.5 mL of solution.
- Each 100 mg single dose SmartJect autoinjector contains a prefilled glass syringe (27 gauge ½ inch) providing 100 mg of SIMPONI per 1 mL of solution.
Prefilled Syringe
- Each 50 mg single dose prefilled glass syringe (27 gauge ½ inch) contains 50 mg of SIMPONI per 0.5 mL of solution.
- Each 100 mg single dose prefilled glass syringe (27 gauge ½ inch) contains 100 mg of SIMPONI per 1 mL of solution.
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Serious Infections
Patients treated with SIMPONI are at increased risk for developing serious infections involving various organ systems and sites that may lead to hospitalization or death.
Opportunistic infections due to bacterial, mycobacterial, invasive fungal, viral, or parasitic organisms including aspergillosis, blastomycosis, candidiasis, coccidioidomycosis, histoplasmosis, legionellosis, listeriosis, pneumocystosis, and tuberculosis have been reported with TNF-blockers. Patients have frequently presented with disseminated rather than localized disease. The concomitant use of a TNF-blocker and abatacept or anakinra was associated with a higher risk of serious infections; therefore, the concomitant use of SIMPONI and these biologic products is not recommended [see Warnings and Precautions (5.5, 5.6) and Drug Interactions (7.2)].
Treatment with SIMPONI should not be initiated in patients with an active infection, including clinically important localized infections. Patients greater than 65 years of age, patients with co-morbid conditions and/or patients taking concomitant immunosuppressants such as corticosteroids or methotrexate may be at greater risk of infection. Consider the risks and benefits of treatment prior to initiating SIMPONI in patients:
- with chronic or recurrent infection;
- who have been exposed to tuberculosis;
- with a history of an opportunistic infection;
- who have resided or traveled in areas of endemic tuberculosis or endemic mycoses, such as histoplasmosis, coccidioidomycosis, or blastomycosis; or
- with underlying conditions that may predispose them to infection.
Monitoring
Closely monitor patients for the development of signs and symptoms of infection during and after treatment with SIMPONI. Discontinue SIMPONI if a patient develops a serious infection, an opportunistic infection, or sepsis. For a patient who develops a new infection during treatment with SIMPONI, perform a prompt and complete diagnostic workup appropriate for an immunocompromised patient, initiate appropriate antimicrobial therapy and closely monitor them.
Serious Infection in Clinical Trials
In controlled Phase 3 trials through Week 16 in patients with RA, PsA, and AS, serious infections were observed in 1.4% of SIMPONI-treated patients and 1.3% of control-treated patients. In the controlled Phase 3 trials through Week 16 in patients with RA, PsA, and AS, the incidence of serious infections per 100 patient-years of follow-up was 5.7 (95% CI: 3.8, 8.2) for the SIMPONI group and 4.2 (95% CI: 1.8, 8.2) for the placebo group. In the controlled Phase 2/3 trial through Week 6 of SIMPONI induction in UC, the incidence of serious infections in SIMPONI 200/100 mg-treated patients was similar to the incidence of serious infections in placebo-treated patients. Through Week 60, the incidence of serious infections was similar in patients who received SIMPONI induction and 100 mg during maintenance compared with patients who received SIMPONI induction and placebo during the maintenance portion of the UC trial. Serious infections observed in SIMPONI-treated patients included sepsis, pneumonia, cellulitis, abscess, tuberculosis, invasive fungal infections, and hepatitis B infection.
Tuberculosis
Cases of reactivation of tuberculosis or new tuberculosis infections have been observed in patients receiving TNF-blockers, including patients who have previously received treatment for latent or active tuberculosis. Evaluate patients for tuberculosis risk factors and test for latent infection prior to initiating SIMPONI and periodically during therapy.
Treatment of latent tuberculosis infection prior to therapy with TNF-blockers has been shown to reduce the risk of tuberculosis reactivation during therapy. Prior to initiating SIMPONI, assess if treatment for latent tuberculosis is needed; an induration of 5 mm or greater is a positive tuberculin skin test, even for patients previously vaccinated with Bacille Calmette-Guerin (BCG).
Consider anti-tuberculosis therapy prior to initiation of SIMPONI in patients with a past history of latent or active tuberculosis in whom an adequate course of treatment cannot be confirmed, and for patients with a negative test for latent tuberculosis but having risk factors for tuberculosis infection. Consultation with a physician with expertise in the treatment of tuberculosis is recommended to aid in the decision whether initiating anti-tuberculosis therapy is appropriate for an individual patient.
Cases of active tuberculosis have occurred in patients treated with SIMPONI during and after treatment for latent tuberculosis. Monitor patients for the development of signs and symptoms of tuberculosis including patients who tested negative for latent tuberculosis infection prior to initiating therapy, patients who are on treatment for latent tuberculosis, or patients who were previously treated for tuberculosis infection.
Consider tuberculosis in the differential diagnosis in patients who develop a new infection during SIMPONI treatment, especially in patients who have previously or recently traveled to countries with a high prevalence of tuberculosis, or who have had close contact with a person with active tuberculosis.
In the controlled and uncontrolled portions of the Phase 2 RA and Phase 3 RA, PsA, and AS trials, the incidence of active TB was 0.23 and 0 per 100 patient-years in 2347 SIMPONI-treated patients and 674 placebo-treated patients, respectively. Cases of TB included pulmonary and extra pulmonary TB. The overwhelming majority of the TB cases occurred in countries with a high incidence rate of TB. In the controlled Phase 2/3 trial of SIMPONI induction through Week 6 in UC, no cases of TB were observed in SIMPONI 200/100 mg-treated patients or in placebo-treated patients. Through Week 60, the incidence per 100 patient-years of TB in patients who received SIMPONI induction and 100 mg during the maintenance portion of the UC trial was 0.52 (95% CI: 0.11, 1.53). One case of TB was observed in the placebo maintenance group in a patient who received SIMPONI intravenous (IV) induction.
Invasive Fungal Infections
If patients develop a serious systemic illness and they reside or travel in regions where mycoses are endemic, consider invasive fungal infection in the differential diagnosis. Consider appropriate empiric antifungal therapy and take into account both the risk for severe fungal infection and the risks of antifungal therapy while a diagnostic workup is being performed. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. To aid in the management of such patients, consider consultation with a physician with expertise in the diagnosis and treatment of invasive fungal infections.
Hepatitis B Virus Reactivation
The use of TNF-blockers including SIMPONI has been associated with reactivation of hepatitis B virus (HBV) in patients who are chronic hepatitis B carriers (i.e., surface antigen positive). In some instances, HBV reactivation occurring in conjunction with TNF-blocker therapy has been fatal. The majority of these reports have occurred in patients who received concomitant immunosuppressants.
All patients should be tested for HBV infection before initiating TNF-blocker therapy. For patients who test positive for hepatitis B surface antigen, consultation with a physician with expertise in the treatment of hepatitis B is recommended before initiating TNF-blocker therapy. The risks and benefits of treatment should be considered prior to prescribing TNF-blockers, including SIMPONI, to patients who are carriers of HBV. Adequate data are not available on whether anti-viral therapy can reduce the risk of HBV reactivation in HBV carriers who are treated with TNF-blockers. Patients who are carriers of HBV and require treatment with TNF-blockers should be closely monitored for clinical and laboratory signs of active HBV infection throughout therapy and for several months following termination of therapy.
In patients who develop HBV reactivation, TNF-blockers should be stopped and antiviral therapy with appropriate supportive treatment should be initiated. The safety of resuming TNF-blockers after HBV reactivation has been controlled is not known. Therefore, prescribers should exercise caution when considering resumption of TNF-blockers in this situation and monitor patients closely.
5.2 Malignancies
Malignancies, some fatal, have been reported among children, adolescents, and young adults who received treatment with TNF-blocking agents (initiation of therapy ≤ 18 years of age), of which SIMPONI is a member. Approximately half the cases were lymphomas, including Hodgkin's and non-Hodgkin's lymphoma. The other cases represented a variety of malignancies, including rare malignancies that are usually associated with immunosuppression, and malignancies that are not usually observed in children and adolescents. The malignancies occurred after a median of 30 months (range 1 to 84 months) after the first dose of TNF blocker therapy. Most of the patients were receiving concomitant immunosuppressants. These cases were reported post-marketing and are derived from a variety of sources, including registries and spontaneous postmarketing reports.
The risks and benefits of TNF-blocker treatment including SIMPONI should be considered prior to initiating therapy in patients with a known malignancy other than a successfully treated non-melanoma skin cancer (NMSC) or when considering continuing a TNF-blocker in patients who develop a malignancy.
In the controlled portions of clinical trials of TNF-blockers including SIMPONI, more cases of lymphoma have been observed among patients receiving anti-TNF treatment compared with patients in the control groups. During the controlled portions of the Phase 2 trials in RA, and the Phase 3 trials in RA, PsA and AS, the incidence of lymphoma per 100 patient-years of follow-up was 0.21 (95% CI: 0.03, 0.77) in the combined SIMPONI group compared with an incidence of 0 (95% CI: 0., 0.96) in the placebo group. In the controlled and uncontrolled portions of these clinical trials in 2347 SIMPONI-treated patients with a median follow-up of 1.4 years, the incidence of lymphoma was 3.8-fold higher than expected in the general U.S. population according to the SEER database (adjusted for age, gender, and race).1 Through Week 60 of the UC trials, there were no cases of lymphoma with SIMPONI. Patients with RA and other chronic inflammatory diseases, particularly patients with highly active disease and/or chronic exposure to immunosuppressant therapies, may be at higher risk (up to several fold) than the general population for the development of lymphoma, even in the absence of TNF-blocking therapy. Cases of acute and chronic leukemia have been reported with postmarketing TNF-blocker use in rheumatoid arthritis and other indications. Even in the absence of TNF blocker therapy, patients with rheumatoid arthritis may be at a higher risk (approximately 2-fold) than the general population for the development of leukemia.
Rare post-marketing cases of hepatosplenic T-cell lymphoma (HSTCL) have been reported in patients treated with TNF-blocking agents. This rare type of T-cell lymphoma has a very aggressive disease course and is usually fatal. Nearly all of the reported TNF-blocker associated cases have occurred in patients with Crohn's disease with some occurring in ulcerative colitis patients. The majority were in adolescent and young adult males. Almost all these patients had received treatment with azathioprine (AZA) or 6-mercaptopurine (6–MP) concomitantly with a TNF blocker at or prior to diagnosis. The potential risk with the combination of AZA or 6-MP and SIMPONI should be carefully considered. A risk for the development for hepatosplenic T-cell lymphoma in patients treated with TNF-blockers cannot be excluded.
During the controlled portions of the Phase 2 trial in RA, and the Phase 3 trials in RA, PsA and AS, the incidence of malignancies other than lymphoma per 100 patient-years of follow-up was not elevated in the combined SIMPONI group compared with the placebo group. In the controlled and uncontrolled portions of these trials, the incidence of malignancies, other than lymphoma, in SIMPONI-treated patients was similar to that expected in the general U.S. population according to the SEER database (adjusted for age, gender, and race).1 In the 6-week placebo-controlled portions of the SIMPONI Phase 2/3 clinical trials in UC, the incidence of non-lymphoma malignancies (excluding non-melanoma skin cancer) was similar between the SIMPONI and the placebo group. Through Week 60, the incidence of non-lymphoma malignancies (excluding non-melanoma skin cancer) was similar to the general U.S. population according to the SEER database (adjusted for age, gender, and race).1 Short follow-up periods, such as those of one year or less in the studies above, may not adequately reflect the true incidence of malignancies.
It is not known if SIMPONI treatment influences the risk for developing dysplasia or colon cancer. All patients with ulcerative colitis who are at increased risk for dysplasia or colon carcinoma (for example, patients with long-standing ulcerative colitis or primary sclerosing cholangitis), or who had a prior history of dysplasia or colon carcinoma should be screened for dysplasia at regular intervals before therapy and throughout their disease course. This evaluation should include colonoscopy and biopsies per local recommendations. In patients with newly diagnosed dysplasia treated with SIMPONI, the risks and benefits to the individual patient must be carefully reviewed and consideration should be given to whether therapy should be continued.
Melanoma has been reported in patients treated with TNF-blocking agents, including SIMPONI. Merkel cell carcinoma has been reported in patients treated with TNF-blocking agents. Periodic skin examination is recommended for all patients, particularly those with risk factors for skin cancer.
In controlled trials of other TNF-blockers in patients at higher risk for malignancies (e.g., patients with COPD, patients with Wegener's granulomatosis treated with concomitant cyclophosphamide) a greater portion of malignancies occurred in the TNF-blocker group compared to the controlled group. In an exploratory 1-year clinical trial evaluating the use of 50, 100 and 200 mg of SIMPONI in 309 patients with severe persistent asthma, 6 patients developed malignancies other than NMSC in the SIMPONI groups compared to none in the control group. Three of the 6 patients were in the 200 mg SIMPONI group.
5.3 Congestive Heart Failure
Cases of worsening congestive heart failure (CHF) and new onset CHF have been reported with TNF-blockers, including SIMPONI. In several exploratory trials of other TNF-blockers in the treatment of CHF, there were greater proportions of TNF-blocker treated patients who had CHF exacerbations requiring hospitalization or increased mortality. SIMPONI has not been studied in patients with a history of CHF and SIMPONI should be used with caution in patients with CHF. If a decision is made to administer SIMPONI to patients with CHF, these patients should be closely monitored during therapy, and SIMPONI should be discontinued if new or worsening symptoms of CHF appear.
5.4 Demyelinating Disorders
Use of TNF-blockers, of which SIMPONI is a member, has been associated with rare cases of new onset or exacerbation of central nervous system (CNS) demyelinating disorders, including multiple sclerosis (MS) and peripheral demyelinating disorders, including Guillain-Barré syndrome. Cases of central demyelination, MS, optic neuritis, and peripheral demyelinating polyneuropathy have rarely been reported in patients treated with SIMPONI [see Adverse Reactions (6.1)]. Prescribers should exercise caution in considering the use of TNF-blockers, including SIMPONI, in patients with central or peripheral nervous system demyelinating disorders. Discontinuation of SIMPONI should be considered if these disorders develop.
5.5 Use with Abatacept
In controlled trials, the concurrent administration of another TNF-blocker and abatacept was associated with a greater proportion of serious infections than the use of a TNF-blocker alone; and the combination therapy, compared to the use of a TNF-blocker alone, has not demonstrated improved clinical benefit in the treatment of RA. Therefore, the combination of TNF-blockers including SIMPONI and abatacept is not recommended [see Drug Interactions (7.2)].
5.6 Use with Anakinra
Concurrent administration of anakinra (an interleukin-1 antagonist) and another TNF-blocker, was associated with a greater portion of serious infections and neutropenia and no additional benefits compared with the TNF-blocker alone. Therefore, the combination of anakinra with TNF-blockers, including SIMPONI, is not recommended [see Drug Interactions (7.2)].
5.7 Switching Between Biological Disease Modifying Antirheumatic Drugs
Care should be taken when switching from one biological product to another biological product since overlapping biological activity may further increase the risk of infection.
5.8 Hematologic Cytopenias
There have been post-marketing reports of pancytopenia, leukopenia, neutropenia, aplastic anemia, and thrombocytopenia in patients receiving TNF-blockers. In clinical trials, cases of pancytopenia, leukopenia, neutropenia, and thrombocytopenia have also occurred in SIMPONI-treated patients. Caution should be exercised when using TNF-blockers, including SIMPONI, in patients who have or have had significant cytopenias.
5.9 Vaccinations/Therapeutic Infectious Agents
Live Vaccines
Patients treated with SIMPONI may receive vaccinations, except for live vaccines. In patients receiving anti-TNF therapy, limited data are available on the response to live vaccination, or on the secondary transmission of infection by live vaccines. Use of live vaccines could result in clinical infections, including disseminated infections.
Therapeutic Infectious Agents
Other uses of therapeutic infectious agents such as live attenuated bacteria (e.g., BCG bladder instillation for the treatment of cancer) could result in clinical infections, including disseminated infections. It is recommended that therapeutic infectious agents not be given concurrently with SIMPONI.
Non-live Vaccines
In the Phase 3 PsA trial, after pneumococcal vaccination, a similar proportion of SIMPONI-treated and placebo-treated patients were able to mount an adequate immune response of at least a 2-fold increase in antibody titers to pneumococcal polysaccharide vaccine. In both SIMPONI-treated and placebo-treated patients, the proportions of patients with response to pneumococcal vaccine were lower among patients receiving MTX compared with patients not receiving MTX. The data suggest that SIMPONI does not suppress the humoral immune response to the pneumococcal vaccine.
5.10 Hypersensitivity Reactions
In post-marketing experience, serious systemic hypersensitivity reactions (including anaphylactic reaction) have been reported following SIMPONI administration. Some of these reactions occurred after the first administration of SIMPONI. If an anaphylactic or other serious allergic reaction occurs, administration of SIMPONI should be discontinued immediately and appropriate therapy instituted.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety data described below are based on 5 pooled, randomized, double-blind, controlled Phase 3 trials in patients with RA, PsA, and AS (Trials RA-1, RA-2, RA-3, PsA, and AS) [see Clinical Studies (14.1, 14.2, and 14.3)]. These 5 trials included 639 control-treated patients and 1659 SIMPONI-treated patients including 1089 with RA, 292 with PsA, and 278 with AS. The safety data in 1233 SIMPONI-treated patients with ulcerative colitis from 3 pooled, randomized, double-blind, controlled Phase 2/3 trials are also described below (Trials UC-1, UC-2, and UC-3) [see Clinical Studies (14.4)]. The proportion of patients who discontinued treatment due to adverse reactions in the controlled Phase 3 trials through Week 16 in RA, PsA and AS was 2% for SIMPONI-treated patients and 3% for placebo-treated patients. The most common adverse reactions leading to discontinuation of SIMPONI in the controlled Phase 3 trials in RA, PsA and AS through Week 16 were sepsis (0.2%), alanine aminotransferase increased (0.2%), and aspartate aminotransferase increased (0.2%). The most common adverse drug reactions leading to discontinuation through Week 60 of the UC trials in patients who received SIMPONI induction and 100 mg during maintenance compared with patients who received SIMPONI induction and placebo during maintenance were tuberculosis (0.3% vs 0.6%) and anemia (0.3% vs 0%), respectively.
The most serious adverse reactions were:
- Serious Infections [see Warnings and Precautions (5.1)]
- Malignancies [see Warnings and Precautions (5.2)]
Upper respiratory tract infection and nasopharyngitis were the most common adverse reactions reported in the combined Phase 3 RA, PsA and AS trials through Week 16, occurring in 7% and 6% of SIMPONI-treated patients as compared with 6% and 5% of control-treated patients, respectively.
Infections
In controlled Phase 3 trials through Week 16 in RA, PsA, and AS, infections were observed in 28% of SIMPONI-treated patients compared to 25% of control-treated patients. For serious infections, see the Warnings and Precautions section [see Warnings and Precautions (5.1)]. In the controlled Phase 2/3 trial of SIMPONI induction through Week 6 in UC, the rates of infections were similar in SIMPONI 200/100 mg-treated patients and placebo-treated patients, or approximately 12%. Through Week 60, the incidence per patient year of infections was similar in patients who received SIMPONI induction and 100 mg during maintenance compared with patients who received SIMPONI induction and placebo during the maintenance portion of the UC trial.
Demyelinating Disorders
In the controlled Phase 2/3 trial of SIMPONI induction through Week 6, no cases of demyelination were observed in SIMPONI 200/100 mg-treated patients or placebo-treated patients. Through Week 60, there were no cases of demyelination in the SIMPONI 100 mg group during maintenance. One case of CNS demyelination was observed in the placebo maintenance group in a patient who received SIMPONI 400/200 mg during induction.
Liver Enzyme Elevations
There have been reports of severe hepatic reactions including acute liver failure in patients receiving TNF-blockers. In controlled Phase 3 trials of SIMPONI in patients with RA, PsA, and AS through Week 16, ALT elevations ≥ 5 × ULN occurred in 0.2% of control-treated patients and 0.7% of SIMPONI-treated patients and ALT elevations ≥ 3 × ULN occurred in 2% of control-treated patients and 2% of SIMPONI-treated patients. Since many of the patients in the Phase 3 trials for RA, PsA, and AS were also taking medications that cause liver enzyme elevations (e.g., NSAIDs, MTX), the relationship between SIMPONI and liver enzyme elevation is not clear.
In Phase 2/3 UC trials, the incidence of ALT elevations ≥ 5 × ULN was similar in SIMPONI-treated patients and placebo-treated patients, or approximately 1%, with an average duration of follow-up of 46 weeks and 18 weeks, respectively. ALT elevations ≥ 3 × ULN occurred in 2.0% of SIMPONI-treated patients compared with 1.5% of placebo-treated patients with an average duration of follow-up of 46 weeks and 18 weeks, respectively.
Autoimmune Disorders and Autoantibodies
The use of TNF-blockers, including SIMPONI, has been associated with the formation of autoantibodies and, rarely, with the development of a lupus-like syndrome. In the controlled Phase 3 trials in patients with RA, PsA, and AS through Week 14, there was no association of SIMPONI treatment and the development of newly positive anti-dsDNA antibodies. In Phase 3 trials in RA, PsA, and AS through 1 year of follow up, 4.0% of SIMPONI-treated patients and 2.6% of control patients were newly ANA-positive (at titers of 1:160 or greater). The frequency of anti-dsDNA antibodies at 1 year of follow up was uncommon in patients who were anti-dsDNA negative at baseline. Through Week 60 of the UC trials, 3.5% of patients who received SIMPONI induction and 100 mg during maintenance were newly ANA-positive (at titers of 1:160 or greater) compared with 3.5% of patients who received SIMPONI induction and placebo during the maintenance portion of the UC trial. The frequency of anti-dsDNA antibodies at 1 year of follow up in patients who were anti-dsDNA negative at baseline was 0.5% in patients receiving SIMPONI induction and 100 mg during maintenance compared with 0% in patients who received SIMPONI induction and placebo during maintenance.
Injection Site Reactions
In controlled Phase 3 trials through Week 16 in RA, PsA and AS, 6% of SIMPONI-treated patients had injection site reactions compared with 2% of control-treated patients. The majority of the injection site reactions were mild and the most frequent manifestation was injection site erythema.
In the controlled Phase 2/3 trial through Week 6 in UC, 3.4% of SIMPONI-treated patients had injection site reactions compared with 1.5% in control-treated patients. The majority of the injection site reactions were mild and moderate and the most frequent manifestation was injection site erythema.
In controlled Phase 2 and 3 trials in RA, PsA, AS, and Phase 2/3 UC trials, no patients treated with SIMPONI developed anaphylactic reactions.
Immunogenicity
Antibodies to SIMPONI were detected in 57 (4%) of SIMPONI-treated patients across the Phase 3 RA, PsA, and AS trials through Week 24. Similar rates were observed in each of the three indications. Patients who received SIMPONI with concomitant MTX had a lower proportion of antibodies to SIMPONI than patients who received SIMPONI without MTX (approximately 2% versus 7%, respectively).
The presence of serum concentrations of golimumab can interfere with the detection of antibodies to SIMPONI leading to inconclusive results. In UC trials, 34 (3%), 341 (28%) and 823 (69%) of SIMPONI-treated subjects were positive, negative and inconclusive for antibodies to SIMPONI, respectively. Treatment with concomitant immunomodulators (AZA, 6-MP and MTX) resulted in a lower proportion of patients with antibodies to SIMPONI than patients receiving SIMPONI without immunomodulators (2% versus 4%, respectively).
Of the patients with a positive antibody response to SIMPONI in the Phase 2 and 3 trials, most were determined to have neutralizing antibodies to golimumab as measured by a cell-based functional assay.
The small number of patients positive for antibodies to SIMPONI limits the ability to draw definitive conclusions regarding the relationship between antibodies to golimumab and clinical efficacy or safety measures.
The data above reflect the percentage of patients whose test results were considered positive for antibodies to SIMPONI in an ELISA assay, and are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody positivity in an assay may be influenced by several factors including sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to SIMPONI with the incidence of antibodies to other products may be misleading.
Other Adverse Reactions
Table 1 summarizes the adverse drug reactions that occurred at a rate of at least 1% in the SIMPONI ± DMARD group and with a higher incidence than in the placebo ± DMARD group during the controlled period of the 5 pooled Phase 3 trials through Week 16 in patients with RA, PsA, and AS.
| SIMPONI ± DMARDs | Placebo ± DMARDs | |
|---|---|---|
| Patients treated | 1659 | 639 |
| Adverse Reaction | ||
| Infections and Infestations | ||
| Upper respiratory tract infection (nasopharyngitis, pharyngitis, laryngitis, and rhinitis) | 16% | 13% |
| Viral infections (such as influenza and herpes) | 5% | 3% |
| Bronchitis | 2% | 1% |
| Superficial fungal infections | 2% | 1% |
| Sinusitis | 2% | 1% |
| General disorders and administration site conditions | ||
| Injection site reaction (injection site erythema, urticaria, induration, pain, bruising, pruritus, irritation, paresthesia) | 6% | 2% |
| Investigations | ||
| Alanine aminotransferase increased | 4% | 3% |
| Aspartate aminotransferase increased | 3% | 2% |
| Vascular disorders | ||
| Hypertension | 3% | 2% |
| Nervous system disorders | ||
| Dizziness | 2% | 1% |
| Paresthesia | 2% | 1% |
| Gastrointestinal Disorders | ||
| Constipation | 1% | <1% |
Less common clinical trial adverse drug reactions
Adverse drug reactions that occurred <1% in SIMPONI-treated patients during the SIMPONI clinical trials that do not appear in the Warnings and Precautions section included the following events listed by system organ class:
Infections and infestations: Septic shock, atypical mycobacterial infection, pyelonephritis, arthritis bacterial, bursitis infective
Neoplasms benign, malignant and unspecified: Leukemia
Skin and subcutaneous tissue disorders: Psoriasis (new onset or worsening, palmar/plantar and pustular), vasculitis (cutaneous)
Vascular disorders: Vasculitis (systemic)
Other clinical trial adverse drug reactions in ulcerative colitis clinical trials
In the Phase 2/3 trials in UC evaluating 1233 SIMPONI-treated patients, no new adverse drug reactions were identified and the frequency of adverse drug reactions was similar to the safety profile observed in patients with RA, PsA and AS.
6.2 Post-marketing Experience
The following adverse reactions have been identified during post-approval use of SIMPONI. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to SIMPONI exposure.
Immune System Disorders: Serious systemic hypersensitivity reactions (including anaphylactic reaction) [see Warnings and Precautions (5.10)], sarcoidosis
Neoplasms benign, malignant and unspecified: Melanoma [see Warnings and Precautions (5.2)]
Respiratory, thoracic and mediastinal disorders: Interstitial lung disease
Skin and subcutaneous tissue disorders: Skin exfoliation, rash
7 DRUG INTERACTIONS
7.1 Methotrexate
For the treatment of RA, SIMPONI should be used with methotrexate (MTX) [see Clinical Studies (14.1)]. Since the presence or absence of concomitant MTX did not appear to influence the efficacy or safety of SIMPONI in the treatment of PsA or AS, SIMPONI can be used with or without MTX in the treatment of PsA and AS [see Clinical Studies (14.2, 14.3) and Clinical Pharmacology (12.3)].
7.2 Biological Products for RA, PsA, and/or AS
An increased risk of serious infections has been seen in clinical RA trials of other TNF-blockers used in combination with anakinra or abatacept, with no added benefit; therefore, use of SIMPONI with abatacept or anakinra is not recommended [see Warnings and Precautions (5.5, 5.6)]. A higher rate of serious infections has also been observed in RA patients treated with rituximab who received subsequent treatment with a TNF-blocker. The concomitant use of SIMPONI with biologics approved to treat RA, PsA, or AS is not recommended because of the possibility of an increased risk of infection.
7.3 Live Vaccines/Therapeutic Infectious Agents
Live vaccines should not be given concurrently with SIMPONI [see Warnings and Precautions (5.9)].
Therapeutic infectious agents should not be given concurrently with SIMPONI [see Warnings and Precautions (5.9)].
Infants born to women treated with SIMPONI during their pregnancy may be at increased risk of infection for up to 6 months. Administration of live vaccines to infants exposed to SIMPONI in utero is not recommended for 6 months following the mother's last SIMPONI injection during pregnancy [see Use in Specific Populations (8.1)].
7.4 Cytochrome P450 Substrates
The formation of CYP450 enzymes may be suppressed by increased levels of cytokines (e.g., TNFα) during chronic inflammation. Therefore, it is expected that for a molecule that antagonizes cytokine activity, such as golimumab, the formation of CYP450 enzymes could be normalized. Upon initiation or discontinuation of SIMPONI in patients being treated with CYP450 substrates with a narrow therapeutic index, monitoring of the effect (e.g., warfarin) or drug concentration (e.g., cyclosporine or theophylline) is recommended and the individual dose of the drug product may be adjusted as needed.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B – There are no adequate and well-controlled trials of SIMPONI in pregnant women. Because animal reproduction and developmental studies are not always predictive of human response, it is not known whether SIMPONI can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. SIMPONI should be used during pregnancy only if clearly needed.
An embryofetal developmental toxicology study was performed in which pregnant cynomolgus monkeys were treated subcutaneously with golimumab during the first trimester with doses up to 50 mg/kg twice weekly (360 times greater than the maximum recommended human dose-MRHD) and has revealed no evidence of harm to maternal animals or fetuses. Umbilical cord blood samples collected at the end of the second trimester showed that fetuses were exposed to golimumab during gestation. In this study, in utero exposure to golimumab produced no developmental defects to the fetus.
A pre- and post-natal developmental study was performed in which pregnant cynomolgus monkeys were treated with golimumab during the second and third trimesters, and during lactation at doses up to 50 mg/kg twice weekly (860 times and 310 times greater than the maximal steady state human blood levels for maternal animals and neonates, respectively) and has revealed no evidence of harm to maternal animals or neonates. Golimumab was present in the neonatal serum from the time of birth and for up to six months postpartum. Exposure to golimumab during gestation and during the postnatal period caused no developmental defects in the infants.
IgG antibodies are known to cross the placenta during pregnancy and have been detected in the serum of infants born to patients treated with these antibodies. Since SIMPONI is an IgG antibody, infants born to women treated with SIMPONI during their pregnancy may be at increased risk of infection for up to 6 months. Administration of live vaccines to infants exposed to SIMPONI in utero is not recommended for 6 months following the mother's last SIMPONI injection during pregnancy [see Warnings and Precautions (5.9)].
8.3 Nursing Mothers
It is not known whether SIMPONI is excreted in human milk or absorbed systemically after ingestion. Because many drugs and immunoglobulins are excreted in human milk, and because of the potential for adverse reactions in nursing infants from SIMPONI, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
In the pre- and post-natal development study in cynomolgus monkeys in which golimumab was administered subcutaneously during pregnancy and lactation, golimumab was detected in the breast milk at concentrations that were approximately 400-fold lower than the maternal serum concentrations.
8.4 Pediatric Use
Safety and effectiveness of SIMPONI in pediatric patients less than 18 years of age have not been established.
8.5 Geriatric Use
In the Phase 3 trials in RA, PsA, and AS, there were no overall differences in SAEs, serious infections, and AEs in SIMPONI-treated patients ages 65 or older (N = 155) compared with younger SIMPONI-treated patients. In UC, there were insufficient numbers of patients aged 65 and over to determine whether they respond differently from patients aged 18 to 65. Because there is a higher incidence of infections in the geriatric population in general, caution should be used in treating geriatric patients with SIMPONI.
10 OVERDOSAGE
In a clinical trial, 5 patients received protocol-directed single infusions of 10 mg/kg of intravenous SIMPONI without serious adverse reactions or other significant reactions. The highest weight patient was 100 kg, and therefore received a single intravenous infusion of 1000 mg of SIMPONI. There were no SIMPONI overdoses in the clinical trials.
11 DESCRIPTION
SIMPONI (golimumab) is a human IgG1қ monoclonal antibody specific for human tumor necrosis factor alpha (TNFα) that exhibits multiple glycoforms with molecular masses of approximately 150 to 151 kilodaltons. SIMPONI was created using genetically engineered mice immunized with human TNF, resulting in an antibody with human-derived antibody variable and constant regions. SIMPONI is produced by a recombinant cell line cultured by continuous perfusion and is purified by a series of steps that includes measures to inactivate and remove viruses.
The SIMPONI drug product is a sterile solution of the golimumab antibody supplied as either a single dose prefilled syringe (with a passive needle safety guard) or a single dose prefilled autoinjector. The Type 1 glass syringe has a coated stopper. The fixed stainless steel needle (5 bevel, 27G, half-inch) is covered with a needle shield to prevent leakage of the solution through the needle and to protect the needle during handling prior to subcutaneous administration. The needle shield is made of a dry natural rubber containing latex.
SIMPONI does not contain preservatives. The solution is clear to slightly opalescent, colorless to light yellow with a pH of approximately 5.5. SIMPONI is provided in two strengths: 50 mg of the golimumab antibody in 0.5 mL of solution and 100 mg of the golimumab antibody in 1 mL of solution. In the 50 mg strength, 0.5 mL of SIMPONI contains 50 mg of the golimumab antibody, 0.44 mg of L-histidine and L-histidine monohydrochloride monohydrate, 20.5 mg of sorbitol, 0.08 mg of polysorbate 80, and Water for Injection. In the 100 mg strength, 1 mL of SIMPONI contains 100 mg of the golimumab antibody, 0.87 mg of L-histidine and L-histidine monohydrochloride monohydrate, 41.0 mg of sorbitol, 0.15 mg of polysorbate 80, and Water for Injection.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Golimumab is a human monoclonal antibody that binds to both the soluble and transmembrane bioactive forms of human TNFα. This interaction prevents the binding of TNFα to its receptors, thereby inhibiting the biological activity of TNFα (a cytokine protein). There was no evidence of the golimumab antibody binding to other TNF superfamily ligands; in particular, the golimumab antibody did not bind or neutralize human lymphotoxin. Golimumab did not lyse human monocytes expressing transmembrane TNF in the presence of complement or effector cells.
Elevated TNFα levels in the blood, synovium, and joints have been implicated in the pathophysiology of several chronic inflammatory diseases such as rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. TNFα is an important mediator of the articular inflammation that is characteristic of these diseases. The exact mechanism by which golimumab treats ulcerative colitis is unknown. Golimumab modulated the in vitro biological effects mediated by TNF in several bioassays, including the expression of adhesion proteins responsible for leukocyte infiltration (E-selectin, ICAM-1 and VCAM-1) and the secretion of proinflammatory cytokines (IL-6, IL-8, G-CSF and GM-CSF).
12.2 Pharmacodynamics
In clinical trials, decreases in C-reactive protein (CRP), interleukin (IL)-6, matrix metalloproteinase 3 (MMP-3), intercellular adhesion molecule (ICAM)-1 and vascular endothelial growth factor (VEGF) were observed following SIMPONI administration in patients with RA, PsA, and AS.
12.3 Pharmacokinetics
Absorption
Following subcutaneous administration of SIMPONI to healthy subjects and patients with active RA, the median time to reach maximum serum concentrations (Tmax) ranged from 2 to 6 days. A subcutaneous injection of 50 mg SIMPONI to healthy subjects produced a mean ± standard deviation maximum serum concentration (Cmax) of 3.2 ± 1.4 µg/mL.
By cross-trial comparisons of mean AUCinf values following an IV or subcutaneous administration of SIMPONI, the absolute bioavailability of subcutaneous SIMPONI was estimated to be approximately 53%.
Distribution
Following a single IV administration over the dose range of 0.1 to 10.0 mg/kg in patients with active RA, mean volume of distribution ranged from 58 to 126 mL/kg. The volume of distribution for SIMPONI indicates that SIMPONI is distributed primarily in the circulatory system with limited extravascular distribution.
Metabolism
The exact metabolic pathway of golimumab is unknown.
Elimination
Following a single IV administration over the dose range of 0.1 to 10.0 mg/kg in patients with active RA, mean systemic clearance of SIMPONI was estimated to be 4.9 to 6.7 mL/day/kg.
Median terminal half-life values were estimated to be approximately 2 weeks in healthy subjects and patients with active RA, PsA or AS.
Population PK analyses indicated that concomitant use of NSAIDs, oral corticosteroids, or sulfasalazine did not influence the apparent clearance of SIMPONI.
Patients who developed anti-golimumab antibodies generally had lower steady-state serum trough concentrations of SIMPONI.
Dose linearity
SIMPONI exhibited dose-proportional pharmacokinetics (PK) in patients with active RA over the dose range of 0.1 to 10 mg/kg following a single intravenous (IV) dose. Following a single SC dose in healthy subjects, dose proportional pharmacokinetics were also observed over a dose range of 50 mg to 400 mg.
Single dose versus multiple doses
When 50 mg SIMPONI was administered subcutaneous to patients with RA, PsA, or AS every 4 weeks, serum concentrations appeared to reach steady state by Week 12. With concomitant use of methotrexate (MTX), treatment with 50 mg SIMPONI subcutaneous every 4 weeks resulted in a mean steady-state trough serum concentration of approximately 0.4–0.6 µg/mL in patients with active RA, approximately 0.5 µg/mL in patients with active PsA, and approximately 0.8 µg/mL in patients with active AS. Patients with RA, PsA, and AS treated with SIMPONI 50 mg and MTX had approximately 52%, 36% and 21% higher mean steady-state trough concentrations of golimumab, respectively compared with those treated with SIMPONI 50 mg without MTX. The presence of MTX also decreased anti-golimumab antibody incidence from 7% to 2% [see Adverse Reactions (6.1)]. For RA, SIMPONI should be used with MTX. In the PsA and AS trials, the presence or absence of concomitant MTX did not appear to influence clinical efficacy and safety parameters [see Drug Interactions (7.1) and Clinical Studies (14.1)].
When induction doses of 200 mg and 100 mg SIMPONI at week 0 and 2, respectively, followed by maintenance doses of 100 mg SIMPONI every 4 weeks were administered subcutaneously in patients with UC, serum golimumab concentrations reached steady state by week 8 after the first maintenance dose. Treatment with 100 mg SIMPONI subcutaneous every 4 weeks during maintenance resulted in a mean steady-state trough serum concentration of approximately 1.8 ± 1.1 µg/mL.
Effect of weight on pharmacokinetics
Population PK analyses showed there was a trend toward higher apparent clearance of SIMPONI with increasing weight. Treatment with the recommended maintenance dose regimen of SIMPONI 100 mg in UC patients did not result in meaningful differences in clinical efficacy among different weight groups. Across the PsA and AS populations, no meaningful differences in clinical efficacy were observed among the subgroups by weight quartile. The RA trial in MTX-experienced and TNF-blocker-naïve patients (Trial RA-2) did show evidence of a reduction in clinical efficacy with increasing body weight, but this effect was observed for both tested doses of SIMPONI (50 mg and 100 mg). There is no need to adjust the dosage of SIMPONI based on a patient's weight.
Special populations
Population PK analyses suggested no PK differences between male and female patients after body weight adjustment in the RA, PsA and UC trials. In the AS trial, female patients showed 13% higher apparent clearance than male patients after body weight adjustment. Subgroup analysis based on gender showed that both female and male patients achieved clinically significant response at the proposed clinical dose. Dosage adjustment based on gender is not needed.
Population PK analyses indicated that PK parameters of SIMPONI were not influenced by age in adult patients. Patients with age ≥ 65 years had apparent clearance of SIMPONI similar to patients with age < 65 years. No ethnicity-related PK differences were observed between Caucasians and Asians, and there were too few patients of other races to assess for PK differences.
No formal trial of the effect of renal or hepatic impairment on the PK of golimumab was conducted.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies of golimumab have not been conducted to evaluate its carcinogenic potential. Mutagenicity studies have not been conducted with golimumab. A fertility study conducted in mice using an analogous anti-mouse TNFα antibody showed no impairment of fertility.
14 CLINICAL STUDIES
14.1 Rheumatoid Arthritis
The efficacy and safety of SIMPONI were evaluated in 3 multicenter, randomized, double-blind, controlled trials (Trials RA-1, RA-2, and RA-3) in 1542 patients ≥ 18 years of age with moderately to severely active RA, diagnosed according to the American College of Rheumatology (ACR) criteria, for at least 3 months prior to administration of trial agent. Patients were required to have at least 4 swollen and 4 tender joints. SIMPONI was administered subcutaneously at doses of 50 mg or 100 mg every 4 weeks. Double-blinded controlled efficacy data were collected and analyzed through Week 24. Patients were allowed to continue stable doses of concomitant low dose corticosteroids (equivalent to ≤ 10 mg of prednisone a day) and/or NSAIDs and patients may have received oral MTX during the trials.
Trial RA-1 evaluated 445 patients who were previously treated (at least 8 to 12 weeks prior to administration of trial agent) with one or more doses of a biologic TNF-blocker without a serious adverse reaction. Patients may have discontinued the biologic TNF-blocker for a variety of reasons. Patients were randomized to receive placebo (n = 150), SIMPONI 50 mg (n = 147), or SIMPONI 100 mg (n = 148). Patients were allowed to continue stable doses of concomitant MTX, sulfasalazine (SSZ), and/or hydroxychloroquine (HCQ) during the trial. The use of other DMARDs including cytotoxic agents or other biologics was prohibited.
Trial RA-2 evaluated 444 patients who had active RA despite a stable dose of at least 15 mg/week of MTX and who had not been previously treated with a biologic TNF-blocker. Patients were randomized to receive background MTX (n = 133), SIMPONI 50 mg + background MTX (n = 89), SIMPONI 100 mg + background MTX (n = 89), or SIMPONI 100 mg monotherapy (n = 133). The use of other DMARDs including SSZ, HCQ, cytotoxic agents, or other biologics was prohibited.
Trial RA-3 evaluated 637 patients with active RA who were MTX-naïve and had not previously been treated with a biologic TNF-blocker. Patients were randomized to receive MTX (n = 160), SIMPONI 50 mg + MTX (n = 159), SIMPONI 100 mg + MTX (n = 159), or SIMPONI 100 mg monotherapy (n = 159). For patients receiving MTX, MTX was administered at a dose of 10 mg/week beginning at Week 0 and increased to 20 mg/week by Week 8. The use of other DMARDs including SSZ, HCQ, cytotoxic agents, or other biologics was prohibited.
The primary endpoint in Trial RA-1 and Trial RA-2 was the percentage of patients achieving an ACR 20 response at Week 14 and the primary endpoint in Trial RA-3 was the percentage of patients achieving an ACR 50 response at Week 24.
In Trials RA-1, RA-2, and RA-3, the median duration of RA disease was 9.4, 5.7, and 1.2 years; and 99%, 75%, and 54% of the patients used at least one DMARD in the past, respectively. Approximately 77% and 57% of patients received concomitant NSAIDs and low dose corticosteroids, respectively, in the 3 pooled RA trials.
Clinical Response
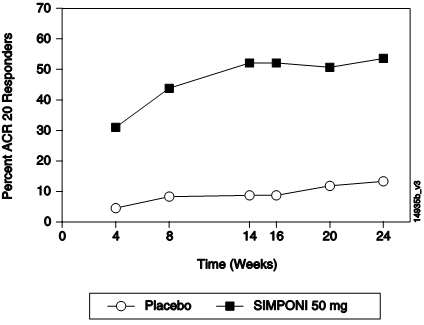
In the 3 RA trials, a greater percentage of patients treated with the combination of SIMPONI and MTX achieved ACR responses at Week 14 (Trials RA-1 and RA-2) and Week 24 (Studies RA-1, RA-2, and RA-3) versus patients treated with the MTX alone. There was no clear evidence of improved ACR response with the higher SIMPONI dose group (100 mg) compared to the lower SIMPONI dose group (50 mg). In Trials RA-2 and RA-3, the SIMPONI monotherapy groups were not statistically different from the MTX monotherapy groups in ACR responses. Table 2 shows the proportion of patients with the ACR response for the SIMPONI 50 mg and control groups in Trials RA-1, RA-2, and RA-3. In the subset of patients who received SIMPONI in combination with MTX in Trial RA-1, the proportion of patients achieving ACR 20, 50 and 70 responses at week 14 were 40%, 18%, and 12%, respectively, in the SIMPONI 50 mg + MTX group (N = 101) compared with 17%, 6%, and 2%, respectively, in the placebo + MTX group (N = 103). Table 3 shows the percent improvement in the components of the ACR response criteria for the SIMPONI 50 mg + MTX and MTX groups in Trial RA-2. The percent of patients achieving ACR 20 responses by visit for Trial RA-2 is shown in Figure 1. ACR 20 responses were observed in 38% of patients in the SIMPONI 50 mg + MTX group at the first assessment (Week 4) after the initial SIMPONI administration.
| Trial RA-1 Active RA previously treated with one or more doses of TNF-blockers |
Trial RA-2 Active RA, despite MTX |
Trial RA-3 Active RA, MTX Naïve |
||||
|---|---|---|---|---|---|---|
Placebo ± DMARDs |
SIMPONI 50 mg ± DMARDs |
Background MTX | SIMPONI 50 mg + Background MTX | MTX | SIMPONI 50 mg + MTX | |
| N |
150 | 147 | 133 | 89 | 160 | 159 |
| ACR 20 | ||||||
| Week 14 | 18% | 35% | 33% | 55% | NA |
NA |
| Week 24 | 16% | 31% | 28% | 60% | 49% | 62% |
| ACR 50 | ||||||
| Week 14 | 7% | 15% | 10% | 35% | NA |
NA |
| Week 24 | 4% | 16% | 14% | 37% | 29% | 40% |
| ACR 70 | ||||||
| Week 14 | 2% | 10% | 4% | 13% | NA |
NA |
| Week 24 | 2% | 9% | 5% | 20% | 16% | 24% |
| Background MTX | SIMPONI 50 mg + Background MTX | |
|---|---|---|
| Note: Baseline values are medians. | ||
| N |
133 | 89 |
| Number of swollen joints (0–66) | ||
| Baseline | 12 | 13 |
| Week 14 | 38% | 62% |
| Number of tender joints (0–68) | ||
| Baseline | 21 | 26 |
| Week 14 | 30% | 60% |
| Patient's assessment of pain (0–10) | ||
| Baseline | 5.7 | 6.1 |
| Week 14 | 18% | 55% |
| Patient's global assessment of disease activity (0–10) | ||
| Baseline | 5.3 | 6.0 |
| Week 14 | 15% | 45% |
| Physician's global assessment of disease activity (0–10) | ||
| Baseline | 5.7 | 6.1 |
| Week 14 | 35% | 55% |
| HAQ score (0–3) | ||
| Baseline | 1.25 | 1.38 |
| Week 14 | 10% | 29% |
| CRP (mg/dL) | ||
| Baseline | 0.8 | 1.0 |
| Week 14 | 2% | 44% |
|
Figure 1. Trial RA - 2 – Percent of Patients Achieving ACR 20 Response by Visit: Randomized Patients |

|
Physical Function Response in Patients with RA
In Trials RA-1 and RA-2, the SIMPONI 50 mg groups demonstrated a greater improvement compared to the control groups in the change in mean Health Assessment Questionnaire Disability Index (HAQ-DI) score from baseline to Week 24: 0.23 vs. 0.03 in RA-1, 0.47 vs. 0.13 in RA-2, respectively. Also in Trials RA-1 and RA-2, the SIMPONI 50 mg groups compared to the control groups had a greater proportion of HAQ responders (change from baseline > 0.22) at Week 24: 43% vs. 27%, 65% vs. 35%, respectively.
14.2 Psoriatic Arthritis
The safety and efficacy of SIMPONI were evaluated in a multi-center, randomized, double-blind, placebo-controlled trial in 405 adult patients with moderately to severely active PsA (≥ 3 swollen joints and ≥ 3 tender joints) despite NSAID or DMARD therapy (Trial PsA). Patients in this trial had a diagnosis of PsA for at least 6 months with a qualifying psoriatic skin lesion of at least 2 cm in diameter. Previous treatment with a biologic TNF-blocker was not allowed. Patients were randomly assigned to placebo (n = 113), SIMPONI 50 mg (n = 146), or SIMPONI 100 mg (n = 146) given subcutaneously every 4 weeks. Patients were allowed to receive stable doses of concomitant MTX (≤ 25 mg/week), low dose oral corticosteroids (equivalent to ≤ 10 mg of prednisone a day), and/or NSAIDs during the trial. The use of other DMARDs including SSZ, HCQ, cytotoxic agents, or other biologics was prohibited. The primary endpoint was the percentage of patients achieving ACR 20 response at Week 14. Placebo-controlled efficacy data were collected and analyzed through Week 24.
Patients with each subtype of PsA were enrolled, including polyarticular arthritis with no rheumatoid nodules (43%), asymmetric peripheral arthritis (30%), distal interphalangeal (DIP) joint arthritis (15%), spondylitis with peripheral arthritis (11%), and arthritis mutilans (1%). The median duration of PsA disease was 5.1 years, 78% of patients received at least one DMARD in the past, and approximately 48% of patients received MTX, and 16% received low dose oral steroids.
Clinical Response in Patients with PsA
SIMPONI ± MTX, compared with placebo ± MTX, resulted in significant improvement in signs and symptoms as demonstrated by the proportion of patients with an ACR 20 response at Week 14 in Trial PsA (see Table 4). There was no clear evidence of improved ACR response with the higher SIMPONI dose group (100 mg) compared to the lower SIMPONI dose group (50 mg). ACR responses observed in the SIMPONI-treated groups were similar in patients receiving and not receiving concomitant MTX. Similar ACR 20 responses at Week 14 were observed in patients with different PsA subtypes. However, the number of patients with arthritis mutilans was too small to allow meaningful assessment. SIMPONI 50 mg treatment also resulted in significantly greater improvement compared with placebo for each ACR component in Trial PsA (Table 5). Treatment with SIMPONI resulted in improvement in enthesitis and skin manifestations in patients with PsA. However, the safety and efficacy of SIMPONI in the treatment of patients with plaque psoriasis has not been established.
The percent of patients achieving ACR 20 responses by visit for Trial PsA is shown in Figure 2. ACR 20 responses were observed in 31% of patients in the SIMPONI 50 mg + MTX group at the first assessment (Week 4) after the initial SIMPONI administration.
Placebo ± MTX |
SIMPONI 50 mg ± MTX |
|
|---|---|---|
| Bold text indicates primary endpoint. | ||
| N |
113 | 146 |
| ACR 20 | ||
| Week 14 | 9% | 51% |
| Week 24 | 12% | 52% |
| ACR 50 | ||
| Week 14 | 2% | 30% |
| Week 24 | 4% | 32% |
| ACR 70 | ||
| Week 14 | 1% | 12% |
| Week 24 | 1% | 19% |
Placebo± MTX |
SIMPONI 50 mg ± MTX |
|
|---|---|---|
| Note: Baseline are median values. | ||
| N
|
113 | 146 |
| Number of swollen joints (0–66) | ||
| Baseline | 10.0 | 11.0 |
| Week 14 | 8% | 60% |
| Number of tender joints (0–68) | ||
| Baseline | 18.0 | 19.0 |
| Week 14 | 0% | 54% |
| Patient's assessment of pain (0–10) | ||
| Baseline | 5.4 | 5.8 |
| Week 14 | -1% | 48% |
| Patient's global assessment of disease activity (0–10) | ||
| Baseline | 5.2 | 5.2 |
| Week 14 | 2% | 49% |
| Physician's global assessment of disease activity (0–10) | ||
| Baseline | 5.2 | 5.4 |
| Week 14 | 7% | 59% |
| HAQ score (0–10) | ||
| Baseline | 1.0 | 1.0 |
| Week 14 | 0% | 28% |
| CRP (mg/dL) (0–10) | ||
| Baseline | 0.6 | 0.6 |
| Week 14 | 0% | 40% |
|
Figure 2. Trial PsA – Percent of ACR 20 PsA Responders by Visit: Randomized Patients |
|
Physical Function Response in Patients with PsA
In Trial PsA, SIMPONI 50 mg demonstrated a greater improvement compared to placebo in the change in mean Health Assessment Questionnaire Disability Index (HAQ-DI) score from baseline to Week 24 (0.33 and -0.01, respectively). In addition, the SIMPONI 50 mg group compared to the placebo group had a greater proportion of HAQ responders (≥ 0.3 change from baseline) at Week 24: 43% vs. 22%, respectively.
14.3 Ankylosing Spondylitis
The safety and efficacy of SIMPONI were evaluated in a multi-center, randomized, double-blind, placebo-controlled trial in 356 adult patients with active ankylosing spondylitis according to modified New York criteria for at least 3 months (Trial AS). Patients had symptoms of active disease [defined as a Bath AS Disease Activity Index (BASDAI) ≥ 4 and VAS for total back pain of ≥ 4, on scales of 0 to 10 cm] despite current or previous NSAID therapy. Patients were excluded if they were previously treated with a biologic TNF-blocker or if they had complete ankylosis of the spine. Patients were randomly assigned to placebo (n = 78), SIMPONI 50 mg (n = 138), or SIMPONI 100 mg (n = 140) administered subcutaneously every 4 weeks. Patients were allowed to continue stable doses of concomitant MTX, sulfasalazine (SSZ), hydroxychloroquine (HCQ), low dose corticosteroids (equivalent to < 10 mg of prednisone a day), and/or NSAIDs during the trial. The use of other DMARDs including cytotoxic agents or other biologics was prohibited.
The primary endpoint was the percentage of patients achieving an ASsessment in Ankylosing Spondylitis (ASAS) 20 response at Week 14. Placebo-controlled efficacy data were collected and analyzed through Week 24.
In Trial AS, the median duration of AS disease was 5.6 years, median duration of inflammatory back pain was 12 years, 83% were HLA-B27 positive, 24% had prior joint surgery or procedure, and 55% received at least one DMARD in the past. During the trial, the use of concomitant DMARDs and/or NSAIDs was as follows: MTX (20%), SSZ (26%), HCQ (1%), low dose oral steroids (16%), and NSAIDs (90%).
Clinical Response in Patients with AS
In Trial AS, SIMPONI ± DMARDs treatment, compared with placebo ± DMARDs, resulted in a significant improvement in signs and symptoms as demonstrated by the proportion of patients with an ASAS 20 response at Week 14 (see Table 6). There was no clear evidence of improved ASAS response with the higher SIMPONI dose group (100 mg) compared to the lower SIMPONI dose group (50 mg). Table 7 shows the percent improvement in the components of the ASAS response criteria for the SIMPONI 50 mg ± DMARDs and placebo ± DMARDs groups in Trial AS.
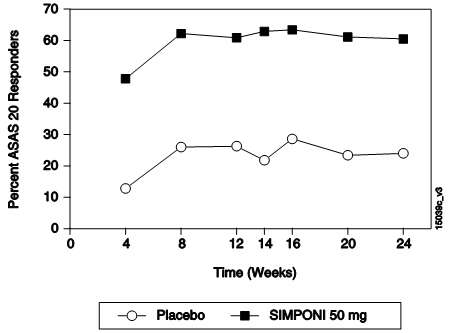
The percent of patients achieving ASAS 20 responses by visit for Trial AS is shown in Figure 3. ASAS 20 responses were observed in 48% of patients in the SIMPONI 50 mg + MTX group at the first assessment (Week 4) after the initial SIMPONI administration.
Placebo ± DMARDs |
SIMPONI 50 mg ± DMARDs |
|
|---|---|---|
| Bold text indicates primary endpoint. | ||
| N |
78 | 138 |
| Responders, % of patients | ||
| ASAS 20 | ||
| Week 14 | 22% | 59% |
| Week 24 | 23% | 56% |
| ASAS 40 | ||
| Week 14 | 15% | 45% |
| Week 24 | 15% | 44% |
Placebo ± DMARDs |
SIMPONI 50 mg ± DMARDs |
|
|---|---|---|
|
N
|
78 | 138 |
| ASAS components | ||
| Patient global assessment (0–10) | ||
| Baseline | 7.2 | 7.0 |
| Week 14 | 13% | 47% |
| Total back pain (0–10) | ||
| Baseline | 7.6 | 7.5 |
| Week 14 | 9% | 50% |
|
BASFI (0–10) |
||
| Baseline | 4.9 | 5.0 |
| Week 14 | -3% | 37% |
|
Inflammation (0–10) |
||
| Baseline | 7.1 | 7.1 |
| Week 14 | 6% | 59% |
|
Figure 3. Trial AS – Percent of AS Patients Achieving ASAS 20 Response by Visit: Randomized Patients |
|
14.4 Ulcerative Colitis
The safety and efficacy of SIMPONI were evaluated in two multi-center, randomized, double-blind, placebo-controlled clinical trials in patients ≥ 18 years of age (Trials UC-1 and UC-2).
Trial UC-1 was an induction trial conducted in patients with moderately to severely active ulcerative colitis (UC), defined as a Mayo score of 6 to 12 [the Mayo score ranges from 0 to 12 and has four subscales that are each scored from 0 (normal) to 3 (most severe): stool frequency, rectal bleeding, findings on endoscopy, and physician global assessment]. At baseline, subjects also had an endoscopy subscore of 2 or 3 on a 3-point scale (an endoscopy score of 2 is defined by marked erythema, absent vascular pattern, friability, erosions; and a score of 3 is defined by spontaneous bleeding, ulceration). Patients were corticosteroid dependent (i.e., an inability to successfully taper corticosteroids without a return of the symptoms of UC) or had an inadequate response to or had failed to tolerate at least one of the following therapies: oral aminosalicylates, oral corticosteroids, azathioprine, or 6-mercaptopurine.
Trial UC-1 was divided into 2 parts. In Part 1 (dose finding), patients were randomized to one of 4 treatment groups: 400 mg SIMPONI administered subcutaneously (SC) at Week 0 and 200 mg at Week 2 (400/200 mg), 200 mg SIMPONI SC at Week 0 and 100 mg at Week 2 (200/100 mg), 100 mg SIMPONI SC at Week 0 and 50 mg at Week 2 (100/50 mg), or placebo SC at Weeks 0 and 2. In Part 2 (dose confirming), efficacy was evaluated in 761 patients who were randomized to receive either 400 mg SIMPONI SC at Week 0 and 200 mg at Week 2, 200 mg SIMPONI SC at Week 0 and 100 mg at Week 2, or placebo SC at Weeks 0 and 2. SIMPONI 100/50 mg SC was not evaluated in Part 2; its safety and effectiveness has not been established in UC. Concomitant stable doses of oral aminosalicylates (5-ASA), oral corticosteroids (less than 40 mg/day), azathioprine (AZA), 6-mercaptopurine (6-MP), and/or methotrexate (MTX) were permitted. Patients who received previous TNF inhibitors were excluded. The primary endpoint was the percent of patients in clinical response at Week 6, defined as a decrease from baseline in the Mayo score by ≥ 30% and ≥ 3 points, accompanied by a decrease in the rectal bleeding subscore of ≥ 1 or a rectal bleeding subscore of 0 (no blood seen) or 1 (streaks of blood with stool less than half the time).
Trial UC-2 was a randomized-withdrawal maintenance trial that evaluated 456 patients who achieved clinical response with SIMPONI induction and tolerated SIMPONI treatment. Patients were randomized to receive SIMPONI 50 mg, SIMPONI 100 mg or placebo administered subcutaneously every 4 weeks. Concomitant stable doses of oral aminosalicylates, azathioprine, 6-mercaptopurine, and/or methotrexate were permitted. Corticosteroids were to be tapered at the start of the maintenance trial. The primary endpoint was the percent of patients maintaining clinical response through Week 54.
Clinical Response, Clinical Remission and Improvement of Endoscopic Appearance of the Mucosa:
In Trial UC-1, a greater proportion of patients achieved clinical response, clinical remission and had improvement of endoscopic appearance of the mucosa at Week 6 in the SIMPONI 200/100 mg group compared with the placebo group. The SIMPONI 400/200 mg group did not demonstrate additional clinical benefit over the SIMPONI 200/100 mg group. Clinical response was defined as a decrease from baseline in the Mayo score of ≥ 30% and ≥ 3 points, accompanied by a decrease in the rectal bleeding subscore of ≥ 1 or a rectal bleeding subscore of 0 or 1. Clinical remission was defined as a Mayo score ≤ 2 points, with no individual subscore > 1. Improvement of endoscopic appearance of the mucosa was defined as a Mayo endoscopy subscore of 0 (normal or inactive disease) or 1 (erythema, decreased vascular pattern, mild friability).
In Trial UC-2, a greater proportion of patients maintained clinical response through Week 54 in the SIMPONI 100 mg group compared with the placebo group. In Trial UC-2, SIMPONI-treated patients in clinical response (which included the subset of patients in clinical remission) in Trial UC-1, were again assessed for clinical remission at Week 30 and Week 54. A greater proportion of patients had clinical remission at both Weeks 30 and 54 without demonstrating a loss of response at any time point through Week 54 in the SIMPONI 100 mg group compared with the placebo group.
These results are shown in Table 8 below.
| Trial UC-1 (6-Week Induction Trial) | |||
|
Placebo N=251 |
SIMPONI 200/100 mg N=253 |
Treatment difference (95% C.I.) |
|
Clinical response |
30% | 51% | 21% (12%, 29%)  |
Clinical remission |
6% | 18% | 11% (6%, 17%)  |
Improvement of endoscopic appearance of the mucosa at Week 6 |
29% | 42% | 14% (5%, 22%) |
|
Trial UC-2 (54-Week Maintenance Trial) |
|||
|
Placebo N=154 |
SIMPONI 100 mg N=151 |
Treatment difference (95% C.I.) |
|
Clinical response |
31% | 50% | 19% (8%, 29%) |
Clinical remission |
16% | 28% | 12% (3%, 21%) |
15 REFERENCES
- SEER [database online]. US Population Data – 1969–2004. Bethesda, MD: National Cancer Institute. Release date: January 3, 2007. Available at: http//seer.cancer.gov/popdata/.
16 HOW SUPPLIED/STORAGE AND HANDLING
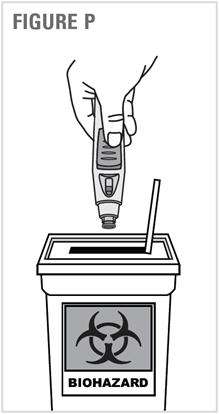
Each SIMPONI prefilled autoinjector or prefilled syringe is packaged in a light-blocking, cardboard outer carton. SIMPONI is available in packs of 1 single dose prefilled syringe or 1 single dose prefilled SmartJect autoinjector. Both the prefilled syringe and the SmartJect autoinjector are for single use and are not to be divided.
Prefilled SmartJect Autoinjector
- Each 50 mg single dose SmartJect autoinjector contains a prefilled glass syringe (27 gauge ½ inch) providing 50 mg of SIMPONI per 0.5 mL of solution. The NDC number for the 50 mg prefilled SmartJect autoinjector is 57894-070-02.
- Each 100 mg single dose SmartJect autoinjector contains a prefilled glass syringe (27 gauge ½ inch) providing 100 mg of SIMPONI per 1 mL of solution. The NDC number for the 100 mg prefilled SmartJect autoinjector is 57894-071-02.
Prefilled Syringe
- Each 50 mg single dose prefilled glass syringe (27 gauge ½ inch) contains 50 mg of SIMPONI per 0.5 mL of solution. The NDC number for the 50 mg prefilled syringe is 57894-070-01.
- Each 100 mg single dose prefilled glass syringe (27 gauge ½ inch) contains 100 mg of SIMPONI per 1 mL of solution. The NDC number for the 100 mg prefilled syringe is 57894-071-01.
Storage and Handling
SIMPONI must be refrigerated at 2°C to 8°C (36°F to 46°F) and protected from light. Keep the product in the original carton to protect from light until the time of use. Do not freeze. Do not shake. Do not use SIMPONI beyond the expiration date (EXP) on the carton or the expiration date on the prefilled syringe (observed through the viewing window) or the prefilled SmartJect autoinjector.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide and Instructions for Use)
Patients should be advised of the potential benefits and risks of SIMPONI. Physicians should instruct their patients to read the Medication Guide before starting SIMPONI therapy and to read it each time the prescription is renewed.
Infections
Inform patients that SIMPONI may lower the ability of their immune system to fight infections. Instruct the patient of the importance of contacting their doctor if they develop any symptoms of infection, including tuberculosis, invasive fungal infections, and hepatitis B reactivation.
Malignancies
Patients should be counseled about the risk of lymphoma and other malignancies while receiving SIMPONI.
Allergic Reactions
Advise latex-sensitive patients that the needle cover on the prefilled syringe as well as the prefilled syringe in the prefilled SmartJect autoinjector contains dry natural rubber (a derivative of latex).
Other Medical Conditions
Advise patients to report any signs of new or worsening medical conditions such as congestive heart failure, demyelinating disorders, autoimmune diseases, liver disease, cytopenias, or psoriasis.
Instructions for Safe Administration
The first self-injection should be performed under the supervision of a qualified healthcare professional. If a patient or caregiver is to administer SIMPONI, he/she should be instructed in injection techniques and their ability to inject subcutaneously should be assessed to ensure the proper administration of SIMPONI
Advise the patient to read the FDA-approved Instructions for Use and provide the following instructions to patients:
- Prior to use, remove the prefilled syringe or the prefilled SmartJect autoinjector from the refrigerator and allow SIMPONI to sit at room temperature outside of the carton for 30 minutes and out of the reach of children.
- Do not warm SIMPONI in any other way. For example, do not warm SIMPONI in a microwave or in hot water.
- Do not remove the prefilled syringe needle cover or SmartJect autoinjector cap while allowing SIMPONI to reach room temperature. Remove these immediately before injection.
- Do not pull the autoinjector away from the skin until you hear a first "click" sound and then a second "click" sound (the injection is finished and the needle is pulled back). It usually takes about 3 to 6 seconds but may take up to 15 seconds for you to hear the second "click" after the first "click". If the autoinjector is pulled away from the skin before the injection is completed, a full dose of SIMPONI may not be administered.
- A puncture-resistant container for disposal of needles and syringes should be used. Patients or caregivers should be instructed in the technique of proper syringe and needle disposal, and be advised not to reuse these items.
Manufactured by:
Janssen Biotech, Inc.
Horsham, PA 19044
US License No. 1864
© Janssen Biotech, Inc. 2014
MEDICATION GUIDE
SIMPONI® (SIM-po-nee)
(golimumab)
Read the Medication Guide that comes with SIMPONI before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your doctor about your medical condition or treatment. It is important to remain under your doctor's care while using SIMPONI.
What is the most important information I should know about SIMPONI?
SIMPONI is a medicine that affects your immune system. SIMPONI can lower the ability of your immune system to fight infections. Some people have serious infections while taking SIMPONI, including tuberculosis (TB), and infections caused by bacteria, fungi, or viruses that spread throughout their body. Some people have died from these serious infections.
- Your doctor should test you for TB and hepatitis B before starting SIMPONI.
- Your doctor should monitor you closely for signs and symptoms of TB during treatment with SIMPONI.
You should not start taking SIMPONI if you have any kind of infection unless your doctor says it is okay.
Before starting SIMPONI, tell your doctor if you:
- think you have an infection or have symptoms of an infection such as:
- fever, sweat, or chills
- muscle aches
- cough
- shortness of breath
- blood in phlegm
- weight loss
- warm, red, or painful skin or sores on your body
- diarrhea or stomach pain
- burning when you urinate or urinate more often than normal
- feel very tired
- are being treated for an infection
- get a lot of infections or have infections that keep coming back
- have diabetes, HIV, or a weak immune system. People with these conditions have a higher chance for infections.
- have TB, or have been in close contact with someone with TB
- live, have lived, or traveled to certain parts of the country (such as the Ohio and Mississippi River valleys and the Southwest) where there is an increased chance for getting certain kinds of fungal infections (histoplasmosis, coccidioidomycosis, blastomycosis). These infections may happen or become more severe if you use SIMPONI. Ask your doctor if you do not know if you have lived in an area where these infections are common.
- have or have had hepatitis B
- use the medicine ORENCIA (abatacept), KINERET (anakinra), ACTEMRA (tocilizumab) or RITUXAN (rituximab)
After starting SIMPONI, call your doctor right away if you have any symptoms of an infection. SIMPONI can make you more likely to get infections or make worse any infection that you have.
Cancer
- For children and adults taking TNF-blocker medicines, including SIMPONI, the chances of getting cancer may increase.
- There have been cases of unusual cancers in children and teenage patients taking TNF-blocking agents.
- People with inflammatory diseases including rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis, especially those with very active disease, may be more likely to get lymphoma.
- Some people treated with SIMPONI have developed certain kinds of skin cancer. If any changes in the appearance of your skin or growths on your skin occur during or after your treatment with SIMPONI, tell your doctor.
- Some people receiving medicines that are like SIMPONI, called TNF-blockers, developed a rare type of cancer called hepatosplenic T-cell lymphoma. This type of cancer often results in death. Most of these people were male teenagers or young men. Also, most people were being treated for Crohn's disease or ulcerative colitis with a TNF-blocker and another medicine called IMURAN® (azathioprine) or PURINETHOL® (6-mercaptopurine, 6-MP).
What is SIMPONI?
SIMPONI is a prescription medicine called a Tumor Necrosis Factor (TNF) blocker. SIMPONI is used in adults:
- with the medicine methotrexate to treat moderately to severely active rheumatoid arthritis (RA)
- to treat active psoriatic arthritis (PsA) alone or with methotrexate
- to treat active ankylosing spondylitis (AS)
- with moderate to severe active ulcerative colitis (UC) when certain other UC medicines have not worked well enough OR cannot be tolerated, OR if it is necessary to continue taking steroid medicines:
- to begin helping some of your symptoms
- in people who respond to SIMPONI, to get their UC under control (induce remission) and keep UC under control (sustain remission)
- to begin to improve the way the lining of your large intestine looks to your doctor during colonoscopy
You may continue to use other medicines that help treat your condition while taking SIMPONI, such as non-steroidal anti-inflammatory drugs (NSAIDs) and prescription steroids, as recommended by your doctor.
What should I tell my doctor before starting treatment with SIMPONI?
SIMPONI may not be right for you. Before starting SIMPONI, tell your doctor about all your medical conditions, including if you:
- have an infection (see "What is the most important information I should know about SIMPONI?").
- have or have had lymphoma or any other type of cancer.
- have or had heart failure.
- have or have had a condition that affects your nervous system, such as multiple sclerosis or Guillain-Barré syndrome.
- have recently received or are scheduled to receive a vaccine. People taking SIMPONI should not receive live vaccines or treatment with a weakened bacteria (such as BCG for bladder cancer). People taking SIMPONI can receive non-live vaccines.
- have a baby and you were using SIMPONI during your pregnancy. Tell your baby's doctor before your baby receives any vaccine. Your baby may have an increased chance of getting an infection for up to 6 months after birth.
- are allergic to rubber or latex. The needle cover on the prefilled syringe and SmartJect® autoinjector contains dry natural rubber.
- are pregnant or planning to become pregnant. It is not known if SIMPONI will harm your unborn baby.
- are breastfeeding. You and your doctor should decide if you will take SIMPONI or breastfeed. You should not do both without talking to your doctor first.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Especially, tell your doctor if you:
- use ORENCIA (abatacept) or KINERET (anakinra). You should not take SIMPONI while you are also taking ORENCIA (abatacept) or KINERET (anakinra).
- use other TNF-blocker medicines, including REMICADE (infliximab), HUMIRA (adalimumab), ENBREL (etanercept), or CIMZIA (certolizumab pegol).
- receive RITUXAN (rituximab) or ACTEMRA (tocilizumab).
Ask your doctor if you are not sure if your medicine is one listed above.
Keep a list of all your medications with you to show your doctor and pharmacist each time you get a new medicine.
How should I use SIMPONI?
- SIMPONI is given as an injection under the skin (subcutaneous injection).
- If your doctor decides that you or a caregiver may be able to give your injections of SIMPONI at home, you should receive training on the right way to prepare and inject SIMPONI. Do not try to inject SIMPONI yourself until you have been shown the right way to give the injections by your doctor or nurse.
- Use SIMPONI exactly as prescribed by your doctor. Your doctor will tell you how much SIMPONI to inject and when to inject it depending on your medical condition.
- SIMPONI comes in a prefilled syringe or SmartJect autoinjector. Your doctor will prescribe the type that is best for you.
- See the detailed Instructions for Use that comes with your SIMPONI for information about the right way to prepare and give your SIMPONI injections at home.
- Do not miss any doses of SIMPONI. If you forget to use SIMPONI, inject your dose as soon as you remember. Then, take your next dose at your regular scheduled time. In case you are not sure when to inject SIMPONI, call your doctor or pharmacist.
What are the possible side effects with SIMPONI?
SIMPONI can cause serious side effects, including:
See " What is the most important information I should know about SIMPONI? "
Hepatitis B infection in people who carry the virus in their blood.
- If you are a carrier of the hepatitis B virus (a virus that affects the liver), the virus can become active while you use SIMPONI. Your doctor should do blood tests before you start treatment with SIMPONI and while you are using SIMPONI. Tell your doctor if you have any of the following symptoms of a possible hepatitis B infection:
- feel very tired
- dark urine
- skin or eyes look yellow
- little or no appetite
- vomiting
- muscle aches
- clay-colored bowel movements
- fevers
- chills
- stomach discomfort
- skin rash
Heart failure, including new heart failure or worsening of heart failure that you already have. New or worse heart failure can happen in people who use TNF-blocker medicines including SIMPONI.
- If you have heart failure, your condition should be watched closely while you take SIMPONI.
- Call your doctor right away if you get new or worsening symptoms of heart failure while taking SIMPONI (such as shortness of breath or swelling of your lower legs or feet).
Nervous System Problems
Rarely, people using TNF-blocker medicines, including SIMPONI, have nervous system problems such as multiple sclerosis or Guillain-Barré syndrome.
- Tell your doctor right away if you get any of these symptoms:
- vision changes
- weakness in your arms or legs
- numbness or tingling in any part of your body
Liver Problems
Liver problems can happen in people who use TNF-blocker medicines, including SIMPONI. These problems can lead to liver failure and death. Call your doctor right away if you have any of these symptoms:
- feel very tired
- skin or eyes look yellow
- poor appetite or vomiting
- pain on the right side of your stomach (abdomen)
Blood Problems
Low blood counts have been seen with TNF-blockers, including SIMPONI. Your body may not make enough blood cells that help fight infections or help stop bleeding. Symptoms include fever, bruising or bleeding easily, or looking pale. Your doctor will check your blood counts before and during treatment with SIMPONI.
Common side effects with SIMPONI include:
- upper respiratory infection (runny nose, sore throat, and hoarseness or laryngitis)
- reaction at the site of injection (redness, swelling, itching, pain, bruising, or tingling)
- viral infections such as flu and oral cold sores
Other side effects with SIMPONI include:
-
Immune System Problems. Rarely, people using TNF-blocker medicines have developed symptoms that are like the symptoms of Lupus. Tell your doctor if you have any of these symptoms:
- a rash on your cheeks or other parts of the body
- sensitivity to the sun
- new joint or muscle pains
- becoming very tired
- chest pain or shortness of breath
- swelling of the feet, ankles, or legs
- Psoriasis. Some people using SIMPONI had new psoriasis or worsening of psoriasis they already had. Tell your doctor if you develop red scaly patches or raised bumps that are filled with pus. Your doctor may decide to stop your treatment with SIMPONI.
-
Allergic Reactions. Allergic reactions can happen in people who use TNF-blocker medicines including SIMPONI. Some reactions may be serious and can be life-threatening. Some of these reactions can happen after receiving your first dose of SIMPONI. Call your doctor right away if you have any of these symptoms of an allergic reaction:
- hives
- swollen face
- breathing trouble
- chest pain
These are not all of the side effects with SIMPONI. Tell your doctor about any side effect that bothers you or does not go away. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store SIMPONI?
- Refrigerate SIMPONI at 36°F to 46°F (2°C to 8°C).
- Do not freeze SIMPONI.
- Keep SIMPONI in the carton to protect it from light when not being used.
- Do not shake SIMPONI.
Keep SIMPONI and all medicines out of the reach of children.
General Information about SIMPONI
- Medicines are sometimes prescribed for purposes other than those listed in the Medication Guide. Do not use SIMPONI for a condition for which it was not prescribed.
- Do not give SIMPONI to other people, even if they have the same condition that you have. It may harm them.
- This Medication Guide summarizes the most important information about SIMPONI. If you would like more information, talk to your doctor. You can ask your doctor or pharmacist for information about SIMPONI that is written for health professionals. For more information go to www.simponi.com or call 1-800-JANSSEN (1-800-526-7736).
What are the ingredients in SIMPONI?
Active ingredient: golimumab.
Inactive ingredients: L-histidine, L-histidine monohydrochloride monohydrate, sorbitol, polysorbate 80, and water for injection. SIMPONI does not contain preservatives.
This Medication Guide has been approved by the U.S. Food and Drug Administration
Manufactured by:
Janssen Biotech, Inc.
Horsham, PA 19044
US License No. 1864
© Janssen Biotech, Inc. 2013
Revised: 11/2013
INSTRUCTIONS FOR USE
SIMPONI® (SIM-po-nee)
(golimumab)
SmartJect® autoinjector
If your doctor decides that you or a caregiver may be able to give your injections of SIMPONI at home, you should receive training on the right way to prepare and inject SIMPONI.
Do not try to inject SIMPONI yourself until you have been shown the right way to give the injections by your doctor or nurse.
It is important to read, understand, and follow these instructions before using the SIMPONI SmartJect autoinjector so you inject the right way. Call your doctor if you or your caregiver has any questions about the right way to inject SIMPONI.
|
Read this information before you start
|
|
Important things to know about your SmartJect autoinjector
|
| When you are ready to inject SIMPONI, position the autoinjector straight onto your skin (90 degrees), then push firmly. Do not press the button until you have pushed the autoinjector firmly against your skin, allowing the green safety sleeve to slide into the clear cover.
|
|
The green safety sleeve (see Figure A) helps prevent accidental injections. The sleeve must slide into the clear cover before you will be able to press the button. |
|
When the button is pressed you will hear a loud first 'click' sound. Do not lift the autoinjector away from your skin. Hold and wait for the second 'click'. It is very important to practice injecting SIMPONI with your doctor or nurse so you become comfortable with this 'click' sound. |
|
Keep holding the autoinjector firmly against your skin until you hear a second 'click' sound (may take 3-15 seconds), then lift the autoinjector. The injection is complete when you hear the second 'click'. If you lift the autoinjector before hearing the second 'click', you may not get the full dose of medicine. |
Important things to remember
|
| Read all instructions below before using SmartJect autoinjector |
Figure A below shows what the SmartJect autoinjector looks like.
STEP 1. Gather and inspect the supplies for your injection
You will need these supplies for an injection of SIMPONI. See Figure B.
- 1 alcohol swab
- 1 cotton ball or gauze
- 1 SIMPONI prefilled SmartJect autoinjector from the refrigerator (stored at 36°F to 46°F (2°C to 8°C))
- 1 sharps disposal container for throwing away the used SmartJect autoinjector. See Step 4.2 for disposal instructions.
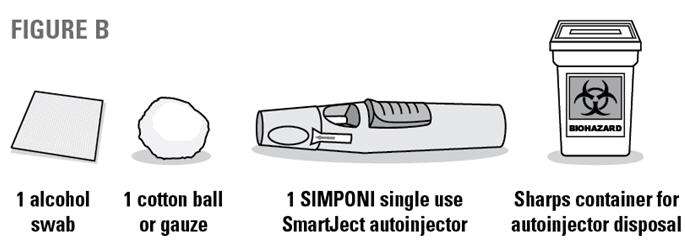
1.1 Check expiration date
- Check the expiration date ("EXP") on the SmartJect autoinjector.
- You can also check the expiration date printed on the back panel of the SIMPONI carton, to the left of the SIMPONI logo.
- If the expiration date has passed, do not use the SmartJect autoinjector. Call your doctor or pharmacist, or call 1-800-JANSSEN (1-800-526-7736) for help.
1.2 Check security seal
- Check the security seal around the cap of the SmartJect autoinjector. If the security seal is broken, do not use the SmartJect autoinjector.
1.3 Wait 30 minutes
|

|
|
|
1.4 Check the liquid in the SmartJect autoinjector
|
|
STEP 2. Choose and prepare the injection site
2.1 Choose the injection site
- The recommended injection site is the front of your middle thighs. See Figure D.
- You can also use the lower part of the abdomen below the navel (belly button), except for the two-inch area directly around the navel. See Figure E.
- If a caregiver is giving you the injection, the outer area of the upper arms may also be used. See Figure E.

- If more than one injection is needed for a dose of SIMPONI, each injection should be given at different sites on the body.
- Choose a different injection site each time you give your injection. See Figures D and E.
- Do not inject into areas where the skin is tender, bruised, red, scaly, or hard. Avoid areas with scars or stretch marks.
2.2 Prepare the injection site
- Wash your hands well with soap and warm water.
- Wipe the injection site with an alcohol swab.
- Do not touch this area again before giving the injection. Allow the skin to dry before injecting.
- Do not fan or blow on the clean area.
STEP 3. Inject SIMPONI using the single dose SmartJect autoinjector
3.1 Remove cap
- Do not remove the cap until you are ready to inject SIMPONI. Inject SIMPONI within 5 minutes after the cap has been removed.
- When you are ready to inject, twist the cap slightly to break the security seal. See Figure F.
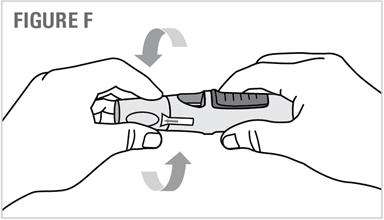
- Pull the cap off and throw it in the trash right away. See Figure G.
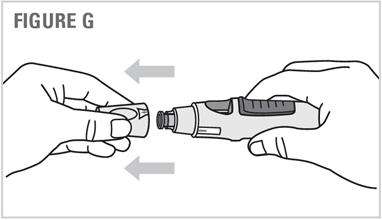
- Do not put the cap back on because it may damage the needle inside the SmartJect autoinjector.
- Do not use your SmartJect autoinjector if it is dropped without the cap in place.
3.2 Push autoinjector firmly against skin
|
|
3.3 Press button to inject. Hold and wait!
|
3.4 Wait for second 'click' (3-15 seconds)
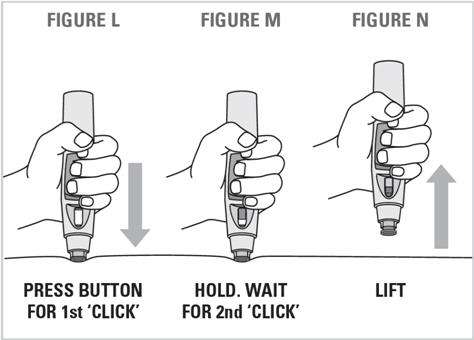
|
|
- Lift the SmartJect autoinjector from the injection site. See Figure N.
- If you have a problem hearing the 'clicks', count for 15 seconds from the time you pressed the button and then lift the SmartJect autoinjector from the injection site.
STEP 4. After the injection
4.1 Check the viewing window
|
|
4.2 Dispose of the used SmartJect autoinjector
|
|
|
|
4.3 Use cotton ball or gauze
- There may be a small amount of blood or liquid at the injection site, which is normal.
- You can press a cotton ball or gauze over the injection site for 10 seconds.
Do not rub the injection site. - You may cover the injection site with a small adhesive bandage, if needed.
| Need more help with your injection? | |
| Quick Reminders |
If you're having difficulty injecting:
|
| Do not press the button until you are ready to inject SIMPONI. | |
| Position the autoinjector straight onto your skin (90 degrees), then push firmly. | |
| Press the raised part of the button to start the injection and listen for the first 'click'. Do not lift the SmartJect autoinjector away from your skin yet. | |
| Keep holding the autoinjector firmly against your skin until you hear the second 'click', or you can count to 15 after pressing the button. | |
| Lift and check the viewing window to confirm that you see the yellow indicator. | |
| For additional questions or assistance, or to share your feedback, call 1-800-JANSSEN (1-800-526-7736). | |
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Janssen Biotech, Inc.
Horsham, PA 19044
US License No. 1864
Revised: 01/2014
Patient Instructions for Use
SIMPONI® (SIM-po-nee)
(golimumab)
Prefilled Syringe
If your doctor decides that you or a caregiver may be able to give your injections of SIMPONI at home, you should receive training on the right way to prepare and inject SIMPONI. Do not try to inject SIMPONI yourself until you have been shown the right way to give the injections by your doctor or nurse.
It is important to read, understand, and follow these instructions so that you inject SIMPONI the right way. Call your doctor if you or your caregiver has any questions about the right way to inject SIMPONI.
Important information about your prefilled syringe:
- Always hold the prefilled syringe by the body of the syringe (see Figure B).
Do not:
- pull back on the plunger at any time.
- shake the SIMPONI prefilled syringe. This may damage the medicine.
- remove the needle cover from the prefilled syringe until you get to that step.
- touch the needle guard activation clips to prevent covering the needle with the needle guard too soon (See Figure B).
- use SIMPONI if it has been frozen or if it has not been stored in the refrigerator. See the Medication Guide section: "how should I store SIMPONI?"
- use your SIMPONI prefilled syringe if it looks damaged.
Step 1: Gather and inspect the supplies for your injection
You will need these supplies for an injection of SIMPONI. See Figure A.
- 1 alcohol swab
- 1 cotton ball or gauze
- 1 SIMPONI prefilled syringe from the refrigerator (stored at 36°F to 46°F (2°C to 8°C))
- 1 sharps disposal container for throwing away the used prefilled syringe. See " 5.1 Disposal of the used prefilled syringe " at the end of these instructions.
| Figure A |
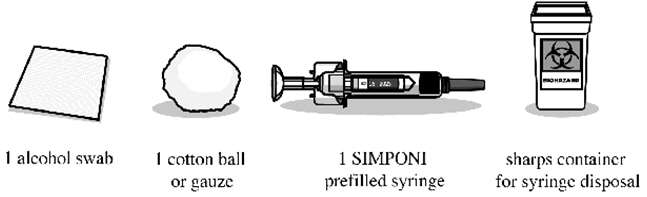
|
The figure below shows what the prefilled syringe looks like. See Figure B.
| Figure B |
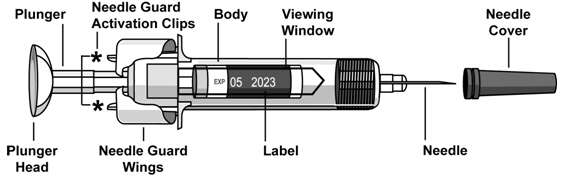
|
Step 2: Get ready to use your prefilled syringe
2.1 Check Expiration Date
- Look for the expiration date printed on the back panel of the SIMPONI carton, to the left of the SIMPONI logo.
- If the expiration date has passed, do not use the prefilled syringe. Call your doctor or pharmacist, or call 1-800-JANSSEN (1-800-526-7736) for help.
2.2 Wait 30 minutes
|

|
2.3 Check the Liquid in the Prefilled Syringe
- Hold your SIMPONI prefilled syringe by the body with the covered needle pointing down. See Figure C.
| Figure C |

|
- Look at the liquid through the viewing window of the prefilled syringe. See Figure C. Make sure that the liquid in the prefilled syringe is clear and colorless to slightly yellow in color. You may see a small amount of tiny particles that are white, or that you can see through. Do not inject the liquid if it is cloudy or discolored, or has large particles in it.
- You may also notice an air bubble. This is normal.
Step 3: Choose and prepare the injection site
3.1 Choose the Injection Site
- The recommended injection site is the front of your middle thighs. See Figure D.
| Figure D |

|
- You can also use the lower part of the abdomen below the navel (belly button), except for the two-inch area directly around the navel. See Figure E.
- If a caregiver is giving you the injection, the outer area of the upper arms may also be used. See Figure E.
- If more than one injection is needed for a dose of SIMPONI, each injection should be given at different sites on the body.
| Figure E |
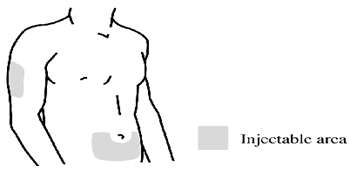
|
- Do not inject into areas where the skin is tender, bruised, red, scaly, or hard. Avoid areas with scars or stretch marks.
3.2 Prepare the Injection Site
- Wash your hands well with soap and warm water.
- Wipe the injection site with an alcohol swab.
- Do not touch this area again before giving the injection. Let your skin dry before injecting.
- Do not fan or blow on the clean area.
Step 4: Inject SIMPONI using the Prefilled Syringe
4.1 Remove the Needle Cover
- Do not remove the needle cover until you are ready to inject SIMPONI. Inject SIMPONI within 5 minutes after you remove the needle cover.
- Do not touch the plunger while removing the needle cover.
- When you are ready to inject, hold the body of the prefilled syringe with one hand, and pull the needle cover straight off. See Figure F.
| Figure F |

|
- Put the needle cover in the trash.
- You may see an air bubble in the prefilled syringe. This is normal.
- You may also see a drop of liquid at the end of the needle. This is normal.
- Do not touch the needle or let it touch any surface.
- Do not use the prefilled syringe if it is dropped without the needle cover in place.
4.2 Position the prefilled syringe and inject SIMPONI
- Hold the body of the prefilled syringe in one hand between the thumb and index fingers. See Figure G.
| Figure G |

|
- Do not pull back on the plunger at any time.
- Use the other hand to gently pinch the area of skin that you previously cleaned. Hold firmly.
- Use a quick, dart-like motion to insert the needle into the pinched skin at about a 45-degree angle. See Figure H.
| Figure H |
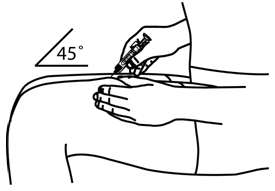
|
- Inject all of the medicine by using your thumb to push in the plunger until the plunger head is completely between the needle guard wings. See Figure I.
| Figure I |
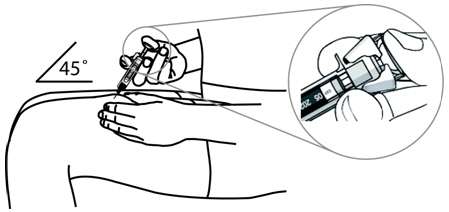
|
- When the plunger is pushed as far as it will go, keep pressure on the plunger head. Take the needle out of the skin and let go of the skin.
- Slowly take your thumb off the plunger head. This will let the empty syringe move up until the entire needle is covered by the needle guard. See Figure J.
| Figure J |
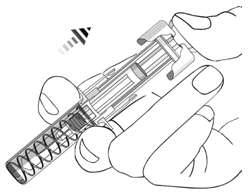
|
Step 5: After the injection
5.1 Disposal of the used prefilled syringe
- Put your used prefilled syringe in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) the prefilled syringe in your household trash. See Figure K.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
| Figure K |

|
5.2 Use Cotton Ball or Gauze
- There may be a small amount of blood or liquid at the injection site, which is normal.
- You can press a cotton ball or gauze over the injection site and hold for 10 seconds. Do not rub the injection site.
- You may cover the injection site with a small adhesive bandage, if needed.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Janssen Biotech, Inc.
Horsham, PA 19044
US License No. 1864
Revised: 05/2013
PRINCIPAL DISPLAY PANEL - 50 mg/0.5 mL Syringe Carton
NDC 57894-070-01
FOR SUBCUTANEOUS INJECTION
Sterile solution in a single dose
prefilled syringe. Discard unused portion.
See package insert for dosing information.
No U.S. standard of potency.
This Product Contains
Dry Natural Rubber.
Rx only.
Simponi®
golimumab
50 mg / 0.5 mL
One single dose prefilled syringe
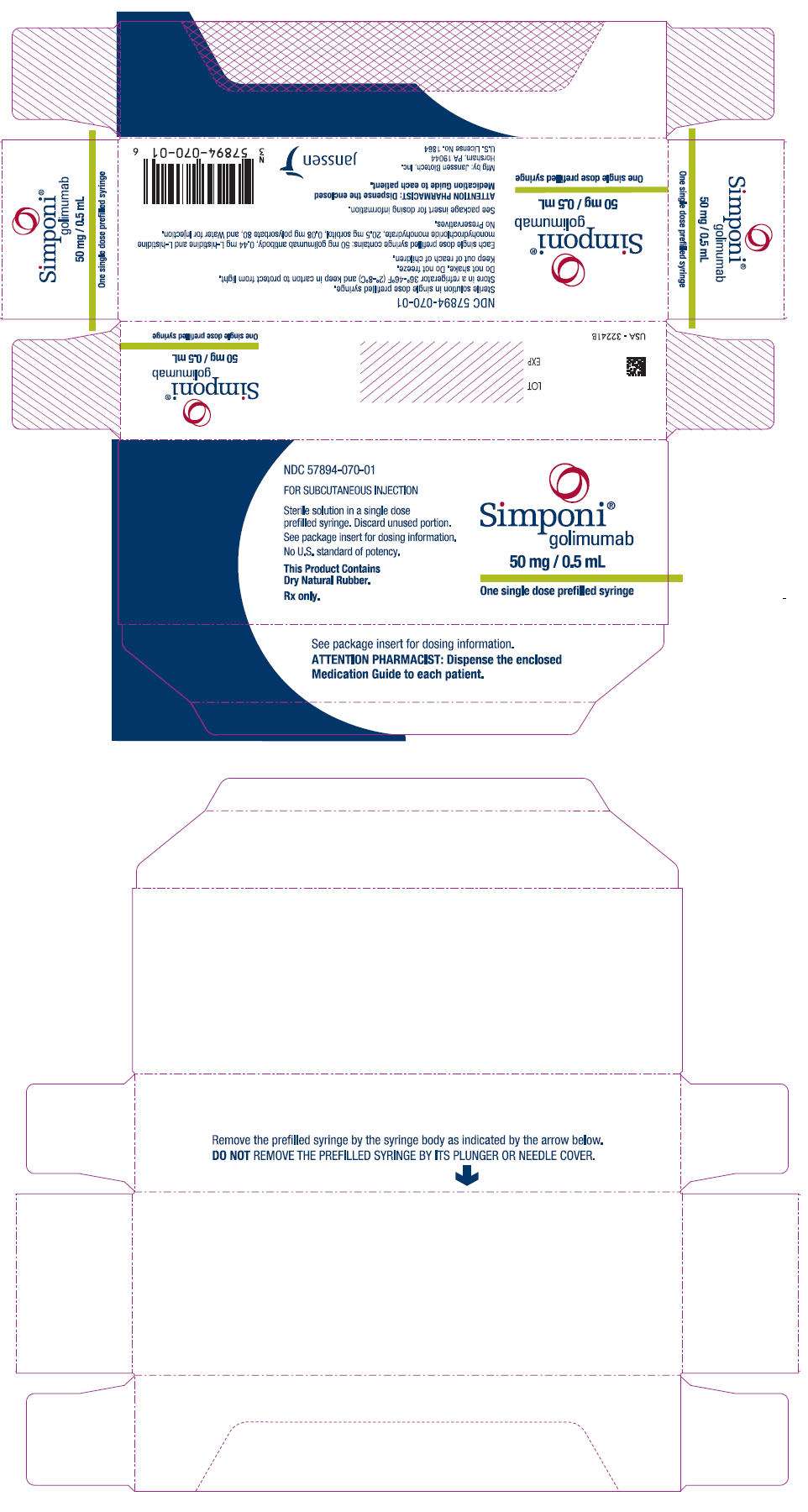
PRINCIPAL DISPLAY PANEL - 100 mg/mL Syringe Carton
NDC 57894-071-01
FOR SUBCUTANEOUS INJECTION
Sterile solution in a single dose
prefilled syringe. Discard unused portion.
See package insert for dosing information.
No U.S. standard of potency.
This Product Contains
Dry Natural Rubber.
Rx only.
Simponi®
golimumab
100 mg/mL
One single dose prefilled syringe
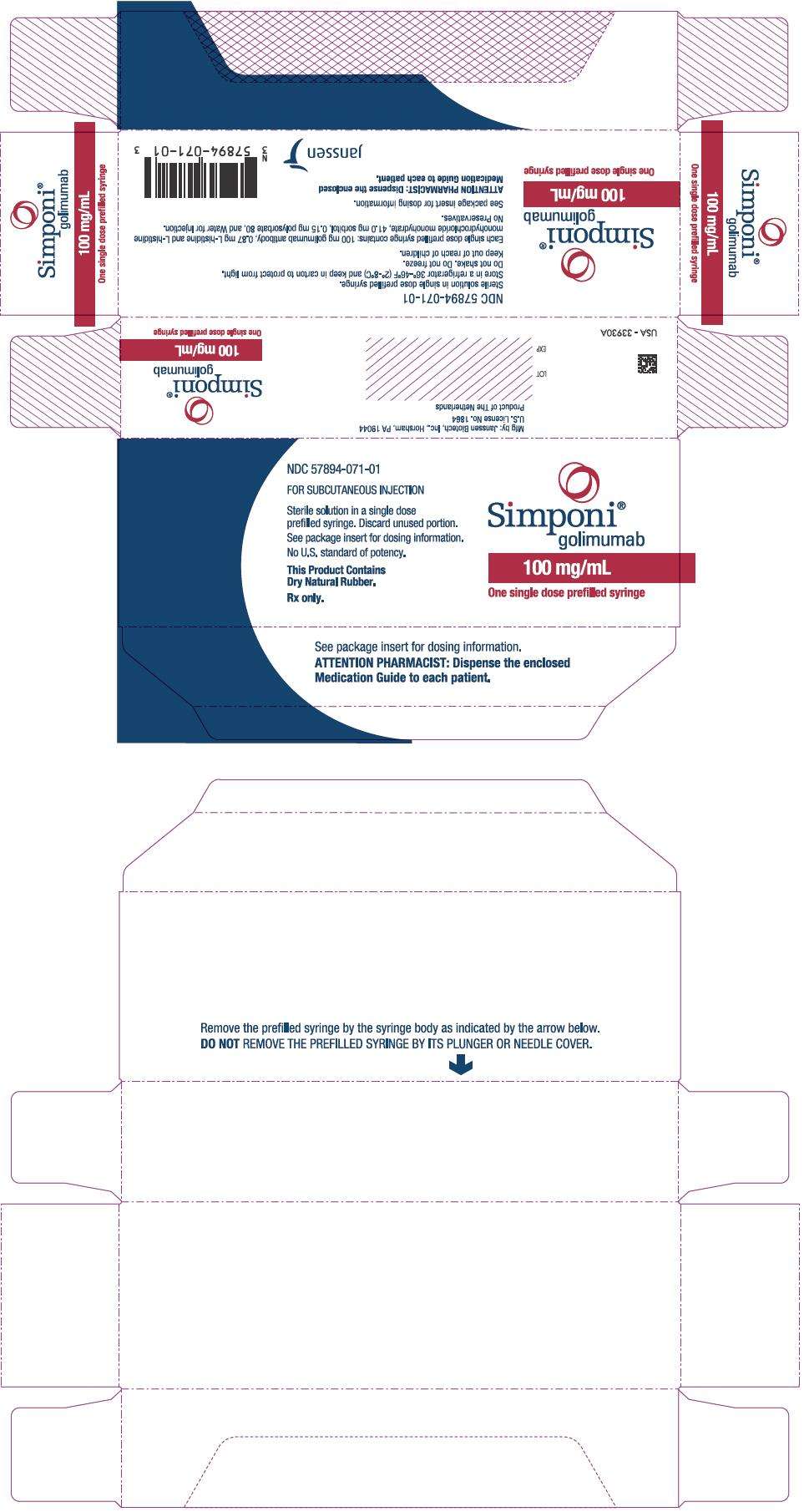
Simponigolimumab INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Simponigolimumab INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||