Levofloxacin
Lake Erie Medical DBA Quality Care Products LLC
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use levofloxacin safely and effectively. See full prescribing information for levofloxacin tablets. Levofloxacin Tablet, Film Coated for Oral useInitial U.S. Approval: 1996MicrobiologyBOXED WARNINGWARNING See full prescribing information for complete boxed warning. Fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture in all ages. This risk is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants [see Warnings and Precautions (5.1)]. Fluoroquinolones, including levofloxacin, may exacerbate muscle weakness in persons with myasthenia gravis. Avoid levofloxacin in patients with a known history of myasthenia gravis [see Warnings and Precautions (5.2)]. INDICATIONS AND USAGE(112.4) Pneumonia: nosocomial (1.1) and community acquired (1.2, 1.3) Acute bacterial sinusitis (1.4) Acute bacterial exacerbation of chronic bronchitis (1.5) Skin and skin structure infections: complicated (1.6) and uncomplicated (1.7) Chronic bacterial prostatitis (1.8) Urinary tract infections: complicated (1.9, 1.10) and uncomplicated (1.12) Acute pyelonephritis (1.11) Inhalational anthrax, post-exposure (1.13) Plague (1.14) DOSAGE AND ADMINISTRATION Dosage in patients with normal renal function (2.1) Type of Infection Dose Every24 hours Duration (days) Nosocomial Pneumonia (1.1) 750 mg 7 to 14 Community Acquired Pneumonia (1.2) 500 mg 7 to 14 Community Acquired Pneumonia (1.3) 750 mg 5 Acute Bacterial Sinusitis (1.4) 750 mg 5 500 mg 10 to 14 Acute Bacterial Exacerbation of Chronic Bronchitis (1.5) 500 mg 7 Complicated Skin and Skin Structure Infections (SSSI) (1.6) 750 mg 7 to 14 Uncomplicated SSSI (1.7) 500 mg 7 to 10 Chronic Bacterial Prostatitis (1.8) 500 mg 28 Complicated Urinary Tract Infection (1.9) or Acute Pyelonephritis (1.11) 750 mg 5 Complicated Urinary Tract Infection (1.10) or Acute Pyelonephritis (1.11) 250 mg 10 Uncomplicated Urinary Tract Infection (1.12) 250 mg 3 Inhalational Anthrax (Post-Exposure) (1.13) Adults and Pediatric Patients > 50 kg Pediatric Patients < 50 kg and ≥ 6 months of age 500 mg8 mg/kg BID (not to exceed250 mg/dose) 6060 Plague (1.14) Adults and Pediatric Patients >50 kg Pediatric Patients
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING
- 1 LEVOFLOXACIN INDICATIONS AND USAGE
- 1.1 Nosocomial Pneumonia
- 1.2 Community-Acquired Pneumonia: 7 to 14 day Treatment Regimen
- 1.3 Community-Acquired Pneumonia: 5-day Treatment Regimen
- 1.4 Acute Bacterial Sinusitis: 5-day and 10 to 14 day Treatment Regimens
- 1.5 Acute Bacterial Exacerbation of Chronic Bronchitis
- 1.6 Complicated Skin and Skin Structure Infections
- 1.7 Uncomplicated Skin and Skin Structure Infections
- 1.8 Chronic Bacterial Prostatitis
- 1.9 Complicated Urinary Tract Infections: 5-day Treatment Regimen
- 1.10 Complicated Urinary Tract Infections: 10-day Treatment Regimen
- 1.11 Acute Pyelonephritis: 5 or 10-day Treatment Regimen
- 1.12 Uncomplicated Urinary Tract Infections
- 1.13 Inhalational Anthrax (Post-Exposure)
- 1.14 Plague
- 2 LEVOFLOXACIN DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 LEVOFLOXACIN CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Tendinopathy and Tendon Rupture
- 5.2 Exacerbation of Myasthenia Gravis
- 5.3 Hypersensitivity Reactions
- 5.4 Other Serious and Sometimes Fatal Reactions
- 5.5 Hepatotoxicity
- 5.6 Central Nervous System Effects
- 5.7 Clostridium difficile-Associated Diarrhea
- 5.8 Peripheral Neuropathy
- 5.9 Prolongation of the QT Interval
- 5.10 Musculoskeletal Disorders in Pediatric Patients and Arthropathic Effects in Animals
- 5.11 Blood Glucose Disturbances
- 5.12 Photosensitivity/Phototoxicity
- 5.13 Development of Drug Resistant Bacteria
- 6 LEVOFLOXACIN ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 LEVOFLOXACIN DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 14.1 Nosocomial Pneumonia
- 14.2 Community-Acquired Pneumonia: 7 to 14 day Treatment Regimen
- 14.3 Community-Acquired Pneumonia: 5-day Treatment Regimen
- 14.4 Acute Bacterial Sinusitis: 5-day and 10 to 14 day Treatment Regimens
- 14.5 Complicated Skin and Skin Structure Infections
- 14.6 Chronic Bacterial Prostatitis
- 14.7 Complicated Urinary Tract Infections and Acute Pyelonephritis: 5-day Treatment Regimen
- 14.8 Complicated Urinary Tract Infections and Acute Pyelonephritis: 10-day Treatment Regimen
- 14.9 Inhalational Anthrax (Post-Exposure)
- 14.10 Plague
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- 17.6 FDA-Approved Medication Guide
- Image of Label
FULL PRESCRIBING INFORMATION
WARNING
Fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture in all ages. This risk is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants [see Warnings and Precautions (5.1)].
Fluoroquinolones, including levofloxacin, may exacerbate muscle weakness in persons with myasthenia gravis. Avoid levofloxacin in patients with a known history of myasthenia gravis [see Warnings and Precautions (5.2)].
1 INDICATIONS AND USAGE
Culture and susceptibility testing
[see Clinical Pharmacology (12.4)]
Pseudomonas aeruginosa
1.1 Nosocomial Pneumonia
Staphylococcus aureus, Pseudomonas aeruginosa, Serratia marcescens, Escherichia coli, Klebsiella pneumoniae, Haemophilus influenzae,Streptococcus pneumoniaePseudomonas aeruginosa[see Clinical Studies (14.1)]
1.2 Community-Acquired Pneumonia: 7 to 14 day Treatment Regimen
Staphylococcus aureus, Streptococcus pneumoniaeStreptococcus pneumoniaeHaemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Moraxella catarrhalis, Chlamydophila pneumoniae, Legionella pneumophila, Mycoplasma pneumoniae [see Dosage and Administration (2.1) and Clinical Studies (14.2)]
nd
1.3 Community-Acquired Pneumonia: 5-day Treatment Regimen
Levofloxacin tablets are indicated for the treatment of community-acquired pneumonia due to Streptococcus pneumoniae (excluding multi-drug-resistant isolates [MDRSP]), Haemophilus influenzae, Haemophilus parainfluenzae, Mycoplasma pneumoniae, or Chlamydophila pneumoniae [see Dosage and Administration (2.1) and Clinical Studies (14.3)].
1.4 Acute Bacterial Sinusitis: 5-day and 10 to 14 day Treatment Regimens
Levofloxacin tablets are indicated for the treatment of acute bacterial sinusitis due to Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis [see Clinical Studies (14.4)].
1.5 Acute Bacterial Exacerbation of Chronic Bronchitis
Levofloxacin tablets are indicated for the treatment of acute bacterial exacerbation of chronic bronchitis due to methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Haemophilus parainfluenzae, or Moraxella catarrhalis.
1.6 Complicated Skin and Skin Structure Infections
Levofloxacin tablets are indicated for the treatment of complicated skin and skin structure infections due to methicillin-susceptible Staphylococcus aureus, Enterococcus faecalis, Streptococcus pyogenes, or Proteus mirabilis [see Clinical Studies (14.5)].
1.7 Uncomplicated Skin and Skin Structure Infections
Staphylococcus aureusStreptococcus pyogenes
1.8 Chronic Bacterial Prostatitis
Escherichia coli, Enterococcus faecalis, Staphylococcus epidermidis [see Clinical Studies (14.6)].
1.9 Complicated Urinary Tract Infections: 5-day Treatment Regimen
Levofloxacin tablets are indicated for the treatment of complicated urinary tract infections due to Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis [see Clinical Studies (14.7)].
1.10 Complicated Urinary Tract Infections: 10-day Treatment Regimen
Enterococcus faecalisEnterobacter cloacae, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis,Pseudomonas aeruginosa [see Clinical Studies (14.8)]
1.11 Acute Pyelonephritis: 5 or 10-day Treatment Regimen
Levofloxacin tablets are indicated for the treatment of acute pyelonephritis caused by Escherichia coli, including cases with concurrent bacteremia [see Clinical Studies (14.7, 14.8)].
1.12 Uncomplicated Urinary Tract Infections
Levofloxacin tablets are indicated for the treatment of uncomplicated urinary tract infections (mild to moderate) due to Escherichia coli, Klebsiella pneumoniae, or Staphylococcus saprophyticus.
1.13 Inhalational Anthrax (Post-Exposure)
Levofloxacin tablets are indicated for inhalational anthrax (post-exposure) to reduce the incidence or progression of disease following exposure to aerosolized Bacillus anthracis. The effectiveness of levofloxacin tablets is based on plasma concentrations achieved in humans, a surrogate endpoint reasonably likely to predict clinical benefit. Levofloxacin tablets have not been tested in humans for the post-exposure prevention of inhalation anthrax. The safety of levofloxacin tablets in adults for durations of therapy beyond 28 days or in pediatric patients for durations of therapy beyond 14 days has not been studied. Prolonged levofloxacin tablets therapy should only be used when the benefit outweighs the risk [see Dosage and Administration (2.1, 2.2) and Clinical Studies (14.9)].
1.14 Plague
areYersinia pestis Y. pestisand[see Dosage and Administration (2.1, 2.2) and Clinical Studies (14.10)]
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Adult Patients with Normal Renal Function
[see Dosage and Administration (2.3)]
| Type of Infection1 | Dosed Every 24 hours | Duration (days)2 |
|---|---|---|
|
1 Due to the designated pathogens [see Indications and Usage (1)]. 2 Sequential therapy (intravenous to oral) may be instituted at the discretion of the physician. 3 Due to methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae (including multi-drug-resistant isolates [MDRSP]), Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Moraxella catarrhalis, Chlamydophila pneumoniae, Legionella pneumophila, or Mycoplasma pneumoniae [see Indications and Usage (1.2)]. 4 Due to Streptococcus pneumoniae (excluding multi-drug-resistant isolates [MDRSP]), Haemophilus influenzae, Haemophilus parainfluenzae, Mycoplasma pneumoniae, or Chlamydophila pneumoniae [see Indications and Usage (1.3)]. 5 This regimen is indicated for cUTI due to Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis and AP due to E. coli, including cases with concurrent bacteremia. 6 This regimen is indicated for cUTI due to Enterococcus faecalis, Enterococcus cloacae, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa; and for AP due to E. coli. 7 Drug administration should begin as soon as possible after suspected or confirmed exposure to aerosolized B. anthracis. This indication is based on a surrogate endpoint. Levofloxacin plasma concentrations achieved in humans are reasonably likely to predict clinical benefit [see Clinical Studies (14.9)]. 8 The safety of levofloxacin tablets in adults for durations of therapy beyond 28 days or in pediatric patients for durations beyond 14 days has not been studied. An increased incidence of musculoskeletal adverse events compared to controls has been observed in pediatric patients [see Warnings and Precautions (5.10), Use in Specific Populations (8.4), and Clinical Studies (14.9)]. Prolonged levofloxacin tablets therapy should only be used when the benefit outweighs the risk. 9 Drug administration should begin as soon as possible after suspected or confirmed exposure to Yersinia pestis. Higher doses of levofloxacin tablets typically used for treatment of pneumonia can be used for treatment of plague, if clinically indicated. |
||
| Nosocomial Pneumonia |
750 mg |
7 to 14 |
| Community Acquired Pneumonia3
|
500 mg |
7 to 14 |
| Community Acquired Pneumonia4
|
750 mg |
5 |
| Acute Bacterial Sinusitis |
750 mg |
5 |
| 500 mg |
10 to 14 |
|
| Acute Bacterial Exacerbation of Chronic Bronchitis |
500 mg |
7 |
| Complicated Skin and Skin Structure Infections (SSSI) |
750 mg |
7 to 14 |
| Uncomplicated SSSI |
500 mg |
7 to 10 |
| Chronic Bacterial Prostatitis |
500 mg |
28 |
| Complicated Urinary Tract Infection (cUTI) or Acute Pyelonephritis (AP)5
|
750 mg |
5 |
| Complicated Urinary Tract Infection (cUTI) or Acute Pyelonephritis (AP)6
|
250 mg |
10 |
| Uncomplicated Urinary Tract Infection |
250 mg |
3 |
| Inhalational Anthrax (Post-Exposure), adult and pediatric patients > 50 kg7,8
Pediatric patients < 50 kg and ≥ 6 months of age 7,8 |
500 mg see Table 2 below (2.2) |
608
608 |
| Plague, adult
and
pediatric patients > 50 kg9
Pediatric patients < 50 kg and ≥ 6 months of age |
500 mg see Table 2 below (2.2) |
10 to 14 10 to 14 |
2.2 Dosage in Pediatric Patients
| Type of Infection1 | Dose | Freq. Once every |
Duration2 |
|---|---|---|---|
|
1 Due to Bacillus anthracis [see Indications and Usage (1.13)] and Yersinia pestis [see Indications and Usage (1.14)].
2 Sequential therapy (intravenous to oral) may be instituted at the discretion of the physician. 3 Drug administration should begin as soon as possible after suspected or confirmed exposure to aerosolized B. anthracis. This indication is based on a surrogate endpoint. Levofloxacin plasma concentrations achieved in humans are reasonably likely to predict clinical benefit [see Clinical Studies (14.9)]. 4 The safety of levofloxacin tablets in pediatric patients for durations of therapy beyond 14 days has not been studied. An increased incidence of musculoskeletal adverse events compared to controls has been observed in pediatric patients [see Warnings and Precautions (5.10), Use in Specific Populations (8.4), and Clinical Studies (14.9)]. Prolonged levofloxacin tablets therapy should only be used when the benefit outweighs the risk. 5 Drug administration should begin as soon as possible after suspected or confirmed exposure to Yersinia pestis. |
|||
| Inhalational Anthrax (post-exposure)3, 4
|
|||
| Pediatric patients > 50 kg |
500 mg |
24 hr |
60 days4
|
| Pediatric patients < 50 kg and ≥ 6 months of age |
8 mg/kg (not to exceed 250 mg per dose) |
12 hr |
60 days4
|
|
Plague
5
|
|||
| Pediatric patients > 50
kg
|
500 mg |
24 hr |
10 to 14 days |
| Pediatric patients < 50 kg and ≥ 6 months of age |
8 mg/kg (not to exceed 250 mg per dose) |
12 hr |
10 to 14 days |
2.3 Dosage Adjustment in Adults with Renal Impairment
[see Use in Specific Populations (8.6)]
| Dosage in Normal Renal Function Every 24 hours |
Creatinine Clearance 20 to 49 mL/min |
Creatinine Clearance 10 to 19 mL/min |
Hemodialysis or Chronic Ambulatory Peritoneal Dialysis (CAPD) |
|---|---|---|---|
| 750 mg |
750 mg every 48 hours |
750 mg initial dose, then 500 mg every 48 hours |
750 mg initial dose, then 500 mg every 48 hours |
| 500 mg |
500 mg initial dose, then 250 mg every 24 hours |
500 mg initial dose, then 250 mg every 48 hours |
500 mg initial dose, then 250 mg every 48 hours |
| 250 mg |
No dosage adjustment required |
250 mg every 48 hours. If treating uncomplicated UTI, then no dosage adjustment is required |
No information on dosing adjustment is available |
2.4 Drug Interaction With Chelation Agents: Antacids, Sucralfate, Metal Cations, Multivitamins
Levofloxacin tablets should be administered at least two hours before or two hours after antacids containing magnesium, aluminum, as well as sucralfate, metal cations such as iron, and multivitamin preparations with zinc or didanosine chewable/buffered tablets or the pediatric powder for oral solution [see Drug Interactions (7.1) and Patient Counseling Information (17.2)].
2.5 Administration Instructions
Food and Levofloxacin Tablets
Hydration for Patients Receiving Levofloxacin Tablets
[see Adverse Reactions (6.1) and Patient Counseling Information (17.2)].
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
Levofloxacin tablets are contraindicated in persons with known hypersensitivity to levofloxacin, or other quinolone antibacterials [see Warnings and Precautions (5.3)].
5 WARNINGS AND PRECAUTIONS
5.1 Tendinopathy and Tendon Rupture
Fluoroquinolones, including levofloxacin, are associated with an increased risk of tendinitis and tendon rupture in all ages. This adverse reaction most frequently involves the Achilles tendon, and rupture of the Achilles tendon may require surgical repair. Tendinitis and tendon rupture in the rotator cuff (the shoulder), the hand, the biceps, the thumb, and other tendon sites have also been reported. The risk of developing fluoroquinolone-associated tendinitis and tendon rupture is further increased in older patients usually over 60 years of age, in those taking corticosteroid drugs, and in patients with kidney, heart or lung transplants. Factors, in addition to age and corticosteroid use, that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis. Tendinitis and tendon rupture have been reported in patients taking fluoroquinolones who do not have the above risk factors. Tendon rupture can occur during or after completion of therapy; cases occurring up to several months after completion of therapy have been reported. Levofloxacin should be discontinued if the patient experiences pain, swelling, inflammation or rupture of a tendon. Patients should be advised to rest at the first sign of tendinitis or tendon rupture, and to contact their healthcare provider regarding changing to a non-quinolone antimicrobial drug [see Adverse Reactions (6.3); Patient Counseling Information (17.3)].
5.2 Exacerbation of Myasthenia Gravis
[see Adverse Reactions (6.3); Patient Counseling Information (17.3)]
5.3 Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity and/or anaphylactic reactions have been reported in patients receiving therapy with fluoroquinolones, including levofloxacin. These reactions often occur following the first dose. Some reactions have been accompanied by cardiovascular collapse, hypotension/shock, seizure, loss of consciousness, tingling, angioedema (including tongue, laryngeal, throat, or facial edema/swelling), airway obstruction (including bronchospasm, shortness of breath, and acute respiratory distress), dyspnea, urticaria, itching, and other serious skin reactions. Levofloxacin should be discontinued immediately at the first appearance of a skin rash or any other sign of hypersensitivity. Serious acute hypersensitivity reactions may require treatment with epinephrine and other resuscitative measures, including oxygen, intravenous fluids, antihistamines, corticosteroids, pressor amines, and airway management, as clinically indicated [see Adverse Reactions (6); Patient Counseling Information (17.3)].
5.4 Other Serious and Sometimes Fatal Reactions
- fever, rash, or severe dermatologic reactions (e.g., toxic epidermal necrolysis, Stevens-Johnson Syndrome);
- vasculitis; arthralgia; myalgia; serum sickness;
- allergic pneumonitis;
- interstitial nephritis; acute renal insufficiency or failure;
- hepatitis; jaundice; acute hepatic necrosis or failure;
- anemia, including hemolytic and aplastic; thrombocytopenia, including thrombotic thrombocytopenic purpura; leukopenia; agranulocytosis; pancytopenia; and/or other hematologic abnormalities.
The drug should be discontinued immediately at the first appearance of skin rash, jaundice, or any other sign of hypersensitivity and supportive measures instituted [see Adverse Reactions (6); Patient Counseling Information (17.3)].
5.5 Hepatotoxicity
Postmarketing reports of severe hepatotoxicity (including acute hepatitis and fatal events) have been received for patients treated with levofloxacin. No evidence of serious drug-associated hepatotoxicity was detected in clinical trials of over 7,000 patients. Severe hepatotoxicity generally occurred within 14 days of initiation of therapy and most cases occurred within 6 days. Most cases of severe hepatotoxicity were not associated with hypersensitivity [see Warnings and Precautions (5.4)]. The majority of fatal hepatotoxicity reports occurred in patients 65 years of age or older and most were not associated with hypersensitivity. Levofloxacin should be discontinued immediately if the patient develops signs and symptoms of hepatitis [see Adverse Reactions (6); Patient Counseling Information (17.3)].
5.6 Central Nervous System Effects
toxic[see Adverse Reactions (6) Drug Interactions (7.4, 7.5) Patient Counseling Information (17.3)]
5.7 Clostridium difficile-Associated Diarrhea
Clostridium difficileC. difficile
C. difficile C. difficile
C. difficile C. difficile,[see Adverse Reactions (6.2), Patient Counseling Information (17.3)].
5.8 Peripheral Neuropathy
Rare cases of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias and weakness have been reported in patients receiving fluoroquinolones, including levofloxacin. Levofloxacin should be discontinued if the patient experiences symptoms of neuropathy including pain, burning, tingling, numbness, and/or weakness or other alterations of sensation including light touch, pain, temperature, position sense, and vibratory sensation in order to prevent the development of an irreversible condition [see Adverse Reactions (6), Patient Counseling Information (17.3)].
5.9 Prolongation of the QT Interval
Some fluoroquinolones, including levofloxacin, have been associated with prolongation of the QT interval on the electrocardiogram and infrequent cases of arrhythmia. Rare cases of torsade de pointes have been spontaneously reported during postmarketing surveillance in patients receiving fluoroquinolones, including levofloxacin. Levofloxacin should be avoided in patients with known prolongation of the QT interval, patients with uncorrected hypokalemia, and patients receiving Class IA (quinidine, procainamide), or Class III (amiodarone, sotalol) antiarrhythmic agents. Elderly patients may be more susceptible to drug-associated effects on the QT interval [see Adverse Reactions (6.3), Use in Specific Populations (8.5), and Patient Counseling Information (17.3)].
5.10 Musculoskeletal Disorders in Pediatric Patients and Arthropathic Effects in Animals
in [see Indications and Usage (1.13, 1.14)] [see Use in Specific Populations (8.4)]
[see Animal Toxicology and/or Pharmacology (13.2)]
5.11 Blood Glucose Disturbances
As with other fluoroquinolones, disturbances of blood glucose, including symptomatic hyper- and hypoglycemia, have been reported with levofloxacin, usually in diabetic patients receiving concomitant treatment with an oral hypoglycemic agent (e.g., glyburide) or with insulin. In these patients, careful monitoring of blood glucose is recommended. If a hypoglycemic reaction occurs in a patient being treated with levofloxacin, levofloxacin should be discontinued and appropriate therapy should be initiated immediately [see Adverse Reactions (6.2); Drug Interactions (7.3); Patient Counseling Information (17.4)].
5.12 Photosensitivity/Phototoxicity
[see Adverse Reactions (6.3); Patient Counseling Information (17.3)].
5.13 Development of Drug Resistant Bacteria
[see Patient Counseling Information (17.1)].
6 ADVERSE REACTIONS
6.1 Serious and Otherwise Important Side Effects
- Tendon Effects [see Warnings and Precautions (5.1)]
- Exacerbation of Myasthenia Gravis [see Warnings and Precautions (5.2)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Other Serious and Sometimes Fatal Reactions [see Warnings and Precautions (5.4)]
- Hepatotoxicity [see Warnings and Precautions (5.5)]
- Central Nervous System Effects [see Warnings and Precautions (5.6)]
- Clostridium difficile-Associated Diarrhea [see Warnings and Precautions (5.7)]
- Peripheral Neuropathy [see Warnings and Precautions (5.8)]
- Prolongation of the QT Interval [see Warnings and Precautions (5.9)]
- Musculoskeletal Disorders in Pediatric Patients [see Warnings and Precautions (5.10)]
- Blood Glucose Disturbances [see Warnings and Precautions (5.11)]
- Photosensitivity/Phototoxicity [see Warnings and Precautions (5.12)]
- Development of Drug Resistant Bacteria [see Warnings and Precautions (5.13)]
[see Dosage and Administration (2.5)]
6.2 Clinical Trial Experience
[see Indications and Usage (1)]
| System/Organ Class | Adverse Reaction | % (N = 7537) |
|---|---|---|
|
a N = 7274 b N = 3758 (women) |
||
|
Infections and Infestations
|
moniliasis |
1 |
|
Psychiatric Disorders
|
insomniaa
[see Warnings and Precautions (5.6)] |
4 |
|
Nervous System Disorders
|
headache dizziness [see Warnings and Precautions (5.6)] |
6 3 |
|
Respiratory, Thoracic and
Mediastinal Disorders |
dyspnea [see Warnings and Precautions (5.3)] |
1 |
|
Gastrointestinal Disorders
|
nausea diarrhea constipation abdominal pain vomiting dyspepsia |
7 5 3 2 2 2 |
|
Skin and Subcutaneous
Tissue Disorders |
rash [see Warnings and Precautions (5.3)]
pruritus |
2 1 |
|
Reproductive System and
Breast Disorders |
vaginitis |
1b
|
|
General Disorders and
Administration Site Conditions |
edema injection site reaction chest pain |
1 1 1 |
| System/Organ Class | Adverse Reaction |
|---|---|
|
a N = 7274 |
|
|
Infections and Infestations
|
genital moniliasis |
|
Blood and Lymphatic System Disorders
|
anemia thrombocytopenia granulocytopenia [see Warnings and Precautions (5.4)] |
|
Immune System Disorders
|
allergic reaction [see Warnings and Precautions (5.3, 5.4)] |
|
Metabolism and Nutrition Disorders
|
hyperglycemia hypoglycemia [see Warnings and Precautions (5.11)] hyperkalemia |
|
Psychiatric Disorders
|
anxiety agitation confusion depression hallucination nightmarea [see Warnings and Precautions (5.6)] sleep disordera anorexia abnormal dreaminga |
|
Nervous System Disorders
|
tremor convulsions [see Warnings and Precautions (5.6)] paresthesia [see Warnings and Precautions (5.8)] vertigo hypertonia hyperkinesias abnormal gait somnolencea syncope |
|
Respiratory, Thoracic and Mediastinal Disorders
|
epistaxis |
|
Cardiac Disorders
|
cardiac arrest palpitation ventricular tachycardia ventricular arrhythmia |
|
Vascular Disorders
|
phlebitis |
|
Gastrointestinal Disorders
|
gastritis stomatitis pancreatitis esophagitis gastroenteritis glossitis pseudomembranous/C. difficile colitis [see Warnings and Precautions (5.7)] |
|
Hepatobiliary Disorders
|
abnormal hepatic function increased hepatic enzymes increased alkaline phosphatase |
|
Skin and Subcutaneous Tissue Disorders
|
urticaria [see Warnings and Precautions (5.3)]
|
|
Musculoskeletal and Connective Tissue Disorders
|
arthralgia tendinitis [see Warnings and Precautions (5.1)] myalgia skeletal pain |
|
Renal and Urinary Disorders
|
abnormal renal function acute renal failure [see Warnings and Precautions (5.4)] |
6.3 Postmarketing Experience
| System/Organ Class | Adverse Reaction |
|---|---|
|
Blood and Lymphatic System Disorders
|
pancytopenia aplastic anemia leucopenia hemolytic anemia [see Warnings and Precautions (5.4)] eosinophilia |
|
Immune System Disorders
|
hypersensitivity reactions, sometimes fatal including: anaphylactic/anaphylactoid reactions anaphylactic shock angioneurotic edema serum sickness [see Warnings and Precautions (5.3, 5.4)] |
|
Psychiatric Disorders
|
psychosis paranoia isolated reports of suicide attempt and suicidal ideation [see Warnings and Precautions (5.6)] |
|
Nervous System Disorders
|
exacerbation of myasthenia gravis [see Warnings and Precautions (5.2)]
anosmia ageusia parosmia dysgeusia peripheral neuropathy [see Warnings and Precautions (5.8)] isolated reports of encephalopathy abnormal electroencephalogram (EEG) dysphonia pseudotumor cerebri [see Warnings and Precautions (5.6)] |
|
Eye Disorders
|
vision disturbance, including diplopia visual acuity reduced vision blurred scotoma |
|
Ear and Labyrinth Disorders
|
hypoacusis tinnitus |
|
Cardiac Disorders
|
isolated reports of torsade de pointes electrocardiogram QT prolonged [see Warnings and Precautions (5.9)] tachycardia |
|
Vascular Disorders
|
vasodilatation |
|
Respiratory, Thoracic and Mediastinal Disorders
|
isolated reports of allergic pneumonitis [see Warnings and Precautions (5.4)]
|
|
Hepatobiliary Disorders
|
hepatic failure (including fatal cases) hepatitis jaundice [see Warnings and Precautions (5.4, 5.5)] |
|
Skin and Subcutaneous Tissue Disorders
|
bullous eruptions to include: Stevens-Johnson Syndrome toxic epidermal necrolysis erythema multiforme [see Warnings and Precautions (5.4)] photosensitivity/phototoxicity reaction [see Warnings and Precautions (5.12)] leukocytoclastic vasculitis |
|
Musculoskeletal and Connective Tissue Disorders
|
tendon rupture [see Warnings and Precautions (5.1)]
muscle injury, including rupture rhabdomyolysis |
|
Renal and Urinary Disorders
|
interstitial nephritis [see Warnings and Precautions (5.4)]
|
|
General Disorders and Administration Site Conditions
|
multi-organ failure pyrexia |
|
Investigations
|
prothrombin time prolonged international normalized ratio prolonged muscle enzymes increased |
7 DRUG INTERACTIONS
7.1 Chelation Agents: Antacids, Sucralfate, Metal Cations, Multivitamins
Levofloxacin Tablets
7.2 Warfarin
[see Adverse Reactions (6.3); Patient Counseling Information (17.4)].
7.3 Antidiabetic Agents
Disturbances of blood glucose, including hyperglycemia and hypoglycemia, have been reported in patients treated concomitantly with fluoroquinolones and an antidiabetic agent. Therefore, careful monitoring of blood glucose is recommended when these agents are coadministered [see Warnings and Precautions (5.11); Adverse Reactions (6.2), Patient Counseling Information (17.4)].
7.4 Non-Steroidal Anti-Inflammatory Drugs
The concomitant administration of a non-steroidal anti-inflammatory drug with a fluoroquinolone, including levofloxacin, may increase the risk of CNS stimulation and convulsive seizures [see Warnings and Precautions (5.6)].
7.5 Theophylline
No significant effect of levofloxacin on the plasma concentrations, AUC, and other disposition parameters for theophylline was detected in a clinical study involving healthy volunteers. Similarly, no apparent effect of theophylline on levofloxacin absorption and disposition was observed. However, concomitant administration of other fluoroquinolones with theophylline has resulted in prolonged elimination half-life, elevated serum theophylline levels, and a subsequent increase in the risk of theophylline-related adverse reactions in the patient population. Therefore, theophylline levels should be closely monitored and appropriate dosage adjustments made when levofloxacin is coadministered. Adverse reactions, including seizures, may occur with or without an elevation in serum theophylline levels [see Warnings and Precautions (5.6)].
7.6 Cyclosporine
No significant effect of levofloxacin on the peak plasma concentrations, AUC, and other disposition parameters for cyclosporine was detected in a clinical study involving healthy volunteers. However, elevated serum levels of cyclosporine have been reported in the patient population when coadministered with some other fluoroquinolones. Levofloxacin Cmax and ke were slightly lower while Tmax and t½ were slightly longer in the presence of cyclosporine than those observed in other studies without concomitant medication. The differences, however, are not considered to be clinically significant. Therefore, no dosage adjustment is required for levofloxacin or cyclosporine when administered concomitantly.
7.7 Digoxin
No significant effect of levofloxacin on the peak plasma concentrations, AUC, and other disposition parameters for digoxin was detected in a clinical study involving healthy volunteers. Levofloxacin absorption and disposition kinetics were similar in the presence or absence of digoxin. Therefore, no dosage adjustment for levofloxacin or digoxin is required when administered concomitantly.
7.8 Probenecid and Cimetidine
No significant effect of probenecid or cimetidine on the Cmax of levofloxacin was observed in a clinical study involving healthy volunteers. The AUC and t1/2 of levofloxacin were higher while CL/F and CLR were lower during concomitant treatment of levofloxacin with probenecid or cimetidine compared to levofloxacin alone. However, these changes do not warrant dosage adjustment for levofloxacin when probenecid or cimetidine is coadministered.
7.9 Interactions with Laboratory or Diagnostic Testing
Some fluoroquinolones, including levofloxacin, may produce false-positive urine screening results for opiates using commercially available immunoassay kits. Confirmation of positive opiate screens by more specific methods may be necessary.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
Based on data on other fluoroquinolones and very limited data on levofloxacin, it can be presumed that levofloxacin will be excreted in human milk. Because of the potential for serious adverse reactions from levofloxacin in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
[see Warnings and Precautions (5.10) and Animal Toxicology and/or Pharmacology (13.2)]
Inhalational Anthrax (Post-Exposure)
[see Indications and Usage (1.13), Dosage and Administration (2.2) and Clinical Studies (14.9)]
Plague
Yersinia pestis Y. pestis[see Indications and Usage (1.14), Dosage and Administration (2.2) and Clinical Studies (14.10)].
Adverse Events
| Follow-up Period | Levofloxacin N = 1340 |
Non-Fluoroquinolonea
N = 893 |
p-valueb |
|---|---|---|---|
|
a Non-Fluoroquinolone: ceftriaxone, amoxicillin/clavulanate, clarithromycin b 2-sided Fisher’s Exact Test c There were 1199 levofloxacin-treated and 804 non-fluoroquinolone-treated children who had a one-year evaluation visit. However, the incidence of musculoskeletal disorders was calculated using all reported events during the specified period for all children enrolled regardless of whether they completed the 1-year evaluation visit. |
|||
|
60 days
|
28 (2.1%) |
8 (0.9%) |
p = 0.038 |
|
1 yearc
|
46 (3.4%) |
16 (1.8%) |
p = 0.025 |
[see Adverse Reactions (6)]
8.5 Geriatric Use
[see Boxed Warning; Warnings and Precautions (5.1); and Adverse Reactions (6.3)]
[see Warnings and Precautions (5.5)].
[see Warnings and Precautions (5.9)].
[see Clinical Pharmacology (12.3)]
8.6 Renal Impairment
Clearance of levofloxacin is substantially reduced and plasma elimination half-life is substantially prolonged in patients with impaired renal function (creatinine clearance <50 mL/min), requiring dosage adjustment in such patients to avoid accumulation. Neither hemodialysis nor continuous ambulatory peritoneal dialysis (CAPD) is effective in removal of levofloxacin from the body, indicating that supplemental doses of levofloxacin are not required following hemodialysis or CAPD [see Dosage and Administration (2.3)].
8.7 Hepatic Impairment
Pharmacokinetic studies in hepatically impaired patients have not been conducted. Due to the limited extent of levofloxacin metabolism, the pharmacokinetics of levofloxacin are not expected to be affected by hepatic impairment.
10 OVERDOSAGE
11 DESCRIPTION
Levofloxacin is a synthetic broad-spectrum antibacterial agent for oral administration. Chemically, levofloxacin, a chiral fluorinated carboxyquinolone, is the pure (-)-(S)-enantiomer of the racemic drug substance ofloxacin. The chemical name is (-)-(S)-9-fluoro-2,3-dihydro-3-methyl-10-(4-methyl-1-piperazinyl)-7-oxo-7H-pyrido[1,2,3-de]-1,4-benzoxazine-6-carboxylic acid hemihydrate.
Figure 1: The Chemical Structure of Levofloxacin
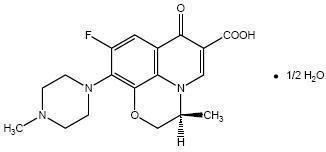
The molecular formula is C18H20FN3O4 • ½ H2O and the molecular weight is 370.38. Levofloxacin USP is a pale or bright yellow, crystalline powder. The molecule exists as a zwitterion at the pH conditions in the small intestine.
The data demonstrate that from pH 0.6 to 5.8, the solubility of levofloxacin USP is essentially constant (approximately 100 mg/mL). Levofloxacin USP is considered soluble to freely soluble in this pH range, as defined by USP nomenclature. Above pH 5.8, the solubility increases rapidly to its maximum at pH 6.7 (272 mg/mL) and is considered freely soluble in this range. Above pH 6.7, the solubility decreases and reaches a minimum value (about 50 mg/mL) at a pH of approximately 6.9.
Levofloxacin USP has the potential to form stable coordination compounds with many metal ions. This in vitro chelation potential has the following formation order: Al+3>Cu+2>Zn+2>Mg+2>Ca+2.
Excipients and Description of Dosage Forms
Levofloxacin tablets are available as film-coated tablets and contain the following inactive ingredients:
250 mg, 500 mg and 750 mg (as expressed in the anhydrous form): croscarmellose sodium, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol 400, polysorbate 80, and titanium dioxide. In addition 250 mg contains iron oxide red and 500 mg contains iron oxide red and iron oxide yellow.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Levofloxacin is a member of the fluoroquinolone class of antibacterial agents [see Clinical Pharmacology (12.4)].
12.3 Pharmacokinetics
The mean ± SD pharmacokinetic parameters of levofloxacin determined under single and steady-state conditions following oral tablet, oral solution, or intravenous (IV) doses of levofloxacin are summarized in Table 8.
| Regimen | Cmax
(mcg/mL) |
Tmax
(h) |
AUC (mcg•h/mL) |
CL/F1
(mL/min) |
Vd/F2
(L) |
t1/2
(h) |
CLR
(mL/min) |
|---|---|---|---|---|---|---|---|
|
1 clearance/bioavailability 2 volume of distribution/bioavailability 3 healthy males 18 to 53 years of age 4 60 min infusion for 250 mg and 500 mg doses, 90 min infusion for 750 mg dose 5 healthy male and female subjects 18 to 54 years of age 6 500 mg every 48 h for patients with moderate renal impairment (CLCR 20 to 50 mL/min) and infections of the respiratory tract or skin 7 dose-normalized values (to 500 mg dose), estimated by population pharmacokinetic modeling 8 healthy males 22 to 75 years of age 9 healthy females 18 to 80 years of age 10 young healthy male and female subjects 18 to 36 years of age 11 healthy elderly male and female subjects 66 to 80 years of age 12 healthy males and females 19 to 55 years of age. * Absolute bioavailability; F=0.99 ± 0.08 from a 500 mg tablet and F=0.99 ± 0.06 from a 750 mg tablet; ND=not determined. |
|||||||
| Single dose | |||||||
| 250 mg oral tablet3 | 2.8 ± 0.4 | 1.6 ± 1 | 27.2 ± 3.9 | 156 ± 20 | ND | 7.3 ± 0.9 | 142 ± 21 |
| 500 mg oral tablet3* | 5.1 ± 0.8 | 1.3 ± 0.6 | 47.9 ± 6.8 | 178 ± 28 | ND | 6.3 ± 0.6 | 103 ± 30 |
| 500 mg oral solution12 | 5.8 ± 1.8 | 0.8 ± 0.7 | 47.8 ± 10.8 | 183 ± 40 | 112 ± 37.2 | 7 ± 1.4 | ND |
| 500 mg IV3 | 6.2 ± 1 | 1 ± 0.1 | 48.3 ± 5.4 | 175 ± 20 | 90 ± 11 | 6.4 ± 0.7 | 112 ± 25 |
| 750 mg oral tablet5* | 9.3 ± 1.6 | 1.6 ± 0.8 | 101 ± 20 | 129 ± 24 | 83 ± 17 | 7.5 ± 0.9 | ND |
| 750 mg IV5 | 11.5 ± 44 | ND | 110 ± 40 | 126 ± 39 | 75 ± 13 | 7.5 ± 1.6 | ND |
| Multiple dose | |||||||
| 500 mg every 24 h oral tablet3 | 5.7 ± 1.4 | 1.1 ± 0.4 | 47.5 ± 6.7 | 175 ± 25 | 102 ± 22 | 7.6 ± 1.6 | 116 ± 31 |
| 500 mg every 24 h IV3 | 6.4 ± 0.8 | ND | 54.6 ± 11.1 | 158 ± 29 | 91 ± 12 | 7 ± 0.8 | 99 ± 28 |
| 500 mg or 250 mg every 24 h IV, patients with bacterial infection6 | 8.7 ± 47 | ND | 72.5 ± 51.27 | 154 ± 72 | 111 ± 58 | ND | ND |
| 750 mg every 24 h oral tablet5 | 8.6 ± 1.9 | 1.4 ± 0.5 | 90.7 ± 17.6 | 143 ± 29 | 100 ± 16 | 8.8 ± 1.5 | 116 ± 28 |
| 750 mg every 24 h IV5 | 12.1 ± 4.14 | ND | 108 ± 34 | 126 ± 37 | 80 ± 27 | 7.9 ± 1.9 | ND |
| 500 mg oral tablet single dose, effects of gender and age: | |||||||
| Male8 | 5.5 ± 1.1 | 1.2 ± 0.4 | 54.4 ± 18.9 | 166 ± 44 | 89 ± 13 | 7.5 ± 2.1 | 126 ± 38 |
| Female9 | 7 ± 1.6 | 1.7 ± 0.5 | 67.7 ± 24.2 | 136 ± 44 | 62 ± 16 | 6.1 ± 0.8 | 106 ± 40 |
| Young10 | 5.5 ± 1 | 1.5 ± 0.6 | 47.5 ± 9.8 | 182 ± 35 | 83 ± 18 | 6 ± 0.9 | 140 ± 33 |
| Elderly11 | 7 ± 1.6 | 1.4 ± 0.5 | 74.7 ± 23.3 | 121 ± 33 | 67 ± 19 | 7.6 ± 2 | 91 ± 29 |
| 500 mg oral single dose tablet, patients with renal insufficiency: | |||||||
| CLCR 50 to 80 mL/min | 7.5 ± 1.8 | 1.5 ± 0.5 | 95.6 ± 11.8 | 88 ± 10 | ND | 9.1 ± 0.9 | 57 ± 8 |
| CLCR 20 to 49 mL/min | 7.1 ± 3.1 | 2.1 ± 1.3 | 182.1 ± 62.6 | 51 ± 19 | ND | 27 ± 10 | 26 ± 13 |
| CLCR <20 mL/min | 8.2 ± 2.6 | 1.1 ± 1 | 263.5 ± 72.5 | 33 ± 8 | ND | 35 ± 5 | 13 ± 3 |
| Hemodialysis | 5.7 ± 1 | 2.8 ± 2.2 | ND | ND | ND | 76 ± 42 | ND |
| CAPD | 6.9 ± 2.3 | 1.4 ± 1.1 | ND | ND | ND | 51 ± 24 | ND |
Absorption
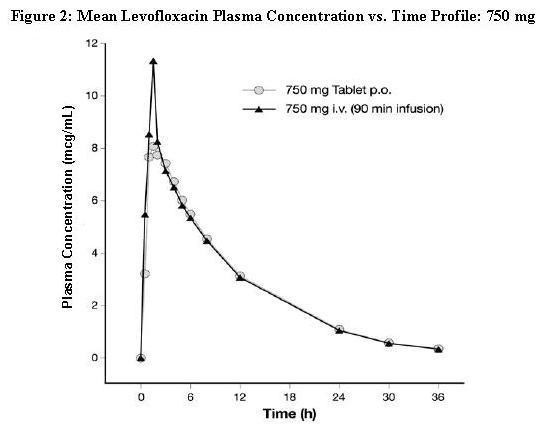
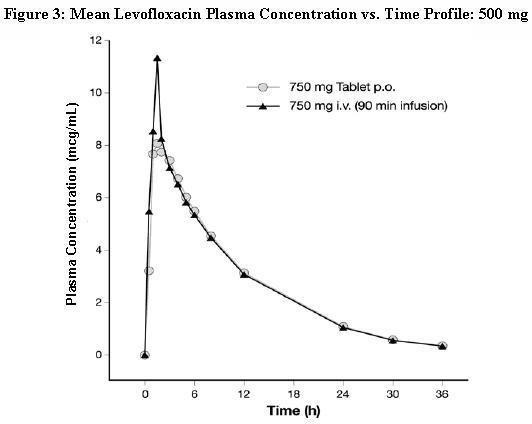
Levofloxacin is rapidly and essentially completely absorbed after oral administration. Peak plasma concentrations are usually attained one to two hours after oral dosing. The absolute bioavailability of levofloxacin from a 500 mg tablet and a 750 mg tablet of levofloxacin are both approximately 99%, demonstrating complete oral absorption of levofloxacin. Following a single intravenous dose of levofloxacin to healthy volunteers, the mean ± SD peak plasma concentration attained was 6.2 ± 1 mcg/mL after a 500 mg dose infused over 60 minutes and 11.5 ± 4 mcg/mL after a 750 mg dose infused over 90 minutes. Levofloxacin oral solution and tablet formulations are bioequivalent.
Levofloxacin pharmacokinetics are linear and predictable after single and multiple oral or IV dosing regimens. Steady-state conditions are reached within 48 hours following a 500 mg or 750 mg once-daily dosage regimen. The mean ± SD peak and trough plasma concentrations attained following multiple once-daily oral dosage regimens were approximately 5.7 ± 1.4 and 0.5 ± 0.2 mcg/mL after the 500 mg doses, and 8.6 ± 1.9 and 1.1 ± 0.4 mcg/mL after the 750 mg doses, respectively. The mean ± SD peak and trough plasma concentrations attained following multiple once-daily IV regimens were approximately 6.4 ± 0.8 and 0.6 ± 0.2 mcg/mL after the 500 mg doses, and 12.1 ± 4.1 and 1.3 ± 0.71 mcg/mL after the 750 mg doses, respectively. Oral administration of a 500 mg dose of levofloxacin with food prolongs the time to peak concentration by approximately 1 hour and decreases the peak concentration by approximately 14% following tablet and approximately 25% following oral solution administration. Therefore, levofloxacin tablets can be administered without regard to food. It is recommended that levofloxacin oral solution be taken 1 hour before or 2 hours after eating.
The plasma concentration profile of levofloxacin after IV administration is similar and comparable in extent of exposure (AUC) to that observed for levofloxacin tablets when equal doses (mg/mg) are administered. Therefore, the oral and IV routes of administration can be considered interchangeable (see Figure 2 and Figure 3).
Distribution
The mean volume of distribution of levofloxacin generally ranges from 74 to 112 L after single and multiple 500 mg or 750 mg doses, indicating widespread distribution into body tissues. Levofloxacin reaches its peak levels in skin tissues and in blister fluid of healthy subjects at approximately 3 hours after dosing. The skin tissue biopsy to plasma AUC ratio is approximately 2 and the blister fluid to plasma AUC ratio is approximately 1 following multiple once-daily oral administration of 750 mg and 500 mg doses of levofloxacin, respectively, to healthy subjects. Levofloxacin also penetrates well into lung tissues. Lung tissue concentrations were generally 2- to 5-fold higher than plasma concentrations and ranged from approximately 2.4 to 11.3 mcg/g over a 24-hour period after a single 500 mg oral dose.
In vitro, over a clinically relevant range (1 to 10 mcg/mL) of serum/plasma levofloxacin concentrations, levofloxacin is approximately 24 to 38% bound to serum proteins across all species studied, as determined by the equilibrium dialysis method. Levofloxacin is mainly bound to serum albumin in humans. Levofloxacin binding to serum proteins is independent of the drug concentration.
Metabolism
Levofloxacin is stereochemically stable in plasma and urine and does not invert metabolically to its enantiomer, D-ofloxacin. Levofloxacin undergoes limited metabolism in humans and is primarily excreted as unchanged drug in the urine. Following oral administration, approximately 87% of an administered dose was recovered as unchanged drug in urine within 48 hours, whereas less than 4% of the dose was recovered in feces in 72 hours. Less than 5% of an administered dose was recovered in the urine as the desmethyl and N-oxide metabolites, the only metabolites identified in humans. These metabolites have little relevant pharmacological activity.
Excretion
Levofloxacin is excreted largely as unchanged drug in the urine. The mean terminal plasma elimination half-life of levofloxacin ranges from approximately 6 to 8 hours following single or multiple doses of levofloxacin given orally or intravenously. The mean apparent total body clearance and renal clearance range from approximately 144 to 226 mL/min and 96 to 142 mL/min, respectively. Renal clearance in excess of the glomerular filtration rate suggests that tubular secretion of levofloxacin occurs in addition to its glomerular filtration. Concomitant administration of either cimetidine or probenecid results in approximately 24% and 35% reduction in the levofloxacin renal clearance, respectively, indicating that secretion of levofloxacin occurs in the renal proximal tubule. No levofloxacin crystals were found in any of the urine samples freshly collected from subjects receiving levofloxacin.
Geriatric
There are no significant differences in levofloxacin pharmacokinetics between young and elderly subjects when the subjects’ differences in creatinine clearance are taken into consideration. Following a 500 mg oral dose of levofloxacin to healthy elderly subjects (66 to 80 years of age), the mean terminal plasma elimination half-life of levofloxacin was about 7.6 hours, as compared to approximately 6 hours in younger adults. The difference was attributable to the variation in renal function status of the subjects and was not believed to be clinically significant. Drug absorption appears to be unaffected by age. Levofloxacin dose adjustment based on age alone is not necessary [see Use in Specific Populations (8.5)].
Pediatrics
The pharmacokinetics of levofloxacin following a single 7 mg/kg intravenous dose were investigated in pediatric patients ranging in age from 6 months to 16 years. Pediatric patients cleared levofloxacin faster than adult patients, resulting in lower plasma exposures than adults for a given mg/kg dose. Subsequent pharmacokinetic analyses predicted that a dosage regimen of 8 mg/kg every 12 hours (not to exceed 250 mg per dose) for pediatric patients 6 months to 17 years of age would achieve comparable steady state plasma exposures (AUC0-24 and Cmax) to those observed in adult patients administered 500 mg of levofloxacin once every 24 hours.
Gender
There are no significant differences in levofloxacin pharmacokinetics between male and female subjects when subjects’ differences in creatinine clearance are taken into consideration. Following a 500 mg oral dose of levofloxacin to healthy male subjects, the mean terminal plasma elimination half-life of levofloxacin was about 7.5 hours, as compared to approximately 6.1 hours in female subjects. This difference was attributable to the variation in renal function status of the male and female subjects and was not believed to be clinically significant. Drug absorption appears to be unaffected by the gender of the subjects. Dose adjustment based on gender alone is not necessary.
Race
The effect of race on levofloxacin pharmacokinetics was examined through a covariate analysis performed on data from 72 subjects: 48 white and 24 non-white. The apparent total body clearance and apparent volume of distribution were not affected by the race of the subjects.
Renal Impairment
Clearance of levofloxacin is substantially reduced and plasma elimination half-life is substantially prolonged in adult patients with impaired renal function (creatinine clearance < 50 mL/min), requiring dosage adjustment in such patients to avoid accumulation. Neither hemodialysis nor continuous ambulatory peritoneal dialysis (CAPD) is effective in removal of levofloxacin from the body, indicating that supplemental doses of levofloxacin are not required following hemodialysis or CAPD [see Dosage and Administration (2.3), Use in Specific Populations (8.6)].
Hepatic Impairment
Pharmacokinetic studies in hepatically impaired patients have not been conducted. Due to the limited extent of levofloxacin metabolism, the pharmacokinetics of levofloxacin are not expected to be affected by hepatic impairment [see Use in Specific Populations (8.7)].
Bacterial Infection
The pharmacokinetics of levofloxacin in patients with serious community-acquired bacterial infections are comparable to those observed in healthy subjects.
Drug-Drug Interactions
The potential for pharmacokinetic drug interactions between levofloxacin and antacids, warfarin, theophylline, cyclosporine, digoxin, probenecid, and cimetidine has been evaluated [see Drug Interactions (7)].
12.4 Microbiology
Mechanism of Action
Mechanism of Resistance
in vitro-9-10
Activity in vitro and in vivo
in vitro
in vitro Indications and Usage (1):
Gram-Positive Bacteria
Enterococcus faecalis
Staphylococcus aureus
Staphylococcus epidermidis
Staphylococcus saprophyticus
Streptococcus pneumoniae
Streptococcus pyogenes
Streptococcus pneumoniaend
Gram-Negative Bacteria
Enterobacter cloacae
Escherichia coli
Haemophilus influenzae
Haemophilus parainfluenzae
Klebsiella pneumoniae
Legionella pneumophila
Moraxella catarrhalis
Proteus mirabilis
Pseudomonas aeruginosa
Serratia marcescens
Other Bacteria
Chlamydophila pneumoniae
Mycoplasma pneumoniae
in vitrobut their clinical significance is unknown: in vitro
Gram-Positive Bacteria
Staphylococcus haemolyticus
Streptococcus (Group C/F)
-hemolytic Streptococcus (Group G)
Streptococcus agalactiae
Streptococcus milleri
streptococci
Bacillus anthracis
Gram-Negative Bacteria
Acinetobacter baumannii
Acinetobacter lwoffii
Bordetella pertussis
Citrobacter koseri
Citrobacter freundii
Enterobacter aerogenes
Enterobacter sakazakii
Klebsiella oxytoca
Morganella morganii
Pantoea agglomerans
Proteus vulgaris
Providencia rettgeri
Providencia stuartii
Pseudomonas fluorescens
Yersinia pestis
Anaerobic Gram-Positive Bacteria
Clostridium perfringens
Susceptibility Tests
in vitro
Dilution techniques
1,2,4
Diffusion techniques:
2,3
| Pathogen | Minimum Inhibitory Concentrations (mcg/mL) |
Disk Diffusion (zone diameter in mm) |
||||
|---|---|---|---|---|---|---|
| S | I | R | S | I | R | |
| S = Susceptible, I = Intermediate, R = Resistant a The current absence of data on resistant isolates precludes defining any categories other than “Susceptible.” Isolates yielding MIC/zone diameter results suggestive of a “nonsusceptible” category should be submitted to a reference laboratory for further testing. |
||||||
|
Enterobacteriaceae
|
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Enterococcus faecalis
|
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Staphylococcus species |
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Pseudomonas aeruginosa
|
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Haemophilus influenzae
|
≤2 |
--a
|
-- |
≥17 |
-- |
-- |
|
Haemophilus parainfluenzae
|
≤2 |
-- |
-- |
≥17 |
-- |
-- |
|
Streptococcus pneumoniae
|
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Streptococcus pyogenes
|
≤2 |
4 |
≥8 |
≥17 |
14-16 |
≤13 |
|
Yersinia pestis4
|
≤0.25 |
-- |
-- |
-- |
-- |
-- |
|
Bacillus anthracis4
|
≤0.25 |
-- |
-- |
-- |
-- |
-- |
SusceptibleIntermediateResistant
Quality Control:
1,2,3,4
| Microorganism | Microorganism QC Number |
MIC (mcg/mL) | Disk Diffusion (zone diameter in mm) |
|---|---|---|---|
|
Enterococcus faecalis
|
ATCC 29212 |
0.25 – 2 |
-- |
|
Escherichia coli
|
ATCC 25922 |
0.008 – 0.06 |
29 – 37 |
|
Escherichia coli
|
ATCC 35218 |
0.015 – 0.06 |
-- |
|
Haemophilus influenzae
|
ATCC 49247 |
0.008 – 0.03 |
32 – 40 |
|
Pseudomonas aeruginosa
|
ATCC 27853 |
0.5 – 4 |
19 – 26 |
|
Staphylococcus aureus
|
ATCC 29213 |
0.06 – 0.5 |
-- |
|
Staphylococcus aureus
|
ATCC 25923 |
-- |
25 – 30 |
|
Streptococcus pneumoniae
|
ATCC 49619 |
0.5 – 2 |
20 – 25 |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
max
S. typhimuriumE. coli)in vitro
13.2 Animal Toxicology and/or Pharmacology
[see Warnings and Precautions (5.10)].
In vitroin vivo
14 CLINICAL STUDIES
14.1 Nosocomial Pneumonia
Pseudomonas aeruginosaS. aureus
| Pathogen | N | Levofloxacin No. (%) of Patients Microbiologic/ Clinical Outcomes |
N | Imipenem/Cilastatin No. (%) of Patients Microbiologic/ Clinical Outcomes |
|---|---|---|---|---|
|
a Methicillin-susceptible S. aureus
b See above text for use of combination therapy c The observed differences in rates for the clinical and microbiological outcomes may reflect other factors that were not accounted for in the study |
||||
| MSSAa
|
21 |
14 (66.7)/13 (61.9) |
19 |
13 (68.4)/15 (78.9) |
|
P. aeruginosab
|
17 |
10 (58.8)/11 (64.7) |
17 |
5 (29.4)/7 (41.2) |
|
S. marcescens
|
11 |
9 (81.8)/7 (63.6) |
7 |
2 (28.6)/3 (42.9) |
|
E. coli
|
12 |
10 (83.3)/7 (58.3) |
11 |
7 (63.6)/8 (72.7) |
|
K. pneumoniaec
|
11 |
9 (81.8)/5 (45.5) |
7 |
6 (85.7)/3 (42.9) |
|
H. influenzae
|
16 |
13 (81.3)/10 (62.5) |
15 |
14 (93.3)/11 (73.3) |
|
S. pneumoniae
|
4 |
3 (75)/3 (75) |
7 |
5 (71.4)/4 (57.1) |
14.2 Community-Acquired Pneumonia: 7 to 14 day Treatment Regimen
Chlamydophila pneumoniae, Mycoplasma pneumoniaeLegionella pneumophila
| Pathogen | No. Pathogens | Bacteriological Eradication Rate (%) |
|---|---|---|
|
H. influenzae
|
55 |
98 |
|
S. pneumoniae
|
83 |
95 |
|
S. aureus
|
17 |
88 |
|
M. catarrhalis
|
18 |
94 |
|
H. parainfluenzae
|
19 |
95 |
|
K. pneumoniae
|
10 |
100 |
Community-Acquired Pneumonia Due to Multi-Drug Resistant Streptococcus pneumoniae
Streptococcus pneumoniae nd
| Screening Susceptibility | Clinical Success | Bacteriological Successc | ||
|---|---|---|---|---|
| n/Na | % | n/Nb | % | |
|
a n=the number of microbiologically evaluable patients who were clinical successes; N=number of microbiologically evaluable patients in the designated resistance group. b n=the number of MDRSP isolates eradicated or presumed eradicated in microbiologically evaluable patients; N=number of MDRSP isolates in a designated resistance group. c One patient had a respiratory isolate that was resistant to tetracycline, cefuroxime, macrolides and TMP/SMX and intermediate to penicillin and a blood isolate that was intermediate to penicillin and cefuroxime and resistant to the other classes. The patient is included in the database based on respiratory isolate. |
||||
|
Penicillin-resistant
|
16/17 |
94.1 |
16/17 |
94.1 |
|
2nd generation Cephalosporin resistant
|
31/32 |
96.9 |
31/32 |
96.9 |
|
Macrolide-resistant
|
28/29 |
96.6 |
28/29 |
96.6 |
|
Trimethoprim/Sulfamethoxazole resistant
|
17/19 |
89.5 |
17/19 |
89.5 |
|
Tetracycline-resistant
|
12/12 |
100 |
12/12 |
100 |
| Type of Resistance | Clinical Success | Bacteriologic Eradication |
|---|---|---|
| Resistant to 2 antibacterials |
17/18 (94.4%) |
17/18 (94.4%) |
| Resistant to 3 antibacterials |
14/15 (93.3%) |
14/15 (93.3%) |
| Resistant to 4 antibacterials |
7/7 (100%) |
7/7 (100%) |
| Resistant to 5 antibacterials |
0 |
0 |
| Bacteremia with MDRSP |
8/9 (89%) |
8/9 (89%) |
14.3 Community-Acquired Pneumonia: 5-day Treatment Regimen
| S. pneumoniae
|
19/20 (95%) |
|
Haemophilus influenzae
|
12/12 (100%) |
|
Haemophilus parainfluenzae
|
10/10 (100%) |
|
Mycoplasma pneumoniae
|
26/27 (96%) |
|
Chlamydophila pneumoniae
|
13/15 (87%) |
14.4 Acute Bacterial Sinusitis: 5-day and 10 to 14 day Treatment Regimens
| Pathogen | Levofloxacin 750 mg x 5 days | Levofloxacin 500 mg x 10 days |
|---|---|---|
| * Note: Forty percent of the subjects in this trial had specimens obtained by sinus endoscopy. The efficacy data for subjects whose specimen was obtained endoscopically were comparable to those presented in the above table. |
||
|
Streptococcus pneumoniae*
|
25/27 (92.6%) |
26/27 (96.3%) |
|
Haemophilus influenzae*
|
19/21 (90.5%) |
25/27 (92.6%) |
|
Moraxella catarrhalis*
|
10/11 (90.9%) |
13/13 (100%) |
14.5 Complicated Skin and Skin Structure Infections
14.6 Chronic Bacterial Prostatitis
3
| Pathogen | Levofloxacin (N = 136) | Ciprofloxacin (N = 125) | ||
|---|---|---|---|---|
| N | Eradication | N | Eradication | |
| * Eradication rates shown are for patients who had a sole pathogen only; mixed cultures were excluded. |
||||
|
E. coli
|
15 |
14 (93.3%) |
11 |
9 (81.8%) |
|
E. faecalis
|
54 |
39 (72.2%) |
44 |
33 (75%) |
|
S. epidermidis*
|
11 |
9 (81.8%) |
14 |
11 (78.6%) |
14.7 Complicated Urinary Tract Infections and Acute Pyelonephritis: 5-day Treatment Regimen
|
a The mITT population included patients who received study medication and who had a positive (≥105 CFU/mL) urine culture with no more than 2 uropathogens at baseline. Patients with missing response were counted as failures in this analysis. b The Microbiologically Evaluable population included patients with a confirmed diagnosis of cUTI or AP, a causative organism(s) at baseline present at ≥ 105 CFU/mL, a valid test-of-cure urine culture, no pathogen isolated from blood resistant to study drug, no premature discontinuation or loss to follow-up, and compliance with treatment (among other criteria). |
|||||
|
Levofloxacin 750 mg orally or IV once daily for 5 days |
Ciprofloxacin 400 mg IV/500 mg orally twice daily for 10 days |
Overall Difference [95% CI] |
|||
| n/N |
% |
n/N |
% |
Levofloxacin- Ciprofloxacin |
|
|
mITT Populationa
|
|||||
| Overall (cUTI or AP) |
252/333 |
75.7 |
239/318 |
75.2 |
0.5 (-6.1, 7.1) |
| cUTI |
168/230 |
73 |
157/213 |
73.7 |
|
| AP |
84/103 |
81.6 |
82/105 |
78.1 |
|
|
Microbiologically Evaluable Populationb
|
|||||
| Overall (cUTI or AP) |
228/265 |
86 |
215/241 |
89.2 |
-3.2 [-8.9, 2.5] |
| cUTI |
154/185 |
83.2 |
144/165 |
87.3 |
|
| AP |
74/80 |
92.5 |
71/76 |
93.4 |
|
| Pathogen | Bacteriological Eradication Rate (n/N) |
% |
|---|---|---|
| * The predominant organism isolated from patients with AP was E. coli: 91% (63/69) eradication in AP and 89% (92/103) in patients with cUTI. |
||
|
Escherichia coli*
|
155/172 |
90 |
|
Klebsiella pneumoniae
|
20/23 |
87 |
|
Proteus mirabilis
|
12/12 |
100 |
14.8 Complicated Urinary Tract Infections and Acute Pyelonephritis: 10-day Treatment Regimen
|
a 1 to 9 days posttherapy for 30% of subjects enrolled prior to a protocol amendment; 5 to 12 days posttherapy for 70% of subjects. b The mITT population included patients who had a pathogen isolated at baseline. Patients with missing response were counted as failures in this analysis. c The Microbiologically Evaluable population included mITT patients who met protocol-specified evaluability criteria. |
||||
| |
Levofloxacin 250 mg once daily for 10 days |
Ciprofloxacin 500 mg twice daily for 10 days |
||
| n/N |
% |
n/N |
% |
|
|
mITT Populationb
|
174/209 |
83.3 |
184/219 |
84 |
|
Microbiologically Evaluable Populationc
|
164/177 |
92.7 |
159/171 |
93 |
14.9 Inhalational Anthrax (Post-Exposure)
[see Indications and Usage (1.13); Dosage and Administration (2.1, 2.2)].
0-24[see Clinical Pharmacology (12.3)]
[see Warnings and Precautions (5.10), Use in Specific Populations (8.4)].
50650B. anthracismax0-24
14.10 Plague
[see Indications and Usage (1.14) Dosage and Administration (2.1) (2.2)]
0-24[see Clinical Pharmacology (12.3)]
5050Yersinia pestis Y. pestis 0-24oY. pestis Y. pestis
15 REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically. Approved Standard – 9th ed. CLSI Document M7-A9, CLSI, 950 West Valley Rd., Suite 2500, Wayne, PA, 2012.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing; 22nd Informational Supplement. CLSI Document M100 – S22, 2012.
- CLSI Performance Standards for Antimicrobial Disk Susceptibility Tests. Approved Standard – 11th ed. CLSI M2-A11, 2012.
- CLSI. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria; Approved Guideline – 2nd ed. CLSI Document M45-A2, 2010.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Levofloxacin Tablets
Levofloxacin Tablets, 250 mg are terra pink colored capsule shaped, biconvex film-coated tablets, debossed with ‘13’ on one side and ‘T’ on the other side.
Levofloxacin Tablets, 500 mg are peach colored capsule shaped, biconvex film-coated tablets, debossed with ‘12’ on one side and ‘T’ on the other side.
35356-783-07 Bottles of 7
35356-783-10 Bottles of 10
35356-783-14 Bottles of 14
Levofloxacin Tablets, 750 mg are white capsule shaped, biconvex film-coated tablets, debossed with ‘11’ on one side and ‘T’ on the other side.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature] in well-closed containers.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Medication Guide (17.6)
17.1 Antibacterial Resistance
Antibacterial drugs including levofloxacin should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When levofloxacin is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by levofloxacin or other antibacterial drugs in the future.
17.2 Administration with Food, Fluids, and Concomitant Medications
17.3 Serious and Potentially Serious Side Effects
- Tendon Disorders: Patients should contact their healthcare provider if they experience pain, swelling, or inflammation of a tendon, or weakness or inability to use one of their joints; rest and refrain from exercise; and discontinue levofloxacin treatment. The risk of severe tendon disorders with fluoroquinolones is higher in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants.
- Exacerbation of Myasthenia Gravis: Patients should inform their physician of any history of myasthenia gravis. Patients should notify their physician if they experience any symptoms of muscle weakness, including respiratory difficulties.
- Hypersensitivity Reactions: Patients should be informed that levofloxacin can cause hypersensitivity reactions, even following the first dose. Patients should discontinue the drug at the first sign of a skin rash, hives or other skin reactions, a rapid heartbeat, difficulty in swallowing or breathing, any swelling suggesting angioedema (e.g., swelling of the lips, tongue, face, tightness of the throat, hoarseness), or other symptoms of an allergic reaction.
- Hepatotoxicity: Severe hepatotoxicity (including acute hepatitis and fatal events) has been reported in patients taking levofloxacin. Patients should inform their physician and be instructed to discontinue levofloxacin treatment immediately if they experience any signs or symptoms of liver injury including: loss of appetite, nausea, vomiting, fever, weakness, tiredness, right upper quadrant tenderness, itching, yellowing of the skin and eyes, light colored bowel movements or dark colored urine.
- Convulsions: Convulsions have been reported in patients taking fluoroquinolones, including levofloxacin. Patients should notify their physician before taking this drug if they have a history of convulsions.
- Neurologic Adverse Effects (e.g., dizziness, lightheadedness, increased intracranial pressure): Patients should know how they react to levofloxacin before they operate an automobile or machinery or engage in other activities requiring mental alertness and coordination. Patients should notify their physician if persistent headache with or without blurred vision occurs.
- Diarrhea: Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
- Peripheral Neuropathies: If symptoms of peripheral neuropathy including pain, burning, tingling, numbness, and/or weakness develop, patients should discontinue treatment and contact their physician.
- Prolongation of the QT Interval: Patients should inform their physician of any personal or family history of QT prolongation or proarrhythmic conditions such as hypokalemia, bradycardia, or recent myocardial ischemia; if they are taking any Class IA (quinidine, procainamide), or Class III (amiodarone, sotalol) antiarrhythmic agents. Patients should notify their physicians if they have any symptoms of prolongation of the QT interval, including prolonged heart palpitations or a loss of consciousness.
- Musculoskeletal Disorders in Pediatric Patients: Parents should inform their child's physician if their child has a history of joint-related problems before taking this drug. Parents of pediatric patients should also notify their child's physician of any tendon or joint-related problems that occur during or following levofloxacin therapy [see Warnings and Precautions (5.10) and Use in Specific Populations (8.4)].
- Photosensitivity/Phototoxicity: Patients should be advised that photosensitivity/phototoxicity has been reported in patients receiving fluoroquinolone antibiotics. Patients should minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while taking fluoroquinolones. If patients need to be outdoors when taking fluoroquinolones, they should wear loose-fitting clothes that protect skin from sun exposure and discuss other sun protection measures with their physician. If a sunburn like reaction or skin eruption occurs, patients should contact their physician.
17.4 Drug Interactions with Insulin, Oral Hypoglycemic Agents, and Warfarin
17.5 Plague and Anthrax Studies
Aurobindo Pharma USA, Inc.
Aurobindo Pharma Limited
17.6 FDA-Approved Medication Guide
MEDICATION GUIDE
Levofloxacin Tablets
What is the most important information I should know about levofloxacin tablets?
Levofloxacin tablets, a fluoroquinolone antibiotic, can cause serious side effects. Some of these serious side effects could result in death.
1. Tendon rupture or swelling of the tendon (tendinitis).
- Tendon problems can happen in people of all ages who take levofloxacin tablets. Tendons are tough cords of tissue that connect muscles to bones.
- The risk of getting tendon problems while you take levofloxacin tablets are higher if you:
- are over 60 years of age
- are taking steroids (corticosteroids)
- have had a kidney, heart or lung transplant.
- Tendon problems can happen in people who do not have the above risk factors when they take levofloxacin tablets.
- Other reasons that can increase your risk of tendon problems can include:
- physical activity or exercise
- kidney failure
- tendon problems in the past, such as in people with rheumatoid arthritis (RA)
- Call your healthcare provider right away at the first sign of tendon pain, swelling or inflammation. Stop taking levofloxacin tablets until tendinitis or tendon rupture has been ruled out by your healthcare provider. Avoid exercise and using the affected area.
- Tendon rupture can happen while you are taking or after you have finished taking levofloxacin tablets. Tendon ruptures have happened up to several months after people have finished taking their fluoroquinolone.
- Get medical help right away if you get any of the following signs or symptoms of a tendon rupture:
- hear or feel a snap or pop in a tendon area
- bruising right after an injury in a tendon area
- unable to move the affected area or bear weight
2. Worsening of myasthenia gravis (a problem that causes muscle weakness).
- See “What are the possible side effects of levofloxacin tablets?”
What are levofloxacin tablets?
- nosocomial pneumonia
- community-acquired pneumonia
- acute sinus infection
- acute worsening of chronic bronchitis
- skin infections, complicated and uncomplicated
- chronic prostate infection
- urinary tract infections, complicated and uncomplicated
- acute kidney infection (pyelonephritis)
- inhalational anthrax
- plague
Who should not take levofloxacin tablets?
Do not take levofloxacin tablets
What should I tell my healthcare provider before taking levofloxacin tablets?
Before you take levofloxacin tablets, tell your healthcare provider if you:
- have tendon problems
- have a problem that causes muscle weakness (myasthenia gravis)
- have central nervous system problems such as seizures (epilepsy)
- have nerve problems
- have or anyone in your family has an irregular heartbeat, especially a condition called “QT prolongation”
- have low blood potassium (hypokalemia)
- have bone problems
- have joint problems including rheumatoid arthritis (RA)
- have kidney problems. You may need a lower dose of levofloxacin tablets if your kidneys do not work well.
- have liver problems
- have diabetes or problems with low blood sugar (hypoglycemia)
- are pregnant or plan to become pregnant. It is not known if levofloxacin tablets will harm your unborn child.
- are breastfeeding or plan to breastfeed. It is not known if levofloxacin passes into your breast milk. You and your healthcare provider should decide if you will take levofloxacin tablets or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take,
- a steroid medicine
- an anti-psychotic medicine
- a tricyclic antidepressant
- a water pill (diuretic)
- certain medicines may keep levofloxacin tablets from working correctly. Take levofloxacin tablets either 2 hours before or 2 hours after taking these medicines or supplements:
- an antacid, multivitamin, or other medicines or supplements that have magnesium, aluminum, iron, or zinc
- sucralfate (Carafate®)
- didanosine (Videx®,Videx®EC)
- a blood thinner (warfarin, Coumadin, Jantoven)
- an oral anti-diabetes medicine or insulin
- an NSAID (Non-Steroidal Anti-Inflammatory Drug). Many common medicines for pain relief are NSAIDs. Taking an NSAID while you take levofloxacin tablets or other fluoroquinolones may increase your risk of central nervous system effects and seizures.
- theophylline (Theo-24®, Elixophyllin®, Theochron®, Uniphyl®, Theolair®)
- a medicine to control your heart rate or rhythm (antiarrhythmics)
How should I take levofloxacin tablets?
- Take levofloxacin tablets exactly as your healthcare provider tells you to take them.
- Take levofloxacin tablets at about the same time each day.
- Drink plenty of fluids while you take levofloxacin tablets.
- Levofloxacin tablets can be taken with or without food.
- If you miss a dose of levofloxacin tablets, take it as soon as you remember. Do not take more than 1 dose in 1 day.
- Do not skip any doses of levofloxacin tablets or stop taking them, even if you begin to feel better, until you finish your prescribed treatment unless:
- you have tendon problems. See “What is the most important information I should know about levofloxacin tablets?” .
- you have a serious allergic reaction. See “What are the possible side effects of levofloxacin tablets?”.
- your healthcare provider tells you to stop taking levofloxacin tablets.
- If you take too much levofloxacin, call your healthcare provider or get medical help right away.
What should I avoid while taking levofloxacin tablets?
- Levofloxacin tablets can make you feel dizzy and lightheaded. Do not drive, operate machinery, or do other activities that require mental alertness or coordination until you know how levofloxacin tablets affect you.
- Avoid sunlamps, tanning beds, and try to limit your time in the sun. Levofloxacin tablets can make your skin sensitive to the sun (photosensitivity) and the light from sunlamps and tanning beds. You could get severe sunburn, blisters or swelling of your skin. If you get any of these symptoms while you take levofloxacin tablets, call your healthcare provider right away. You should use a sunscreen and wear a hat and clothes that cover your skin if you have to be in sunlight.
What are the possible side effects of levofloxacin tablets?
Levofloxacin tablets can cause serious side effects, including:
- See “What is the most important information I should know about l evofloxacin tablets?”
- Serious allergic reactions.
- hives
- trouble breathing or swallowing
- swelling of the lips, tongue, face
- throat tightness, hoarseness
- rapid heartbeat
- faint
- skin rash
Liver damage (hepatotoxicity):
- nausea or vomiting
- stomach pain
- fever
- weakness
- abdominal pain or tenderness
- itching
- unusual tiredness
- loss of appetite
- light colored bowel movements
- dark colored urine
- yellowing of your skin or the whites of your eyes
- Central Nervous System Effects. Seizures have been reported in people who take fluoroquinolone antibiotics including levofloxacin tablets. Tell your healthcare provider if you have a history of seizures. Ask your healthcare provider whether taking levofloxacin tablets will change your risk of having a seizure.
- seizures
- hear voices, see things, or sense things that are not there (hallucinations)
- feel restless
- tremors
- feel anxious or nervous
- confusion
- depression
- trouble sleeping
- nightmares
- feel lightheaded
- feel more suspicious (paranoia)
- suicidal thoughts or acts
- a headache that will not go away, with or without blurred vision.
- Intestine infection (Pseudomembranous colitis)
- Changes in sensation and possible nerve damage (Peripheral Neuropathy)
- pain
- burning
- tingling
- numbness
- weakness
- Serious heart rhythm changes (QT prolongation and torsades de pointes)
- who are elderly
- with a family history of prolonged QT interval
- with low blood potassium (hypokalemia)
- who take certain medicines to control heart rhythm (antiarrhythmics)
- Joint Problems
- Changes in blood sugar
- Sensitivity to sunlight (photosensitivity)
“What should I avoid while taking levofloxacin tablets?”
- nausea
- headache
- diarrhea
- insomnia
- constipation
- dizziness
How should I store levofloxacin tablets?
- Store levofloxacin tablets at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature].
- Keep levofloxacin tablets in a tightly closed container.
Keep levofloxacin tablets and all medicines out of the reach of children.
General information about the safe and effective use of levofloxacin tablets
What are the ingredients in levofloxacin tablets?
Aurobindo Pharma USA, Inc.
Aurobindo Pharma Limited
Image of Label
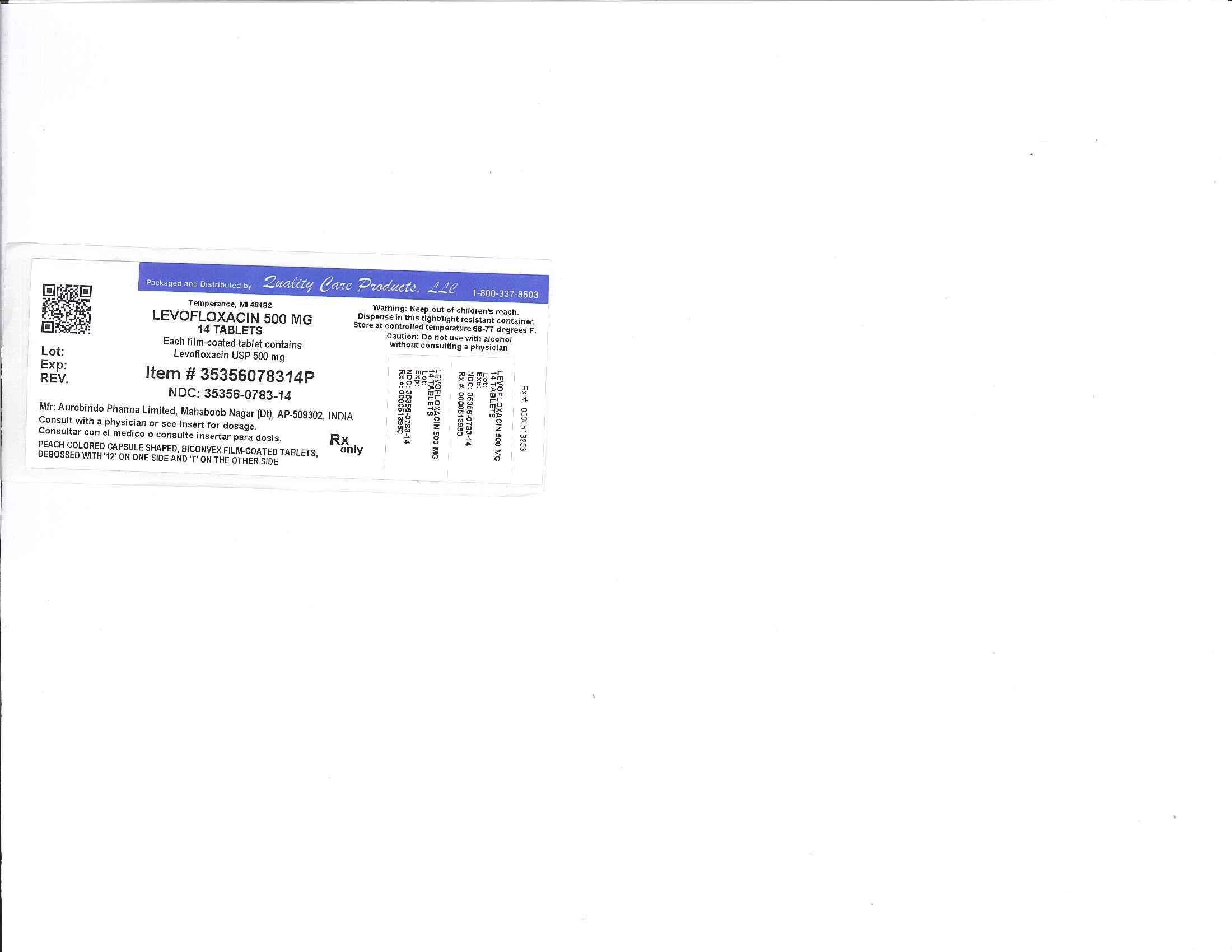
LevofloxacinLevofloxacin TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||