Femring
FULL PRESCRIBING INFORMATION: CONTENTS*
- FEMRING DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL STUDIES
- FEMRING INDICATIONS AND USAGE
- FEMRING CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- FEMRING ADVERSE REACTIONS
- OVERDOSAGE
- FEMRING DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- STORAGE
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
ENDOMETRIAL CANCER
There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding. (See WARNINGS, Malignant neoplasms, Endometrial cancer .)
CARDIOVASCULAR DISORDERS AND PROBABLE DEMENTIA
Estrogen-alone therapy should not be used for the prevention of cardiovascular disease or dementia. (See CLINICAL STUDIES and WARNINGS, Cardiovascular disorders and Dementia.)
The Women's Health Initiative (WHI) estrogen-alone substudy reported increased risks of stroke and deep vein thrombosis (DVT) in postmenopausal women (50 to 79 years of age) during 7.1 years of treatment with daily oral conjugated estrogens (CE) [0.625 mg], relative to placebo. (See CLINICAL STUDIES and WARNINGS, Cardiovascular disorders .)
The Women’s Health Initiative Memory Study (WHIMS) estrogen-alone ancillary study of the WHI reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 5.2 years of treatment with daily CE (0.625 mg)-alone, relative to placebo. It is unknown whether this finding applies to younger postmenopausal women. (See CLINICAL STUDIES and WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .)
In the absence of comparable data, these risks should be assumed to be similar for other doses of CE and other dosage forms of estrogens.
Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
WARNING: CARDIOVASCULAR DISORDERS, BREAST CANCER AND PROBABLE DEMENTIA FOR ESTROGEN PLUS PROGESTIN THERAPY
Estrogens plus progestin therapy should not be used for the prevention of cardiovascular disease or dementia. (See CLINICAL STUDIES and WARNINGS, Cardiovascular disorders , and Dementia .)
The WHI estrogen plus progestin substudy reported increased risks of DVT, pulmonary embolism, stroke, and myocardial infarction in postmenopausal women (50 to 79 years of age) during 5.6 years of treatment with daily oral CE (0.625 mg) combined with medroxyprogesterone acetate (MPA) [2.5 mg], relative to placebo. (See CLINICAL STUDIES and WARNINGS, Cardiovascular disorders .)
The WHI estrogen plus progestin substudy also demonstrated an increased risk of invasive breast cancer. (See CLINICAL STUDIES and WARNINGS, Malignant neoplasms, Breast Cancer .)
The WHIMS estrogen plus progestin ancillary study of the WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with daily CE (0.625 mg) combined with MPA (2.5 mg), relative to placebo. It is unknown whether this finding applies to younger postmenopausal women. (See CLINICAL STUDIES and WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .)
In the absence of comparable data, these risks should be assumed to be similar for other doses of CE and MPA therapy and other combinations and dosage forms of estrogens and progestins.
Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
FEMRING DESCRIPTION
Femring® (estradiol acetate vaginal ring) is an off-white, soft, flexible ring with a central core containing estradiol acetate.
Femring is made of cured silicone elastomer composed of dimethyl polysiloxane silanol, silica (diatomaceous earth), normal propyl orthosilicate, stannous octoate; barium sulfate and estradiol acetate. The rings have the following dimensions: outer diameter 56 mm, cross-sectional diameter 7.6 mm, core diameter 2 mm.
Femring is available in two strengths: Femring 0.05 mg/day has a central core that contains 12.4 mg of estradiol acetate, which releases at a rate equivalent to 0.05 mg of estradiol per day for 3 months. Femring 0.10 mg/day has a central core that contains 24.8 mg of estradiol acetate, which releases at a rate equivalent to 0.10 mg of estradiol per day for 3 months.
Estradiol acetate is chemically described as estra-1,3,5(10)-triene-3,17β-diol-3-acetate. The molecular formula of estradiol acetate is C20H26O3 and the structural formula is:
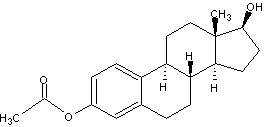
The molecular weight of estradiol acetate is 314.42.
CLINICAL PHARMACOLOGY
Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol, at the receptor level.
The primary source of estrogen in normally cycling adult women is the ovarian follicle which secretes 70 to 500 mcg of estradiol daily depending on the phase of the menstrual cycle. After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone by peripheral tissues. Thus, estrone and the sulfate conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women.
Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These vary in proportion from tissue to tissue.
Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH) through a negative feedback mechanism. Estrogens act to reduce the elevated levels of these hormones seen in postmenopausal women.
Drug delivery from Femring is rapid for the first hour and then declines to a relatively constant rate for the remainder of the 3-month dosing interval. In vitro studies have shown that this initial release is higher as the rings age upon storage. Estradiol acetate is rapidly hydrolyzed to estradiol which is absorbed through the vaginal mucosa as evidenced by the mean time to maximum concentration (tmax) for estradiol of about 1 hour (range 0.25 to 1.5 hrs). Following the maximum concentration (Cmax), serum estradiol decreases rapidly such that by 24 to 48 hours postdose, serum estradiol concentrations are relatively constant through the end of the 3-month dosing interval, see Figure 1 for results from rings stored for 16 months.
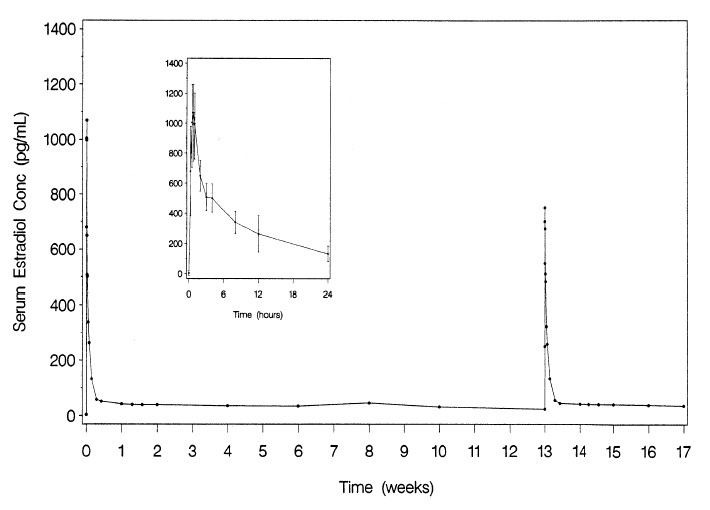
Figure 1. Mean serum estradiol concentrations following multiple dose administration of Femring (0.05 mg/day estradiol) (second dose administered at 13 weeks) (inset: mean (±SD) of serum concentration-time profile for dose 1 from 0-24 hours)
Following administration of Femring (0.05 mg/day estradiol), average serum estradiol concentration was 40.6 pg/mL; the corresponding apparent in vivo estradiol delivery rate was 0.052 mg/day. Following administration of Femring (0.10 mg/day estradiol), average serum estradiol concentration was 76 pg/mL; apparent in vivo delivery rate was 0.097 mg/day. Results are summarized in Table 1 below.
|
Dose (as estradiol) |
|
Number of subjects |
Cmax
(pg/mL) |
Tmax
(hour) |
Cavg
(pg/mL) |
| 0.05 mg/day |
Estradiol† | 25 |
1129 (25) |
0.9 (41) |
40.6 (26) |
|
|
Estrone† | 25 |
141 (25) |
6.2 (84) |
35.9 (21) |
|
|
Estrone sulfate† | 25 |
2365 (44) |
9.3 (39) |
494.6 (48) |
| 0.10 mg/day |
Estradiol‡ | 12 |
1665 (23) |
0.7 (90) |
--§ |
|
|
Estradiol¶ | 11 |
-- |
-- |
76.0 (24) |
|
|
Estrone¶ | 11 |
-- |
-- |
45.7 (25) |
†
‡
§
¶
Consistent with the avoidance of first pass metabolism achieved by vaginal estradiol administration, serum estradiol concentrations were slightly higher than estrone concentrations.
The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estrogens circulate in the blood largely bound to sex hormone binding globulin (SHBG) and to albumin.
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
Estradiol, estrone, and estriol are excreted in the urine along with glucuronide and sulfate conjugates.
No pharmacokinetic studies were conducted in special populations, including patients with renal or hepatic impairment.
In vitro and in vivo studies have shown that estrogens are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. Inducers of CYP3A4 such as St. John’s Wort preparations (Hypericum perforatum), phenobarbital, carbamazepine and rifampin may reduce plasma concentrations of estrogens, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile. Inhibitors of CYP3A4 such as erythromycin, clarithromycin, ketoconazole, itraconazole, ritonavir and grapefruit juice may increase plasma concentrations of estrogens and may result in side effects.
CLINICAL STUDIES
A 13-week double-blind, placebo-controlled clinical trial was conducted to evaluate the efficacy of 2 doses of the vaginal ring in the treatment of moderate to severe vasomotor symptoms in 333 postmenopausal women between 29 and 85 years of age (mean age 51.7 years, 77% were Caucasian) who had at least 7 moderate to severe hot flushes daily or at least 56 moderate to severe hot flushes per week before randomization. Patients were randomized to receive either placebo, Femring 0.05 mg/day or Femring 0.10 mg/day. Femring 0.05 mg/day and Femring 0.10 mg/day were shown to be statistically better than placebo at weeks 4 and 12 for relief of both the frequency and severity of moderate to severe vasomotor symptoms. Frequency results are shown in Table 2. Severity results are shown in Table 3.
| Visit |
Placebo (n = 105) |
Estradiol 0.05 mg/day (n = 111) |
Estradiol 0.10 mg/day (n = 109) |
| Baseline*
|
|
|
|
| Mean (SD) |
83.62 (60.42) |
73.83 (24.53) |
75.11 (25.44) |
| Week 4 |
|
|
|
| Mean (SD) |
51.14 (51.19) |
21.59† (27.76) | 11.37† (19.43) |
| Mean Change from Baseline (SD) |
-32.48 (46.25) |
-52.24† (32.92) | -63.75† (26.68) |
| p value vs. Placebo (95% CI)‡ | - |
less than 0.001 (-30.7, -8.8) | less than 0.001 (-42.2, -20.3) |
| Week 12 |
|
|
|
| Mean (SD) |
42.21 (41.13) |
15.48† (25.42) | 8.25† (16.58) |
| Mean Change from Baseline (SD) |
-41.41 (65.61) |
-58.36† (31.36) | -66.87† (27.44) |
| p value vs. Placebo (95% CI)‡ | - |
0.006 (-30.5, -3.4) |
less than 0.001 (-39.1, -11.8) |
*
†
‡
| Visit |
Placebo (n = 105) |
Estradiol 0.05 mg/day (n = 111) |
Estradiol 0.10 mg/day (n = 109) |
| Baseline*
|
|
|
|
| Mean (SD) |
2.51 (0.26) |
2.46 (0.23) |
2.48 (0.24) |
| Week 4 |
|
|
|
| Mean (SD) |
2.23 (0.71) |
1.67† (1.07) | 1.15† (1.14) |
| Mean Change from Baseline (SD) |
-0.28 (0.69) |
- 0.79† (1.08) | -1.33† (1.10) |
| p value vs. Placebo (95% CI)‡ | - |
less than 0.001 (-0.8, -0.2) | less than 0.001 (-1.3, -0.8) |
| Week 12 |
|
|
|
| Mean (SD) |
2.00 (0.96) |
1.41† (1.17) | 0.92† (1.09) |
| Mean Change from Baseline (SD) |
-0.51 (0.94) |
-1.06† (1.16) | -1.56† (1.06) |
| p value vs. Placebo (95% CI)‡ | - |
less than 0.001 (-0.9, -0.2) | less than 0.001 (-1.4, -0.7) |
*
†
‡
In the same 13-week clinical trial, vaginal superficial cells increased by a mean of 16.0% and 18.9% for Femring 0.05 mg/day and Femring 0.10 mg/day, respectively, as compared to 1.11% for placebo at week 13. A corresponding reduction in parabasal cells was observed at week 13. Vaginal pH decreased for Femring 0.05 mg/day and Femring 0.10 mg/day by a mean of 0.73 and 0.60, respectively, compared to a mean decrease of 0.25 in the placebo group.
The Women’s Health Initiative (WHI) enrolled approximately 27,000 predominantly healthy postmenopausal women in two substudies to assess the risks and benefits of daily oral CE (0.625 mg)-alone or in combination with MPA (2.5 mg) compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of coronary heart disease [(CHD) defined as nonfatal myocardial infarction (MI), silent MI and CHD death], with invasive breast cancer as the primary adverse outcome. A “global index” included the earliest occurrence of CHD, invasive breast cancer, stroke, pulmonary embolism (PE), endometrial cancer (only in the CE plus MPA substudy), colorectal cancer, hip fracture or death due to other cause. The study did not evaluate the effects of CE or CE plus MPA on menopausal symptoms.
WHI Estrogen-Alone Substudy
The WHI estrogen-alone substudy was stopped early because an increased risk of stroke was observed, and it was deemed that no further information would be obtained regarding the risks and benefits of estrogen-alone in predetermined primary endpoints. Results of the estrogen-alone substudy, which included 10,739 women (average age of 63 years, range 50 to 79; 75.3 percent White, 15.1 percent Black, 6.1 percent Hispanic, 3.6 percent Other), after an average follow-up of 7.1 years, are presented in Table 4.
|
Event |
Relative Risk CE vs Placebo (95% nCI*) |
CE n = 5,310 Absolute Risk Women - |
Placebo n = 5,429 per 10,000 Years |
| CHD events† | 0.95 (0.78 - 1.16) |
54 |
57 |
| Non-fatal MI † | 0.91 (0.73 - 1.14) |
40
|
43
|
| CHD death † |
1.01 (0.71 - 1.43)
|
16
|
16
|
| All Stroke† | 1.33 (1.05 - 1.68) |
45 |
33 |
| Ischemic † |
1.55 (1.19 - 2.01)
|
38
|
25
|
| Deep vein thrombosis† , ‡ | 1.47 (1.06 - 2.06) | 23 |
15 |
| Pulmonary embolism† | 1.37 (0.90 - 2.07) |
14 |
10 |
| Invasive breast cancer† | 0.80 (0.62 - 1.04) |
28 |
34 |
| Colorectal cancer§ | 1.08 (0.75 - 1.55) |
17 |
16 |
| Hip fracture† | 0.65 (0.45 - 0.94) |
12 |
19 |
| Vertebral fractures† , ‡ | 0.64 (0.44 - 0.93) |
11 |
18 |
| Lower arm/wrist fractures† , ‡ | 0.58 (0.47 - 0.72) |
35 |
59 |
| Total fractures† , ‡ | 0.71 (0.64 - 0.80) |
144 |
197 |
| Death due to other causes§ , ¶ | 1.08 (0.88 - 1.32) |
53 |
50 |
| Overall mortality† , ‡ | 1.04 (0.88 - 1.22) |
79 |
75 |
| Global Index# | 1.02 (0.92 - 1.13) |
206 |
201 |
†
‡
§
¶
#
For those outcomes included in the WHI “global index” that reached statistical significance, the absolute excess risk per 10,000 women-years in the group treated with CE-alone were 12 more strokes, while the absolute risk reduction per 10,000 women-years was 7 fewer hip fractures. The absolute excess risk of events included in the “global index” was a nonsignificant 5 events per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality. (See BOXED WARNINGS , WARNINGS , and PRECAUTIONS .)
No overall difference for primary CHD events (nonfatal MI, silent MI and CHD death) and invasive breast cancer incidence in women receiving CE-alone compared with placebo was reported in final centrally adjudicated results from the estrogen-alone substudy, after an average follow-up of 7.1 years (see Table 4).
Centrally adjudicated results for stroke events from the estrogen-alone substudy, after an average follow-up of 7.1 years, reported no significant difference in distribution of stroke subtype or severity, including fatal strokes, in women receiving CE-alone compared to placebo. Estrogen-alone increased the risk of ischemic stroke, and this excess was present in all subgroups of women examined (see Table 4).
Timing of the initiation of estrogen therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen-alone substudy stratified by age showed in women 50-59 years of age, a non-significant trend toward reduced risk for CHD [HR 0.63 (95 percent CI 0.36-1.09) and overall mortality [HR 0.71 (95 percent CI 0.46-1.11)].
WHI Estrogen Plus Progestin Substudy
The WHI estrogen plus progestin substudy was also stopped early. According to the predefined stopping rule, after an average follow-up of 5.6 years of treatment, the increased risk of breast cancer and cardiovascular events exceeded the specified benefits included in the “global index”. The absolute excess risk of events included in the “global index” was 19 per 10,000 women-years.
For those outcomes included in the WHI “global index” that reached statistical significance after 5.6 years of follow-up, the absolute excess risks per 10,000 women-years in the group treated with CE plus MPA were 7 more CHD events, 8 more strokes, 10 more PEs, and 8 more invasive breast cancers, while the absolute risk reductions per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures.
Results of the estrogen plus progestin substudy, which included 16,608 women (average 63 years of age, range 50 to 79; 83.9 percent White, 6.8 percent Black, 5.4 percent Hispanic, 3.9 percent Other) are presented in Table 5. These results reflect centrally adjudicated data after an average follow-up of 5.6 years.
|
Event |
Relative Risk CE/MPA vs Placebo (95% nCI†) |
CE/MPA n = 8,506 Absolute Risk Women - |
Placebo n = 8,102 per 10,000 Years |
| CHD events |
1.23 (0.99 - 1.53) |
41 |
34 |
| Non-fatal MI † | 1.28 (1.00 - 1.63) |
31
|
25
|
| CHD death | 1.10 (0.70 - 1.75) |
8
|
8
|
| All strokes |
1.31 (1.03 - 1.68) |
33 |
25 |
| Ischemic Stroke |
1.44 (1.09 - 1.90)
|
26
|
18
|
| Deep vein thrombosis‡ | 1.95 (1.43 - 2.67) |
26 |
13 |
| Pulmonary embolism | 2.13 (1.45 - 3.11) |
18 |
8 |
| Invasive breast cancer§ | 1.24 (1.01 - 1.54) |
41 |
33 |
| Colorectal cancer | 0.61 (0.42 - 0.87) |
10 |
16 |
| Endometrial cancer‡ | 0.81 (0.48 - 1.36) |
6 |
7 |
| Cervical cancer‡ | 1.44 (0.47 - 4.42) |
2 |
1 |
| Hip fracture† | 0.67 (0.47 - 0.96) |
11 |
16 |
| Vertebral fractures‡ | 0.65 (0.46 - 0.92) |
11 |
17 |
| Lower arm/wrist fractures‡ | 0.71 (0.59 - 0.85) |
44 |
62 |
| Total fractures‡ | 0.76 (0.69 - 0.83) |
152 |
199 |
| Overall Mortality‡ , ¶ | 1.00 (0.83 - 1.19) |
52 |
52 |
| Global Index# | 1.13 (1.02 - 1.25) |
184 |
165 |
†
‡
§
¶
#
Timing of the initiation of estrogen therapy relative to the start of menopause may affect the overall risk benefit profile. The WHI estrogen plus progestin substudy stratified by age showed in women 50-59 years of age, a non-significant trend toward reduced risk for overall mortality [HR 0.69 (95 percent CI 0.44-1.07)].
The estrogen-alone Women's Health Initiative Memory Study (WHIMS), an ancillary study of WHI, enrolled 2,947 predominantly healthy hysterectomized postmenopausal women 65 years to 79 years of age and older (45 percent, age 65 to 69 years; 36 percent, 70 to 74 years; 19 percent, 75 years of age and older) to evaluate the effects of daily CE (0.625 mg) on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 5.2 years, the relative risk of probable dementia for CE-alone versus placebo was 1.49 (95 percent CI 0.83–2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years. Probable dementia as defined in this study included Alzheimer’s disease (AD), vascular dementia (VaD) and
mixed types (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and the placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women. (See BOXED WARNINGS , WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .)
The WHIMS estrogen plus progestin ancillary study enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47 percent were age 65 to 69 years of age; 35 percent were 70 to 74 years of age; and 18 percent 75 years of age and older) to evaluate the effects of daily CE (0.625 mg) plus MPA (2.5 mg) on the incidence of probable dementia (primary outcome) compared to placebo.
After an average follow-up of 4 years, the relative risk of probable dementia for CE (0.625 mg) plus MPA (2.5 mg) versus placebo was 2.05 (95 percent CI, 1.21 to 3.48). The absolute risk of probable dementia for CE (0.625 mg) plus MPA (2.5 mg) versus placebo was 45 versus 22 per 10,000 women-years. Probable dementia as defined in this study included Alzheimer’s disease (AD), vascular dementia (VaD) and mixed types (having features of both AD and VaD). The most common classification of probable dementia in the treatment group and placebo group was AD. Since the ancillary study was conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women. (See BOXED WARNINGS , WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .)
When data from the two populations were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95 percent CI 1.19-2.60). Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women. (See BOXED WARNINGS , WARNINGS, Dementia and PRECAUTIONS, Geriatric Use .)
FEMRING INDICATIONS AND USAGE
Femring therapy is indicated in the:
1. Treatment of moderate to severe vasomotor symptoms due to menopause.
2. Treatment of moderate to severe vulvar and vaginal atrophy due to menopause.
FEMRING CONTRAINDICATIONS
Femring should not be used in women with any of the following conditions:
- Undiagnosed abnormal genital bleeding.
- Known, suspected, or history of breast cancer.
- Known or suspected estrogen-dependent neoplasia.
- Active deep vein thrombosis, pulmonary embolism or history of these conditions.
- Active arterial thromboembolic disease (for example, stroke and myocardial infarction) or a history of these conditions.
- Known liver dysfunction or disease.
- Known or suspected pregnancy.
WARNINGS
See BOXED WARNINGS
Femring is used only in the vagina, however, the risks associated with oral estrogens should be taken into account.
An increased risk of stroke and deep vein thrombosis (DVT) has been reported with estrogen-alone therapy. An increased risk of pulmonary embolism, DVT, stroke, and myocardial infarction has been reported with estrogen plus progestin therapy. Should any of these events occur or be suspected, estrogens with or without progestins should be discontinued immediately.
Risk factors for arterial vascular disease (for example, hypertension, diabetes mellitus, tobacco use, hypercholesterolemia and obesity) and/or venous thromboembolism (for example, personal history or family history of VTE, obesity and systemic lupus erythematosus) should be managed appropriately.
a. StrokeIn the Women's Health Initiative (WHI) estrogen-alone substudy, a statistically significant increased risk of stroke was reported in women 50 to 79 years of age receiving daily conjugated estrogens CE (0.625 mg) compared to women of the same age receiving placebo (45 versus 33 per 10,000 women-years). The increase in risk was demonstrated in year one and persisted. (See CLINICAL STUDIES .) Should a stroke occur or be suspected, estrogens should be discontinued immediately.
Sub-group analyses of women 50 to 59 years of age suggest no increased risk of stroke for those women receiving CE (0.625 mg) versus those receiving placebo (18 versus 21 per 10,000 women-years).
In the WHI estrogen plus progestin substudy, a statistically significant increased risk of stroke was reported in all women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to placebo (33 versus 25 per 10,000 women-years). The increase in risk was demonstrated after the first year and persisted. (See CLINICAL STUDIES .)
b. Coronary heart diseaseIn the WHI estrogen-alone substudy, no overall effect on coronary heart disease (CHD) events (defined as nonfatal myocardial infarction [MI], silent MI, or CHD death) was reported in women receiving estrogen-alone compared to placebo. (See CLINICAL STUDIES .)
Subgroup analyses of women 50 to 59 years of age suggest a statistically non-significant reduction in CHD events (CE 0.625 mg compared to placebo) in women with less than 10 years since menopause (8 versus 16 per 10,000 women-years).
In the WHI estrogen plus progestin substudy, there was a statistically non-significant increased risk of CHD events in women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (41 versus 34 per 10,000 women-years). An increase in relative risk was demonstrated in year 1, and a trend toward decreasing relative risk was reported in years 2 through 5.
In postmenopausal women with documented heart disease (n = 2,763, average age 66.7 years), in a controlled clinical trial of secondary prevention of cardiovascular disease (Heart and Estrogen/Progestin Replacement Study; HERS), treatment with daily CE (0.625 mg) plus MPA (2.5 mg) demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE plus MPA did not reduce the overall rate of CHD events in postmenopausal women with established coronary heart disease. There were more CHD events in the CE plus MPA-treated group than in the placebo group in year 1, but not during the subsequent years. Two thousand three hundred and twenty one (2,321) women from the original HERS trial agreed to participate in an open-label extension of HERS, HERS II. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE/MPA group and the placebo group in the HERS, the HERS II, and overall.
c. Venous thromboembolism (VTE)In the WHI estrogen-alone substudy, the risk of VTE (DVT and pulmonary embolism [PE]), was increased for women receiving daily CE (0.625 mg) compared to placebo (30 versus 22 per 10,000 women-years), although only the increased risk of DVT reached statistical significance (23 versus 15 per 10,000 women-years). The increase in VTE risk was demonstrated during the first 2 years. (See CLINICAL STUDIES .) Should a VTE occur or be suspected, estrogens should be discontinued immediately.
In the WHI estrogen plus progestin substudy, a statistically significant 2-fold greater rate of VTE was reported in women receiving daily CE (0.625 mg) plus MPA (2.5 mg) compared to women receiving placebo (35 versus 17 per 10,000 women-years). Statistically significant increases in risk for both DVT (26 versus 13 per 10,000 women-years) and PE (18 versus 8 per 10,000 women-years) were also demonstrated. The increase in VTE risk was observed during the first year and persisted. (See CLINICAL STUDIES .) Should a VTE occur or be suspected, estrogens should be discontinued immediately.
If feasible, estrogens should be discontinued at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism or during periods of prolonged immobilization.
a. Endometrial cancerAn increased risk of endometrial cancer has been reported with the use of unopposed estrogen therapy in a woman with a uterus. The reported endometrial cancer risk among unopposed estrogen users is about 2- to 12-fold greater than in nonusers, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than one year. The greatest risk appears associated with prolonged use, with increased risks of 15- to 24-fold for five to ten years or more, and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
Clinical surveillance of all women using estrogen-alone or estrogen plus progestin therapy is important. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal genital bleeding.
There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
b. Breast cancerThe most important randomized clinical trial providing information about breast cancer in estrogen-alone users is the Women’s Health Initiative (WHI) substudy of daily CE (0.625 mg). In the WHI estrogen-alone substudy, after an average of 7.1 years of follow-up, daily CE (0.625 mg) was not associated with an increased risk of invasive breast cancer (relative risk [RR] 0.80). (See CLINICAL STUDIES .)
The most important clinical trial providing information about breast cancer in estrogen plus progestin users is the WHI substudy of daily CE (0.625 mg) plus MPA (2.5 mg). After a mean follow-up of 5.6 years, the estrogen plus progestin substudy reported an increased risk of breast cancer in women who took daily CE plus MPA. In this substudy, prior use of estrogen-alone or estrogen plus progestin therapy was reported by 26 percent of the women. The relative risk of invasive breast cancer was 1.24, and the absolute risk was 41 versus 33 cases per 10,000 women-years for estrogen plus progestin compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86 and the absolute risk was 46 versus 25 cases per 10,000 women-years for estrogen plus progestin compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 versus 36 cases per 10,000 women-years for estrogen plus progestin compared with placebo. In the same substudy, invasive breast cancers were larger and diagnosed at a more advanced stage in the CE (0.625 mg) plus MPA (2.5 mg) group compared with the placebo group. Metastatic disease was rare with no apparent difference between the two groups. Other prognostic factors, such as histologic subtype, grade and hormone receptor status did not differ between the groups. (See CLINICAL STUDIES .)
Consistent with the WHI clinical trial, observational studies have also reported an increased risk of breast cancer for estrogen plus progestin therapy, and a smaller increased risk for estrogen-alone therapy, after several years of use. The risk increased with duration of use, and appeared to return to baseline over about 5 years after stopping treatment (only the observational studies have substantial data on risk after stopping). Observational studies also suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen plus progestin therapy as compared to estrogen-alone therapy. However, these studies have not generally found significant variation in the risk of breast cancer among different estrogens or among different estrogen plus progestin combinations, doses, or routes of administration.
The use of estrogen-alone and estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation.
All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors and prior mammogram results.
c. Ovarian cancerThe WHI estrogen plus progestin substudy reported a statistically non-significant increased risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE plus MPA versus placebo was 1.58 (95 percent nCI 0.77-3.24). The absolute risk for CE plus MPA versus placebo was 4 versus 3 cases per 10,000 women-years. In some epidemiologic studies, the use of estrogen-only products, in particular for 5 or more years, has been associated with an increased risk of ovarian cancer. However, the duration of exposure associated with increased risk is not consistent across all epidemiologic studies and some report no association.
In the estrogen-alone Women's Health Initiative Memory Study (WHIMS), an ancillary study of WHI, a population of 2,947 hysterectomized women 65 to 79 years of age was randomized to daily CE (0.625 mg) or placebo. In the WHIMS estrogen plus progestin ancillary study, a population of 4,532 postmenopausal women 65 to 79 years of age was randomized to daily CE (0.625 mg) plus MPA (2.5 mg) or placebo.
In the WHIMS estrogen-alone ancillary study, after an average follow-up of 5.2 years, 28 women in the estrogen-alone group and 19 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE-alone versus placebo was 1.49 (95 percent nCI 0.83-2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years. (See CLINICAL STUDIES and PRECAUTIONS, Geriatric Use .)
In the WHIMS estrogen plus progestin ancillary study, after an average follow-up of 4 years, 40 women in the CE plus MPA group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95 percent nCI 1.21-3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 versus 22 cases per 10,000 women-years. (See CLINICAL STUDIES and PRECAUTIONS, Geriatric Use .)
When data from the two populations were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95 percent nCI 1.19-2.60). Since both substudies were conducted in women aged 65 to 79 years, it is unknown whether these findings apply to younger postmenopausal women. (See BOXED WARNINGS and PRECAUTIONS, Geriatric Use .)
A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
Estrogen administration may lead to severe hypercalcemia in women with breast cancer and bone metastases. If hypercalcemia occurs, use of the drug should be stopped and appropriate measures taken to reduce the serum calcium level.
Retinal vascular thrombosis has been reported in women receiving estrogens. Discontinue medication pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, estrogens should be permanently discontinued.
PRECAUTIONS
1. Addition of a progestin when a woman has not had a hysterectomy
Studies of the addition of a progestin for 10 or more days of a cycle of estrogen administration, or daily with estrogen in a continuous regimen, have reported a lowered incidence of endometrial hyperplasia than would be induced by estrogen treatment alone. Endometrial hyperplasia may be a precursor to endometrial cancer.
There are, however, possible risks that may be associated with the use of progestins with estrogens compared to estrogen-alone regimens. These include an increased risk of breast cancer.
2. Elevated blood pressure
In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen.
3. Hypertriglyceridemia
In patients with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis. Consider discontinuation of treatment if pancreatitis develops.
4. Hepatic impairment and/or a past history of cholestatic jaundice
Estrogens may be poorly metabolized in women with impaired liver function. For women with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, caution should be exercised and in the case of recurrence, medication should be discontinued.
5. Hypothyroidism
Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Women with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Women dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. These women should have their thyroid function monitored in order to maintain their free thyroid hormone levels in an acceptable range.
6. Fluid retention
Estrogens may cause some degree of fluid retention. Women with conditions that might be influenced by this factor, such as cardiac or renal dysfunction, warrant careful observation when estrogens are prescribed.
7. Hypocalcemia
Estrogens should be used with caution in women with hypoparathyroidism as estrogen-induced hypocalcemia may occur.
8. Exacerbation of endometriosis
A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen-alone therapy. For women known to have residual endometriosis post-hysterectomy, the addition of progestin should be considered.
9. Exacerbation of other conditions
Estrogen therapy may cause an exacerbation of asthma, diabetes mellitus, epilepsy, migraine, porphyria, systemic lupus erythematosus and hepatic hemangiomas, and should be used with caution in women with these conditions.
10. Vaginal use and expulsion
Femring may not be suitable for women with conditions that make the vagina more susceptible to vaginal irritation or ulceration, or make expulsions more likely, such as narrow vagina, vaginal stenosis, vaginal infection, cervical prolapse, rectoceles and cystoceles. If local treatment of a vaginal infection is required, Femring can remain in place during treatment.
Physicians are advised to discuss the PATIENT INFORMATION leaflet with patients for whom they prescribe Femring.
Serum follicle stimulating hormone and estradiol levels have not been shown to be useful in the management of moderate to severe symptoms of vulvar and vaginal atrophy.
- Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII-X complex, II-VII-X complex, and beta-thromboglobulin; decreased levels of antifactor Xa and antithrombin III, decreased antithrombin III activity; increased levels of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
- Increased thyroid-binding globulin (TBG) levels leading to increased circulating total thyroid hormone levels as measured by protein-bound iodine (PBI), T4 levels (by column or by radioimmunoassay) or T3 levels by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Women on thyroid replacement therapy may require higher doses of thyroid hormone.
- Other binding proteins may be elevated in serum, for example, corticosteroid binding globulin (CBG), sex hormone binding globulin (SHBG)) leading to increased total circulating corticosteroids and sex steroids, respectively. Free hormone concentrations, such as testosterone and estradiol, may be decreased. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-1-antitrypsin, ceruloplasmin).
- Increased plasma HDL and HDL2 cholesterol subfraction concentrations, reduced LDL cholesterol concentration, increased triglycerides levels.
- Impaired glucose tolerance.
Long-term continuous administration of natural and synthetic estrogens in certain animal species increases the frequency of carcinomas of the breast, uterus, cervix, vagina, testis, and liver.
Estradiol acetate was assayed for mutation in four histidine-requiring strains of Salmonella typhimurium and in two tryptophan-requiring strains of Escherichia coli. Estradiol acetate did not induce mutation in any of the bacterial strains tested under the conditions employed.
Femring should not be used during pregnancy. (See CONTRAINDICATIONS .)
There appears to be little or no increased risk of birth defects in children born to women who have used estrogens and progestins as an oral contraceptive inadvertently during early pregnancy.
Femring should not be used during lactation. Estrogen administration to nursing mothers has been shown to decrease the quantity and quality of the breast milk. Detectable amounts of estrogens have been identified in the milk of mothers receiving estrogens.
Femring is not indicated in children. Clinical studies have not been conducted in the pediatric population.
There have not been sufficient numbers of geriatric women involved in clinical studies utilizing Femring to determine whether those over 65 years of age differ from younger subjects in their response to Femring.
The Women’s Health Initiative Study
In the Women's Health Initiative (WHI) estrogen-alone substudy (daily conjugated estrogens 0.625 mg versus placebo), there was a higher relative risk of stroke in women greater than 65 years of age.
In the WHI estrogen plus progestin substudy, there was a higher relative risk of nonfatal stroke and invasive breast cancer in women greater than 65 years of age.
The Women’s Health Initiative Memory Study
In the Women’s Health Initiative Memory Study (WHIMS) of postmenopausal women 65 to 79 years of age, there was an increased risk of developing probable dementia in the estrogen-alone and the estrogen plus progestin groups when compared to placebo.
Since both substudies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women.
FEMRING ADVERSE REACTIONS
See BOXED WARNINGS, WARNINGS and PRECAUTIONS.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a 13-week clinical trial that included 225 postmenopausal women treated with Femring and 108 women treated with placebo vaginal rings, adverse events that occurred at a rate of ≥ 2 percent are summarized in Table 6.
|
Adverse Event |
Placebo (n = 108) |
Estradiol 0.05 mg/day (n = 113) |
Estradiol 0.10 mg/day (n = 112) |
|
|
n (%) |
n (%) |
n (%) |
| Headache (NOS) |
10 (9.3) |
8 (7.1) |
11 (9.8) |
| Intermenstrual Bleeding |
2 (1.9) |
9 (8.0) |
11 (9.8) |
| Vaginal Candidiasis |
3 (2.8) |
7 (6.2) |
12 (10.7) |
| Breast Tenderness |
2 (1.9) |
7 (6.2) |
12 (10.7) |
| Back Pain |
4 (3.7) |
7 (6.2) |
4 (3.6) |
| Genital Disorder Femal (NOS) |
9 (8.3) |
3 (2.7) |
3 (2.7) |
| Upper Respiratory Tract Infection (NOS) |
6 (5.6) |
5 (4.4) |
4 (3.6) |
| Abdominal Distension |
3 (2.8) |
8 (7.1) |
3 (2.7) |
| Vaginal discharge |
9 (8.3) |
2 (1.8) |
3 (2.7) |
| Vulvovaginitis (NOS) |
7 (6.5) |
6 (5.3) |
1 (0.9) |
| Nausea |
5 (4.6) |
3 (2.7) |
2 (1.8) |
| Arthralgia |
4 (3.7) |
2 (1.8) |
2 (1.8) |
| Sinusitis (NOS) |
2 (1.9) |
2 (1.8) |
4 (3.6) |
| Uterine Pain |
1 (0.9) |
2 (1.8) |
5 (4.5) |
| Nasopharyngitis |
3 (2.8) |
2 (1.8) |
2 (1.8) |
| Pain in Limb |
3 (2.8) |
1 (0.9) |
3 (2.7) |
| Urinary Tract Infection (NOS) |
2 (1.9) |
1 (0.9) |
4 (3.6) |
| Vaginal Irritation |
4 (3.7) |
1 (0.9) |
2 (1.8) |
- A few cases of toxic shock syndrome (TSS) have been reported in women using vaginal rings. TSS is a rare, but serious disease that may cause death. Warning signs of TSS include fever, nausea, vomiting, diarrhea, muscle pain, dizziness, faintness, or a sunburn-rash on face and body.
- A few cases of ring adherence to the vaginal or bladder wall, making ring removal difficult, have been reported in women using vaginal rings. Patients should be carefully evaluated for vaginal or bladder wall ulceration or erosion. If an ulceration or erosion has occurred, consideration should be given to leaving the ring out and not replacing it until healing is complete to prevent the ring from adhering to the vaginal tissue.
- A few cases of bowel obstruction associated with vaginal ring use have been reported. Persistent abdominal complaints consistent with obstruction should be carefully evaluated.
- A few cases of inadvertent ring insertion into the urinary bladder, which may require surgical removal, have been reported for women using vaginal rings. Persistent unexplained urinary symptoms should be carefully evaluated.
The following additional adverse reactions have been identified during post-approval use of Femring. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
1. Genitourinary system
Uterine cancer, vaginal hemorrhage, ovarian cyst, irregular menstruation, metrorrhagia, menorrhagia, dysmenorrhea, uterine enlargement.
2. Breasts
Breast cancer, fibrocystic breast disease, breast disorder, breast mass, breast enlargement, breast pain, nipple pain, breast discharge.
3. Cardiovascular
Chest pain, increased blood pressure, irregular heart rate, pulmonary embolism, cerebrovascular accident (stroke), hemiparesis, transient ischemic attack, thrombosis.
4. Gastrointestinal
Abdominal pain, pancreatitis, cholecystitis, cholelithiasis, vomiting.
5. Skin
Generalized erythema, erythema multiforme, erythema nodosum, rash, hirsutism, pruritis.
6. Eyes
Blindness, contact lens intolerance.
7. Central Nervous System
Dizziness, headache, depression, nervousness, mood disturbances, irritability.
8. Miscellaneous
Medical device complication, back pain, angioedema, weight increased/decreased, edema, libido increased/decreased, urticaria, hypersensitivity, anaphylaxis.
OVERDOSAGE
Overdosage of estrogen may cause nausea and vomiting, breast tenderness, dizziness, abdominal pain, drowsiness/fatigue and withdrawal bleeding may occur in women. Treatment of overdose consists of discontinuation of Femring with institution of appropriate symptomatic care.
FEMRING DOSAGE AND ADMINISTRATION
Generally, when estrogen is prescribed for a postmenopausal woman with a uterus, a progestin should also be considered to reduce the risk of endometrial cancer. A woman without a uterus does not need a progestin. In some cases, however, hysterectomized women with a history of endometriosis may need a progestin.
Use of estrogen-alone, or in combination with a progestin, should be with the lowest effective dose and for the shortest duration consistent with treatment goals and risks for the individual woman. Postmenopausal women should be re-evaluated periodically as clinically appropriate to determine if treatment is still necessary. (See BOXED WARNINGS and WARNINGS .)
Two doses of Femring are available, 0.05 mg/day and 0.10 mg/day, for the treatment of moderate to severe vasomotor symptoms and/or vulvar and vaginal atrophy due to menopause.
Patients should be started at the lowest dose. The lowest effective dose of Femring has not been determined.
Hands should be thoroughly washed before and after ring insertion.
Femring Insertion
Insert upon removal from the protective pouch.
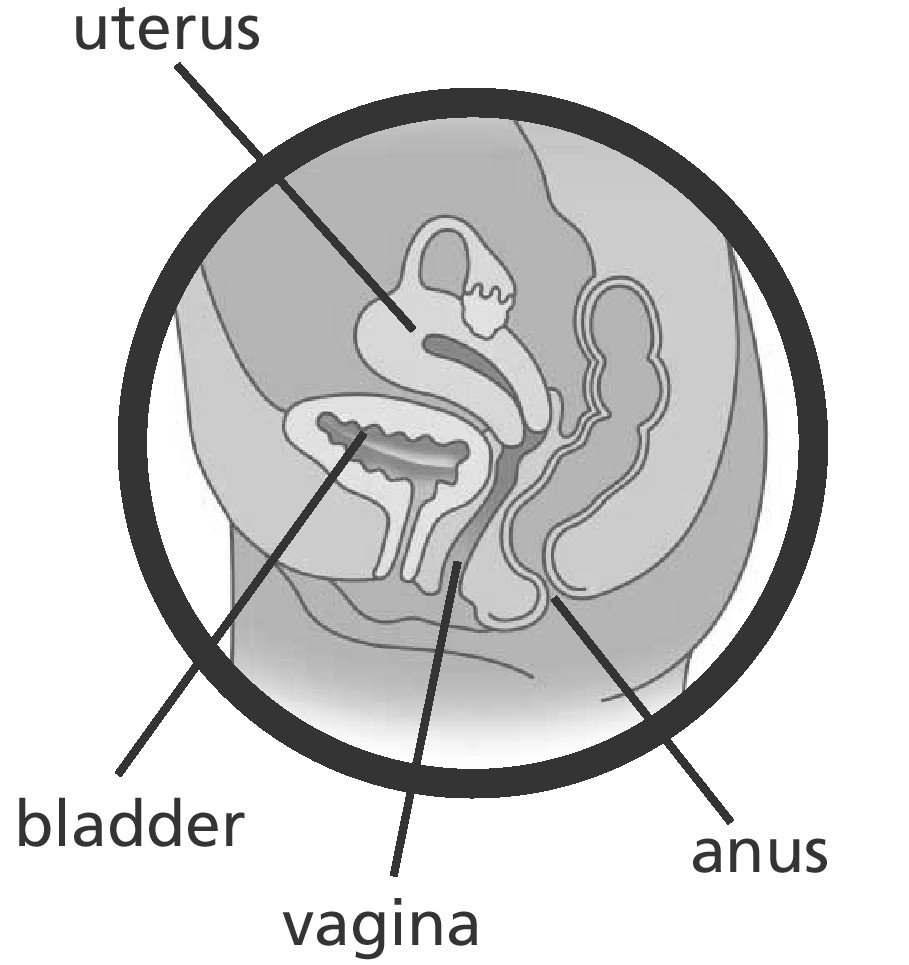
The opposite sides of the vaginal ring should be pressed together and inserted into the vagina. The exact position is not critical to its function. When Femring is in place, the patient should not feel anything. If the patient feels discomfort, the vaginal ring is probably not far enough inside the vagina. Gently push Femring further into the vagina.
Femring Use
Femring should remain in place for 3 months and then be replaced by a new Femring.
The patient should not feel Femring when it is in place and it should not interfere with sexual intercourse. Straining upon bowel movement may make Femring move down in the lower part of the vagina. If so, it may be repositioned with a finger.
If Femring is expelled totally from the vagina, it should be rinsed in lukewarm water and reinserted by the patient (or healthcare provider if necessary).
Femring Removal
Femring may be removed by looping a finger through the ring and pulling it out.
For patient instructions, see PATIENT INFORMATION .
HOW SUPPLIED
Each Femring® (estradiol acetate vaginal ring) is individually packaged in a pouch consisting of one side medical grade paper and the other side polyester/polyethylene laminate.
NDC 54868-6030-0 Femring® 0.10 mg/day (estradiol acetate vaginal ring) is available in single units.
Relabeling of "Additional Barcode" by
Physicians Total Care, Inc.
Tulsa, OK 74146
STORAGE
Store at 25˚ C (77˚ F); excursions permitted to 15˚ - 30˚ C (59˚ - 86˚ F) [see USP Controlled Room Temperature].
Femring® (estradiol acetate vaginal ring)
Read this PATIENT INFORMATION before you start using Femring and read what you get each time you refill your Femring prescription. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about Femring (an estrogen product)?
- Using estrogen-alone therapy increases your chance of getting cancer of the uterus (womb).
Report any unusual vaginal bleeding right away while you are using Femring. Vaginal bleeding after menopause may be a warning sign of cancer of the uterus (womb). Your healthcare provider should check any unusual vaginal bleeding to find out the cause.
- Do not use estrogen-alone therapy to prevent heart disease, heart attacks or dementia (decline of brain function).
- Using estrogen-alone therapy may increase your chances of getting strokes or blood clots.
- Using estrogen-alone therapy may increase your chance of getting dementia, based on a study of women age 65 or older.
- Do not use estrogens with progestins to prevent heart disease, heart attacks, or dementia.
- Using estrogens with progestins may increase your chances of getting heart attacks, strokes, breast cancer, or blood clots.
- Using estrogens with progestins may increase your chance of getting dementia, based on a study of women age 65 years or older.
- You and your healthcare provider should talk regularly about whether you still need treatment with Femring.
What is Femring?
Femring (estradiol acetate vaginal ring) is an off-white, soft, flexible vaginal ring with a center that contains an estrogen. Femring should be removed after 90 days of continuous use. If continuation of therapy is indicated, a new flexible ring should be replaced.
What is Femring used for?
Femring is used after menopause to:
- reduce moderate to severe hot flashes
Estrogens are hormones made by a woman’s ovaries. The ovaries normally stop making estrogens when a woman is between 45 to 55 years old. This drop in body estrogen levels causes the "change of life" or menopause (the end of monthly menstrual periods). Sometimes, both ovaries are removed during an operation before natural menopause takes place. The sudden drop in estrogen levels causes "surgical menopause".
When the estrogen levels begin dropping, some women develop very uncomfortable symptoms, such as feelings of warmth in the face, neck, and chest, or sudden strong feelings of heat and sweating ("hot flashes" or "hot flushes"). In some women the symptoms are mild and they will not need estrogens. In other women, symptoms can be more severe. You and your healthcare provider should talk regularly about whether you still need treatment with Femring.
- treat menopausal changes in and around the vagina
You and your healthcare provider should talk regularly about whether you still need treatment with Femring to control these problems.
Who should not use Femring?
Do not start using Femring if you:
- Have unusual vaginal bleeding
-
Currently have or have had certain
cancers
Estrogens may increase the chances of getting certain types of cancers including cancer of the breast or uterus. If you have or had cancer, talk with your healthcare provider about whether you should use Femring. - Had a stroke or heart attack
- Currently have or have had blood clots
- Currently have or have had liver problems
- Are allergic to any of the ingredients in Femring. See the list of ingredients in Femring at the end of this leaflet.
- Think you may be pregnant
Tell your healthcare provider:
- If you have any unusual vaginal bleeding. Vaginal bleeding after menopause may be a warning sign of cancer of the uterus (womb). Your healthcare provider should check any unusual vaginal bleeding to find out the cause.
- About all of your medical problems. Your healthcare provider may need to check you more carefully if you have certain conditions, such as asthma (wheezing), epilepsy (seizures), diabetes, migraine, endometriosis, lupus, or problems with your heart, liver, thyroid, kidneys or have high calcium levels in your blood.
- About all the medicines you take. This includes prescription and nonprescription medicines, vitamins and herbal supplements. Some medicines may affect how Femring works. Femring may also affect how your other medicines work.
- If you are going to have surgery or will be on bed rest. You may need to stop taking estrogens.
- If you are breastfeeding. The hormone in Femring can pass into your milk.
How should I use Femring?
- Start at the lowest dose and talk to your healthcare provider about how well that dose is working for you.
- Estrogens should be used at the lowest dose possible for your treatment only as long as needed. The lowest effective dose of Femring has not been determined. You and your healthcare provider should talk regularly (for example, every 3 to 6 months) about the dose you are using and whether you still need treatment with Femring.
- Femring is inserted into your vagina by you or your healthcare provider.
- Femring should stay in your vagina for 3 months.
- After 3 months Femring should be removed and a new Femring should be inserted.
|
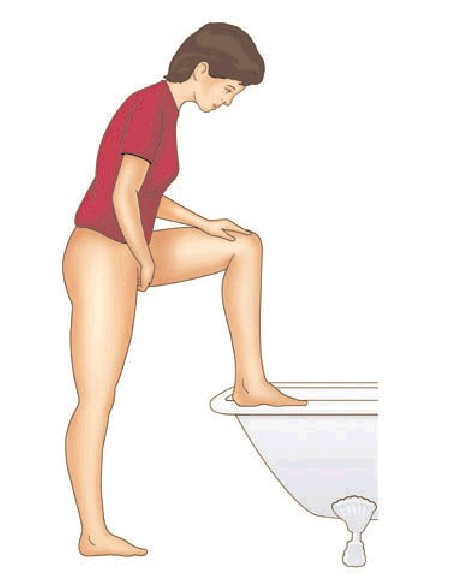
To insert Femring into your vagina:
|
|
| DIAGRAM 1a |
|
| DIAGRAM 1b |
| 4. Use your thumb and index finger (pointer finger) to press the sides of the ring together. You may find it easier to insert Femring if you twist it into a figure-of-eight shape (Diagram 2). |

|
| DIAGRAM 2 |
5. Use your other hand and hold open the folds of skin around your vagina
(Diagram 3).
|
|
DIAGRAM 3 |
|
6. Place the tip of the ring in the vaginal opening and then use your index finger to push the folded ring gently into your vagina. Push it up towards your lower back as far as you can (Diagram 4). |

|
| DIAGRAM 4 |
| If the ring feels uncomfortable, you probably did not push it into your vagina
far enough. Use your index finger to push the ring as far as you can into your
vagina (Diagram 5). There is no danger of Femring being
pushed too far up in the vagina or getting lost. |

|
| DIAGRAM 5 |
| Femring should now be in your upper vagina (Diagram 6). The exact position of Femring in the vagina is not important for it to work. |

|
| DIAGRAM 6 |
| 7. Wash your hands when you are done. |
|
After 3 months, Femring may no longer release enough medicine to control your menopausal symptoms. To continue to have symptom relief your current Femring should be removed and replaced with a new one if you and your healthcare provider have decided that you still need treatment with Femring. To remove Femring: 1. Wash and dry your hands. 2. Choose the position that is most comfortable for you (see Diagrams 1a and 1b). 3. Put a finger into your vagina and hook it through the ring. (Diagram 7). |

|
| DIAGRAM 7 |
|
4. Gently pull downwards and forwards to remove Femring. 5. Wrap the used ring in tissue or toilet paper and put it in a trash can. 6. Wash your hands. |
Insert another ring now if your healthcare provider has told you to.
If your Femring comes out of your vagina before 3 months, clean it with warm water and put it back in your vagina.
- Femring can come out if it is not put in far enough.
- Femring can come out when you are pushing hard during a bowel movement.
- Femring can come out if your vaginal muscles are weak.
If Femring comes out often, tell your healthcare provider. Femring may not be right for you.
Call your healthcare provider if you have any problems putting Femring in your vagina or taking it out.
You may leave Femring in place if you need to use medicine for a vaginal infection.
You may leave Femring in place during sex (intercourse). If you take Femring out during intercourse or it comes out, clean it with warm water and put it back in your vagina.
If you lose your Femring, a new Femring should be put in place for 3 months.
What are the possible side effects of vaginal rings?
A few cases of toxic shock syndrome (TSS) have been reported in women using vaginal rings. Toxic shock syndrome is a rare but serious illness caused by a bacterial infection. If you have fever, nausea, vomiting, diarrhea, muscle pain, dizziness, faintness, or a sunburn-rash on face and body, remove Femring and contact your healthcare provider. A few cases of a vaginal ring becoming attached to the vaginal wall, making ring removal difficult, have been reported. Rare cases of a vaginal ring being inserted into the bladder, instead of the vagina, also have been reported.
What are the possible side effects of estrogens?
Side effects are grouped by how serious they are and how often they happen when you are treated.
Serious but less common side effects include:
- Breast cancer
- Cancer of the uterus
- Stroke
- Heart attack
- Blood clots
- Dementia
- Gallbladder disease
- Ovarian cancer
- High blood pressure
- Liver problems
- High blood sugar
- Enlargement of benign tumors of the uterus (“fibroids”)
Some of the warning signs of serious side effects include:
- Breast lumps
- Unusual vaginal bleeding
- Dizziness and faintness
- Changes in speech
- Severe headaches
- Chest pain
- Shortness of breath
- Pains in your legs
- Changes in vision
- Vomiting
- Yellowing of the skin, eyes or nail beds
Call your healthcare provider right away if you get any of these warning signs or any other unusual symptom that concerns you.
Less serious but common side effects include:
- Headache
- Breast pain
- Irregular vaginal bleeding or spotting
- Stomach/abdominal cramps, bloating
- Nausea and vomiting
- Hair loss
- Fluid retention
- Vaginal yeast infection
- Reactions from inserting Femring such as burning, irritation, and itching
These are not all the possible side effects of Femring. For more information, ask your healthcare provider or pharmacist.
What can I do to lower my chances of getting a serious side effect with Femring?
- Talk with your healthcare provider regularly about whether you should continue using Femring.
- If you have a uterus, talk to your healthcare provider about whether the addition of a progestin is right for you. The addition of a progestin is generally recommended for a woman with a uterus to reduce the chance of getting cancer of the uterus. See your healthcare provider right away if you get vaginal bleeding while using Femring.
- If you have fever, nausea, vomiting, diarrhea, muscle pain, dizziness, faintness, or a sunburn-rash on face and body, remove Femring and contact your healthcare provider.
- Contact your healthcare provider right away if you have difficulty removing Femring.
- Have a pelvic exam, breast exam and mammogram (breast x-ray) every year unless your healthcare provider tells you something else. If members of your family have had breast cancer or if you have ever had breast lumps or an abnormal mammogram, you may need to have breast examinations more often.
- If you have high blood pressure, high cholesterol (fat in the blood), diabetes, are overweight, or if you use tobacco, you may have higher chances of getting heart disease. Ask your healthcare provider for ways to lower your chances for getting heart disease.
General information about safe and effective use of Femring.
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use Femring for conditions for which it was not prescribed. Do not give Femring to other people, even if they have the same symptoms you have. It may harm them.
Keep Femring out of the reach of children.
This leaflet provides a summary of the most important information about Femring. If you would like more information, talk with your healthcare provider or pharmacist. You can ask for information about Femring that is written for health professionals. You can get more information by calling the toll free number 800-521-8813.
What are the ingredients in Femring?
Femring contains estradiol acetate, an estrogen. It also contains cured silicone elastomer composed of dimethyl polysiloxane silanol, silica (diatomaceous earth), normal propyl orthosilicate, stannous octoate; and barium sulfate. There are no coloring agents in Femring.
Manufactured by: Warner Chilcott UK, Ltd., Larne, Northern Ireland, UK
Marketed by: Warner Chilcott (US), LLC, Rockaway, NJ 07866
1-800-521-8813
To report SUSPECTED ADVERSE REACTIONS, contact Warner Chilcott at 1-800-521-8813 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.

6201G071
REVISED September 2009
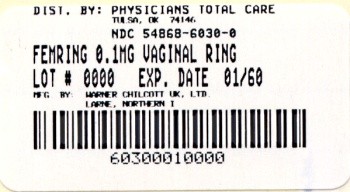
PRINCIPAL DISPLAY PANEL
Femring
(estradiol acetate vaginal ring)
0.10 mg/day
Rx ONLY
(Contains 24.8 mg estradiol acetate to deliver the equivalent of 0.10 mg estradiol per day for three months.)
Other ingredients: barium sulfate and cured elastomer.
Store at 25oC (77oF); excursions permitted to 15o - 30oC (59o - 86oF).
[see USP Controlled Room Temperature]
For intravaginal use only.
CONTENTS: 1 VAGINAL RING
Femringestradiol acetate RING
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||