Dexamethasone
Morton Grove Pharmaceuticals, Inc.
DEXAMETHASONE ELIXIR, USP (0.5 mg/5 mL)
FULL PRESCRIBING INFORMATION: CONTENTS*
- DEXAMETHASONE DESCRIPTION
- CLINICAL PHARMACOLOGY
- DEXAMETHASONE INDICATIONS AND USAGE
- DEXAMETHASONE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- DEXAMETHASONE ADVERSE REACTIONS
- OVERDOSAGE
- DEXAMETHASONE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
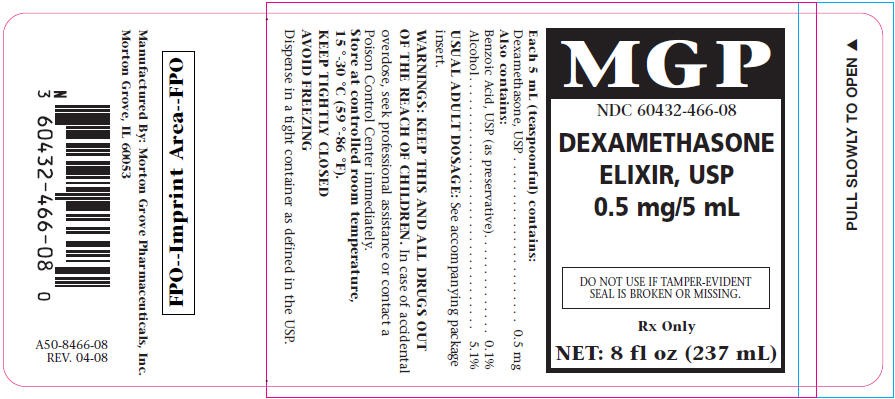
- PRINCIPAL DISPLAY PANEL - 237 mL Bottle Label
FULL PRESCRIBING INFORMATION
Rx only
DEXAMETHASONE DESCRIPTION
Each 5 mL (teaspoonful) contains:
Dexamethasone, USP 0.5 mg
Also contains:
Benzoic Acid, USP 0.1%
(as preservative)
Alcohol 5.1%
Inactive Ingredients: Artificial Raspberry Flavor; Citric Acid, USP; FD&C Red No. 40; Liquid Sugar; Propylene Glycol, USP and Purified Water, USP. It may also contain Sodium Citrate, USP.
Glucocorticoids are adrenocortical steroids, both naturally occurring and synthetic, which are readily absorbed from the gastrointestinal tract.
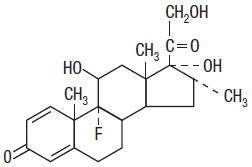
Dexamethasone, a synthetic adrenocortical steroid, is a white to practically white, odorless, crystalline powder. It is stable in air. It is practically insoluble in water. The molecular weight is 392.47. It is designated chemically as 9-fluoro-11β,17,21-trihydroxy-16α-methylpregna-1,4-diene-3,20-dione. The molecular formula is C22H29FO5 and the structural formula is:
CLINICAL PHARMACOLOGY
Naturally occurring glucocorticoids, (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, including dexamethasone, are primarily used for their potent antiinflammatory effects in disorders of many organ systems.
Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli.
At equipotent anti-inflammatory doses, dexamethasone almost completely lacks the sodium-retaining property of hydrocortisone and closely related derivatives of hydrocortisone.
DEXAMETHASONE INDICATIONS AND USAGE
-
Endocrine Disorders: Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance).
Congenital adrenal hyperplasia
Nonsuppurative thyroiditis
Hypercalcemia associated with cancer -
Rheumatic Disorders: As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Psoriatic arthritis
Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy)
Ankylosing spondylitis
Acute and subacute bursitis
Acute nonspecific tenosynovitis
Acute gouty arthritis
Post-traumatic osteoarthritis
Synovitis of osteoarthritis
Epicondylitis -
Collagen Diseases: During an exacerbation or as maintenance therapy in selected cases of:
Systemic lupus erythematosus
Acute rheumatic carditis -
Dermatologic Diseases:
Pemphigus
Bullous dermatitis herpetiformis
Severe erythema multiforme (Stevens-Johnson syndrome)
Exfoliative dermatitis
Mycosis fungoides
Severe psoriasis
Severe seborrheic dermatitis -
Allergic States: Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment:
Seasonal or perennial allergic rhinitis
Bronchial asthma
Contact dermatitis
Atopic dermatitis
Serum sickness
Drug hypersensitivity reactions -
Ophthalmic Diseases: Severe acute and chronic allergic and inflammatory processes involving the eye and its adnexa, such as:
Allergic conjunctivitis
Keratitis
Allergic corneal marginal ulcers
Herpes zoster ophthalmicus
Iritis and iridocyclitis
Chorioretinitis
Anterior segment inflammation
Diffuse posterior uveitis and choroiditis
Optic neuritis
Sympathetic ophthalmia -
Respiratory Diseases:
Symptomatic sarcoidosis
Loeffler's syndrome not manageable by other means
Berylliosis
Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy
Aspiration pneumonitis -
Hematologic Disorders:
Idiopathic thrombocytopenic purpura in adults
Secondary thrombocytopenia in adults
Acquired (autoimmune) hemolytic anemia
Erythroblastopenia (RBC anemia)
Congenital (erythroid) hypoplastic anemia -
Neoplastic Diseases: For palliative management of:
Leukemia and lymphomas in adults
Acute leukemia of childhood - Edematous States: To induce a diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus
-
Gastrointestinal Diseases: To tide the patient over a critical period of the disease in:
Ulcerative colitis
Regional enteritis -
Miscellaneous:
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy
Trichinosis with neurologic or myocardial involvement - Diagnostic testing of adrenocortical hyperfunction.
DEXAMETHASONE CONTRAINDICATIONS
-
-
WARNINGS
In patients on corticosteroid therapy subjected to unusual stress, increased dosage of rapidly acting corticosteroids before, during, and after the stressful situation is indicated.
Drug-induced secondary adrenocortical insufficiency may result from too rapid withdrawal of corticosteroids and may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. If the patient is receiving steroids already, dosage may have to be increased. Since mineralocorticoid secretion may be impaired, salt and/or a mineralocorticoid should be administered concurrently.
Corticosteroids may mask some signs of infection, and new infections may appear during their use. There may be decreased resistance and inability to localize infection when corticosteroids are used. Moreover, corticosteroids may affect the nitroblue-tetrazolium test for bacterial infection and produce false-negative results.
In cerebral malaria, a double-blind trial has shown that the use of corticosteroids is associated with prolongation of coma and a higher incidence of pneumonia and gastrointestinal bleeding.
Corticosteroids may activate latent amebiasis. Therefore, it is recommended that latent or active amebiasis be ruled out before initiating corticosteroid therapy in any patient who has spent time in the tropics or any patient with unexplained diarrhea.
Prolonged use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to fungi or viruses.
Usage in Pregnancy
Since adequate human reproduction studies have not been done with corticosteroids, use of these drugs in pregnancy or in women of childbearing potential requires that the anticipated benefits be weighed against the possible hazards to the mother and embryo or fetus. Infants born of mothers who have received substantial doses of corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Corticosteroids appear in breast milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other unwanted effects. Mothers taking pharmacologic doses of corticosteroids should be advised not to nurse.
Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Administration of live virus vaccines, including smallpox, is contraindicated in individuals receiving immunosuppressive doses of corticosteroids. If inactivated viral or bacterial vaccines are administered to individuals receiving immunosuppressive doses of corticosteroids, the expected serum antibody response may not be obtained. However, immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy, e.g., for Addison's disease.
Persons who are on drugs which suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have more serious or even fatal course in non-immune children or adults on corticosteroids. In such children or adults who have not had these diseases, particular care should be taken to avoid exposure. How the dose, route and duration of corticosteroid administration affects the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZlG) may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information.) If chickenpox develops, treatment with antiviral agents may be considered.
The use of Dexamethasone Elixir in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate antituberculous regimen.
If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary as reactivation of the disease may occur. During prolonged corticosteroid therapy, these patients should receive chemoprophylaxis.
Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
PRECAUTIONS
Following prolonged therapy, withdrawal of corticosteroids may result in symptoms of the corticosteroid withdrawal syndrome including fever, myalgia, arthralgia, and malaise. This may occur in patients even without evidence of adrenal insufficiency.
There is an enhanced effect of corticosteroids in patients with hypothyroidism and in those with cirrhosis.
Corticosteroids should be used cautiously in patients with ocular herpes simplex because of possible corneal perforation.
The lowest possible dose of corticosteroid should be used to control the condition under treatment, and when reduction in dosage is possible, the reduction should be gradual.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression, to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia.
Steroids should be used with caution in nonspecific ulcerative colitis, if there is a probability of impending perforation, abscess, or other pyogenic infection, diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, renal insufficiency, hypertension, osteoporosis and myasthenia gravis. Fat embolism has been reported as a possible complication of hypercortisonism.
When large doses are given, some authorities advise that corticosteroids be taken with meals and antacids taken between meals to help to prevent peptic ulcer.
Growth and development of infants and children on prolonged corticosteroid therapy should be carefully observed.
Steroids may increase or decrease motility and number of spermatozoa in some patients.
Phenytoin, phenobarbital, ephedrine, and rifampin may enhance the metabolic clearance of corticosteroids, resulting in decreased blood levels and lessened physiologic activity, thus requiring adjustment in corticosteroid dosage. These interactions may interfere with dexamethasone suppression tests which should be interpreted with caution during administration of these drugs.
False-negative results in the dexamethasone suppression test (DST) in patients being treated with indomethacin have been reported. Thus, results of the DST should be interpreted with caution in these patients.
The prothrombin time should be checked frequently in patients who are receiving corticosteroids and coumarin anticoagulants at the same time because of reports that corticosteroids have altered the response to these anticoagulants. Studies have shown that the usual effect produced by adding corticosteroids is inhibition of response to coumarins, although there have been some conflicting reports of potentiation not substantiated by studies.
When corticosteroids are administered concomitantly with potassium-depleting diuretics, patients should be observed closely for development of hypokalemia.
Information for Patients
Persons who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chickenpox or measles. Patients should also be advised that if they are exposed, medical advice should be sought without delay.
DEXAMETHASONE ADVERSE REACTIONS
Fluid and Electrolyte Disturbances:
-
-
-
-
-
-
Musculoskeletal:
-
-
-
-
-
-
-
-
Gastrointestinal:
-
-
-
-
-
Dermatologic:
-
-
-
-
-
-
-
Neurologic:
-
-
-
-
-
Endocrine:
-
-
-
-
-
-
-
-
Ophthalmic:
-
-
-
-
Metabolic:
-
Cardiovascular:
-
Other:
-
-
-
-
-
-
-
OVERDOSAGE
Reports of acute toxicity and/or death following overdosage of glucocorticoids are rare. In the event of overdosage, no specific antidote is available; treatment is supportive and symptomatic.
The oral LD50 of dexamethasone in female mice was 6.5 g/kg.
DEXAMETHASONE DOSAGE AND ADMINISTRATION
For oral administration: DOSAGE REQUIREMENTS ARE VARIABLE AND MUST BE INDIVIDUALIZED ON THE BASIS OF THE DISEASE AND THE RESPONSE OF THE PATIENT.
The initial dosage varies from 0.75 to 9 mg a day depending on the disease being treated. In less severe diseases doses lower than 0.75 mg may suffice, while in severe diseases doses higher than 9 mg may be required. The initial dosage should be maintained or adjusted until the patient's response is satisfactory. If satisfactory clinical response does not occur after a reasonable period of time, discontinue DEXAMETHASONE ELIXIR and transfer the patient to other therapy.
After a favorable initial response, the proper maintenance dosage should be determined by decreasing the initial dosage in small amounts to the lowest dosage that maintains an adequate clinical response.
Patients should be observed closely for signs that might require dosage adjustment, including changes in clinical status resulting from remissions or exacerbations of the disease, individual drug responsiveness, and the effect of stress (e.g., surgery, infection, trauma). During stress it may be necessary to increase dosage temporarily.
If the drug is to be stopped after more than a few days of treatment, it usually should be withdrawn gradually.
The following milligram equivalents facilitate changing to DEXAMETHASONE ELIXIR from other glucocorticoids:
| DEXAMETHASONE ELIXIR | METHYLPREDNI-SOLONE AND TRIAMCINOLONE | PREDNISOLONE AND PREDNISONE | HYDROCORTISONE | CORTISONE |
|---|---|---|---|---|
| 0.75 mg = | 4 mg = | 5 mg = | 20 mg = | 25 mg |
Dexamethasone suppression tests
- Tests for Cushing's syndrome.
Give 1 mg of Dexamethasone orally at 11:00 p.m. Blood is drawn for plasma cortisol determination at 8:00 a.m. the following morning.
For greater accuracy, give 0.5 mg of Dexamethasone orally every 6 hours for 48 hours. Twenty-four hour urine collections are made for determination of 17-hydroxycorticosteroid excretion. - Test to distinguish Cushing's syndrome due to pituitary ACTH excess from Cushing's syndrome due to other causes.
Give 2 mg of Dexamethasone orally every 6 hours for 48 hours. Twenty-four hour urine collections are made for determination of 17-hydroxycorticosteroid excretion.
HOW SUPPLIED
DEXAMETHASONE ELIXIR 0.5 mg/5 mL is supplied as a clear, red, raspberry-flavored liquid in the following sizes:
100 mL fill in a 4 fl oz bottle with separately packaged dropper assembly. Dropper graduated for 0.125 mg and 0.25 mg.
8 fl oz (No Dropper) (237 mL)
RECOMMENDED STORAGE
Store at controlled room temperature, 15 °–30 °C (59 °–86 °F).
KEEP TIGHTLY CLOSED
AVOID FREEZING
Dispense in a tight container as defined in the USP.
Rx Only
Product No.: 8466
Manufactured By: Morton Grove Pharmaceuticals, Inc.
Morton Grove, IL 60053
A50-8466-08 REV. 04-08
PRINCIPAL DISPLAY PANEL - 237 mL Bottle Label
MGP
NDC 60432-466-08
DEXAMETHASONE
ELIXIR, USP
0.5 mg/5 mL
DO NOT USE IF TAMPER-EVIDENT
SEAL IS BROKEN OR MISSING.
Rx Only
NET: 8 fl oz (237 mL)
DexamethasoneDexamethasone ELIXIR
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||