Warfarin Sodium
Lake Erie Medical DBA Quality Care Products LLC
Warfarin Sodium Tablets, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARFARIN SODIUM DESCRIPTION
- CLINICAL PHARMACOLOGY
- WARFARIN SODIUM INDICATIONS AND USAGE
- WARFARIN SODIUM CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- INFORMATION FOR PATIENTS
- PEDIATRIC USE
- GERIATRIC USE
- WARFARIN SODIUM ADVERSE REACTIONS
- OVERDOSAGE
- WARFARIN SODIUM DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- REFERENCES
- Image of 1mg Label
- Image of 2.5mg Label
- Image of 2mg Label
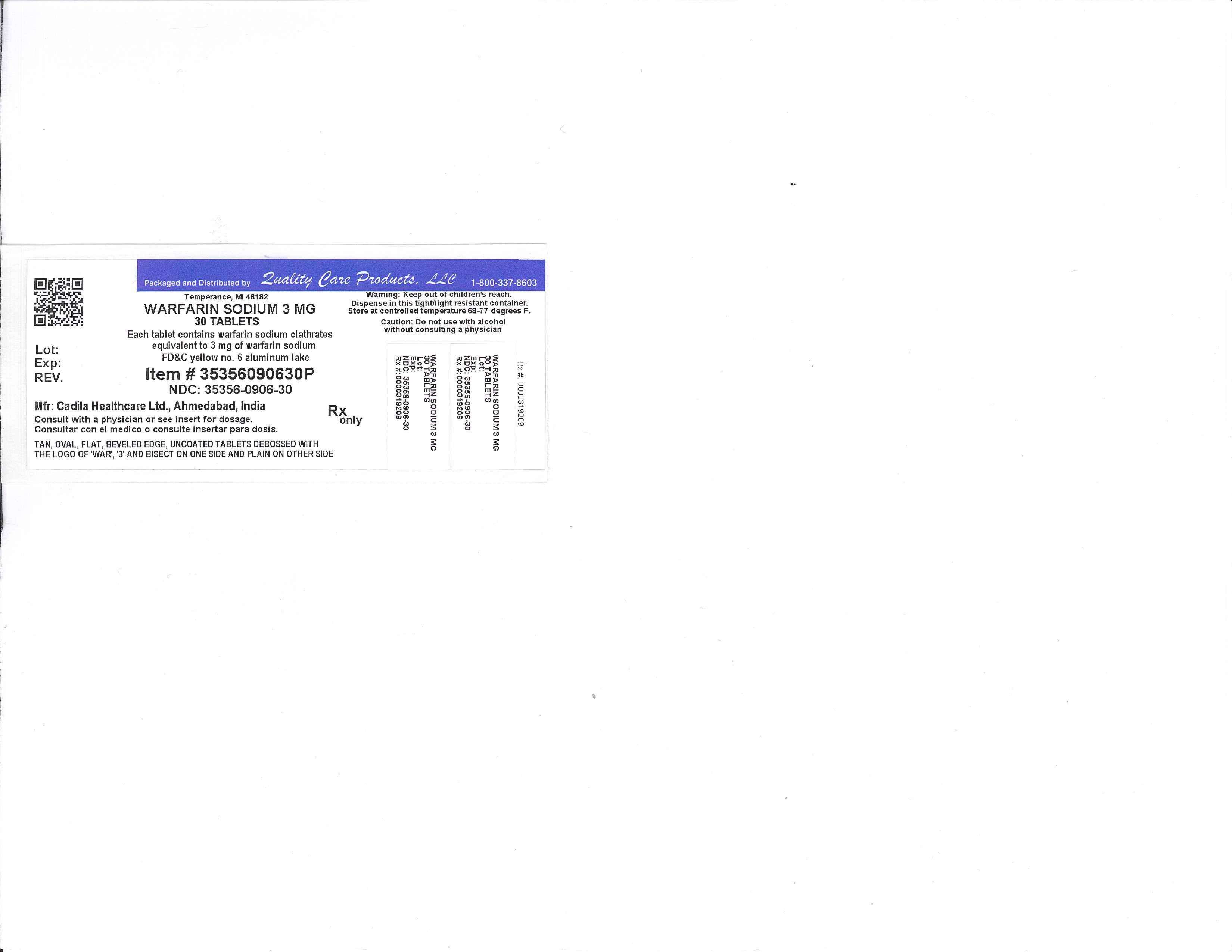
- Image of 3mg Label
FULL PRESCRIBING INFORMATION
Anticoagulant
WARNING: BLEEDING RISK
Warfarin sodium can cause major or fatal bleeding. Bleeding is more likely to occur during the starting period and with a higher dose (resulting in a higher INR). Risk factors for bleeding include high intensity of anticoagulation (INR >4.0), age ≥65, highly variable INRs, history of gastrointestinal bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, malignancy, trauma, renal insufficiency, concomitant drugs (see PRECAUTIONS ) and long duration of warfarin therapy. Regular monitoring of INR should be performed on all treated patients. Those at high risk of bleeding may benefit from more frequent INR monitoring, careful dose adjustment to desired INR, and a shorter duration of therapy. Patients should be instructed about prevention measures to minimize risk of bleeding and to report immediately to physicians signs and symptoms of bleeding (see PRECAUTIONS: Information for Patients ).
WARFARIN SODIUM DESCRIPTION
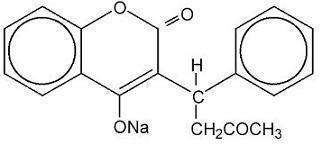
Warfarin sodium tablet (crystalline warfarin sodium) is an anticoagulant, which acts by inhibiting vitamin K-dependent coagulation factors. Chemically, it is 3-(α-acetonylbenzyl)-4-hydroxycoumarin and is a racemic mixture of the R- and S-enantiomers. Crystalline warfarin sodium is an isopropanol clathrate. The crystallization of warfarin sodium virtually eliminates trace impurities present in amorphous warfarin. Its molecular formula is C19H15NaO4, and its structural formula may be represented by the following:
Crystalline warfarin sodium occurs as a white crystalline powder, odorless or practically odorless.
Each warfarin sodium tablet intended for oral administration contains warfarin sodium clathrates equivalent to 1 mg or 2 mg or 2.5 mg or 3 mg or 4 mg or 5 mg or 6 mg or 7.5 mg or 10 mg of warfarin sodium. In addition each tablet contains the inactive ingredients hydroxypropyl cellulose, lactose monohydrate, magnesium stearate and pregelatinized starch. Additionally each 1 mg tablet contains D&C red no. 6 barium lake, 2 mg tablet contains FD&C blue no. 2 aluminum lake and FD&C red no. 40 aluminum lake, 2.5 mg tablet contains D&C yellow no. 10 aluminum lake and FD&C blue no. 1 aluminum lake, 3 mg tablet contains FD&C yellow no. 6 aluminum lake, FD&C blue no. 2 aluminum lake and FD&C red no. 40 aluminum lake, 4 mg tablet contains FD&C blue no. 1 aluminum lake, 5 mg tablet contains FD&C yellow no. 6 aluminum lake, 6 mg tablet contains FD&C yellow no. 6 aluminum lake and FD&C blue no. 1 aluminum lake, 7.5 mg tablet contains D&C yellow no. 10 aluminum lake and FD&C yellow no.6 aluminum lake and 10 mg tablet is dye free.
CLINICAL PHARMACOLOGY
Warfarin sodium tablets and other coumarin anticoagulants act by inhibiting the synthesis of vitamin K dependent clotting factors, which include Factors II, VII, IX and X, and the anticoagulant proteins C and S. Half-lives of these clotting factors are as follows: Factor II - 60 hours, VII - 4-6 hours, IX - 24 hours, and X - 48-72 hours. The half-lives of proteins C and S are approximately 8 hours and 30 hours, respectively. The resultant in vivo effect is a sequential depression of Factor VII, Protein C, Factor IX, Protein S, and Factor X and II activities. Vitamin K is an essential cofactor for the post ribosomal synthesis of the vitamin K dependent clotting factors. The vitamin promotes the biosynthesis of γ-carboxyglutamic acid residues in the proteins which are essential for biological activity.
Mechanism of Action
Warfarin is thought to interfere with clotting factor synthesis by inhibition of the C1 subunit of the vitamin K epoxide reductase (VKORC1) enzyme complex, thereby reducing the regeneration of vitamin K1 epoxide. The degree of depression is dependent upon the dosage administered and, in part, by the patient’s VKORC1 genotype. Therapeutic doses of warfarin decrease the total amount of the active form of each vitamin K dependent clotting factor made by the liver by approximately 30% to 50%.
An anticoagulation effect generally occurs within 24 hours after drug administration. However, peak anticoagulant effect may be delayed 72 to 96 hours. The duration of action of a single dose of racemic warfarin is 2 to 5 days. The effects of warfarin sodium tablets may become more pronounced as effects of daily maintenance doses overlap. Anticoagulants have no direct effect on an established thrombus, nor do they reverse ischemic tissue damage. However, once a thrombus has occurred, the goal of anticoagulant treatment is to prevent further extension of the formed clot and prevent secondary thromboembolic complications which may result in serious and possibly fatal sequelae.
Pharmacokinetics
Warfarin sodium is a racemic mixture of the R- and S-enantiomers. The S-enantiomer exhibits 2-5 times more anticoagulant activity than the R-enantiomer in humans, but generally has a more rapid clearance.
Absorption
Warfarin sodium tablet is essentially completely absorbed after oral administration with peak concentration generally attained within the first 4 hours.
Distribution
There are no differences in the apparent volumes of distribution after intravenous and oral administration of single doses of warfarin solution. Warfarin distributes into a relatively small apparent volume of distribution of about 0.14 liter/kg. A distribution phase lasting 6 to 12 hours is distinguishable after rapid intravenous or oral administration of an aqueous solution. Using a one compartment model, and assuming complete bioavailability, estimates of the volumes of distribution of R- and S-warfarin are similar to each other and to that of the racemate. Concentrations in fetal plasma approach the maternal values, but warfarin has not been found in human milk (see WARNINGS: Lactation ). Approximately 99% of the drug is bound to plasma proteins.
Metabolism
The elimination of warfarin is almost entirely by metabolism. Warfarin sodium tablets are stereoselectively metabolized by hepatic microsomal enzymes (cytochrome P-450) to inactive hydroxylated metabolites (predominant route) and by reductases to reduced metabolites (warfarin alcohols). The warfarin alcohols have minimal anticoagulant activity. The metabolites are principally excreted into the urine; and to a lesser extent into the bile. The metabolites of warfarin that have been identified include dehydrowarfarin, two diastereoisomer alcohols, 4'-, 6-, 7-, 8- and 10-hydroxywarfarin. The cytochrome P-450 isozymes involved in the metabolism of warfarin include 2C9, 2C19, 2C8, 2C18, 1A2, and 3A4. 2C9 is likely to be the principal form of human liver P-450 which modulates the in vivo anticoagulant activity of warfarin.
The S-enantiomer of warfarin is mainly metabolized to 7-hydroxywarfarin by CYP2C9, a polymorphic enzyme. The variant alleles CYP2C9*2 and CYP2C9*3 result in decreased in vitro CYP2C9 enzymatic 7-hydroxylation of S-warfarin. The frequencies of these allelles in Caucasians are approximately 11% and 7% for CYP2C9*2 and CYP2C9*3, respectively1. Patients with one or more of these variant CYP2C9 alleles have decreased S-warfarin clearance (Table 1).2
|
CYP2C9 Genotype |
N |
S-Warfarin Clearance/Lean Body Weight |
|
(mL/min/kg) |
||
|
Mean (SD) |
||
| *1/*1 | 118 | 0.065 (0.025) |
| *1/*2 or*1/*3 | 59 | 0.041 (0.021) |
| *2/*2, *2/*3or *3/*3 | 11 | 0.020 (0.011) |
| Total | 188 |
Other CYP2C9 alleles associated with reduced enzymatic activity occur at lower frequencies, including *5, *6, and *11 alleles in populations of African ancestry and *5, *9 and *11 alleles in Caucasians.
Pharmacogenomics
A meta-analysis of 9 qualified studies including 2775 patients (99% Caucasian) was performed to examine the clinical outcomes associated with CYP2C9 gene variants in warfarin-treated patients.3 In this meta-analysis, 3 studies assessed bleeding risks and 8 studies assessed daily dose requirements. The analysis suggested an increased bleeding risk for patients carrying either the CYP2C9*2 or CYP2C9*3 alleles. Patients carrying at least one copy of the CYP2C9*2 allele required a mean daily warfarin dose that was 17% less than the mean daily dose for patients homozygous for the CYP2C9*1 allele. For patients carrying at least one copy of the CYP2C9*3 allele, the mean daily warfarin dose was 37% less than the mean daily dose for patients homozygous for the CYP2C9*1 allele.
In an observational study, the risk of achieving INR >3 during the first 3 weeks of warfarin therapy was determined in 219 Swedish patients retrospectively grouped by CYP2C9 genotype. The relative risk of over anticoagulation as measured by INR >3 during the first 2 weeks of therapy was approximately doubled for those patients classified as *2 or *3 compared to patients who were homozygous for the *1 allele.4
Warfarin reduces the regeneration of vitamin K from vitamin K epoxide in the vitamin K cycle, through inhibition of vitamin K epoxide reductase (VKOR), a multiprotein enzyme complex. Certain single nucleotide polymorphisms in the VKORC1 gene (especially the -1639G>A allele) have been associated with lower dose requirements for warfarin. In 201 Caucasian patients treated with stable warfarin doses, genetic variations in the VKORC1 gene were associated with lower warfarin doses. In this study, about 30% of the variance in warfarin dose could be attributed to variations in the VKORC1 gene alone; about 40% of the variance in warfarin dose could be attributed to variations in VKORC1 and CYP2C9 genes combined.5 About 55% of the variability in warfarin dose could be explained by the combination of VKORC1 and CYP2C9 genotypes, age, height, body weight, interacting drugs, and indication for warfarin therapy in Caucasian patients.5 Similar observations have been reported in Asian patients.6,7
Excretion
The terminal half-life of warfarin after a single dose is approximately one week; however, the effective half-life ranges from 20 to 60 hours, with a mean of about 40 hours. The clearance of R-warfarin is generally half that of S-warfarin, thus as the volumes of distribution are similar, the half-life of R-warfarin is longer than that of S-warfarin. The half-life of R-warfarin ranges from 37 to 89 hours, while that of S-warfarin ranges from 21 to 43 hours. Studies with radiolabeled drug have demonstrated that up to 92% of the orally administered dose is recovered in urine. Very little warfarin is excreted unchanged in urine. Urinary excretion is in the form of metabolites.
Elderly
Patients 60 years or older appear to exhibit greater than expected PT/INR response to the anticoagulant effects of warfarin. The cause of the increased sensitivity to the anticoagulant effects of warfarin in this age group is unknown. This increased anticoagulant effect from warfarin may be due to a combination of pharmacokinetic and pharmacodynamic factors. Racemic warfarin clearance may be unchanged or reduced with increasing age. Limited information suggests there is no difference in the clearance of S-warfarin in the elderly versus young subjects. However, there may be a slight decrease in the clearance of R-warfarin in the elderly as compared to the young. Therefore, as patient age increases, a lower dose of warfarin is usually required to produce a therapeutic level of anticoagulation.
Asians
Asian patients may require lower initiation and maintenance doses of warfarin. One non-controlled study conducted in 151 Chinese outpatients reported a mean daily warfarin requirement of 3.3 ± 1.4 mg to achieve an INR of 2 to 2.5. These patients were stabilized on warfarin for various indications. Patient age was the most important determinant of warfarin requirement in Chinese patients with a progressively lower warfarin requirement with increasing age.
Renal Dysfunction
Renal clearance is considered to be a minor determinant of anticoagulant response to warfarin. No dosage adjustment is necessary for patients with renal failure.
Hepatic Dysfunction
Hepatic dysfunction can potentiate the response to warfarin through impaired synthesis of clotting factors and decreased metabolism of warfarin.
Clinical Trials
Atrial Fibrillation (AF)
In five prospective randomized controlled clinical trials involving 3711 patients with non-rheumatic AF, warfarin significantly reduced the risk of systemic thromboembolism including stroke (see Table 2 ). The risk reduction ranged from 60% to 86% in all except one trial (CAFA: 45%) which stopped early due to published positive results from two of these trials. The incidence of major bleeding in these trials ranged from 0.6 to 2.7% (see Table 2 ). Meta-analysis findings of these studies revealed that the effects of warfarin in reducing thromboembolic events including stroke were similar at either moderately high INR (2.0-4.5) or low INR (1.4-3.0). There was a significant reduction in minor bleeds at the low INR. Similar data from clinical studies in valvular atrial fibrillation patients are not available.
|
N |
Thromboembolism |
% Major Bleeding |
||||||
|
Study |
Warfarin-Treated Patients | Control Patients |
PT Ratio |
INR |
% Risk Reduction |
p-value |
Warfarin-Treated Patients | Control Patients |
| AFASAK | 335 | 336 | 1.5-2.0 | 2.8-4.2 | 60 | 0.027 | 0.6 | 0.0 |
| SPAF | 210 | 211 | 1.3-1.8 | 2.0-4.5 | 67 | 0.01 | 1.9 | 1.9 |
| BAATAF | 212 | 208 | 1.2-1.5 | 1.5-2.7 | 86 | <0.05 | 0.9 | 0.5 |
| CAFA | 187 | 191 | 1.3-1.6 | 2.0-3.0 | 45 | 0.25 | 2.7 | 0.5 |
| SPINAF | 260 | 265 | 1.2-1.5 | 1.4-2.8 | 79 | 0.001 | 2.3 | 1.5 |
Myocardial Infarction
WARIS (The Warfarin Re-Infarction Study) was a double-blind, randomized study of 1214 patients 2 to 4 weeks post-infarction treated with warfarin to a target INR of 2.8 to 4.8. [But note that a lower INR was achieved and increased bleeding was associated with INR’s above 4.0; (see DOSAGE AND ADMINISTRATION )]. The primary endpoint was a combination of total mortality and recurrent infarction. A secondary endpoint of cerebrovascular events was assessed. Mean follow-up of the patients was 37 months. The results for each endpoint separately, including an analysis of vascular death, are provided in the following table:
|
Event |
Warfarin |
Placebo |
RR |
% Risk Reduction |
|
(N=607) |
(N=607) |
(95% CI) |
(p- value) |
|
|
RR= Relative risk; Risk reduction = (I - RR); CI=Confidence interval; MI=Myocardial infarction; py = patient years |
||||
| Total Patient Years of Follow-up | 2018 | 1944 | ||
| Total Mortality | 94 (4.7/100 py) | 123 (6.3/100 py) | 0.76 (0.60, 0.97) | 24 (p=0.030) |
| Vascular Death | 82 (4.1/100 py) | 105 (5.4/100 py) | 0.78 (0.60, 1.02) | 22 (p=0.068) |
| Recurrent MI | 82 (4.1/100 py) | 124 (6.4/100 py) | 0.66 (0.51, 0.85) | 34 (p=0.001) |
| Cerebrovascular Event | 20 (1.0/100 py) | 44 (2.3/100 py) | 0.46 (0.28, 0.75) | 54 (p=0.002) |
WARIS II (The Warfarin, Aspirin, Re-Infarction Study) was an open-label randomized study of 3630 patients hospitalized for acute myocardial infarction treated with warfarin target INR 2.8 to 4.2, aspirin 160 mg/day, or warfarin target INR 2.0 to 2.5 plus aspirin 75 mg/day prior to hospital discharge. There were approximately four times as many major bleeding episodes in the two groups receiving warfarin than in the group receiving aspirin alone. Major bleeding episodes were not more frequent among patients receiving aspirin plus warfarin than among those receiving warfarin alone, but the incidence of minor bleeding episodes was higher in the combined therapy group. The primary endpoint was a composite of death, nonfatal reinfarction, or thromboembolic stroke. The mean duration of observation was approximately 4 years. The results for WARIS II are provided in the following table8:
| Event | Aspirin (N=1206) | Warfarin (N=1216) | Aspirin plus Warfarin (N=1208) | Rate Ratio (95% CI) | p-value |
|
ND = not determined. |
|||||
| No. of Events | |||||
| Reinfarction | 117 | 90 | 69 | 0.56 (0.41-0.78) 0.74 (0.55-0.98)  |
<0.001 0.03 |
| Thromboembolic stroke | 32 | 17 | 17 | 0.52 (0.28-0.98) 0.52 (0.28-0.97)  |
0.03 0.03 |
Major Bleeding |
8 | 33 | 28 | 3.35 4.00  |
ND ND |
Minor Bleeding |
39 | 103 | 133 | 3.21 2.55  |
ND ND |
| Death | 92 | 96 | 95 | 0.82 | |
Mechanical and Bioprosthetic Heart Valves
In a prospective, randomized, open label, positive-controlled study9 in 254 patients, the thromboembolic-free interval was found to be significantly greater in patients with mechanical prosthetic heart valves treated with warfarin alone compared with dipyridamole-aspirin (p<0.005) and pentoxifylline-aspirin (p<0.05) treated patients. Rates of thromboembolic events in these groups were 2.2, 8.6, and 7.9/100 patient years, respectively. Major bleeding rates were 2.5, 0.0, and 0.9/100 patient years, respectively.
In a prospective, open label, clinical trial comparing moderate (INR 2.65) vs. high intensity (INR 9.0) warfarin therapies in 258 patients with mechanical prosthetic heart valves, thromboembolism occurred with similar frequency in the two groups (4.0 and 3.7 events/100 patient years, respectively). Major bleeding was more common in the high intensity group (2.1 events/100 patient years) vs. 0.95 events/100 patient years in the moderate intensity group.10
In a randomized trial in 210 patients comparing two intensities of warfarin therapy (INR 2.0-2.25 vs. INR 2.5-4.0) for a three-month period following tissue heart valve replacement, thromboembolism occurred with similar frequency in the two groups (major embolic events 2.0% vs. 1.9%, respectively and minor embolic events 10.8% vs. 10.2%, respectively). Major bleeding complications were more frequent with the higher intensity (major hemorrhages 4.6%) vs. none in the lower intensity.11
WARFARIN SODIUM INDICATIONS AND USAGE
Warfarin sodium tablets are indicated for the prophylaxis and/or treatment of venous thrombosis and its extension, and pulmonary embolism.
Warfarin sodium tablets are indicated for the prophylaxis and/or treatment of the thromboembolic complications associated with atrial fibrillation and/or cardiac valve replacement.
Warfarin sodium tablets are indicated to reduce the risk of death, recurrent myocardial infarction, and thromboembolic events such as stroke or systemic embolization after myocardial infarction.
WARFARIN SODIUM CONTRAINDICATIONS
Anticoagulation is contraindicated in any localized or general physical condition or personal circumstance in which the hazard of hemorrhage might be greater than the potential clinical benefits of anticoagulation, such as:
Pregnancy
Warfarin sodium tablets are contraindicated in women who are or may become pregnant because the drug passes through the placental barrier and may cause fatal hemorrhage to the fetus in utero. Furthermore, there have been reports of birth malformations in children born to mothers who have been treated with warfarin during pregnancy.
Embryopathy characterized by nasal hypoplasia with or without stippled epiphyses (chondrodysplasia punctata) has been reported in pregnant women exposed to warfarin during the first trimester. Central nervous system abnormalities also have been reported, including dorsal midline dysplasia characterized by agenesis of the corpus callosum, Dandy-Walker malformation, and midline cerebellar atrophy. Ventral midline dysplasia, characterized by optic atrophy, and eye abnormalities have been observed. Mental retardation, blindness, and other central nervous system abnormalities have been reported in association with second and third trimester exposure. Although rare, teratogenic reports following in utero exposure to warfarin include urinary tract anomalies such as single kidney, asplenia, anencephaly, spina bifida, cranial nerve palsy, hydrocephalus, cardiac defects and congenital heart disease, polydactyly, deformities of toes, diaphragmatic hernia, corneal leukoma, cleft palate, cleft lip, schizencephaly, and microcephaly.
Spontaneous abortion and stillbirth are known to occur and a higher risk of fetal mortality is associated with the use of warfarin. Low birth weight and growth retardation have also been reported.
Women of childbearing potential who are candidates for anticoagulant therapy should be carefully evaluated and the indications critically reviewed with the patient. If the patient becomes pregnant while taking this drug, she should be apprised of the potential risks to the fetus, and the possibility of termination of the pregnancy should be discussed in light of those risks.
Hemorrhagic tendencies or blood dyscrasias
Recent or contemplated surgery of
(1) central nervous system; (2) eye; (3) traumatic surgery resulting in large open surfaces.
Bleeding tendencies associated with active ulceration or overt bleeding of
(1) gastrointestinal, genitourinary or respiratory tracts; (2) cerebrovascular hemorrhage;
(3) aneurysms-cerebral, dissecting aorta; (4) pericarditis and pericardial effusions;
(5) bacterial endocarditis.
Threatened abortion, eclampsia and preeclampsia
Inadequate laboratory facilities
Unsupervised patients with senility, alcoholism, or psychosis or other lack of patient cooperation
Spinal puncture and other diagnostic or therapeutic procedures with potential for uncontrollable bleeding
Miscellaneous
Major regional, lumbar block anesthesia, malignant hypertension and known hypersensitivity to warfarin or to any other components of this product.
WARNINGS
The most serious risks associated with anticoagulant therapy with warfarin sodium are hemorrhage in any tissue or organ12 (see BLACK BOX WARNING ) and, less frequently (<0.1%), necrosis and/or gangrene of skin and other tissues. Hemorrhage and necrosis have in some cases been reported to result in death or permanent disability. Necrosis appears to be associated with local thrombosis and usually appears within a few days of the start of anticoagulant therapy. In severe cases of necrosis, treatment through debridement or amputation of the affected tissue, limb, breast or penis has been reported. Careful diagnosis is required to determine whether necrosis is caused by an underlying disease. Warfarin therapy should be discontinued when warfarin is suspected to be the cause of developing necrosis and heparin therapy may be considered for anticoagulation. Although various treatments have been attempted, no treatment for necrosis has been considered uniformly effective. See below for information on predisposing conditions. These and other risks associated with anticoagulant therapy must be weighed against the risk of thrombosis or embolization in untreated cases.
It cannot be emphasized too strongly that treatment of each patient is a highly individualized matter. Warfarin sodium tablets, a narrow therapeutic range (index) drug, may be affected by factors such as other drugs and dietary vitamin K. Dosage should be controlled by periodic determinations of prothrombin time (PT)/International Normalized Ratio (INR). Determinations of whole blood clotting and bleeding times are not effective measures for control of therapy. Heparin prolongs the one-stage PT. When heparin and warfarin sodium tablets are administered concomitantly, refer below to CONVERSION FROM HEPARIN THERAPY for recommendations.
Increased caution should be observed when warfarin sodium tablets are administered in the presence of any predisposing condition where added risk of hemorrhage, necrosis, and/or gangrene is present.
Anticoagulation therapy with warfarin sodium tablets may enhance the release of atheromatous plaque emboli, thereby increasing the risk of complications from systemic cholesterol microembolization, including the "purple toes syndrome". Discontinuation of warfarin sodium tablets therapy is recommended when such phenomena are observed.
Systemic atheroemboli and cholesterol microemboli can present with a variety of signs and symptoms including purple toes syndrome, livedo reticularis, rash, gangrene, abrupt and intense pain in the leg, foot, or toes, foot ulcers, myalgia, penile gangrene, abdominal pain, flank or back pain, hematuria, renal insufficiency, hypertension, cerebral ischemia, spinal cord infarction, pancreatitis, symptoms simulating polyarteritis, or any other sequelae of vascular compromise due to embolic occlusion. The most commonly involved visceral organs are the kidneys followed by the pancreas, spleen, and liver. Some cases have progressed to necrosis or death.
Purple toes syndrome is a complication of oral anticoagulation characterized by a dark, purplish or mottled color of the toes, usually occurring between 3-10 weeks, or later, after the initiation of therapy with warfarin or related compounds. Major features of this syndrome include purple color of plantar surfaces and sides of the toes that blanches on moderate pressure and fades with elevation of the legs; pain and tenderness of the toes; waxing and waning of the color over time. While the purple toes syndrome is reported to be reversible, some cases progress to gangrene or necrosis which may require debridement of the affected area, or may lead to amputation.
Warfarin sodium tablets should be used with caution in patients with heparin-induced thrombocytopenia and deep venous thrombosis. Cases of venous limb ischemia, necrosis, and gangrene have occurred in patients with heparin-induced thrombocytopenia and deep venous thrombosis when heparin treatment was discontinued and warfarin therapy was started or continued. In some patients sequelae have included amputation of the involved area and/or death.13
The decision to administer anticoagulants in the following conditions must be based upon clinical judgment in which the risks of anticoagulant therapy are weighed against the benefits:
Lactation
Based on very limited published data, warfarin has not been detected in the breast milk of mothers treated with warfarin. The same limited published data report that some breast-fed infants, whose mothers were treated with warfarin, had prolonged prothrombin times, although not as prolonged as those of the mothers. The decision to breast-feed should be undertaken only after careful consideration of the available alternatives. Women who are breast-feeding and anticoagulated with warfarin should be very carefully monitored so that recommended PT/INR values are not exceeded. It is prudent to perform coagulation tests and to evaluate vitamin K status in infants before advising women taking warfarin to breast-feed. Effects in premature infants have not been evaluated.
Severe to moderate hepatic or renal insufficiency
Infectious diseases or disturbances of intestinal flora: sprue, antibiotic therapy
Trauma which may result in internal bleeding
Surgery or trauma resulting in large exposed raw surfaces
Indwelling catheters
Severe to moderate hypertension
Known or suspected deficiency in protein C mediated anticoagulant response
Hereditary or acquired deficiencies of protein C or its cofactor, protein S, have been associated with tissue necrosis following warfarin administration. Not all patients with these conditions develop necrosis, and tissue necrosis occurs in patients without these deficiencies. Inherited resistance to activated protein C has been described in many patients with venous thromboembolic disorders but has not yet been evaluated as a risk factor for tissue necrosis. The risk associated with these conditions, both for recurrent thrombosis and for adverse reactions, is difficult to evaluate since it does not appear to be the same for everyone. Decisions about testing and therapy must be made on an individual basis. It has been reported that concomitant anticoagulation therapy with heparin for 5 to 7 days during initiation of therapy with warfarin sodium tablets may minimize the incidence of tissue necrosis. Warfarin therapy should be discontinued when warfarin is suspected to be the cause of developing necrosis and heparin therapy may be considered for anticoagulation.
Miscellaneous
Polycythemia vera, vasculitis, and severe diabetes.
PRECAUTIONS
Periodic determination of PT/INR is essential (see DOSAGE AND ADMINISTRATION: LABORATORY CONTROL ). Numerous factors, alone or in combination, including changes in diet, medications, botanicals and genetic variations in the CYP2C9 and VKORC1 enzymes (see CLINICAL PHARMACOLOGY, Pharmacogenomics ) may influence the response of the patient to warfarin.
Drug/Drug and Drug/Disease Interactions
It is generally good practice to monitor the patient’s response with additional PT/INR determinations in the period immediately after discharge from the hospital, and whenever other medications, including botanicals, are initiated, discontinued or taken irregularly. The following factors are listed for reference; however, other factors may also affect the anticoagulant response.
Drugs may interact with warfarin sodium tablets through pharmacodynamic or pharmacokinetic mechanisms. Pharmacodynamic mechanisms for drug interactions with warfarin sodium tablets are synergism (impaired hemostasis, reduced clotting factor synthesis), competitive antagonism (vitamin K), and altered physiologic control loop for vitamin K metabolism (hereditary resistance). Pharmacokinetic mechanisms for drug interactions with warfarin sodium tablets are mainly enzyme induction, enzyme inhibition, and reduced plasma protein binding. It is important to note that some drugs may interact by more than one mechanism.
The following factors, alone or in combination, may be responsible for INCREASED PT/INR response:
ENDOGENOUS FACTORS:
| blood dyscrasias — | diarrhea | hyperthyroidism |
| see CONTRAINDICATIONS | elevated temperature | poor nutritional state |
| cancer | hepatic disorders | steatorrhea |
| collagen vascular disease | infectious hepatitis | vitamin K deficiency |
| congestive heart failure | jaundice |
EXOGENOUS FACTORS:
Potential drug interactions with warfarin sodium tablets are listed below by drug class and by specific drugs.
|
Classes of Drug |
||
|
also: other medications affecting blood elements which may modify hemostasis dietary deficiencies prolonged hot weather unreliable PT/INR determinations |
||
| 5-lipoxygenase Inhibitor | Antiplatelet Drugs/Effects | Leukotriene Receptor Antagonist |
| Adrenergic Stimulants, Central | Antithyroid Drugs† | Monoamine Oxidase Inhibitors |
| Alcohol Abuse Reduction | Beta-Adrenergic Blockers | Narcotics, prolonged |
| Preparations | Cholelitholytic Agents | Nonsteroidal Anti- |
| Analgesics | Diabetes Agents, Oral | Inflammatory Agents |
| Anesthetics, Inhalation | Diuretics† | Proton Pump Inhibitors |
| Antiandrogen | Fungal Medications, | Psychostimulants |
| Antiarrhythmics† | Intravaginal, Systemic† | Pyrazolones |
| Antibiotics† | Gastric Acidity and Peptic | Salicylates |
| Aminoglycosides (oral) | Ulcer Agents† | Selective Serotonin |
| Cephalosporins, parenteral | Gastrointestinal | Reuptake Inhibitors |
| Macrolides | Prokinetic Agents | Steroids, Adrenocortical† |
| Miscellaneous | Ulcerative Colitis Agents | Steroids, Anabolic (17-Alkyl |
| Penicillins, intravenous, | Gout Treatment Agents | Testosterone Derivatives) |
| high dose | Hemorrheologic Agents | Thrombolytics |
| Quinolones (fluoroquinolones) | Hepatotoxic Drugs | Thyroid Drugs |
| Sulfonamides, long acting | Hyperglycemic Agents | Tuberculosis Agents† |
| Tetracyclines | Hypertensive Emergency Agents | Uricosuric Agents |
| Anticoagulants | Hypnotics† | Vaccines |
| Anticonvulsants† | Hypolipidemics† | Vitamins† |
| Antidepressants† | Bile Acid-Binding Resins† | |
| Antimalarial Agents | Fibric Acid Derivatives | |
| Antineoplastics† | HMG-CoA Reductase Inhibitors† | |
| Antiparasitic/Antimicrobials | ||
|
Specific Drugs Reported |
||
| acetaminophen | fenoprofen | paroxetine |
alcohol |
fluconazole | penicillin G, intravenous |
| allopurinol | fluorouracil | pentoxifylline |
| aminosalicylic acid | fluoxetine | phenylbutazone |
| amiodarone HCl | flutamide | phenytoin |
| argatroban | fluvastatin | piperacillin |
| aspirin | fluvoxamine | piroxicam |
| atenolol | gefitinib | pravastatin |
atorvastatin |
gemfibrozil | prednisone |
| azithromycin | glucagon | propafenone |
| bivalirudin | halothane | propoxyphene |
| capecitabine | heparin | propranolol |
| cefamandole | ibuprofen | propylthiouracil |
| cefazolin | ifosfamide | quinidine |
| cefoperazone | indomethacin | quinine |
| cefotetan | influenza virus vaccine | rabeprazole |
| cefoxitin | itraconazole | ranitidine |
| ceftriaxone | ketoprofen | rofecoxib |
| celecoxib | ketorolac | sertraline |
| cerivastatin | lansoprazole | simvastatin |
| chenodiol | lepirudin | stanozolol |
| chloramphenicol | levamisole | streptokinase |
chloral hydrate |
levofloxacin | sulfamethizole |
| chlorpropamide | levothyroxine | sulfamethoxazole |
cholestyramine |
liothyronine | sulfinpyrazone |
| cimetidine | lovastatin | sulfisoxazole |
| ciprofloxacin | mefenamic acid | sulindac |
| cisapride | methimazole |
tamoxifen |
| clarithromycin | methyldopa | tetracycline |
| clofibrate | methylphenidate | thyroid |
| warfarin sodium overdose | methylsalicylate ointment (topical) | ticarcillin |
cyclophosphamide |
metronidazole | ticlopidine |
| danazol | miconazole | tissue plasminogen |
| dextran | (intravaginal, oral, systemic) | activator (t-PA) |
| dextrothyroxine | moricizine hydrochloride |
tolbutamide |
| diazoxide | nalidixic acid | tramadol |
| diclofenac | naproxen | trimethoprim/sulfamethoxazole |
| dicumarol | neomycin | urokinase |
| diflunisal | norfloxacin | valdecoxib |
| disulfiram | ofloxacin | valproate |
| doxycycline | olsalazine | vitamin E |
| erythromycin | omeprazole | zafirlukast |
| esomeprazole | oxandrolone | zileuton |
| ethacrynic acid | oxaprozin | |
| ezetimibe | oxymetholone | |
| fenofibrate | pantoprazole | |
The following factors, alone or in combination, may be responsible for DECREASED PT/INR response:
ENDOGENOUS FACTORS:
| edema | hypothyroidism |
| hereditary coumarin resistance | nephrotic syndrome |
| hyperlipemia |
EXOGENOUS FACTORS:
Potential drug interactions with warfarin sodium tablets are listed below by drug class and by specific drugs.
|
Classes of Drugs |
||
|
also: diet high in vitamin K unreliable PT/INR determinations |
||
| Adrenal Cortical Steroid Inhibitors | Antipsychotic Medications | Hypolipidemics† |
| Antacids | Antithyroid Drugs† | Bile Acid-Binding Resins† |
| Antianxiety Agents Antiarrhythmics† |
Barbiturates Diuretics† |
HMG-CoA Reductase Inhibitors† |
| Anticonvulsants† | Enteral Nutritional Supplements | Immunosuppressives |
| Antidepressants† | Fungal Medications, Systemic† | Oral Contraceptives, |
| Antihistamines | Gastric Acidity and Peptic Ulcer Agents† | Estrogen Containing |
| Antineoplastics† | Hypnotics† | Selective Estrogen Receptor Modulators |
| Steroids, Adrenocortical† | ||
| Tuberculosis Agents†
Vitamins† |
||
|
Specific Drugs Reported: |
||
alcohol |
warfarin sodium underdosage | phenytoin |
| aminoglutethimide | cyclophosphamide |
pravastatin |
| amobarbital | dicloxacillin | prednisone |
atorvastatin |
ethchlorvynol | primidone |
| azathioprine | glutethimide | propylthiouracil |
| butabarbital | griseofulvin | raloxifene |
| butalbital | haloperidol | ranitidine |
| carbamazepine | meprobamate | rifampin |
chloral hydrate |
6-mercaptopurine | secobarbital |
| chlordiazepoxide | methimazole |
spironolactone |
| chlorthalidone | moricizine hydrochloride |
sucralfate |
cholestyramine |
nafcillin | trazodone |
| clozapine | paraldehyde | vitamin C (high dose) |
| corticotropin | pentobarbital | vitamin K |
| cortisone | phenobarbital | |
Because a patient may be exposed to a combination of the above factors, the net effect of warfarin sodium tablets on PT/INR response may be unpredictable. More frequent PT/INR monitoring is therefore advisable. Medications of unknown interaction with coumarins are best regarded with caution. When these medications are started or stopped, more frequent PT/INR monitoring is advisable.
It has been reported that concomitant administration of warfarin and ticlopidine may be associated with cholestatic hepatitis.
Botanical (Herbal) Medicines
Caution should be exercised when botanical medicines (botanicals) are taken concomitantly with warfarin sodium tablets. Few adequate, well-controlled studies exist evaluating the potential for metabolic and/or pharmacologic interactions between botanicals and warfarin sodium tablets. Due to a lack of manufacturing standardization with botanical medicinal preparations, the amount of active ingredients may vary. This could further confound the ability to assess potential interactions and effects on anticoagulation. It is good practice to monitor the patient’s response with additional PT/INR determinations when initiating or discontinuing botanicals.
Specific botanicals reported to affect warfarin sodium tablets therapy include the following:
- Bromelains, danshen, dong quai (Angelica sinensis), garlic, Ginkgo biloba, ginseng, and cranberry products are associated most often with an INCREASE in the effects of warfarin sodium tablets.
- Coenzyme Q10 (ubidecarenone) and St. John’s wort are associated most often with a DECREASE in the effects of warfarin sodium tablets.
Some botanicals may cause bleeding events when taken alone (e.g., garlic and Ginkgo biloba) and may have anticoagulant, antiplatelet and/or fibrinolytic properties. These effects would be expected to be additive to the anticoagulant effects of warfarin sodium tablets. Conversely, other botanicals may have coagulant properties when taken alone or may decrease the effects of warfarin sodium tablets.
Some botanicals that may affect coagulation are listed below for reference; however, this list should not be considered all-inclusive. Many botanicals have several common names and scientific names. The most widely recognized common botanical names are listed.
|
Botanicals that contain coumarins with potential anticoagulant effects: |
||
Agrimony |
Celery | Parsley |
| Alfalfa | Chamomile | Passion Flower |
| Angelica (Dong Quai) | (German and Roman) | Prickly Ash (Northern) |
| Aniseed | Dandelion |
Quassia |
| Arnica | Fenugreek | Red Clover |
| Asa Foetida | Horse Chestnut | Sweet Clover |
Bogbean |
Horseradish | Sweet Woodruff |
| Boldo | Licorice |
Tonka Beans |
| Buchu | Meadowsweet |
Wild Carrot |
Capsicum |
Nettle | Wild Lettuce |
Cassia |
||
|
Miscellaneous botanicals with anticoagulant properties: |
||
|
Bladder Wrack (Fucus) |
Pau d’arco | - |
|
Botanicals that contain salicylate and/or have antiplatelet properties: |
||
Agrimony |
Dandelion |
Meadowsweet |
| Aloe Gel | Feverfew | Onion |
| Aspen | Garlic |
Policosanol |
| Black Cohosh | German Sarsaparilla | Poplar |
| Black Haw | Ginger | Senega |
Bogbean |
Ginkgo Biloba | Tamarind |
Cassia |
Ginseng (Panax) |
Willow |
| Clove | Licorice |
Wintergreen |
|
Botanicals with fibrinolytic properties: |
||
| Bromelains | Garlic |
Inositol Nicotinate |
Capsicum |
Ginseng | Onion |
|
(Panax) |
||
|
Botanicals with coagulant properties: |
||
Agrimony |
Mistletoe | |
| Goldenseal | Yarrow | |
Effect on Other Drugs
Coumarins may also affect the action of other drugs. Hypoglycemic agents (chlorpropamide and tolbutamide) and anticonvulsants (phenytoin and phenobarbital) may accumulate in the body as a result of interference with either their metabolism or excretion.
Consideration for Increased Bleeding Risk
Warfarin sodium is a narrow therapeutic range (index) drug, and additional caution should be observed when warfarin sodium is administered to certain patients. Reported risk factors for bleeding include high intensity of anticoagulation (INR >4.0), age ≥65, highly variable INRs, history of gastrointestinal bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, malignancy, trauma, renal insufficiency, concomitant drugs (see PRECAUTIONS ) and long duration of warfarin therapy. Identification of risk factors for bleeding and certain genetic variations in CYP2CP and VKORC1 in a patient may increase the need for more frequent INR monitoring and the use of lower warfarin doses (see CLINICAL PHARMACOLOGY: Metabolism and DOSAGE AND ADMINISTRATION ). Bleeding is more likely to occur during the starting period and with a higher dose of warfarin sodium (resulting in a higher INR).
Intramuscular (I.M.) injections of concomitant medications should be confined to the upper extremities which permits easy access for manual compression, inspections for bleeding and use of pressure bandages.
Caution should be observed when warfarin sodium tablets are administered concomitantly with nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, to be certain that no change in anticoagulation dosage is required. In addition to specific drug interactions that might affect PT/INR, NSAIDs, including aspirin, can inhibit platelet aggregation, and can cause gastrointestinal bleeding, peptic ulceration and/or perforation.
INFORMATION FOR PATIENTS
The objective of anticoagulant therapy is to decrease the clotting ability of the blood so that thrombosis is prevented, while avoiding spontaneous bleeding. Effective therapeutic levels with minimal complications are in part dependent upon cooperative and well-instructed patients who communicate effectively with their physician. Patients should be advised: Strict adherence to prescribed dosage schedule is necessary. Do not take or discontinue any other medication, including salicylates (e.g., aspirin and topical analgesics), other over-the-counter medications, and botanical (herbal) products except on advice of the physician. Avoid alcohol consumption. Do not take warfarin sodium tablets during pregnancy and do not become pregnant while taking it (see CONTRAINDICATIONS ). Avoid any activity or sport that may result in traumatic injury. Prothrombin time tests and regular visits to physician or clinic are needed to monitor therapy. Carry identification stating that warfarin sodium tablets are being taken. If the prescribed dose of warfarin sodium tablets is forgotten, notify the physician immediately. Take the dose as soon as possible on the same day but do not take a double dose of warfarin sodium tablets the next day to make up for missed doses. The amount of vitamin K in food may affect therapy with warfarin sodium tablets. Eat a normal, balanced diet maintaining a consistent amount of vitamin K. Avoid drastic changes in dietary habits, such as eating large amounts of green leafy vegetables. You should also avoid intake of cranberry juice or any other cranberry products. Notify your health care provider if any of these products are part of your normal diet. Contact physician to report any illness, such as diarrhea, infection or fever. Notify physician immediately if any unusual bleeding or symptoms occur. Signs and symptoms of bleeding include: pain, swelling or discomfort, prolonged bleeding from cuts, increased menstrual flow or vaginal bleeding, nosebleeds, bleeding of gums from brushing, unusual bleeding or bruising, red or dark brown urine, red or tar black stools, headache, dizziness, or weakness. If therapy with warfarin sodium tablets is discontinued, patients should be cautioned that the anticoagulant effects of warfarin sodium tablets may persist for about 2 to 5 days. Patients should be informed that all warfarin sodium, USP, products represent the same medication, and should not be taken concomitantly, as overdosage may result. A Medication Guide14 should be available to patients when their prescriptions for warfarin sodium are issued.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity and mutagenicity studies have not been performed with warfarin sodium tablets. The reproductive effects of warfarin sodium tablets have not been evaluated. The use of warfarin during pregnancy has been associated with the development of fetal malformation in human (see CONTRAINDICATIONS ).
Use in Pregnancy
Pregnancy Category X - see CONTRAINDICATIONS .
PEDIATRIC USE
Safety and effectiveness in pediatric patients below the age of 18 have not been established, in randomized, controlled clinical trials. However, the use of warfarin sodium tablets in pediatric patients is well-documented for the prevention and treatment of thromboembolic events. Difficulty achieving and maintaining therapeutic PT/INR ranges in the pediatric patient has been reported. More frequent PT/INR determinations are recommended because of possible changing warfarin requirements.
GERIATRIC USE
Patients 60 years or older appear to exhibit greater than expected PT/INR response to the anticoagulant effects of warfarin (see CLINICAL PHARMACOLOGY ). Warfarin sodium tablets are contraindicated in any unsupervised patient with senility. Caution should be observed with administration of warfarin sodium to elderly patients in any situation or physical condition where added risk of hemorrhage is present. Lower initiation and maintenance doses of warfarin sodium tablets are recommended for elderly patients (see DOSAGE AND ADMINISTRATION ).
WARFARIN SODIUM ADVERSE REACTIONS
Potential adverse reactions to warfarin sodium tablets may include:
- Fatal or nonfatal hemorrhage from any tissue or organ. This is a consequence of the anticoagulant effect. The signs, symptoms, and severity will vary according to the location and degree or extent of the bleeding. Hemorrhagic complications may present as paralysis; paresthesia; headache, chest, abdomen, joint, muscle or other pain; dizziness; shortness of breath, difficult breathing or swallowing; unexplained swelling; weakness; hypotension; or unexplained shock. Therefore, the possibility of hemorrhage should be considered in evaluating the condition of any anticoagulated patient with complaints which do not indicate an obvious diagnosis. Bleeding during anticoagulant therapy does not always correlate with PT/INR (see OVERDOSAGE: Treatment ).
- Bleeding which occurs when the PT/INR is within the therapeutic range warrants diagnostic investigation since it may unmask a previously unsuspected lesion, e.g., tumor, ulcer, etc.
- Necrosis of skin and other tissues (see WARNINGS ).
- Adverse reactions reported infrequently include: hypersensitivity/allergic reactions, including anaphylactic reactions, systemic cholesterol microembolization, purple toes syndrome, hepatitis, cholestatic hepatic injury, jaundice, elevated liver enzymes, hypotension, vasculitis, edema, anemia, pallor, fever, rash, dermatitis, including bullous eruptions, urticaria, angina syndrome, chest pain, abdominal pain including cramping, flatulence/bloating, fatigue, lethargy, malaise, asthenia, nausea, vomiting, diarrhea, pain, headache, dizziness, loss of consciousness, syncope, coma, taste perversion, pruritus, alopecia, cold intolerance, and paresthesia including feeling cold and chills.
Rare events of tracheal or tracheobronchial calcification have been reported in association with long-term warfarin therapy. The clinical significance of this event is unknown.
Priapism has been associated with anticoagulant administration, however, a causal relationship has not been established.
OVERDOSAGE
Signs and Symptoms
Suspected or overt abnormal bleeding (e.g., appearance of blood in stools or urine, hematuria, excessive menstrual bleeding, melena, petechiae, excessive bruising or persistent oozing from superficial injuries) are early manifestations of anticoagulation beyond a safe and satisfactory level.
Treatment
Excessive anticoagulation, with or without bleeding, may be controlled by discontinuing warfarin sodium tablets therapy and if necessary, by administration of oral or parenteral vitamin K1. (Please see recommendations accompanying vitamin K1 preparations prior to use.)15, 16
Such use of vitamin K1 reduces response to subsequent warfarin sodium tablets therapy. Patients may return to a pretreatment thrombotic status following the rapid reversal of a prolonged PT/INR. Resumption of warfarin sodium administration reverses the effect of vitamin K, and a therapeutic PT/INR can again be obtained by careful dosage adjustment. If rapid anticoagulation is indicated, heparin may be preferable for initial therapy.
If minor bleeding progresses to major bleeding, give 5 to 25 mg (rarely up to 50 mg) parenteral vitamin K1. In emergency situations of severe hemorrhage, clotting factors can be returned to normal by administering 200 to 500 mL of fresh whole blood or fresh frozen plasma, or by giving commercial Factor IX complex.
A risk of hepatitis and other viral diseases is associated with the use of these blood products; Factor IX complex is also associated with an increased risk of thrombosis. Therefore, these preparations should be used only in exceptional or life-threatening bleeding episodes secondary to warfarin sodium overdosage.
Purified Factor IX preparations should not be used because they cannot increase the levels of prothrombin, Factor VII and Factor X which are also depressed along with the levels of Factor IX as a result of warfarin sodium tablets treatment. Packed red blood cells may also be given if significant blood loss has occurred. Infusions of blood or plasma should be monitored carefully to avoid precipitating pulmonary edema in elderly patients or patients with heart disease.
WARFARIN SODIUM DOSAGE AND ADMINISTRATION
The dosage and administration of warfarin sodium tablets must be individualized for each patient according to the particular patient’s PT/INR response to the drug. The dosage should be adjusted based upon the patient’s PT/INR.15, 16, 17, 18, 19 The best available information supports the following recommendations for dosing of warfarin sodium tablets.
Venous Thromboembolism (including deep venous thrombosis [DVT] and pulmonary embolism [PE])
For patients with a first episode of DVT or PE secondary to a transient (reversible) risk factor, treatment with warfarin for 3 months is recommended. For patients with a first episode of idiopathic DVT or PE, warfarin is recommended for at least 6 to 12 months. For patients with two or more episodes of documented DVT or PE, indefinite treatment with warfarin is suggested. For patients with a first episode of DVT or PE who have documented antiphospholipid antibodies or who have two or more thrombophilic conditions, treatment for 12 months is recommended and indefinite therapy is suggested. For patients with a first episode of DVT or PE who have documented deficiency of antithrombin, deficiency of Protein C or Protein S, or the Factor V Leiden or prothrombin 20210 gene mutation, homocystinemia, or high Factor VIII levels (>90th percentile of normal), treatment for 6 to 12 months is recommended and indefinite therapy is suggested for idiopathic thrombosis. The risk-benefit should be reassessed periodically in patients who receive indefinite anticoagulant treatment.12, 20 The dose of warfarin should be adjusted to maintain a target INR of 2.5 (INR range, 2.0 to 3.0) for all treatment durations. These recommendations are supported by the 7th ACCP guidelines.15, 17, 21, 22
Atrial Fibrillation
Five recent clinical trials evaluated the effects of warfarin in patients with non-valvular atrial fibrillation (AF). Meta-analysis findings of these studies revealed that the effects of warfarin in reducing thromboembolic events including stroke were similar at either moderately high INR (2.0-4.5) or low INR (1.4-3.0). There was a significant reduction in minor bleeds at the low INR. There are no adequate and well-controlled studies in populations with atrial fibrillation and valvular heart disease. Similar data from clinical studies in valvular atrial fibrillation patients are not available. The trials in non-valvular atrial fibrillation support the American College of Chest Physicians’ (7th ACCP) recommendation that an INR of 2.0-3.0 be used for warfarin therapy in appropriate AF patients.17
Oral anticoagulation therapy with warfarin is recommended in patients with persistent or paroxysmal AF (PAF) (intermittent AF) at high risk of stroke (i.e., having any of the following features: prior ischemic stroke, transient ischemic attack, or systemic embolism, age >75 years, moderately or severely impaired left ventricular systolic function and/or congestive heart failure, history of hypertension, or diabetes mellitus). In patients with persistent AF or PAF, age 65 to 75 years, in the absence of other risk factors, but who are at intermediate risk of stroke, antithrombotic therapy with either oral warfarin or aspirin, 325 mg/day, is recommended. For patients with AF and mitral stenosis, anticoagulation with oral warfarin is recommended (7th ACCP). For patients with AF and prosthetic heart valves, anticoagulation with oral warfarin should be used; the target INR may be increased and aspirin added depending on valve type and position, and on patient factors.17
Post-Myocardial Infarction
The results of the WARIS II study and 7th ACCP guidelines suggest that in most healthcare settings, moderate- and low-risk patients with a myocardial infarction should be treated with aspirin alone over oral vitamin-K antagonist (VKA) therapy plus aspirin. In healthcare settings in which meticulous INR monitoring is standard and routinely accessible, for both high- and low-risk patients after myocardial infarction (MI), long-term (up to 4 years) high-intensity oral warfarin (target INR, 3.5; range, 3.0 to 4.0) without concomitant aspirin or moderate-intensity oral warfarin (target INR, 2.5; range, 2.0 to 3.0) with aspirin is recommended. For high-risk patients with MI, including those with a large anterior MI, those with significant heart failure, those with intracardiac thrombus visible on echocardiography, and those with a history of a thromboembolic event, therapy with combined moderate-intensity (INR, 2.0 to 3.0) oral warfarin plus lowdose aspirin (≤100 mg/day) for 3 months after the MI is suggested.23
Mechanical and Bioprosthetic Heart Valves
For all patients with mechanical prosthetic heart valves, warfarin is recommended. For patients with a St. Jude Medical (St. Paul, MN) bileaflet valve in the aortic position, a target INR of 2.5 (range, 2.0 to 3.0) is recommended. For patients with tilting disk valves and bileaflet mechanical valves in the mitral position, the 7th ACCP recommends a target INR of 3.0 (range, 2.5 to 3.5). For patients with caged ball or caged disk valves, a target INR of 3.0 (range, 2.5 to 3.5) in combination with aspirin, 75 to 100 mg/day is recommended. For patients with bioprosthetic valves, warfarin therapy with a target INR of 2.5 (range, 2.0 to 3.0) is recommended for valves in the mitral position and is suggested for valves in the aortic position for the first 3 months after valve insertion.15
Recurrent Systemic Embolism and Other Indications
Oral anticoagulation therapy has not been evaluated by properly designed clinical trials in patients with valvular disease associated with atrial fibrillation, patients with mitral stenosis, and patients with recurrent systemic embolism of unknown etiology. A moderate dose regimen (INR 2.0 to 3.0) is recommended for these patients.17
An INR of greater than 4.0 appears to provide no additional therapeutic benefit in most patients and is associated with a higher risk of bleeding.
Initial Dosage
The dosing of warfarin sodium tablets must be individualized according to patient’s sensitivity to the drug as indicated by the PT/INR. Use of a large loading dose may increase the incidence of hemorrhagic and other complications, does not offer more rapid protection against thrombi formation, and is not recommended. It is recommended that warfarin sodium tablets therapy be initiated with a dose of 2 to 5 mg per day with dosage adjustments based on the results of PT/INR determinations.17, 18 The lower initiation doses should be considered for patients with certain genetic variations in CYP2C9 and VKORC1 enzymes as well as for elderly and/or debilitated patients and patients with potential to exhibit greater than expected PT/INR responses to warfarin sodium tablets (see CLINICAL PHARMACOLOGY and PRECAUTIONS ).
Maintenance
Most patients are satisfactorily maintained at a dose of 2 to 10 mg daily. Flexibility of dosage is provided by breaking scored tablets in half. The individual dose and interval should be gauged by the patient’s prothrombin response. Acquired or inherited warfarin resistance is rare, but should be suspected if large daily doses of warfarin sodium tablets are required to maintain a patient’s PT/INR within a normal therapeutic range. Lower maintenance doses are recommended for elderly and/or debilitated patients and patients with a potential to exhibit greater than expected PT/INR response to warfarin sodium tablets (see PRECAUTIONS ).
Duration of Therapy
The duration of therapy in each patient should be individualized. In general, anticoagulant therapy should be continued until the danger of thrombosis and embolism has passed.14, 15, 17, 18, 21, 22
Missed Dose
The anticoagulant effect of warfarin sodium tablets persists beyond 24 hours. If the patient forgets to take the prescribed dose of warfarin sodium tablets at the scheduled time, the dose should be taken as soon as possible on the same day. The patient should not take the missed dose by doubling the daily dose to make up for missed doses, but should refer back to his or her physician.
LABORATORY CONTROL
The PT reflects the depression of vitamin K dependent Factors VII, X and II. A system of standardizing the PT in oral anticoagulant control was introduced by the World Health Organization in 1983. It is based upon the determination of an International Normalized Ratio (INR) which provides a common basis for communication of PT results and interpretations of therapeutic ranges.24 The PT should be determined daily after the administration of the initial dose until PT/INR results stabilize in the therapeutic range. Intervals between subsequent PT/INR determinations should be based upon the physician’s judgment of the patient’s reliability and response to warfarin sodium tablets in order to maintain the individual within the therapeutic range. Acceptable intervals for PT/INR determinations are normally within the range of one to four weeks after a stable dosage has been determined. To ensure adequate control, it is recommended that additional PT tests be done when other warfarin products are interchanged with warfarin sodium tablets, USP, as well as whenever other medications are initiated, discontinued, or taken irregularly (see PRECAUTIONS ). Safety and efficacy of warfarin therapy can be improved by increasing the quality of laboratory control. Reports suggest that in usual care monitoring, patients are in therapeutic range only 33%-64% of the time. Time in therapeutic range is significantly greater (56%-93%) in patients managed by anticoagulation clinics, among self-testing and self-monitoring patients, and in patients managed with the help of computer programs.25 Self-testing patients had fewer bleeding events than patients in usual care.25
TREATMENT DURING DENTISTRY AND SURGERY
The management of patients who undergo dental and surgical procedures requires close liaison between attending physicians, surgeons and dentists.15, 19 PT/INR determination is recommended just prior to any dental or surgical procedure. In patients undergoing minimal invasive procedures who must be anticoagulated prior to, during, or immediately following these procedures, adjusting the dosage of warfarin sodium tablets to maintain the PT/INR at the low end of the therapeutic range may safely allow for continued anticoagulation. The operative site should be sufficiently limited and accessible to permit the effective use of local procedures for hemostasis. Under these conditions, dental and minor surgical procedures may be performed without undue risk of hemorrhage. Some dental or surgical procedures may necessitate the interruption of warfarin sodium tablets therapy. When discontinuing warfarin sodium tablets even for a short period of time, the benefits and risks should be strongly considered.
CONVERSION FROM HEPARIN THERAPY
Since the anticoagulant effect of warfarin sodium tablets is delayed, heparin is preferred initially for rapid anticoagulation. Conversion to warfarin sodium tablets may begin concomitantly with heparin therapy or may be delayed 3 to 6 days. To ensure continuous anticoagulation, it is advisable to continue full dose heparin therapy and that warfarin sodium tablets therapy be overlapped with heparin for 4 to 5 days, until warfarin sodium tablets have produced the desired therapeutic response as determined by PT/INR. When warfarin sodium tablets have produced the desired PT/INR or prothrombin activity, heparin may be discontinued.
Warfarin sodium tablets may increase the activated partial thromboplastin time (aPTT) test, even in the absence of heparin. A severe elevation (>50 seconds) in activated partial thromboplastin time (aPTT) with a PT/INR in the desired range has been identified as an indication of increased risk of postoperative hemorrhage.
During initial therapy with warfarin sodium tablets, the interference with heparin anticoagulation is of minimal clinical significance.
As heparin may affect the PT/INR, patients receiving both heparin and warfarin sodium tablets should have blood for PT/INR determination drawn at least:
- 5 hours after the last IV bolus dose of heparin, or
- 4 hours after cessation of a continuous IV infusion of heparin, or
- 24 hours after the last subcutaneous heparin injection.
HOW SUPPLIED
Warfarin Sodium Tablets, 1 mg are pink, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘1’ and bisect on one side and plain on other side and are supplied as follows:
Warfarin Sodium Tablets, 2 mg are lavender, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘2’ and bisect on one side and plain on other side and are supplied as follows:
Warfarin Sodium Tablets, 2.5 mg are green, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘2½’ and bisect on one side and plain on other side and are supplied as follows
Warfarin Sodium Tablets, 3 mg are tan, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘3’ and bisect on one side and plain on other side and are supplied as follows:
Warfarin Sodium Tablets, 4 mg are blue, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘4’ and bisect on one side and plain on other side and are supplied as follows:
Warfarin Sodium Tablets, 5 mg are peach, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘5’ and bisect on one side and plain on other side and are supplied as follows
Warfarin Sodium Tablets, 7.5 mg are yellow, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘7½’ and bisect on one side and plain on other side and are supplied as follows:
Warfarin Sodium Tablets, 10 mg are white to off white, oval, flat, beveled edge, uncoated tablets debossed with the logo of ‘WAR’, ‘10’ and bisect on one side and plain on other side and are supplied as follows:
Storage
Store at 20° - 25°C (68° - 77°F) [see USP Controlled Room Temperature]. Protect from light.
Dispense in a tight, light-resistant container as defined in the USP.
REFERENCES
- Yasar U, Eliasson E, Dahl M, Johansson I, Ingelman-Sundberg, M, Sjoqvist F. Validation of methods for CYP2C9 genotyping: Frequencies of mutant alleles in Swedish population. Biochem Biophys Res Comm. 1999; 254:628-631.
- Herman D, Locatelli I, Grabnar I, et al. Influence of CYP2C9 polymorphisms, demographic factors and concomitant drug therapy on warfarin metabolism and maintenance dose. Pharmacogenomics J. 2005;5:193-202.
- Sanderson S, Emery J, Higgins J. CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: A HuGEnet™ systemic review and meta-analysis. Genet Med. 2005;7:97-104.
- Lindh JD, Lundgren S, Holm L, Alfredsson L, Rane A. Several-fold increase in risk of overanticoagulation by CYP2C9 mutations. Clin Pharmacol Ther. 2005;78:540-550.
- Wadelius M, Chen LY, Downes K, et al. Common VKORC1 and GGCX polymorphisms associated with warfarin dose. Pharmacogenomics J. 2005;5:262-270.
- Veenstra DL, You JHS, Rieder MJ, et al. Association of Vitamin K epoxide reductase complex 1 (VKORC1) variants with warfarin dose in a Hong Kong Chinese patient population. Pharmacogenet Genomics. 2005;15-687-691.
- Takahashi H, Wilkinson GR, Nutescu EA, et al. Different contributions of polymorphisms in VKORC1 and CYP2C9 to intra- and inter-population differences in maintenance doses of warfarin in Japanese, Caucasians and African Americans. Pharmacogenet Genomics. 2006;16:101-110.
- Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002;347:969-974.
- Mok CK, Boey J, Wang R, et al. Warfarin versus dipyridamole-aspirin and pentoxifylline-aspirin for prevention of prosthetic valve thromboembolism: a prospective randomized clinical trial. Circ. 2985;72:1059-1063.
- Saour JN, Sieck JO, Mamo LA, Gallus AS. Trial of different intensities of anticoagulation in patients with prosthetic heart valves. N Engl J Med. 1990;322:428-432.
- Turpie AG, Hirsh J, Gunstensen J, Nelson H, Gent M. Randomized comparison to two intensities of oral anticoagulant therapy after tissue heart valve replacement. Lancet. 1988;331:1242-1245.
- Bller HR, Agnelli G, Hull RD, Hyers TM, Prins MH and Raskob GE. Antithrombotic Therapy for Venous Thromboembolic Disease. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:401S-428S.
- Warkentin TE, Elavathil LJ, Hayward CPM, Johnston MG, Russett JI, Kelton JG. The pathogenesis of venous limb gangrene associated with heparin-induced thrombocytopenia. Ann Intern Med. 1997;127:804-812.
- Warfarin Sodium Tablets, USP Medication Guide. Princeton, NJ: Zydus Pharmaceuticals USA Inc.; 08/07.
- Salem DN, Stein PD, Al-Ahmad, et al. Antithrombotic therapy in valvular heart disease–native and prosthetic. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:457S-482S.
- American Geriatrics Society Clinical Practice Guidelines. The Use of Oral Anticoagulants (Warfarin) in Older People. J Amer Geriatr Soc. 2000;48:224-227.
- Singer DE, Albers GW, Dalen JE, Go AS, Halperin JL, and Manning WJ. Antithrombotic Therapy in Atrial Fibrillation. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:429S-456S.
- Jaffer AK and Bragg L. Practical Tips for warfarin dosing and monitoring. Cleveland Clinic J Med. 2003;70:361-371.
- Jaffer AK, Brotman DJ, Chukwumerije N. When patients on warfarin need surgery. Cleveland Clinic J Med. 2003;70:973-984.
- Kearon C, Ginsberg JS, Kovacs M, et al, for the Extended Low-Intensity Anticoagulation for Thrombo-Embolism Investigators. Comparison of low-intensity warfarin therapy with conventional-intensity warfarin therapy for long-term prevention of recurrent venous thromboembolism. N Engl J Med. 2003;349:631-639.
- Schulman S, Granqvist S, Holmstrm M, et al. The Duration of Oral Anticoagulant Trial Study Group. The duration of oral anticoagulant therapy after a second episode of venous thromboembolism. N Engl J Med. 1997;336:393-398.
- Ridker PM, Goldhaber SZ, Danielson E, et al, for the PREVENT Investigators. Long-term, low-intensity warfarin therapy for the prevention of recurrent venous thromboembolism. N Engl J Med. 2003;348:1425-1434.
- Harrington RA, Becker RC, Ezekowitz M, et al. Antithrombotic therapy for coronary artery disease. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:513S-548S.
- Ansell J, Hirsh J, Pollen L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:204S-233S.
- Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet. 2006;367:404-411.
Image of 1mg Label
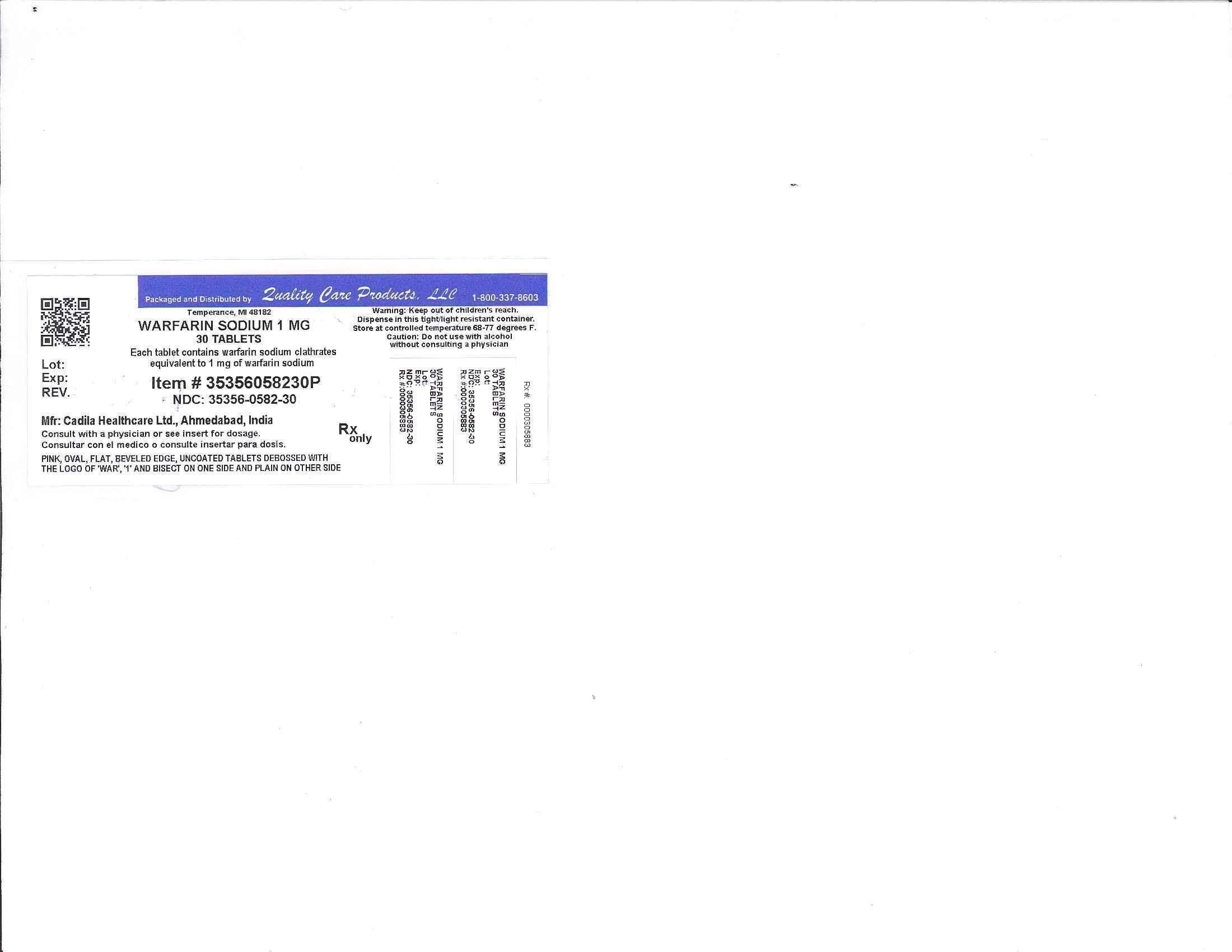
Image of 2.5mg Label

Image of 2mg Label

Image of 3mg Label
Warfarin SodiumWarfarin Sodium TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Warfarin SodiumWarfarin Sodium TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Warfarin SodiumWarfarin Sodium TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Warfarin SodiumWarfarin Sodium TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||