Testim
Lake Erie Medical DBA Quality Care Products LLC
Testim 1% (testosterone gel) CIII
FULL PRESCRIBING INFORMATION: CONTENTS*
- TESTIM DESCRIPTION
- CLINICAL PHARMACOLOGY
- TESTIM INDICATIONS AND USAGE
- TESTIM CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- TESTIM ADVERSE REACTIONS
- DRUG ABUSE AND DEPENDENCE
- OVERDOSAGE
- TESTIM DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
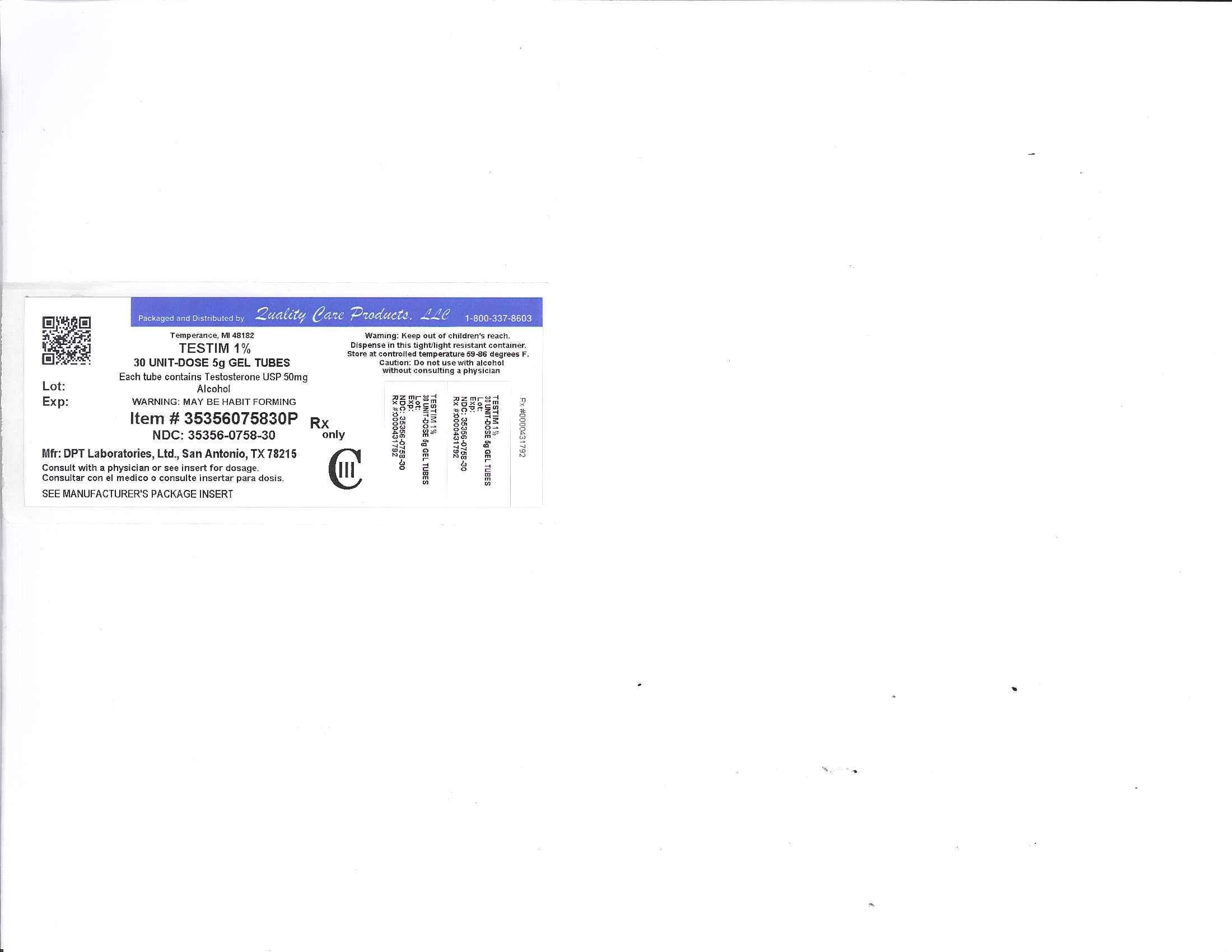
- Image of Label
FULL PRESCRIBING INFORMATION
WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
- Virilization has been reported in children who were secondarily exposed to testosterone gel.
- Children should avoid contact with unwashed or unclothed application sites in men using testosterone gel.
- Healthcare providers should advise patients to strictly adhere to recommended instructions for use.
(See WARNINGS, Potential for Secondary Exposure to Testosterone)
TESTIM DESCRIPTION
Testim® (testosterone gel) is a clear to translucent hydroalcoholic topical gel containing 1% testosterone. Testim® provides continuous transdermal delivery of testosterone for 24 hours, following a single application to intact, clean, dry skin of the shoulders and upper arms.
One 5 g or two 5 g tubes of Testim® contains 50 mg or 100 mg of testosterone, respectively, to be applied daily to the skin’s surface. Approximately 10% of the applied testosterone dose is absorbed across skin of average permeability during a 24-hour period.
The active pharmacological ingredient in Testim® is testosterone.

Testosterone USP is a white to practically white crystalline powder chemically described as 17-β hydroxyandrost-4-en-3-one. Inactive ingredients in Testim® are purified water, pentadecalactone, carbopol, acrylates, propylene glycol, glycerin, polyethylene glycol, ethanol (74%), and tromethamine.
CLINICAL PHARMACOLOGY
Testim® 1% (testosterone gel) delivers physiologic amounts of testosterone, producing circulating testosterone levels that approximate normal levels (e.g., 300 – 1000 ng/dL) seen in healthy men.
Testosterone – General Androgen Effects:
Testosterone and dihydrotestosterone (DHT), endogenous androgens, are responsible for normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of the prostate, seminal vesicles, penis, and scrotum; the development of male hair distribution, such as facial, pubic, chest, and axillary hair; laryngeal enlargement; vocal cord thickening; alterations in body musculature; and fat distribution.
Male hypogonadism results from insufficient secretion of testosterone and is characterized by low serum testosterone concentrations. Symptoms associated with male hypogonadism include decreased sexual desire with or without impotence, fatigue and loss of energy, mood depression, regression of secondary sexual characteristics, and osteoporosis. Hypogonadism is a risk factor for osteoporosis in men.
Drugs in the androgen class also promote retention of nitrogen, sodium, potassium, phosphorus, and decreased urinary excretion of calcium.
Androgens have been reported to increase protein anabolism and decrease protein catabolism. Nitrogen balance is improved only when there is sufficient intake of calories and protein. Androgens have been reported to stimulate the production of red blood cells by enhancing erythropoietin production.
Androgens are responsible for the growth spurt of adolescence and for the eventual termination of linear growth brought about by fusion of the epiphyseal growth centers. In children, exogenous androgens accelerate linear growth rates but may cause a disproportionate advancement in bone maturation. Use over long periods may result in fusion of the epiphyseal growth centers and termination of the growth process.
During exogenous administration of androgens, endogenous testosterone release may be inhibited through feedback inhibition of pituitary luteinizing hormone (LH). At large doses of exogenous androgens, spermatogenesis may also be suppressed through feedback inhibition of pituitary follicle-stimulating hormone (FSH).
There is a lack of substantial evidence that androgens are effective in accelerating fracture healing or in shortening post-surgical convalescence.
Pharmacokinetics
The pharmacokinetics of Testim® have been evaluated with administration of doses containing 50 mg and 100 mg of testosterone to adult males with morning testosterone levels ≤300 ng/dL.
Absorption
Testim® is a topical formulation that dries quickly when applied to the skin surface. The skin serves as a reservoir for the sustained release of testosterone into the systemic circulation. Approximately 10% of the testosterone applied on the skin surface is absorbed into the systemic circulation during a 24-hour period.
Single Dose
In single dose studies, when either Testim® 50 mg or 100 mg was administered, absorption of testosterone into the blood continued for the entire 24 hour dosing period. Also, mean peak and average serum concentrations within the normal range were achieved within 24 hours.
Multiple Dose
With single daily applications of Testim® 50 mg and 100 mg, follow-up measurements at 30 and 90 days after starting treatment have confirmed that serum testosterone and DHT concentrations are generally maintained within the normal range.
Figure 1 summarizes the 24-hour pharmacokinetic profile of testosterone for patients maintained on Testim® 50 mg or Testim® 100 mg for 30 days.
Figure 1
Mean Steady-State Serum Testosterone (±SD) (ng/dL) Concentrations on Day 30 in Patients Applying Testim® Once Daily

The average daily testosterone concentration produced by Testim® 100 mg at Day 30 was 612 (± 286) ng/dL and by Testim® 50 mg at Day 30 was 365 (± 187) ng/dL.
Figure 2 summarizes the 24-hour pharmacokinetic profile of DHT for patients maintained on Testim® 50 mg or Testim® 100 mg for 30 days.
Figure 2
Mean Steady-State Serum Dihydrotestosterone (±SD) (pg/mL) Concentrations on Day 30 in Patients Applying Testim® Once Daily

The average daily DHT concentration produced by Testim® 100 mg at Day 30 was 555 (± 293) pg/mL and by Testim® 50 mg at Day 30 was 346 (± 212) pg/mL.
Washing
The effect of showering (with mild soap) at 1, 2 and 6 hours post application of Testim® 100 mg was evaluated in a clinical trial in 12 men. The study demonstrated that the overall effect of washing was to lessen testosterone levels; however, when washing occurred two or more hours post drug application, serum testosterone levels remained within the normal range.
Distribution
Circulating testosterone is chiefly bound in the serum to sex hormone-binding globulin (SHBG) and albumin. The albumin-bound fraction of testosterone easily dissociates from albumin and is presumed to be bioactive. The portion of testosterone bound to SHBG is not considered biologically active. Approximately 40% of testosterone in plasma is bound to SHBG, 2% remains unbound (free) and the rest is bound to albumin and other proteins. The amount of SHBG in the serum and the total testosterone level will determine the distribution of bioactive and nonbioactive androgen.
Metabolism
There is considerable variation in the half-life of testosterone as reported in the literature, ranging from ten to 100 minutes.
Testosterone is metabolized to various 17-keto steroids through two different pathways. The major active metabolites of testosterone are estradiol and DHT. Testosterone is metabolized to DHT by steroid 5α-reductase located in the skin, liver, and the urogenital tract of the male. DHT binds with greater affinity to SHBG than does testosterone. In many tissues, the activity of testosterone depends on its reduction to DHT, which binds to cytosol receptor proteins. The steroid-receptor complex is transported to the nucleus where it initiates transcription and cellular changes related to androgen action. In reproductive tissues, DHT is further metabolized to 3α and 3β androstanediol. Inactivation of testosterone occurs primarily in the liver.
DHT concentrations increased in parallel with testosterone concentrations during Testim® treatment. After 90 days of treatment, mean DHT concentrations remained generally within the normal range for Testim®-treated subjects.
Excretion
About 90% of a testosterone dose given intramuscularly is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and metabolites; about 6% of a dose is excreted in the feces, mostly in the unconjugated form.
Special Population
In patients treated with Testim® there are no observed differences in the average daily serum testosterone concentration at steady-state based on age or cause of hypogonadism. No formal studies were conducted in a pediatric age population or in patients with renal or hepatic insufficiencies.
Clinical Studies
Testim® was evaluated in a randomized multicenter, multi-dose, active and placebo controlled 90-day study in 406 adult males with morning testosterone levels ≤300 ng/dL. The study was double-blind for the doses of Testim® and placebo, but open label for the non-scrotal testosterone transdermal system. During the first 60 days, patients were evenly randomized to Testim® 50 mg, Testim® 100 mg, placebo gel, or testosterone transdermal system. At Day 60, patients receiving Testim® were maintained at the same dose, or were titrated up or down within their treatment group, based on 24-hour averaged serum testosterone concentration levels obtained on Day 30.
Of 192 hypogonadal men who were appropriately titrated with Testim® and who had sufficient data for analysis, 74% achieved an average serum testosterone level within the normal range on treatment Day 90.
Table 1 summarizes the mean testosterone concentrations on Day 30 for patients receiving Testim® 50 mg or 100 mg.
|
Testim®
50 mg n=94 |
Testim®
100 mg n=95 |
Placebo n=93 |
|
|
Cavg
(ng/dL) |
365 ± 187 | 612 ± 286 | 216 ± 79 |
|
Cmax
(ng/dL) |
538 ± 371 | 897 ± 565 | 271 ± 110 |
|
Cmin
(ng/dL) |
223 ± 126 | 394 ±189 | 164 ± 64 |
At Day 30, patients receiving Testim® 100 mg daily showed significant improvement from baseline in multiple sexual function parameters as measured by patient questionnaires when compared to placebo. These parameters included sexual motivation, sexual desire, sexual activity and spontaneous erections. For Testim® 100 mg, improvements in sexual motivation, spontaneous erections, and sexual desire were maintained through Day 90. Sexual enjoyment and satisfaction with erection duration were improved compared to baseline but these improvements were not significant compared to the placebo group.
In Testim®-treated patients, the number of days in which sexual activity was reported to occur increased by 123% from baseline at Day 30 and was still increased from baseline by 59% at Day 90. The number of days with spontaneous erections increased by 137% at Day 30 and was maintained at 78% at Day 90 for Testim®-treated patients compared to baseline.
Table 2 summarizes the changes in body composition at Day 90 for patients receiving Testim® 50 mg or 100 mg as measured by standardized whole body DEXA (Dual Energy X-ray Absorptiometry) scanning.
| Days of Treatment |
Lean Body Mass (Muscle) (kg) |
Total Fat Mass (kg) |
% Body Fat |
| Baseline | 61.6 | 29.4 | 30.9 |
| Day 90 | 63.3 | 28.6 | 29.8 |
| Change from Baseline | ↑1.6 | ↓0.8 | ↓1.1 |
At Day 90, mean increases from baseline in lean body mass and mean decreases from baseline in total fat mass and percent body fat in Testim®-treated patients were significant when compared to placebo-treated patients.
Potential for Testosterone Transfer
The potential for dermal testosterone transfer following Testim® use was evaluated in two clinical trials with males dosed with Testim® and their untreated female partners.
In the first trial (AUX-TG-206), 30 couples were evenly randomized to five groups. In the first four groups, 100 mg of Testim® was applied to the male abdomen and the couples were then asked to rub abdomen-to-abdomen for 15 minutes at 1 hour, 4 hours, 8 hours or 12 hours after dose application, respectively. In these couples, serum testosterone concentrations in female partners increased from baseline by at least 4 times and potential for transfer was seen at all timepoints.
When 6 males used a shirt to cover the abdomen at 15 minutes post-application and partners again rubbed abdomens for 15 minutes at the 1 hour timepoint, the potential for transfer was markedly reduced.
In the second trial (AUX-TG-209), 24 couples were evenly randomized to four groups. Testim® 100 mg was applied to the male arms and shoulders. In one group, 15 minutes of direct skin-to-skin rubbing began at 4 hours after application. In these six women, all of whom showered immediately after the rubbing activity, mean maximum serum testosterone concentrations increased from baseline by approximately 4 times. When males wore a long-sleeved T-shirt and rubbing was started at 1 and at 4 hours after application, the transfer of testosterone from male to female partners was prevented.
TESTIM INDICATIONS AND USAGE
Testim® is indicated for testosterone replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone:
- Primary hypogonadism (congenital or acquired): testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchiectomy, Klinefelter's syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. These men usually have low serum testosterone levels and gonadotropins (FSH, LH) above the normal range.
- Hypogonadotropic hypogonadism (congenital or acquired): idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. These men have low testosterone serum levels but have gonadotropins in the normal or low range.
Testim® has not been clinically evaluated in males under 18 years of age.
TESTIM CONTRAINDICATIONS
Androgens are contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate. Testim® is not indicated for use in women, has not been evaluated for use in women, and must not be used in women.
Pregnant and nursing women should avoid skin contact with Testim® application sites on men. Testosterone may cause fetal harm. Testosterone exposure during pregnancy has been reported to be associated with fetal abnormalities. In the event that unwashed or unclothed skin to which Testim® has been applied comes in direct contact with the skin of a pregnant or nursing woman, the general area of contact on the woman should be immediately washed with soap and water.
Testim® should not be used in patients with known hypersensitivity to any of its ingredients, including testosterone USP that is chemically synthesized from soy.
WARNINGS
- Men with benign prostatic hyperplasia (BPH) are at an increased risk for worsening of BPH. In addition, men treated with androgens may be at an increased risk for prostate cancer. Geriatric patients and other patients with clinical or demographic characteristics that are recognized to be associated with an increased risk of prostate cancer should be evaluated for the presence of prostate cancer prior to initiation of testosterone replacement therapy. In men receiving testosterone replacement therapy, surveillance for prostate cancer should be consistent with current practices for eugonadal men (see PRECAUTIONS, Carcinogenesis, Mutagenesis, Impairment of Fertility and Laboratory Tests).
- Potential for Secondary Exposure to Testosterone
- Secondary exposure to testosterone in children and women can occur with testosterone gel use in men. Cases of secondary exposure resulting in virilization of children have been reported in postmarketing surveillance of testosterone-containing gel products. Signs and symptoms have included enlargement of the penis or clitoris, development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases, these signs and symptoms regressed with removal of the exposure to testosterone. In a few cases, however, enlarged genitalia did not fully return to age-appropriate normal size, and bone age remained modestly greater than chronological age. The risk of transfer was increased in some of these cases by not adhering to precautions for the appropriate use of the testosterone gel product.
- Inappropriate changes in genital size or development of pubic hair or libido in children, or changes in body hair distribution, significant increase in acne, or other signs of virilization in adult women should be brought to the attention of a physician, and the possibility of secondary exposure to testosterone gel should also be brought to the attention of a physician. Testosterone gel should be promptly discontinued until the cause of virilization has been identified.
-
Strict adherence to the following precautions is advised in order to minimize the potential for secondary exposure to testosterone from Testim®-treated skin:
- Children and women should avoid contact with Testim® application sites on the skin of men using Testim.
- Testim® should only be applied to the shoulders or upper arms (area of application should be limited to the area that will be covered by the patient’s short sleeve t-shirt).
- Patients should wash their hands thoroughly and immediately with soap and water after application of Testim®.
- Patients should cover the application site(s) with clothing (e.g., a shirt) after the gel has dried.
- Prior to any situation in which skin-to-skin contact is anticipated, patients should wash the application site(s) thoroughly with soap and water to remove any testosterone residue.
- In the event that unwashed or unclothed skin to which Testim® has been applied comes in direct contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible. Studies show that residual testosterone is removed from the skin surface by washing with soap and water.
- Testim® should not be applied to the abdomen.
- Prolonged use of high doses of orally active 17-alpha-alkyl androgens (e.g., methyltestosterone) has been associated with serious hepatic adverse effects (peliosis hepatis, hepatic neoplasms, cholestatic hepatitis, and jaundice). Peliosis hepatis can be a life-threatening or fatal complication. Long-term therapy with testosterone enanthate, which elevates blood levels for prolonged periods has produced multiple hepatic adenomas. Transdermal testosterone is not known to produce these adverse effects.
- Edema, with or without congestive heart failure, may be a serious complication in patients with preexisting cardiac, renal, or hepatic disease. In addition to discontinuation of the drug, diuretic therapy may be required.
- Gynecomastia occasionally develops and occasionally persists in patients being treated for hypogonadism.
- The treatment of hypogonadal men with testosterone may potentiate sleep apnea in some patients, especially those with risk factors such as obesity or chronic lung diseases.
PRECAUTIONS
General
The physician should instruct patients to report any of the following:
- Too frequent or persistent erections of the penis.
- Any changes in skin color, ankle swelling or unexplained nausea and vomiting.
- Breathing disturbances, including those associated with sleep.
Information for Patients
Advise patients to carefully read the Medication Guide that accompanies each carton of Testim® single-use tubes.
Advise patients of the following:
- Men with known or suspected prostate or breast cancer should not use Testim®.
- Secondary exposure to testosterone in children and women can occur with the use of testosterone gel products in men. Cases of secondary exposure to testosterone have been reported in children with signs and symptoms including enlargement of the penis or clitoris, premature development of pubic hair, increased erections, and aggressive behavior.
Unexpected sexual development including inappropriate enlargement of the penis or clitoris, premature development of pubic hair, increased erections, and aggressive behavior in children, or changes in hair distribution, increase in acne, or other signs of testosterone effects in adult women should be brought to the attention of a physician and the possibility of secondary exposure to testosterone gel also should be brought to the attention of a physician. Testosterone gel should be promptly discontinued until the cause of virilization is identified. -
Strict adherence to the following precautions is advised in order to minimize the potential for secondary exposure to testosterone from Testim®-treated skin:
- Children and women should avoid contact with Testim® application sites on the skin of men using Testim®.
- Testim® should only be applied to the shoulders or upper arms (area of application should be limited to the area that will be covered by the patient’s short sleeve t-shirt).
- Patients should wash their hands thoroughly and immediately with soap and water after application of Testim®.
- Patients should cover the application site(s) with clothing (e.g., a shirt) after the gel has dried.
- Prior to any situation in which skin-to-skin contact is anticipated, patients should wash the application site(s) thoroughly with soap and water to remove any testosterone residue.
- In the event that unwashed or unclothed skin to which testosterone gel has been applied comes in direct contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible. Studies show that residual testosterone is removed from the skin surface by washing with soap and water.
Also advise patients of the following:
- Testim® should not be applied to the scrotum, penis, or abdomen.
- Testim® should be applied once daily at approximately the same time each day to clean dry skin of the shoulders and/or upper arms.
- Washing or swimming may lessen testosterone levels; however, when washing occurs two or more hours post drug application, serum testosterone levels remain within the normal range.
Laboratory Tests
- Hemoglobin and hematocrit levels should be checked periodically (to detect polycythemia) in patients on long-term androgen therapy.
- Liver function, prostate specific antigen (PSA), cholesterol, and high-density lipoprotein (HDL) should be checked periodically.
- To ensure proper dosing, serum testosterone concentrations should be measured (see DOSAGE AND ADMINISTRATION).
Drug Interactions
Oxyphenbutazone: Concurrent administration of oxyphenbutazone and androgens may result in elevated serum levels of oxyphenbutazone.
Insulin: In diabetic patients, the metabolic effects of androgens may decrease blood glucose and, therefore, insulin requirements.
Propranolol: In a published pharmacokinetic study of an injectable testosterone product, administration of testosterone cypionate led to an increased clearance of propranolol in the majority of men tested. It is unknown if this would apply to Testim®.
Corticosteroids: The concurrent administration of testosterone with ACTH or corticosteroids may enhance edema formation; thus these drugs should be administered cautiously, particularly in patients with cardiac or hepatic disease.
Drug/Laboratory Test Interactions
Androgens may decrease levels of thyroxin-binding globulin, resulting in decreased total T4 serum levels and increased resin uptake of T3 and T4. Free thyroid hormone levels remain unchanged, however, and there is no clinical evidence of thyroid dysfunction.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal Data: Testosterone has been tested by subcutaneous injection and implantation in mice and rats. In mice, the implant induced cervical-uterine tumors, which metastasized in some cases. There is suggestive evidence that injection of testosterone into some strains of female mice increases their susceptibility to hepatoma. Testosterone is also known to increase the number of tumors and decrease the degree of differentiation of chemically induced carcinomas of the liver in rats.
Human Data: There are rare reports of hepatocellular carcinoma in patients receiving long-term oral therapy with androgens in high doses. Withdrawal of the drugs did not lead to regression of the tumors in all cases.
Geriatric patients treated with androgens may be at an increased risk for the development of prostatic hyperplasia and prostatic carcinoma. Geriatric patients and other patients with clinical or demographic characteristics that are recognized to be associated with an increased risk of prostate cancer should be evaluated for the presence of prostate cancer prior to initiation of testosterone replacement therapy.
In men receiving testosterone replacement therapy, surveillance for prostate cancer should be consistent with current practices for eugonadal men.
Pregnancy Category X (see Contraindications) – Teratogenic Effects: Testim® is not indicated for women and must not be used in women. Testosterone may cause fetal harm.
Nursing Mothers: Testim® is not indicated for women and must not be used in nursing mothers.
Pediatric Use: Safety and efficacy of Testim® in patients <18 years old has not been established.
TESTIM ADVERSE REACTIONS
In a controlled clinical study, 304 patients were treated with Testim® 50 mg or 100 mg or placebo gel for up to 90 days. Two hundred-five (205) patients received Testim® 50 mg or 100 mg daily and 99 patients received placebo. Patients with adverse events that were possibly or probably related to study drug and reported by ≥1% of the Testim® patients and greater than placebo are listed in Table 3.
| Event | Testim®
50 mg |
Testim®
100 mg |
Placebo |
| Application Site Reactions | 2% | 4% | 3% |
| Benign Prostatic Hyperplasia | 0% | 1% | 1% |
| Blood Pressure Diastolic Decreased |
1% | 0% | 0% |
| Blood Pressure Increased | 1% | 1% | 0% |
| Gynecomastia | 1% | 0% | 0% |
| Headache | 1% | 1% | 0% |
| Hematocrit/hemoglobin Increased |
1% | 2% | 0% |
| Hot Flushes | 1% | 0% | 0% |
| Insomnia | 1% | 0% | 0% |
| Lacrimation Increased | 1% | 0% | 0% |
| Mood Swings | 1% | 0% | 0% |
| Smell Disorder | 1% | 0% | 0% |
| Spontaneous Penile Erection | 1% | 0% | 0% |
| Taste Disorder | 1% | 1% | 0% |
The following adverse events possibly or probably related to Testim® occurred in fewer than 1% of patients but were greater in Testim® groups compared to the placebo group: activated partial thromboplastin time prolonged, blood creatinine increased, prothrombin time prolonged, appetite increased, sensitive nipples, and acne.
In this clinical trial of Testim®, six patients had adverse events that led to their discontinuation. These events included: vertigo, coronary artery disease, depression with suicidal ideation, urinary tract infection/pneumonia (none of which were considered related to Testim® administration), mood swings and hypertension. No Testim® patients discontinued due to skin reaction.
In one foreign Phase 3 trial, one subject discontinued due to a skin-related adverse event. In the pivotal U.S. and European Phase 3 trials combined, at the 50 mg dosage strength, the percentage of subjects reporting clinically notable increases in hematocrit or hemoglobin were similar to placebo. However, in the 100 mg dose group, 2.3% and 2.8% of patients had a clinically notable increase in hemoglobin (≥ 19 gm/dL) or hematocrit (≥ 58%), respectively.
In the combined ongoing U.S. and European open label extension studies, approximately 140 patients received Testim® for at least 6 months. The preliminary results from these studies are consistent with those reported for the U.S. controlled clinical trial.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of testosterone gel products. Because the reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Secondary Exposure to Testosterone in Children
Cases of secondary exposure to testosterone resulting in virilization of children have been reported in postmarketing surveillance of testosterone gel products. Signs and symptoms of these reported cases have included enlargement of the clitoris (with surgical intervention) or of the penis, development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases with a reported outcome, these signs and symptoms were reported to have regressed with removal of the testosterone gel exposure. In a few cases, however, enlarged genitalia did not fully return to age-appropriate normal size, and bone age remained modestly greater than chronological age. In some of the cases, direct contact with the sites of application on the skin of men using testosterone gel was reported. In at least one reported case, the reporter considered the possibility of secondary exposure from items such as the testosterone gel user’s shirts and/or other fabrics, such as towels and sheets (see WARNINGS).
DRUG ABUSE AND DEPENDENCE
Testim® contains testosterone, a Schedule III controlled substance as defined by the Anabolic Steroids Control Act. Oral ingestion of Testim® will not result in clinically significant serum testosterone concentrations due to extensive first-pass metabolism.
OVERDOSAGE
There were no reports of overdose in the Testim® clinical trials. There is one report of acute overdosage by injection of testosterone enanthate: testosterone levels of up to 11,400 ng/dL were implicated in a cerebrovascular accident.
TESTIM DOSAGE AND ADMINISTRATION
The recommended starting dose of Testim® is 5 g of gel (one tube) containing 50 mg of testosterone applied once daily (preferably in the morning) to clean, dry intact skin of the shoulders and/or upper arms (area of application should be limited to the area that will be covered by the patient’s short sleeve t-shirt). Morning serum testosterone levels should then be measured approximately 14 days after initiation of therapy to ensure proper serum testosterone levels are achieved. If the serum testosterone concentration is below the normal range, or if the desired clinical response is not achieved, the daily Testim® dose may be increased from 5 g (one tube) to 10 g (two tubes) as instructed by the physician.
Upon opening the tube the entire contents should be squeezed into the palm of the hand and immediately applied to the shoulders and/or upper arms (area of application should be limited to the area that will be covered by the patient’s short sleeve t-shirt). Application sites should be allowed to dry for a few minutes prior to dressing. Hands should be washed thoroughly with soap and water after Testim® has been applied.
In order to prevent transfer to another person, clothing should be worn to cover the application sites. If direct skin-to-skin contact with another person is anticipated, the application sites must be washed thoroughly with soap and water.
In order to maintain serum testosterone levels in the normal range, the sites of application should not be washed for at least two hours after application of Testim®.
Do not apply Testim® to the genitals or to the abdomen.
HOW SUPPLIED
Testim® contains testosterone, a Schedule III controlled substance as defined by the Anabolic Steroids Control Act. Testim® is supplied in unit-dose tubes in cartons of 30. Each tube contains 50 mg testosterone in 5 g of gel, and is supplied as follows:
| NDC Number | Strength | Package Size |
| 66887-001-05 | 1% (50 mg) | 30 tubes: 5 g per tube |
Storage
Store at room temperature 25°C (77°F); Excursions permitted to 15°-30°C (59°-86°F) [See USP Controlled Room Temperature].
Disposal
Keep out of the reach of children.
Used Testim® tubes should be discarded in household trash in a manner that prevents accidental exposure of children or pets; contents flammable.
RX Only
Manufactured for:
Auxilium Pharmaceuticals, Inc.
Malvern, PA 19355 USA
By: DPT Laboratories, Ltd.
San Antonio, TX 78215
Issued: September 2009
PL-0705-001.b
129092
Medication Guide
TESTIM®
(těs TIM) 1%, CIII
(testosterone gel)
Read the Medication Guide that comes with TESTIM before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or your treatment.
What is the most important information I should know about TESTIM?
-
Early signs and symptoms of puberty have happened in young children who were accidentally exposed to testosterone through contact with men using TESTIM.
Signs and symptoms of early puberty in a child may include:- enlarged penis or clitoris
- early development of pubic hair
- increased erections or sex drive
- aggressive behavior
-
TESTIM can transfer from your body to others. Women and children should avoid contact with the unwashed or unclothed area where TESTIM has been applied to your skin.
Stop using TESTIM and call your doctor right away if you see any signs and symptoms in a child or a woman that may have occurred through accidental exposure to TESTIM.
Signs and symptoms of exposure to Testim in children may include:- enlarged penis or clitoris
- early development of pubic hair
- increased erections or sex drive
- aggressive behavior
Signs and symptoms of exposure to TESTIM in women may include:- changes in body hair
- a large increase in acne
To lower the risk of transfer of TESTIM from your body to others, you should follow these important instructions:
- Apply TESTIM only to the areas of your shoulders and upper arms that will be covered by a short sleeve T-shirt.
- Wash your hands right away with soap and water after applying TESTIM.
- After the gel has dried, cover the application area with clothing. Keep the area covered until you have washed the application area well or have showered.
- If you expect to have skin-to-skin contact with another person, first wash the application area well with soap and water.
- If a woman or child makes contact with the TESTIM application area, that area on the woman or child should be washed well with soap and water right away.
What is TESTIM?
TESTIM is a prescription medicine that contains testosterone. TESTIM is used to treat adult males who have low or no testosterone.
It is not known if TESTIM is safe or effective in children younger than 18 years old. Exposure of children to testosterone may affect bone growth.
TESTIM is a controlled substance (CIII) because it contains testosterone that can be a target for people who abuse prescription medicines. Keep your TESTIM in a safe place to protect it. Never give your TESTIM to anyone else, even if they have the same symptoms you have. Selling or giving away this medicine may harm others and it is against the law.
Who should not use TESTIM?
TESTIM is not meant for use in women.
Do not use TESTIM if you:
- have breast cancer
- have or might have prostate cancer
- are pregnant or may become pregnant or are breast-feeding. TESTIM may harm your unborn or breast-feeding baby.
Women who are pregnant or who may become pregnant should avoid contact with the area of skin where TESTIM has been applied. - are allergic to testosterone or any of the ingredients in TESTIM including soy. See the end of this Medication Guide for a complete list of ingredients in TESTIM.
Talk to your doctor before taking this medicine if you have any of the above conditions.
What should I tell my doctor before using TESTIM?
Before you use TESTIM, tell your doctor if you:
- have breast cancer or prostate cancer
- have urinary problems due to an enlarged prostate
- have heart problems
- have liver or kidney problems
- have problems breathing while you sleep (sleep apnea)
- have any other medical conditions
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
TESTIM and certain other medicines you take can affect each other.
Especially, tell your doctor if you take:
- insulin
- propranolol
- corticosteroids
Ask your doctor or pharmacist for a list of these medicines, if you are not sure.
Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine.
How should I use TESTIM?
- It is important that you apply TESTIM exactly as prescribed by your doctor. Your doctor will tell you how much TESTIM to apply and when to apply it.
- Your doctor may change your TESTIM dose. Do not change your TESTIM dose without talking to your doctor.
- Your doctor will test your blood before you start and while you take TESTIM.
- TESTIM is for skin use only.
- Apply TESTIM only to the areas of your shoulders and upper arms that will be covered by a short sleeve t-shirt. Apply TESTIM at the same time each day.
- Do not apply TESTIM to your penis, scrotum or abdomen.
To apply TESTIM:
- Remove the cap from the tube and use the top of the cap to pierce the metal seal on the top of the tube.
- Squeeze all of the TESTIM out of the tube into the palm of your hand. Squeeze from the bottom of the tube to the top.
- Apply all of the TESTIM gel to your shoulders and upper arms. Rub the gel onto your skin for several seconds until the gel is dry.
- Replace the cap and throw away the tube in the trash out of the reach of children to avoid accidental exposure.
- Wash you hands with soap and water right away after you apply TESTIM.
- Let the application areas dry for a few minutes before putting on a shirt.
- To reduce transfer of TESTIM to others, clothes (such as a t-shirt) should always be worn to cover the TESTIM application areas until you have washed the application areas well with soap and water.
- Wait at least 2 hours after applying TESTIM before showering or swimming to make sure TESTIM is absorbed into your body.
- TESTIM is flammable until dry. Let the gel dry before smoking or going near an open flame.
What are the possible side effects of TESTIM?
TESTIM can cause serious side effects including:
- See “What is the most important information I should know about TESTIM?”.
-
If you already have enlargement of your prostate gland your signs and symptoms can get worse while using TESTIM. This can include:
- increased urination at night
- trouble starting your urine stream
- having to pass urine many times during the day
- having an urge that you have to go to the bathroom right away
- having a urine accident
- being unable to pass urine or weak urine flow
- Possible increased risk of prostate cancer. Your doctor should check you for prostate cancer or any other prostate problems before you start and while you use TESTIM.
- In large doses TESTIM may lower your sperm count.
- Swelling of your ankles, feet, or body, with or without heart failure. This may cause serious problems for people who have heart, kidney or liver disease.
- Enlarged or painful breasts.
- Having problems breathing while you sleep (sleep apnea).
- Blood clots in the legs. This can include pain, swelling or redness of your legs.
Call your doctor right away if you have any of the serious side effects listed above.
The most common side effects of TESTIM include:
- skin irritation where TESTIM is applied
- increased red blood cell count
- headache
- increased blood pressure
Other side effects include more erections than are normal for you or erections that last a long time.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of TESTIM. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store TESTIM?
- Store TESTIM between 59°F to 86°F (15°C to 30°C).
- Safely throw away used TESTIM tubes in household trash. Be careful to prevent accidental exposure of children or pets.
- Keep TESTIM away from fire.
Keep TESTIM and all medicines out of the reach of children.
General information about TESTIM
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use TESTIM for a condition for which it was not prescribed. Do not give TESTIM to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about TESTIM. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about TESTIM that is written for health professionals.
For more information, go to www.TESTIM.com or call 1-877-663-0412.
What are the ingredients in TESTIM?
Active ingredient: testosterone (that may be made from soy)
Inactive ingredients: purified water, pentadecalactone, carbopol, acrylates, propylene glycol, glycerin, polyethylene glycol, ethanol (74%), and tromethamine.
This Medication Guide has been approved by the US Food and Drug Administration.
Manufactured for:
Auxilium Pharmaceuticals, Inc.
Malvern, PA 19355 USA
By: DPT Laboratories, Ltd.
San Antonio, TX 78215
Medication Guide issued: 11/2011
PL-0705-002.c
129794
Image of Label
Testimtestosterone GEL
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||