Oxymorphone hydrochloride
Lake Erie Medical DBA Quality Care Products LLC
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use oxymorphone hydrochloride extended-release tablets safely and effectively. See full prescribing information for oxymorphone hydrochloride extended-release tablets. Oxymorphone hydrochloride (Oxymorphone hydrochloride) TABLET, EXTENDED RELEASE for ORAL use.Initial U.S. Approval: 1959RECENT MAJOR CHANGESBoxed Warning 07/2012Indications and Usage (1) 07/2012Dosage and Administration (2) 07/2012Contraindications (4) 07/2012Warnings and Precautions (5) 07/2012BOXED WARNING WARNING: ABUSE POTENTIAL, LIFE-THREATENING RESPIRATORY DEPRESSION, ACCIDENTAL EXPOSURE, AND INTERACTION WITH ALCOHOL See full prescribing information for complete boxed warning. Oxymorphone hydrochloride extended-release tablets contains oxymorphone, a Schedule II controlled substance. Monitor for signs of misuse, abuse, and addiction during oxymorphone hydrochloride extended-release tablet therapy. ( 5.1 , 9 ) Fatal respiratory depression may occur, with highest risk at initiation and with dose increases. Instruct patients on proper administration of oxymorphone hydrochloride extended-release tablets to reduce the risk. ( 5.2 ) Accidental ingestion of oxymorphone hydrochloride extended-release tablets can result in fatal overdose of oxymorphone, especially in children. ( 5.3 ) Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol while taking oxymorphone hydrochloride extended-release tablets because of the risk of increased, and potentially fatal, plasma oxymorphone levels. ( 5.4 ) INDICATIONS AND USAGE Oxymorphone hydrochloride extended-release tablets are an opioid agonist indicated for the relief of moderate to severe pain in patients requiring continuous around-the-clock opioid treatment for an extended period of time. (1) Limitations of Use Oxymorphone hydrochloride extended-release tablets are not for use: As an as-needed (prn) analgesic (1) For pain that is mild or not expected to persist for an extended period of time (1) For acute pain (1) For postoperative pain, unless the patient is already receiving chronic opioid therapy prior to surgery, or if the postoperative pain is expected to be moderate to severe and persist for an extended period of time (1) DOSAGE AND ADMINISTRATION Individualize dosing based on patient’s prior analgesic treatment experience, and titrate as needed to provide adequate analgesia and minimize adverse reactions. (2.1, 2.2) Administer on an empty stomach, at least 1 hour prior to or 2 hours after eating. (2.1) Instruct patients to swallow oxymorphone hydrochloride extended-release tablets are intact. (2.4) Do not abruptly discontinue oxymorphone hydrochloride extended-release tablets in a physically dependent patient. (2.3, 5.13) Reduce the dose of oxymorphone hydrochloride extended-release tablets in patients with mild hepatic impairment and patients with renal impairment. (2.5, 2.6) DOSAGE FORMS AND STRENGTHS Extended-Release Tablets, 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, 30 mg, and 40 mg CONTRAINDICATIONS Significant respiratory depression (4) Acute or severe bronchial asthma (4) Known or suspected paralytic ileus (4) Hypersensitivity to oxymorphone (4) Moderate or severe hepatic impairment (4) WARNINGS AND PRECAUTIONS See Boxed WARNINGS Elderly, cachectic, and debilitated patients, and patients with chronic pulmonary disease: Monitor closely because of increased risk of respiratory depression. (5.5, 5.6) Interaction with CNS depressants: Consider dose reduction of one or both drugs because of additive effects. (5.7, 7.2) Hypotensive effect: Monitor during dose initiation and titration. (5.9) Patients with head injury or increased intracranial pressure: Monitor for sedation and respiratory depression. Avoid use of oxymorphone hydrochloride extended-release tablets in patients with impaired consciousness or coma susceptible to intracranial effects of CO2 retention. (5.10) Respiratory depression: Increased risk in elderly, debilitated patients, and those suffering from conditions accompanied by hypoxia, hypercapnia, or decreased respiratory reserve. (5.2) Side Effects Adverse reactions in ≥2% of patients in placebo-controlled trials: nausea, constipation, dizziness, somnolence, vomiting, pruritus, headache, sweating increased, dry mouth, sedation, diarrhea, insomnia, fatigue, appetite decreased, and abdominal pain. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Actavis at 1-800-432-8534 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS CNS depressants: Increased risk of respiratory depression, hypotension, profound sedation, coma or death. When combined therapy with CNS depressant is contemplated, the dose of one or both agents should be reduced. (7.2) Mixed agonist/antagonist opioids (i.e., pentazocine, nalbuphine, and butorphanol): May reduce analgesic effect and/or precipitate withdrawal symptoms. (7.3) USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm. (8.1) Nursing mothers: Closely monitor infants of nursing women receiving oxymorphone hydrochloride extended-release tablets. (8.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
FULL PRESCRIBING INFORMATION
RECENT MAJOR CHANGES
Abuse Potential
Oxymorphone hydrochloride extended-release tablets contains oxymorphone, an opioid agonist and Schedule II controlled substance with an abuse liability similar to other opioid agonists, legal or illicit [see Warnings and Precautions (5.1) ]. Assess each patient’s risk for opioid abuse or addiction prior to prescribing oxymorphone hydrochloride extended-release tablets. The risk for opioid abuse is increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depressive disorder). Routinely monitor all patients receiving oxymorphone hydrochloride extended-release tablets for signs of misuse, abuse, and addiction during treatment [see Drug Abuse and Dependence (9) ].
Life-threatening Respiratory Depression
Respiratory depression, including fatal cases, may occur with use of oxymorphone hydrochloride extended-release tablets, even when the drug has been used as recommended and not misused or abused [see Warnings and Precautions (5.2) ]. Proper dosing and titration are essential and oxymorphone hydrochloride extended-release tablets should only be prescribed by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain. Monitor for respiratory depression, especially during initiation of oxymorphone hydrochloride extended-release tablets or following a dose increase. Instruct patients to swallow oxymorphone hydrochloride extended-release tablets whole. Crushing, dissolving, or chewing oxymorphone hydrochloride extended-release tablets can cause rapid release and absorption of a potentially fatal dose of oxymorphone.
Accidental Exposure
Accidental ingestion of oxymorphone hydrochloride extended-release tablets, especially in children, can result in a fatal overdose of oxymorphone [see Warnings and Precautions (5.3) ].
Interaction with Alcohol
The co-ingestion of alcohol with oxymorphone hydrochloride extended-release tablets may result in an increase of plasma levels and potentially fatal overdose of oxymorphone [see Warnings and Precautions (5.4) ]. Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products that contain alcohol while on oxymorphone hydrochloride extended-release tablets.
-
Oxymorphone hydrochloride extended-release tablets are indicated for the relief of moderate to severe pain in patients requiring continuous, around-the-clock opioid treatment for an extended period of time.
Limitations of Usage
Oxymorphone hydrochloride extended-release tablets are not intended for use:
- As an as-needed (prn) analgesic
- For pain that is mild or not expected to persist for an extended period of time
- For acute pain
- For postoperative pain unless the patient is already receiving chronic opioid therapy prior to surgery or if the postoperative pain is expected to be moderate to severe and persist for an extended period of time.
Initiate the dosing regimen for each patient individually, taking into account the patient's prior analgesic treatment experience. Monitor patients closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy with oxymorphone hydrochloride extended-release tablets [see Warnings and Precautions (5.2)].
Consider the following factors when selecting an initial dose of oxymorphone hydrochloride extended-release tablets:
- Total daily dose, potency, and any prior opioid the patient has been taking previously;
- Reliability of the relative potency estimate used to calculate the equivalent dose of oxymorphone needed (Note: potency estimates may vary with the route of administration);
- Patient's degree of opioid experience and opioid tolerance;
- General condition and medical status of the patient;
- Concurrent medication;
- Type and severity of the patient's pain.
Oxymorphone hydrochloride extended-release tablets are administered at a frequency of twice daily (every 12 hours). Administer on an empty stomach, at least 1 hour prior to or 2 hours after eating.
Use of Oxymorphone Hydrochloride Extended-Release Tablets as the First Opioid Analgesic
Initiate oxymorphone hydrochloride extended-release tablet therapy with the 5 mg tablet twice daily (at 12-hour intervals). Adjust the dose of oxymorphone hydrochloride extended-release tablet in increments of 5 to 10 mg every 12 hours every 3 to 7 days.
Conversion from Oxymorphone Hydrochloride Tablets to Oxymorphone Hydrochloride Extended-Release Tablets
Patients receiving oxymorphone hydrochloride tablets may be converted to oxymorphone hydrochloride extended-release tablets by administering half the patient's total daily oral oxymorphone hydrochloride tablets dose as oxymorphone hydrochloride extended-release tablets, every 12 hours.
Conversion from Parenteral Oxymorphone to Oxymorphone Hydrochloride Extended-Release Tablets
The absolute oral bioavailability of oxymorphone hydrochloride extended-release tablets is approximately 10%. Convert patients receiving parenteral oxymorphone to oxymorphone hydrochloride extended-release tablets by administering 10 times the patient's total daily parenteral oxymorphone dose as oxymorphone hydrochloride extended-release tablets in two equally divided doses (e.g., [IV dose x 10] divided by 2). Due to patient variability with regards to opioid analgesic response, upon conversion monitor patients closely to evaluate for adequate analgesia and side effects.
Conversion from Other Oral Opioids to Oxymorphone Hydrochloride Extended-Release Tablets
While there are useful tables of oral and parenteral equivalents, there is substantial inter-patient variability in the relative potency of different opioid drugs and formulations. As such, it is safer to underestimate a patient’s 24-hour oral oxymorphone dose and provide rescue medication (e.g. immediate-release oxymorphone) than to overestimate the 24-hour oral oxymorphone dose and manage an adverse reaction. Consider the following general points:
In a Phase 3 clinical trial with an open-label titration period, patients were converted from their prior opioid to oxymorphone hydrochloride extended-release tablets using the following table as a guide for the initial oxymorphone hydrochloride extended-release tablet dose.
- The table is not a table of equianalgesic doses.
- The conversion ratios in this table are only to be used for the conversion from oral therapy with one of the listed opioid analgesics to oxymorphone hydrochloride extended-release tablets.
- Do not use this table to convert from oxymorphone hydrochloride extended-release tablets to another opioid. Doing so will result in an over-estimation of the dose of the new opioid and may result in fatal overdose.
For example, a patient receiving oxycodone at a total daily dose of 40 mg would then be converted to a total daily dose of 20 mg of oxymorphone (40 mg x 0.5), dosed as oxymorphone hydrochloride extended-release tablets 10 mg twice daily.
| Oral | ||
| Opioid | Total Daily Oral Dose | Conversion Ratio |
| Oxymorphone | 10 mg | 1 |
| Hydrocodone | 20 mg | 0.5 |
| Oxycodone | 20 mg | 0.5 |
| Methadone | 20 mg | 0.5 |
| Morphine | 30 mg | 0.333 |
Individually titrate oxymorphone hydrochloride extended-release tablets to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving oxymorphone hydrochloride extended-release tablets to assess the maintenance of pain control and the relative incidence of adverse reactions. During chronic therapy, especially for non-cancer-related pain (or pain associated with other terminal illnesses), periodically reassess the continued need for the use of opioid analgesics.
If the level of pain increases, attempt to identify the source of increased pain, while adjusting the oxymorphone hydrochloride extended-release tablet dose to decrease the level of pain. Because steady-state plasma concentrations are approximated within 3 days, oxymorphone hydrochloride extended-release tablet dosage adjustments, preferably at increments of 5 to 10 mg every 12 hours, may be done every 3 to 7 days. Patients who experience breakthrough pain may require dosage adjustment or rescue medication with a small dose of an immediate-release medication (e.g. immediate-release oxymorphone).
During chronic, around-the-clock opioid therapy, especially for non-cancer pain syndromes, reassess the continued need for around-the-clock opioid therapy periodically (e.g., every 6 to 12 months) as appropriate.
If signs of excessive opioid-related adverse reactions are observed, the next dose may be reduced. Adjust the dose to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
When a patient no longer requires therapy with oxymorphone hydrochloride extended-release tablets, use a gradual downward titration of the dose every two to four days, to prevent signs and symptoms of withdrawal in the physically-dependent patient. Do not abruptly discontinue oxymorphone hydrochloride extended-release tablets.
Instruct patients to swallow oxymorphone hydrochloride extended-release tablets intact. The tablets are not to be crushed, dissolved, or chewed due to the risk of rapid release and absorption of a potentially fatal dose of oxymorphone [see Warnings and Precautions (5.2)]. Administer on an empty stomach, at least 1 hour prior to or 2 hours after eating.
Oxymorphone hydrochloride extended-release tablets are contraindicated in patients with moderate or severe hepatic impairment.
In opioid-naïve patients with mild hepatic impairment, initiate treatment with the 5 mg dose. For patients on prior opioid therapy, start oxymorphone hydrochloride extended-release tablets at 50% lower than the starting dose for a patient with normal hepatic function on prior opioids and titrate slowly. Monitor patients closely for signs of respiratory or central nervous system depression [see Warnings and Precautions (5.2), Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
In patients with creatinine clearance rates less than 50 mL/min, start oxymorphone hydrochloride extended-release tablets in the opioid-naïve patient with the 5 mg dose. For patients on prior opioid therapy, start oxymorphone hydrochloride extended-release tablets at 50% lower than the starting dose for a patient with normal renal function on prior opioids and titrate slowly. Monitor patients closely for signs of respiratory or central nervous system depression [see Warnings and Precautions (5.2), Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
The steady-state plasma concentrations of oxymorphone are approximately 40% higher in elderly subjects than in young subjects. Initiate dosing with oxymorphone hydrochloride extended-release tablets in patients 65 years of age and over using the 5 mg dose and monitor closely for signs of respiratory and central nervous system depression when initiating and titrating oxymorphone hydrochloride extended-release tablets to adequate analgesia [see Warnings and Precautions (5.2), Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)]. For patients on prior opioid therapy, start oxymorphone hydrochloride extended-release tablets at 50% lower than the starting dose for a younger patient on prior opioids and titrate slowly.
The 5 mg dosage form is a light pink, round tablet, debossed with “ ” on one side and “227” on the other side.
” on one side and “227” on the other side.
The 7.5 mg dosage form is a gray, round tablet, debossed with “ ” on one side and “261” on the other side.
” on one side and “261” on the other side.
The 10 mg dosage form is an orange, round tablet, debossed with “ ” on one side and “228” on the other side.
” on one side and “228” on the other side.
The 15 mg dosage form is a white to off-white, round tablet, debossed with “ ” on one side and “262” on the other side.
” on one side and “262” on the other side.
The 20 mg dosage form is a light tan to tan, round tablet, debossed with “ ” on one side and “229” on the other side.
” on one side and “229” on the other side.
The 30 mg dosage form is a pink, round tablet, debossed with “ ” on one side and “263” on the other side.
” on one side and “263” on the other side.
The 40 mg dosage form is a yellow, round tablet, debossed with “ ” on one side and “230” on the other side.
” on one side and “230” on the other side.
Oxymorphone hydrochloride extended-release tablets are contraindicated in patients with:
- Significant respiratory depression
- Acute or severe bronchial asthma or hypercarbia
- Known or suspected paralytic ileus
- Moderate and severe hepatic impairment [see Clinical Pharmacology (12.3), Warnings and Precautions (5.8)].
- Hypersensitivity (e.g. anaphylaxis) to oxymorphone, any other ingredients in oxymorphone hydrochloride extended-release tablets, or to morphine analogs such as codeine [see Adverse Reactions (6.1)].
Oxymorphone hydrochloride extended-release tablets contain oxymorphone, an opioid agonist and a Schedule II controlled substance. Oxymorphone can be abused in a manner similar to other opioid agonists, legal or illicit. Opioid agonists are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing oxymorphone hydrochloride extended-release tablets in situations where there is concern about increased risks of misuse, abuse, or diversion. Concerns about abuse, addiction, and diversion should not, however, prevent the proper management of pain.
Assess each patient’s risk for opioid abuse or addiction prior to prescribing oxymorphone hydrochloride extended-release tablets. The risk for opioid abuse is increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). Patients at increased risk may still be appropriately treated with modified-release opioid formulations; however these patients will require intensive monitoring for signs of misuse, abuse, or addiction. Routinely monitor all patients receiving opioids for signs of misuse, abuse, and addiction because these drugs carry a risk for addiction even under appropriate medical use.
Misuse or abuse of oxymorphone hydrochloride extended-release tablets by crushing, chewing, snorting, or injecting the dissolved product will result in the uncontrolled delivery of the opioid and pose a significant risk that could result in overdose and death [see Overdosage (10)].
Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Respiratory depression is the primary risk of oxymorphone hydrochloride extended-release tablets. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with a “sighing” pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status [see Overdosage (10)].
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of oxymorphone hydrochloride extended-release tablets, the risk is greatest during the initiation of therapy or following a dose increase. Closely monitor patients for respiratory depression when initiating therapy with oxymorphone hydrochloride extended-release tablets and following dose increases. Instruct patients against use by individuals other than the patient for whom oxymorphone hydrochloride extended-release tablets was prescribed and to keep oxymorphone hydrochloride extended-release tablets out of the reach of children, as such inappropriate use may result in fatal respiratory depression.
To reduce the risk of respiratory depression, proper dosing and titration of oxymorphone hydrochloride extended-release tablets are essential [see Dosage and Administration (2.1, 2.2)]. Overestimating the oxymorphone hydrochloride extended-release tablets dose when converting patients from another opioid product can result in fatal overdose with the first dose. Respiratory depression has also been reported with use of modified-release opioids when used as recommended and not misused or abused.
To further reduce the risk of respiratory depression, consider the following:
- Proper dosing and titration are essential and oxymorphone hydrochloride extended-release tablets should only be prescribed by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain.
- Instruct patients to swallow oxymorphone hydrochloride extended-release tablets intact. The tablets are not to be crushed, dissolved, or chewed. The resulting oxymorphone dose may be fatal, particularly in opioid-naïve individuals.
- Oxymorphone hydrochloride extended-release tablets are contraindicated in patients with respiratory depression and in patients with conditions that increase the risk of life-threatening respiratory depression [see Contraindications (4)].
Accidental consumption of oxymorphone hydrochloride extended-release tablets, especially in children, can result in a fatal overdose of oxymorphone.
The co-ingestion of alcohol with oxymorphone hydrochloride extended-release tablets can result in an increase of oxymorphone plasma levels and potentially fatal overdose of oxymorphone. Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol while on oxymorphone hydrochloride extended-release tablet therapy [see Clinical Pharmacology (12.3)].
Respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics due to poor fat stores, muscle wasting, or altered clearance compared to younger, healthier patients. Therefore, monitor such patients closely, particularly when initiating and titrating oxymorphone hydrochloride extended-release tablets and when oxymorphone hydrochloride extended-release tablets are given concomitantly with other drugs that depress respiration [see Warnings and Precautions (5.2)].
Monitor patients with significant chronic obstructive pulmonary disease or cor pulmonale, and patients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression for respiratory depression, particularly when initiating therapy and titrating with oxymorphone hydrochloride extended-release tablets, as in these patients, even usual therapeutic doses of oxymorphone hydrochloride extended-release tablets may decrease respiratory drive to the point of apnea [see Warnings and Precautions (5.2)]. Consider the use of alternative non-opioid analgesics in these patients if possible.
Hypotension, profound sedation, coma, or respiratory depression may result if oxymorphone hydrochloride extended-release tablets are used concomitantly with other CNS depressants (e.g., sedatives, anxiolytics, hypnotics, neuroleptics, other opioids). When considering the use of oxymorphone hydrochloride extended-release tablets in a patient taking a CNS depressant, assess the duration of use of the CNS depressant and the patient’s response, including the degree of tolerance that has developed to CNS depression. Additionally, consider the patient’s use, if any, of alcohol or illicit drugs that cause CNS depression. If oxymorphone hydrochloride extended-release tablet therapy is to be initiated in a patient taking a CNS depressant, start with a lower oxymorphone hydrochloride extended-release tablet dose than usual and monitor patients for signs of sedation and respiratory depression and consider using a lower dose of the concomitant CNS depressant [see Drug Interactions (7.2)].
A study of oxymorphone hydrochloride extended-release tablets in patients with hepatic disease indicated greater plasma concentrations than those with normal hepatic function [See Clinical Pharmacology (12.3)]. Oxymorphone hydrochloride extended-release tablets are contraindicated in patients with moderate or severe hepatic impairment. In patients with mild hepatic impairment reduce the starting dose to the lowest dose and monitor for signs of respiratory and central nervous system depression [see Dosage and Administration (2.5)].
Oxymorphone hydrochloride extended-release tablets may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is an increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g. phenothiazines or general anesthetics) [see Drug Interactions (7.2)]. Monitor these patients for signs of hypotension after initiating or titrating the dose of oxymorphone hydrochloride extended-release tablets. In patients with circulatory shock, oxymorphone hydrochloride extended-release tablets may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of oxymorphone hydrochloride extended-release tablets in patients with circulatory shock.
Monitor patients taking oxymorphone hydrochloride extended-release tablets who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors) for signs of sedation and respiratory depression, particularly when initiating therapy with oxymorphone hydrochloride extended-release tablets. Oxymorphone hydrochloride extended-release tablets may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of oxymorphone hydrochloride extended-release tablets in patients with impaired consciousness or coma.
Oxymorphone hydrochloride extended-release tablets are contraindicated in patients with paralytic ileus. Avoid the use of oxymorphone hydrochloride extended-release tablets in patients with other GI obstruction.
The oxymorphone in oxymorphone hydrochloride extended-release tablets may cause spasm of the sphincter of Oddi. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms. Opioids may cause increases in the serum amylase.
The oxymorphone in oxymorphone hydrochloride extended-release tablets may aggravate convulsions in patients with convulsive disorders, and may induce or aggravate seizures in some clinical settings. Monitor patients with a history of seizure disorders for worsened seizure control during oxymorphone hydrochloride extended-release tablet therapy.
Avoid the use of mixed agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, and butorphanol) in patients who have received or are receiving a course of therapy with an opioid agonist analgesic, including oxymorphone hydrochloride extended-release tablets. In these patients, mixed agonists/antagonists analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms.
When discontinuing oxymorphone hydrochloride extended-release tablets, gradually taper the dose [see Dosage and Administration (2.3)]. Do not abruptly discontinue oxymorphone hydrochloride extended-release tablets.
Oxymorphone hydrochloride extended-release tablets may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of oxymorphone hydrochloride extended-release tablets and know how they will react to the medication.
The following serious adverse reactions are discussed elsewhere in the labeling:
- Respiratory Depression [see Warnings and Precautions (5.2)]
- Chronic Pulmonary Disease [see Warnings and Precautions (5.6)]
- Head Injuries and Increased Intracranial Pressure [see Warnings and Precautions (5.10)]
- Interactions with Other CNS Depressants [see Warnings and Precautions (5.7)]
- Hypotensive Effect [see Warnings and Precautions (5.9)]
- Gastrointestinal Effects [see Warnings and Precautions (5.11)]
- Seizures [see Warnings and Precautions (5.12)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of oxymorphone hydrochloride extended-release tablets was evaluated in a total of 2011 patients in open-label and controlled clinical trials. The clinical trials enrolled of patients with moderate to severe chronic non-malignant pain, cancer pain, and post surgical pain. The most common serious adverse events reported with administration of oxymorphone hydrochloride extended-release tablets were chest pain, pneumonia and vomiting.
Tables 1 and 2 list the most frequently occurring adverse reactions (in at least 5% of patients) from the placebo-controlled trials in patients with low back pain.
| Open-Label Titration Period | Double-Blind Treatment Period | ||
| Oxymorphone Hydrochloride | Oxymorphone Hydrochloride | ||
| Extended-Release Tablets | Extended-Release Tablets | Placebo | |
| Preferred Term | (N = 325) | (N = 105) | (N = 100) |
| Constipation | 26% | 7% | 1% |
| Somnolence | 19% | 2% | 0% |
| Nausea | 18% | 11% | 9% |
| Dizziness | 11% | 5% | 3% |
| Headache | 11% | 4% | 2% |
| Pruritus | 7% | 3% | 1% |
| Open-Label Titration Period | Double-Blind Treatment Period | ||
| Oxymorphone Hydrochloride | Oxymorphone Hydrochloride | ||
| Extended-Release Tablets | Extended-Release Tablets | Placebo | |
| Preferred Term | (N = 250) | (N = 70) | (N = 72) |
| Nausea | 20% | 3% | 1% |
| Constipation | 12% | 6% | 1% |
| Headache | 12% | 3% | 0% |
| Somnolence | 11% | 3% | 0% |
| Vomiting | 9% | 0% | 1% |
| Pruritus | 8% | 0% | 0% |
| Dizziness | 6% | 0% | 0% |
The following table lists adverse reactions that were reported in at least 2% of patients in placebo-controlled trials (N=5).
| MedDRA Preferred Term | Oxymorphone Hydrochloride Extended-Release | |
| Tablets (N=1259) | Placebo (N=461) | |
| Nausea | 33% | 13% |
| Constipation | 28% | 13% |
| Dizziness (Excl Vertigo) | 18% | 8% |
| Somnolence | 17% | 2% |
| Vomiting | 16% | 4% |
| Pruritus | 15% | 8% |
| Headache | 12% | 6% |
| Sweating increased | 9% | 9% |
| Dry mouth | 6% | <1% |
| Sedation | 6% | 8% |
| Diarrhea | 4% | 6% |
| Insomnia | 4% | 2% |
| Fatigue | 4% | 1% |
| Appetite decreased | 3% | <1% |
| Abdominal pain | 3% | 2% |
The common (≥1% to <10%) adverse drug reactions reported at least once by patients treated with oxymorphone hydrochloride extended-release tablets in the clinical trials organized by MedDRA’s (Medical Dictionary for Regulatory Activities) System Organ Class and not represented in Table 1 were:
Eye disorders: vision blurred
Gastrointestinal disorders: diarrhea, abdominal pain, dyspepsia
General disorders and administration site conditions: dry mouth, appetite decreased, fatigue, lethargy, weakness, pyrexia, dehydration, weight decreased, edema
Nervous system disorders: insomnia
Psychiatric disorders: anxiety, confusion, disorientation, restlessness, nervousness, depression
Respiratory, thoracic and mediastinal disorders: dyspnea
Vascular disorders: flushing and hypertension
Other less common adverse reactions known with opioid treatment that were seen <1% in the oxymorphone hydrochloride extended-release tablet trials include the following: Bradycardia, palpitation, syncope, tachycardia, postural hypotension, miosis, abdominal distention, ileus, hot flashes, allergic reactions, hypersensitivity, urticaria, oxygen saturation decreased, central nervous system depression, depressed level of consciousness, agitation, dysphoria, euphoric mood, hallucination, mental status changes, difficult micturition, urinary retention, hypoxia, respiratory depression, respiratory distress, clamminess, dermatitis, hypotension.
The following adverse reactions have been identified during post approval use of oxymorphone hydrochloride extended-release tablets. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Nervous system disorder: amnesia, convulsion, memory impairment
Concomitant use of alcohol with oxymorphone hydrochloride extended-release tablets can result in an increase of oxymorphone plasma levels and potentially fatal overdose of oxymorphone. Instruct patients not to consume alcoholic beverages or use prescription or non-prescription products containing alcohol while on oxymorphone hydrochloride extended-release tablet therapy [see Clinical Pharmacology (12.3)].
Concurrent use of oxymorphone hydrochloride extended-release tablets and other CNS depressants including sedatives, hypnotics, tranquilizers, general anesthetics, phenothiazines, other opioids, and alcohol can increase the risk of respiratory depression, hypotension, profound sedation, or coma. Monitor patients receiving CNS depressants and oxymorphone hydrochloride extended-release tablets for signs of respiratory depression and hypotension. When such combined therapy is contemplated, reduce the initial dose of one or both agents.
Mixed agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, butorphanol, or buprenorphine) may reduce the analgesic effect of oxymorphone hydrochloride extended-release tablets or may precipitate withdrawal symptoms in these patients. Avoid the use of mixed agonist/antagonist analgesics in patients receiving oxymorphone hydrochloride extended-release tablets.
Cimetidine can potentiate opioid-induced respiratory depression. Monitor patients for respiratory depression when oxymorphone hydrochloride extended-release tablets and cimetidine are used concurrently.
Anticholinergics or other medications with anticholinergic activity when used concurrently with opioid analgesics may result in increased risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. Monitor patients for signs of respiratory and central nervous system depression when oxymorphone hydrochloride extended-release tablets are used concurrently with anticholinergic drugs.
The safety of using oxymorphone in pregnancy has not been established with regard to possible adverse effects on fetal development. The use of oxymorphone hydrochloride extended-release tablets in pregnancy, in nursing mothers, or in women of child-bearing potential requires that the possible benefits of the drug be weighed against the possible hazards to the mother and the child.
Prolonged use of opioid analgesics during pregnancy may cause fetal-neonatal physical dependence.
Teratogenic Effects (Pregnancy Category C)
There are no adequate and well-controlled studies of oxymorphone in pregnant women. Oxymorphone hydrochloride extended-release tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus [see Use in Specific Populations (8.2)].
Oxymorphone hydrochloride administration did not cause malformations at any doses evaluated during developmental toxicity studies in rats (≤25 mg/kg/day) or rabbits (≤50 mg/kg/day). These doses are (3-fold and (12-fold the human dose of 40 mg every 12 hours, based on body surface area. There were no developmental effects in rats treated with 5 mg/kg/day or rabbits treated with 25 mg/kg/day. Fetal weights were reduced in rats and rabbits given doses of ≥10 mg/kg/day and 50 mg/kg/day, respectively. These doses are (1.2-fold and (12-fold the human dose of 40 mg every 12 hours based on body surface area, respectively. There were no effects of oxymorphone hydrochloride on intrauterine survival in rats at doses ≤25 mg/kg/day, or rabbits at ≤50 mg/kg/day in these studies (see Non-teratogenic Effects, below). In a study that was conducted prior to the establishment of Good Laboratory Practices (GLP) and not according to current recommended methodology, a single subcutaneous injection of oxymorphone hydrochloride on gestation day 8 was reported to produce malformations in offspring of hamsters that received 15.5-fold the human dose of 40 mg every 12 hours based on body surface area. This dose also produced 20% maternal lethality.
Non-teratogenic Effects
Oxymorphone hydrochloride administration to female rats during gestation in a pre- and postnatal developmental toxicity study reduced mean litter size (18%) at a dose of 25 mg/kg/day, attributed to an increased incidence of stillborn pups. An increase in neonatal death occurred at ≥5 mg/kg/day. Post-natal survival of the pups was reduced throughout weaning following treatment of the dams with 25 mg/kg/day. Low pup birth weight and decreased postnatal weight gain occurred in pups born to oxymorphone-treated pregnant rats given a dose of 25 mg/kg/day. This dose is (3-fold higher than the human dose of 40 mg every 12 hours on a body surface area basis.
Oxymorphone hydrochloride extended-release tablets are not for use in women during and immediately prior to labor, where shorter acting analgesics or other analgesic techniques are more appropriate [see Indications and Usage (1)]. Occasionally, opioid analgesics may prolong labor through by temporarily reducing the strength, duration, and frequency of uterine contractions. However, these effects are not consistent and may be offset by an increased rate of cervical dilatation which tends to shorten labor.
Opioids cross the placenta and may produce respiratory depression and psychophysiologic effects in neonates. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression. An opioid antagonist, such as naloxone, should be available for reversal of opioid-induced respiratory depression in the neonate in such situations.
It is not known whether oxymorphone is excreted in human milk. Because many drugs, including some opioids, are excreted in human milk, caution should be exercised when oxymorphone hydrochloride extended-release tablets are administered to a nursing woman. Monitor infants who may be exposed to oxymorphone hydrochloride extended-release through breast milk for excess sedation and respiratory depression. Withdrawal symptoms can occur in breast-fed infants when maternal administration of an opioid analgesic is stopped, or when breast-feeding is stopped.
The safety and effectiveness of oxymorphone hydrochloride extended-release tablets in patients below the age of 18 years have not been established.
Of the total number of subjects in clinical studies of oxymorphone hydrochloride extended-release tablets, 27% were 65 and over, while 9% were 75 and over. No overall differences in effectiveness were observed between these subjects and younger subjects. There were several adverse events that were more frequently observed in subjects 65 and over compared to younger subjects. These adverse events included dizziness, somnolence, confusion, and nausea. On average, age greater than 65 years was associated with a 1.4-fold increase in oxymorphone AUC and a 1.5-fold increase in Cmax. Initiate dosing with oxymorphone hydrochloride extended-release tablets in patients 65 years of age and over using the 5 mg dose and monitor closely for signs of respiratory and central nervous system depression when initiating and titrating oxymorphone hydrochloride extended-release tablets. For patients on prior opioid therapy, start at 50% of the starting dose for a younger patient on prior opioids and titrate slowly.
Patients with mild hepatic impairment have an increase in oxymorphone bioavailability of 1.6-fold. In opioid-naïve patients with mild hepatic impairment, initiate oxymorphone hydrochloride extended-release tablets using the 5 mg dose and monitor closely for respiratory and central nervous system depression. Oxymorphone hydrochloride extended-release tablets are contraindicated for patients with moderate and severe hepatic impairment [see Contraindications (4), Warnings and Precautions (5.8), and Dosage and Administration (2.5)]. For patients on prior opioid therapy, start at the 50% of the dose for that a patient with normal hepatic function on prior opioids and titrate slowly.
Patients with moderate to severe renal impairment were shown to have an increase in oxymorphone bioavailability ranging from 57 to 65% [see Clinical Pharmacology (12.3)]. Start opioid-naïve patients with the 5 mg dose of oxymorphone hydrochloride extended-release tablets and titrate slowly while closely monitoring for respiratory and central nervous system depression [see Dosage and Administration (2.6)]. For patients on prior opioid therapy, start at 50% of the dose for a patient with normal renal function on prior opioids and titrate slowly.
Chronic maternal use of oxymorphone during pregnancy can affect the fetus with subsequent withdrawal signs. Neonatal withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. The onset, duration and severity of neonatal withdrawal syndrome vary based on the drug used, duration of use, the dose of last maternal use, and rate of elimination of the drug by the newborn. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening and should be treated according to protocols developed by neonatology experts.
Oxymorphone hydrochloride extended-release tablets contain oxymorphone, a mu opioid agonist and a Schedule II controlled substance with an abuse liability similar to other opioids including fentanyl, hydromorphone, methadone, morphine, oxycodone and tapentadol. Oxymorphone hydrochloride extended-release tablets can be abused and is subject to criminal diversion [see Warnings and Precautions (5.1)].
The high drug content in extended release formulations adds to the risk of adverse outcomes from abuse and misuse.
All patients treated with opioids require careful monitoring for signs of abuse and addiction, since use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Drug abuse is the intentional non-therapeutic use of an over-the-counter or prescription drug, even once, for its rewarding psychological or physiological effects. Drug abuse includes, but is not limited to the following examples: the use of a prescription or over-the counter drug to get ”high”, or the use of steroids for performance enhancement and muscle build up.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and include: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance , and sometimes a physical withdrawal.
"Drug seeking" behavior is very common to addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated claims of loss of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” (visiting multiple prescribers) to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
Oxymorphone hydrochloride extended-release tablets, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful recordkeeping of prescribing information, including quantity, frequency, and renewal requests as required by state law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to reduce abuse of opioid drugs.
Risks Specific to Abuse of Oxymorphone Hydrochloride Extended-Release Tablets
Oxymorphone hydrochloride extended-release tablets are for oral use only. Abuse of oxymorphone hydrochloride extended-release tablets pose a risk of overdose and death. This risk is increased with concurrent abuse of oxymorphone hydrochloride extended-release tablets with alcohol and other substances. Taking cut, broken, chewed, crushed, or dissolved oxymorphone hydrochloride extended-release tablets enhances drug release and increases the risk of over dose and death.
Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dose reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity, e.g., naloxone, nalmefene, or mixed agonist/antagonist analgesics (pentazocine, butorphanol, buprenorphine, nalbuphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Oxymorphone hydrochloride extended-release tablets should not be abruptly discontinued [see Dosage and Administration (2.3)]. If oxymorphone hydrochloride extended-release tablets are abruptly discontinued in a physically-dependent patient, an abstinence syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including: irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations (8.2, 8.8)].
Clinical Presentation
Acute overdosage with oxymorphone is manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, sometimes, pulmonary edema, bradycardia, hypotension, and death. Marked mydriasis rather than miosis may be seen due to severe hypoxia in overdose situations.
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation if needed. Employ other supportive measures (including oxygen, vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life support techniques.
The opioid antagonists, naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to oxymorphone overdose. Such agents should be administered cautiously to patients who are known, or suspected to be, physically dependent on oxymorphone hydrochloride extended-release tablets. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute withdrawal syndrome.
Because the duration of reversal would be expected to be less than the duration of action of oxymorphone in oxymorphone hydrochloride extended-release tablets, carefully monitor the patient until spontaneous respiration is reliably reestablished. Oxymorphone hydrochloride extended-release tablets will continue to release oxymorphone adding to the oxymorphone load for up to 24 hours after administration, necessitating prolonged monitoring. If the response to opioid antagonists is suboptimal or not sustained, additional antagonist should be given as directed in the product’s prescribing information.
In an individual physically dependent on opioids, administration of an opioid receptor antagonist may precipitate an acute withdrawal. The severity of the withdrawal produced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be begun with care and by titration with smaller than usual doses of the antagonist.
Oxymorphone hydrochloride extended-release tablets are for oral use and contain oxymorphone, a semi-synthetic opioid analgesic. Oxymorphone hydrochloride extended-release tablets are supplied in 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, 30 mg,and 40 mg tablet strengths for oral administration. The tablet strength describes the amount of oxymorphone hydrochloride, USP per tablet.
The tablets contain the following inactive ingredients: colloidal silicon dioxide, hypromellose, magnesium stearate, and microcrystalline cellulose. In addition the 5 mg tablets contain titanium dioxide and red iron oxide. The 7.5 mg tablets contain titanium dioxide and black iron oxide. The 10 mg tablets contain red iron oxide and yellow iron oxide. The 15 mg tablets contain titanium dioxide and yellow iron oxide. The 20 mg tablets contain black iron oxide, titanium dioxide, and yellow iron oxide. The 30 mg tablets contain titanium dioxide and red iron oxide. The 40 mg tablets contain black iron oxide and yellow iron oxide.
The chemical name of oxymorphone hydrochloride, USP is 4, 5( -epoxy-3, 14-dihydroxy-17-methylmorphinan-6-one hydrochloride, a white or slightly off-white, odorless powder, which is sparingly soluble in alcohol and ether, but freely soluble in water. The molecular weight of oxymorphone hydrochloride is 337.80. The pKa1 and pKa2 of oxymorphone at 37°C are 8.17 and 9.54, respectively. The octanol/aqueous partition coefficient at 37°C and pH 7.4 is 0.98.
The structural formula for oxymorphone hydrochloride, USP is as follows:

Oxymorphone, an opioid agonist, is relatively selective for the mu receptor, although it can interact with other opioid receptors at higher doses.
The precise mechanism of analgesia, the principal therapeutic action of oxymorphone, is unknown. Specific central nervous system (CNS) opiate receptors and endogenous compounds with morphine-like activity have been identified throughout the brain and spinal cord and are likely to play a role in the expression and perception of analgesic effects. In addition, opioid receptors have also been identified within the peripheral nervous system (PNS). The role that these receptors play in these drugs’ analgesic effects is unknown.
Effects on the Central Nervous System (CNS)
The principal therapeutic action of oxymorphone is analgesia. Oxymorphone causes respiratory depression, in part by a direct effect on the brainstem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation. Oxymorphone depresses the cough reflex by direct effect on the cough center in the medulla.
Oxymorphone causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Overdosage (10)]. Other therapeutic effects of oxymorphone include anxiolysis, euphoria, and feeling of relaxation, drowsiness and changes in mood.
Effects on the Gastrointestinal Tract and on Other Smooth Muscle
Gastric, biliary and pancreatic secretions are decreased by oxymorphone. Oxymorphone causes a reduction in motility and is associated with an increase in tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm. The end result is constipation. Oxymorphone can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi, and transient elevations in serum amylase. Oxymorphone may also cause spasm of the sphincter of the urinary bladder.
Effects on the Cardiovascular System
Oxymorphone produces peripheral vasodilation which may result in orthostatic hypotension. Release of histamine can occur and may contribute to opioid-induced hypotension. Manifestations of histamine release may include orthostatic hypotension, pruritus, flushing, red eyes, and sweating.
Effects on the Endocrine System
Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown.
Concentration-Efficacy Relationships
The minimum effective plasma concentration of oxymorphone for analgesia varies widely among patients, especially among patients who have been previously treated with agonist opioids. As a result, individually titrate patients to achieve a balance between therapeutic and adverse effects. The minimum effective analgesic concentration of oxymorphone for any individual patient may increase over time due to an increase in pain, progression of disease, development of a new pain syndrome and/or potential development of analgesic tolerance.
Concentration-Adverse Experience Relationships
There is a general relationship between increasing opioid plasma concentration and increasing frequency of adverse experiences such as nausea, vomiting, CNS effects, and respiratory depression.
CNS Depressant/Alcohol Interaction
Additive pharmacodynamic effects may be expected when oxymorphone hydrochloride extended-release tablets are used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression.
Absorption
The absolute oral bioavailability of oxymorphone is approximately 10%.
Steady-state levels are achieved after three days of multiple dose administration. Under both single-dose and steady-state conditions, dose proportionality has been established for the 5 mg, 10 mg, 20 mg, and 40 mg doses of oxymorphone hydrochloride extended-release tablets, for both peak plasma levels (Cmax) and extent of absorption (AUC) (see Table 4).
| Regimen | Dosage | Cmax | AUC | T½ |
| (ng/mL) | (ng·hr/mL) | (hr) | ||
| NA = not applicable | ||||
| a Results after 5 days of q12h dosing. | ||||
| Single Dose | 5 mg | 0.27±0.13 | 4.54±2.04 | 11.30±10.81 |
| 10 mg | 0.65±0.29 | 8.94±4.16 | 9.83±5.68 | |
| 20 mg | 1.21±0.77 | 17.81±7.22 | 9.89±3.21 | |
| 40 mg | 2.59±1.65 | 37.90±16.20 | 9.35±2.94 | |
| Multiple Dosea | 5 mg | 0.70±0.55 | 5.60±3.87 | NA |
| 10 mg | 1.24±0.56 | 9.77±3.52 | NA | |
| 20 mg | 2.54±1.35 | 19.28±8.32 | NA | |
| 40 mg | 4.47±1.91 | 36.98±13.53 | NA | |
Food Effect
Two studies examined the effect of food on the bioavailability of single doses of 20 and 40 mg of oxymorphone hydrochloride extended-release tablets in healthy volunteers. In both studies, after the administration of oxymorphone hydrochloride extended-release tablets, the Cmax was increased by approximately 50% in fed subjects compared to fasted subjects. A similar increase in Cmax was also observed with oxymorphone solution.
The AUC was unchanged in one study and increased by approximately 18% in the other study in fed subjects following the administration of oxymorphone hydrochloride extended-release tablets. Examination of the AUC suggests that most of the difference between fed and fasting conditions occurs in the first four hours after dose administration. After oral dosing with a single dose of 40 mg, a peak oxymorphone plasma level of 2.8 ng/mL is achieved at 1 hour in fasted subjects and a peak of 4.25 ng/mL is achieved at 2 hours in fed subjects and that beyond the 12 hour time point, there is very little difference in the curves. As a result, oxymorphone hydrochloride extended-release tablets should be dosed at least one hour prior to or two hours after eating [see Dosage and Administration (2.1, 2.2)].
Distribution
Formal studies on the distribution of oxymorphone in various tissues have not been conducted. Oxymorphone is not extensively bound to human plasma proteins; binding is in the range of 10% to 12%.
Metabolism
Oxymorphone is highly metabolized, principally in the liver, and undergoes reduction or conjugation with glucuronic acid to form both active and inactive metabolites. The two major metabolites of oxymorphone are oxymorphone-3-glucuronide and 6-OH-oxymorphone. The mean plasma AUC for oxymorphone-3-glucuronide is approximately 90-fold higher than the parent compound. The pharmacologic activity of the glucuronide metabolite has not been evaluated. 6-OH-oxymorphone has been shown in animal studies to have analgesic bioactivity. The mean plasma 6-OH-oxymorphone AUC is approximately 70% of the oxymorphone AUC following single oral doses, but is essentially equivalent to the parent compound at steady-state.
Excretion
Because oxymorphone is extensively metabolized, <1% of the administered dose is excreted unchanged in the urine. On average, 33% to 38% of the administered dose is excreted in the urine as oxymorphone-3-glucuronide and less than 1% excreted as 6-OH-oxymorphone in subjects with normal hepatic and renal function. In animals given radiolabeled oxymorphone, approximately 90% of the administered radioactivity was recovered within 5 days of dosing. The majority of oxymorphone-derived radioactivity was found in the urine and feces.
Special Populations
Geriatric Patients
The steady-state plasma concentrations of oxymorphone, 6-OH-oxymorphone, and oxymorphone-3-glucuronide are approximately 40% higher in elderly subjects (( 65 years of age) than in young subjects (18 to 40 years of age). On average, age greater than 65 years was associated with a 1.4-fold increase in oxymorphone AUC and a 1.5-fold increase in Cmax. This observation does not appear related to a difference in body weight, metabolism, or excretion of oxymorphone [see Use in Specific Populations (8.5)].
Gender
The effect of gender was evaluated following single- and multiple-doses of oxymorphone hydrochloride extended-release tablets in male and female adult volunteers. There was a consistent tendency for female subjects to have slightly higher AUCSS and Cmax values than male subjects; however, gender differences were not observed when AUCSS and Cmax were adjusted by body weight.
Hepatic Impairment
The bioavailability of orally administered oxymorphone is markedly increased in patients with moderate to severe liver disease. The disposition of oxymorphone was compared in six patients with mild, five patients with moderate, and one patient with severe hepatic impairment and 12 subjects with normal hepatic function. The bioavailability of oxymorphone was increased by 1.6-fold in patients with mild hepatic impairment and by 3.7-fold in patients with moderate hepatic impairment. In one patient with severe hepatic impairment, the bioavailability was increased by 12.2-fold. The half-life of oxymorphone was not significantly affected by hepatic impairment.
Renal Impairment
Data from a pharmacokinetic study involving 24 patients with renal dysfunction show an increase of 26%, 57%, and 65% in oxymorphone bioavailability in mild (creatinine clearance 51 to 80 mL/min; n=8), moderate (creatinine clearance 30 to 50 mL/min; n=8), and severe (creatinine clearance <30 mL/min; n=8) patients, respectively, compared to healthy controls.
Drug Interaction/Alcohol Interaction
An in vivo study of the effect of alcohol (40%, 20%, 4% and 0%) on the bioavailability of a single dose of 40 mg of oxymorphone hydrochloride extended-release tablets in healthy, fasted volunteers demonstrated a highly variable effect on Cmax with concomitant administration of alcohol and oxymorphone hydrochloride extended-release tablets. The change in Cmax ranged from a decrease of 50% to an increase of 270% across all conditions studied. Following administration of 240 mL of 40% ethanol, the Cmax increased on average by 70% and up to 270% in individual subjects. Following the concomitant administration of 240 mL of 20% ethanol, the Cmax increased on average by 31% and up to 260% in individual subjects. Following the concomitant administration of 240 mL of 4 % ethanol, the Cmax increased 7% on average and by as much as 110% for individual subjects. After oral dosing with a single dose of 40 mg in fasted subjects, the mean peak oxymorphone plasma level is 2.4 ng/mL and the median Tmax is 2 hours. Following co-administration of oxymorphone hydrochloride extended-release tablets and alcohol (240 mL of 40% ethanol) in fasted subjects, the mean peak oxymorphone level is 3.9 ng/mL and the median Tmax is 1.5 hours (range 0.75 to 6 hours). The oxymorphone mean AUC was 13% higher after co-administration of 240 mL of 40% alcohol. The AUC was essentially unaffected in subjects following the co-administration of oxymorphone hydrochloride extended-release tablets and ethanol (240 mL of 20% or 4% ethanol).
In vitro studies have demonstrated that oxymorphone hydrochloride extended-release tablets does not release oxymorphone more rapidly in 500 mL of 0.1N HCl solutions containing ethanol (4%, 20%, and 40%).
Instruct patients to avoid use of alcohol when taking oxymorphone hydrochloride extended-release tablets.
In vitro studies revealed little to no biotransformation of oxymorphone to 6-OH-oxymorphone by any of the major cytochrome P450 (CYP P450) isoforms at therapeutically relevant oxymorphone plasma concentrations.
No inhibition of any of the major CYP P450 isoforms was observed when oxymorphone was incubated with human liver microsomes at concentrations of ≤15.1 mcg/mL. An inhibition of CYP3A4 activity occurred at oxymorphone concentrations ≥45.3 mcg/mL. Therefore, it is not expected that oxymorphone, or its metabolites will act as inhibitors of any of the major CYP P450 enzymes in vivo.
Increases in the activity of the CYP 2C9 and CYP 3A4 isoforms occurred when oxymorphone was incubated with human hepatocytes. However, clinical drug interaction studies with oxymorphone hydrochloride extended-release tablets showed no induction of CYP450 3A4 or 2C9 enzyme activity, indicating that no dose adjustment for CYP 3A4- or 2C9-mediated drug-drug interactions is required.
Carcinogenesis
Long-term studies have been completed to evaluate the carcinogenic potential of oxymorphone in both Sprague-Dawley rats and CD-1 mice. Oxymorphone HCl was administered to Sprague-Dawley rats (2.5, 5, and 10 mg/kg/day in males and 5, 10, and 25 mg/kg/day in females) for 2 years by oral gavage. The systemic drug exposure (AUC ng•h/mL) at the 10 mg/kg/day in male rats was 0.34-fold and at the 25 mg/kg/day dose in female rats was 1.5-fold the human exposure at a dose of 260 mg/day. No evidence of carcinogenic potential was observed in rats. Oxymorphone was administered to CD-1 mice (10, 25, 75 and 150 mg/kg/day) for 2 years by oral gavage. The systemic drug exposure (AUC ng•h/mL) at the 150 mg/kg/day dose in mice was 14.5-fold (in males) and 17.3-fold (in females) times the human exposure at a dose of 260 mg/day. No evidence of carcinogenic potential was observed in mice.
Mutagenesis
Oxymorphone hydrochloride was not mutagenic when tested in the in vitro bacterial reverse mutation assay (Ames test) at concentrations of ≤5270 mcg/plate, or in an in vitro mammalian cell chromosome aberration assay performed with human peripheral blood lymphocytes at concentrations ≤5000 mcg/mL with or without metabolic activation. Oxymorphone hydrochloride tested positive in both the rat and mouse in vivo micronucleus assays. An increase in micronucleated polychromatic erythrocytes occurred in mice given doses ≥250 mg/kg and in rats given doses of 20 and 40 mg/kg. A subsequent study demonstrated that oxymorphone hydrochloride was not aneugenic in mice following administration of up to 500 mg/kg. Additional studies indicate that the increased incidence of micronucleated polychromatic erythrocytes in rats may be secondary to increased body temperature following oxymorphone administration. Doses associated with increased micronucleated polychromatic erythrocytes also produce a marked, rapid increase in body temperature. Pretreatment of animals with sodium salicylate minimized the increase in body temperature and prevented the increase in micronucleated polychromatic erythrocytes after administration of 40 mg/kg oxymorphone.
Impairment of Fertility
Oxymorphone hydrochloride did not affect reproductive function or sperm parameters in male rats at any dose tested (≤50 mg/kg/day). The highest dose tested is (6-fold the human dose of 40 mg every 12 hours, based on body surface area. In female rats, an increase in the length of the estrus cycle and decrease in the mean number of viable embryos, implantation sites and corpora lutea were observed at doses of oxymorphone ≥10 mg/kg/day. The dose of oxymorphone associated with reproductive findings in female rats is 1.2-fold the human dose of 40 mg every 12 hours based on a body surface area. The dose of oxymorphone that produced no adverse effects on reproductive findings in female rats is 0.6-fold the human dose of 40 mg every 12 hours on a body surface area basis.
The efficacy and safety of oxymorphone hydrochloride extended-release tablets have been evaluated in double-blind, controlled clinical trials in opioid-naïve and opioid-experienced patients with moderate to severe pain including low back pain.
12-Week Study in Opioid-Naïve Patients with Low Back Pain
Patients with chronic low back pain who were suboptimally responsive to their non-opioid therapy entered a 4-week, open-label dose titration phase. Patients initiated therapy with two days of treatment with oxymorphone hydrochloride extended-release tablets 5 mg, every 12 hours. Thereafter, patients were titrated to a stabilized dose, at increments of 5 to 10 mg every 12 hours every 3 to 7 days. Of the patients who were able to stabilize within the Open-Label Titration Period, the mean±SD VAS score at Screening was 69.4±11.8 mm and at Baseline (beginning of Double-Blind Period) were 18.5±11.2 mm and 19.3±11.3 mm for the oxymorphone ER and placebo groups, respectively. Sixty three percent of the patients enrolled were able to titrate to a tolerable dose and were randomized into a 12-week double-blind treatment phase with placebo or their stabilized dose of oxymorphone hydrochloride extended-release tablets. The mean±SD stabilized doses were 39.2±26.4 mg and 40.9±25.3 mg for the oxymorphone hydrochloride extended-release tablets and placebo groups, respectively; total daily doses ranged from 10 to 140 mg. During the first 4 days of double-blind treatment patients were allowed an unlimited number of oxymorphone hydrochloride tablets, an immediate-release (IR) formulation of oxymorphone, 5 mg tablets, every 4 to 6 hours as supplemental analgesia; thereafter the number of oxymorphone hydrochloride tablets was limited to two tablets per day. This served as a tapering method to minimize opioid withdrawal symptoms in placebo patients. Sixty-eight percent of patients treated with oxymorphone hydrochloride extended-release tablets completed the 12-week treatment compared to 47% of patients treated with placebo. Oxymorphone hydrochloride extended-release tablets provided superior analgesia compared to placebo. The analgesic effect of oxymorphone hydrochloride extended-release tablets was maintained throughout the double-blind treatment period in 89% of patients who completed the study. These patients reported a decrease, no change, or a ≤10 mm increase in VAS score from Day 7 until the end of the study.
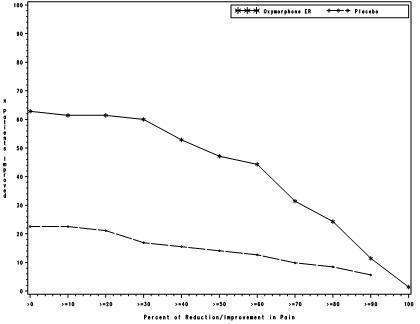
The proportion of patients with various degrees of improvement from screening to study endpoint is shown in Figure 1. The figure is cumulative, so that patients whose change from baseline is, for example, 30%, are also included at every level of improvement below 30%. Patients who did not complete the study were assigned 0% improvement.
Figure 1: Percent Reduction in Average Pain Intensity from Screening to Final Visit

12-Week Study in Opioid-Experienced Patients with Low Back Pain
Patients on chronic opioid therapy entered a 4-week, open-label titration phase with oxymorphone hydrochloride extended-release tablets dosed every 12 hours at an approximated equianalgesic dose of their pre-study opioid medication. Of the patients who were able to stabilize within the Open-Label Titration Period, the mean±SD VAS score at Screening was 69.5±17.0 mm and at Baseline (beginning of Double-Blind Period) were 23.9±12.1 mm and 22.2±10.8 mm for the oxymorphone ER and placebo groups, respectively. Stabilized patients entered a 12-week double-blind treatment phase with placebo or their stabilized dose of oxymorphone hydrochloride extended-release tablets. The mean±SD stabilized doses were 80.9±59.3 mg and 93.3±61.3 mg for the oxymorphone hydrochloride extended-release tablets and placebo groups, respectively; total daily doses ranged from 20 to 260 mg. During the first 4 days of double-blind treatment, patients were allowed an unlimited number of oxymorphone hydrochloride 5 mg tablets, every 4 to 6 hours as supplemental analgesia; thereafter the number of oxymorphone hydrochloride tablets was limited to two tablets per day. This served as a tapering method to minimize opioid withdrawal symptoms in placebo patients. Fifty seven percent of patients were titrated to a stabilized dose within approximately 4 weeks of oxymorphone hydrochloride extended-release tablets dose titration. Seventy percent of patients treated with oxymorphone hydrochloride extended-release tablets and 26% of patients treated with placebo completed the 12-week treatment. Oxymorphone hydrochloride extended-release tablets provided superior analgesia compared to placebo. The analgesic effect of oxymorphone hydrochloride extended-release tablets was maintained throughout the double-blind treatment period in 80 % of patients who completed the study. These patients reported a decrease, no change, or a ≤10 mm increase in VAS score from Day 7 until the end of the study.
The proportion of patients with various degrees of improvement from screening to study endpoint is shown in Figure 2. The figure is cumulative, so that patients whose change from baseline is, for example, 30%, are also included at every level of improvement below 30%. Patients who did not complete the study were assigned 0% improvement.
Figure 2: Percent Reduction in Average Pain Intensity from Screening to Final Visit
Oxymorphone hydrochloride extended-release tablets are supplied as follows:
5 mg
Light pink, round tablets, debossed with “ ” on one side and “227” on the other side.
” on one side and “227” on the other side.
7.5 mg
Gray, round tablets, debossed with “ ” on one side and “261” on the other side.
” on one side and “261” on the other side.
10 mg
Orange, round tablets, debossed with “ ” on one side and “228” on the other side.
” on one side and “228” on the other side.
15 mg
White to off-white, round tablets, debossed with “ ” on one side and “262” on the other side.
” on one side and “262” on the other side.
NDC: 35356-655-30 Bottles of 30
NDC: 35356-655-60 Bottles of 60
NDC: 35356-655-90 Bottles of 90
20 mg
Light tan to tan, round tablets, debossed with “ ” on one side and “229” on the other side.
” on one side and “229” on the other side.
30 mg
Pink, round tablets, debossed with “ ” on one side and “263” on the other side.
” on one side and “263” on the other side.
40 mg
Yellow, round tablets, debossed with “ ” on one side and “230” on the other side.
” on one side and “230” on the other side.
Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F). [See USP Controlled Room Temperature].
Dispense in tight container as defined in the USP, with a child-resistant closure (as required).
See FDA-approved patient labeling (Medication Guide)
Abuse Potential
Inform patients that oxymorphone hydrochloride extended-release tablets contain oxymorphone, a Schedule II controlled substance that is subject to abuse. Instruct patients not to share oxymorphone hydrochloride extended-release tablets with others and to take steps to protect oxymorphone hydrochloride extended-release tablets from theft or misuse.
Life-threatening Respiratory Depression
Discuss the risk of respiratory depression with patients, explaining that the risk is greatest when starting oxymorphone hydrochloride extended-release tablets or when the dose is increased. Advise patients how to recognize respiratory depression and to seek medical attention if they are experiencing breathing difficulties.
Accidental Exposure
Instruct patients to take steps to store oxymorphone hydrochloride extended-release tablets securely. Accidental exposure, especially in children, may result in serious harm or death. Advise patients to dispose of unused oxymorphone hydrochloride extended-release tablets by flushing the tablets down the toilet.
Risks from Concomitant Use of Alcohol and other CNS Depressants
Inform patients that the concomitant use of alcohol with oxymorphone hydrochloride extended-release tablets can increase the risk of life-threatening respiratory depression. Instruct patients not to consume alcoholic beverages, as well as prescription and over-the-counter drug products that contain alcohol, during treatment with oxymorphone hydrochloride extended-release tablets.
Inform patients that potentially serious additive effects may occur if oxymorphone hydrochloride extended-release tablets are used with other CNS depressants, and not to use such drugs unless supervised by a health care provider.
Important Administration Instructions
Instruct patients how to properly take oxymorphone hydrochloride extended-release tablets, including the following:
- Swallowing oxymorphone hydrochloride extended-release tablets whole
- Not crushing, chewing, or dissolving the tablets
- Using oxymorphone hydrochloride extended-release tablets exactly as prescribed to reduce the risk of life-threatening adverse reactions (e.g., respiratory depression)
- Not discontinuing oxymorphone hydrochloride extended-release tablets without first discussing the need for a tapering regimen with the prescriber
Hypotension
Inform patients that oxymorphone hydrochloride extended-release tablets may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position).
Driving or Operating Heavy Machinery
Inform patients that oxymorphone hydrochloride extended-release tablets may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication.
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention.
Anaphylaxis
Inform patients that anaphylaxis has been reported with ingredients contained in oxymorphone hydrochloride extended-release tablets. Advise patients how to recognize such a reaction and when to seek medical attention.
Pregnancy
Advise female patients that oxymorphone hydrochloride extended-release tablets can cause fetal harm and to inform the prescriber if they are pregnant or plan to become pregnant.
Rx Only
Manufactured by:
Actavis Elizabeth LLC
200 Elmora Avenue
Elizabeth, NJ 07207 USA
40-9113
Revised - July 2013
Oxymorphone Hydrochloride Extended-Release Tablets, CII
Rx only
Oxymorphone Hydrochloride Extended-Release Tablets are:
- A strong prescription pain medicine that contains an opioid (narcotic) that is used to treat moderate to severe around-the-clock pain.
Important information about Oxymorphone Hydrochloride Extended-Release Tablets:
- Get emergency help right away if you take too much oxymorphone hydrochloride extended-release tablets (overdose). Oxymorphone hydrochloride extended-release tablet overdose can cause life threatening breathing problems that can lead to death.
- Never give anyone else your oxymorphone hydrochloride extended-release tablets. They could die from taking it. Store oxymorphone hydrochloride extended-release tablets away from children and in a safe place to prevent stealing or abuse. Selling or giving away oxymorphone hydrochloride extended-release tablets is against the law.
Do not take Oxymorphone Hydrochloride Extended-Release Tablets if you have:
- severe asthma, trouble breathing, or other lung problems.
- a bowel blockage or have narrowing of the stomach or intestines.
Before taking Oxymorphone Hydrochloride Extended-Release Tablets, tell your healthcare provider if you have a history of:
- head injury, seizures ● liver, kidney, thyroid problems
- problems urinating ● pancreas or gallbladder problems
- abuse of street or prescription drugs, alcohol addiction, or mental health problems.
Tell your healthcare provider if you are:
- pregnant or planning to become pregnant. Oxymorphone hydrochloride extended-release tablets may harm your unborn baby.
- breastfeeding. Oxymorphone hydrochloride may pass into breast milk and may harm your baby.
- taking prescription or over-the-counter medicines, vitamins, or herbal supplements.
When taking Oxymorphone Hydrochloride Extended-Release Tablets:
- Do not change your dose. Take oxymorphone hydrochloride extended-release tablets exactly as prescribed by your healthcare provider.
- Take your prescribed dose every 12 hours at the same time every day on an empty stomach, at least 1 hour before or 2 hours after meals. Do not take more than your prescribed dose in 24 hours. If you miss a dose, take the missed dose as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule.
- Swallow oxymorphone hydrochloride extended-release tablets whole. Do not cut, break, chew, crush, dissolve, or inject oxymorphone hydrochloride extended-release tablets.
- Call your healthcare provider if the dose you are taking does not control your pain.
- Do not stop taking oxymorphone hydrochloride extended-release tablets without talking to your healthcare provider.
- After you stop taking oxymorphone hydrochloride extended-release tablets, flush any unused tablets down the toilet.
While taking Oxymorphone Hydrochloride Extended-Release Tablets Do Not:
- Drive or operate heavy machinery,until you know how oxymorphone hydrochloride extended-release tablets affect you. Oxymorphone hydrochloride extended-release tablets can make you sleepy, dizzy, or lightheaded.
- Drink alcohol or use prescription or over-the-counter medicines that contain alcohol.
The possible side effects of Oxymorphone Hydrochloride Extended-Release Tablets:
- constipation, nausea, sleepiness, vomiting, tiredness, headache, dizziness, abdominal pain.
- Call your healthcare provider if you have any of these symptoms and they are severe.
Get emergency medical help if you have:
- trouble breathing, shortness of breath, fast heartbeat, chest pain, swelling of your face, tongue or throat, extreme drowsiness, or you are feeling faint.
These are not all the possible side effects of oxymorphone hydrochloride extended-release tablets. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to dailymed.nlm.nih.gov. For more information about oxymorphone hydrochloride extended-release tablets, call Actavis at 1-800-432-8534.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Actavis Elizabeth LLC
200 Elmora Avenue
Elizabeth, NJ 07207 USA
40-9113
(MG 41-1184/0712)
Image of Label
Oxymorphone hydrochlorideOxymorphone hydrochloride TABLET, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||