Irinotecan Hydrochloride
For Intravenous Use Only
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING
- IRINOTECAN HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL STUDIES
- IRINOTECAN HYDROCHLORIDE INDICATIONS AND USAGE
- IRINOTECAN HYDROCHLORIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- IRINOTECAN HYDROCHLORIDE ADVERSE REACTIONS
- OVERDOSAGE
- IRINOTECAN HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- REFERENCES
- Irinotecan HCl Injection 40 mg Carton Label
- Irinotecan HCl Injection 100 mg Carton Label
FULL PRESCRIBING INFORMATION
WARNING
Irinotecan hydrochloride injection should be administered only under the supervision of a physician who is experienced in the use of cancer chemotherapeutic agents. Appropriate management of complications is possible only when adequate diagnostic and treatment facilities are readily available. Irinotecan hydrochloride injection can induce both early and late forms of diarrhea that appear to be mediated by different mechanisms. Both forms of diarrhea may be severe. Early diarrhea (occurring during or shortly after infusion of irinotecan hydrochloride injection) may be accompanied by cholinergic symptoms of rhinitis, increased salivation, miosis, lacrimation, diaphoresis, flushing, and intestinal hyperperistalsis that can cause abdominal cramping. Early diarrhea and other cholinergic symptoms may be prevented or ameliorated by atropine (see PRECAUTIONS, General section). Late diarrhea (generally occurring more than 24 hours after administration of irinotecan hydrochloride injection) can be life threatening since it may be prolonged and may lead to dehydration, electrolyte imbalance, or sepsis. Late diarrhea should be treated promptly with loperamide. Patients with diarrhea should be carefully monitored and given fluid and electrolyte replacement if they become dehydrated or antibiotic therapy if they develop ileus, fever, or severe neutropenia (see WARNINGS section). Administration of irinotecan hydrochloride injection should be interrupted and subsequent doses reduced if severe diarrhea occurs (see DOSAGE AND ADMINISTRATION section).
Severe myelosuppression may occur (see WARNINGS section).
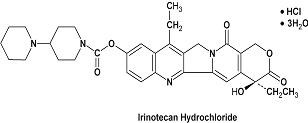
IRINOTECAN HYDROCHLORIDE DESCRIPTION
Irinotecan hydrochloride injection is an antineoplastic agent of the topoisomerase I inhibitor class. Irinotecan hydrochloride was clinically investigated as CPT-11.
Irinotecan hydrochloride injection is supplied as a sterile, pale yellow, clear, aqueous solution. It is available in two single-dose sizes: 2 mL fill vials contain 40 mg irinotecan hydrochloride and 5 mL fill vials contain 100 mg irinotecan hydrochloride. Each milliliter of solution contains 20 mg of irinotecan hydrochloride (on the basis of the trihydrate salt), 45 mg of sorbitol NF powder, 0.9 mg of lactic acid, USP. The pH of the solution has been adjusted to 3.5 (range, 3.0 to 3.8) with sodium hydroxide, NF or hydrochloric acid, NF. Irinotecan hydrochloride injection is intended for dilution with 5% Dextrose Injection, USP (D5W), or 0.9% Sodium Chloride Injection, USP, prior to intravenous infusion. The preferred diluent is 5% Dextrose Injection, USP.
Mappia foetida (S) H
3338462
CLINICAL PHARMACOLOGY
Irinotecan is a derivative of camptothecin. Camptothecins interact specifically with the enzyme topoisomerase I which relieves torsional strain in DNA by inducing reversible single-strand breaks. Irinotecan and its active metabolite SN-38 bind to the topoisomerase I-DNA complex and prevent religation of these single-strand breaks. Current research suggests that the cytotoxicity of irinotecan is due to double-strand DNA damage produced during DNA synthesis when replication enzymes interact with the ternary complex formed by topoisomerase I, DNA, and either irinotecan or SN-38. Mammalian cells cannot efficiently repair these double-strand breaks.
Irinotecan serves as a water-soluble precursor of the lipophilic metabolite SN-38. SN-38 is formed from irinotecan by carboxylesterase-mediated cleavage of the carbamate bond between the camptothecin moiety and the dipiperidino side chain. SN-38 is approximately 1000 times as potent as irinotecan as an inhibitor of topoisomerase I purified from human and rodent tumor cell lines. In vitro cytotoxicity assays show that the potency of SN-38 relative to irinotecan varies from 2- to 2000-fold. However, the plasma area under the concentration versus time curve (AUC) values for SN-38 are 2% to 8% of irinotecan and SN-38 is 95% bound to plasma proteins compared to approximately 50% bound to plasma proteins for irinotecan (see Pharmacokinetics). The precise contribution of SN-38 to the activity of irinotecan hydrochloride injection is thus unknown. Both irinotecan and SN-38 exist in an active lactone form and an inactive hydroxy acid anion form. A pH-dependent equilibrium exists between the two forms such that an acid pH promotes the formation of the lactone, while a more basic pH favors the hydroxy acid anion form.
Administration of irinotecan has resulted in antitumor activity in mice bearing cancers of rodent origin and in human carcinoma xenografts of various histological types.
Pharmacokinetics
After intravenous infusion of irinotecan in humans, irinotecan plasma concentrations decline in a multiexponential manner, with a mean terminal elimination half-life of about 6 to 12 hours. The mean terminal elimination half-life of the active metabolite SN-38 is about 10 to 20 hours. The half-lives of the lactone (active) forms of irinotecan and SN-38 are similar to those of total irinotecan and SN-38, as the lactone and hydroxy acid forms are in equilibrium.
22
|
Cmax - Maximum plasma concentration AUC0-24 - Area under the plasma concentration-time curve from time 0 to 24 hours after the end of the 90- minute infusion t½ - Terminal elimination half-life Vz - Volume of distribution of terminal elimination phase CL - Total systemic clearance a Plasma specimens collected for 24 hours following the end of the 90- minute infusion. b Plasma specimens collected for 48 hours following the end of the 90- minute infusion. Because of the longer collection period, these values provide a more accurate reflection of the terminal elimination half-lives of irinotecan and SN-38. |
|||||||||
|
Dose (mg/m2 ) |
Irinotecan
|
SN-38
|
|||||||
|
Cmax
(ng/mL) |
AUC0-24
(ng.h/mL) |
t1/2
(h) |
Vz
(L/m2) |
CL
(L/h/m2) |
Cmax
(ng/mL) |
AUC0-24
(ng.h/mL) |
t1/2
(h) |
||
| 125 (N=64) |
1,660 ± 797 |
10,200 ± 3,270 |
5.8a
± 0.7 |
110 ± 48.5 |
13.3 ± 6.01 |
26.3 ± 11.9 |
229 ± 108 |
10.4a
± 3.1 |
|
| 340 (N=6) |
3,392 ± 874 |
20,604 ± 6,027 |
11.7b
± 1 |
234 ± 69.6 |
13.9 ± 4 |
56 ± 28.2 |
474 ± 245 |
21b
± 4.3 |
|
Irinotecan exhibits moderate plasma protein binding (30% to 68% bound). SN-38 is highly bound to human plasma proteins (approximately 95% bound). The plasma protein to which irinotecan and SN-38 predominantly binds is albumin.
Metabolism and Excretion: The metabolic conversion of irinotecan to the active metabolite SN-38 is mediated by carboxylesterase enzymes and primarily occurs in the liver. In vitro studies indicate that irinotecan, SN-38 and another metabolite aminopentane carboxylic acid (APC), do not inhibit cytochrome P-450 isozymes. SN-38 is subsequently conjugated predominantly by the enzyme UDP-glucuronosyl transferase 1A1 (UGT1A1) to form a glucuronide metabolite. UGT1A1 activity is reduced in individuals with genetic polymorphisms that lead to reduced enzyme activity such as the UGT1A1*28 polymorphism. Approximately 10% of the North American population is homozygous for the UGT1A1*28 allele (also referred to as UGT1A1 7/7 genotype). In a prospective study, in which irinotecan was administered as a single-agent (350 mg/m2) on a once-every-3-week schedule, patients with the UGT1A1 7/7 genotype had a higher exposure to SN-38 than patients with the wild-type UGT1A1 allele (UGT1A1 6/6 genotype) (see WARNINGS and DOSAGE AND ADMINISTRATION sections). SN-38 glucuronide had 1/50 to 1/100 the activity of SN-38 in cytotoxicity assays using two cell lines in vitro. The disposition of irinotecan has not been fully elucidated in humans. The urinary excretion of irinotecan is 11% to 20%; SN-38, <1%; and SN-38 glucuronide, 3%. The cumulative biliary and urinary excretion of irinotecan and its metabolites (SN-38 and SN-38 glucuronide) over a period of 48 hours following administration of irinotecan in two patients ranged from approximately 25% (100 mg/m2) to 50% (300 mg/m2).
Pharmacokinetics in Special Populations
Geriatric: The pharmacokinetics of irinotecan administered using the weekly schedule was evaluated in a study of 183 patients that was prospectively designed to investigate the effect of age on irinotecan toxicity. Results from this trial indicate that there are no differences in the pharmacokinetics of irinotecan, SN-38, and SN-38 glucuronide in patients <65 years of age compared with patients ≥65 years of age. In a study of 162 patients that was not prospectively designed to investigate the effect of age, small (less than 18%) but statistically significant differences in dose-normalized irinotecan pharmacokinetic parameters in patients <65 years of age compared to patients ≥65 years of age were observed. Although dose-normalized AUC0-24 for SN-38 in patients ≥65 years of age was 11% higher than in patients <65 years of age, this difference was not statistically significant. No change in the starting dose is recommended for geriatric patients receiving the weekly dosage schedule of irinotecan. (see DOSAGE AND ADMINISTRATION section).
Pediatric: See Pediatric Use under PRECAUTIONS section
Gender: The pharmacokinetics of irinotecan do not appear to be influenced by gender.
Race: The influence of race on the pharmacokinetics of irinotecan has not been evaluated.
Hepatic Insufficiency: DOSAGE AND ADMINISTRATION PRECAUTIONS: Patients at Particular Risk sections .
Renal Insufficiency: The influence of renal insufficiency on the pharmacokinetics of irinotecan has not been evaluated. Therefore, caution should be undertaken in patients with impaired renal function. Irinotecan is not recommended for use in patients on dialysis.
Drug-Drug Interactions
Anticonvulsants: Exposure to irinotecan and its active metabolite SN-38 is substantially reduced in adult and pediatric patients concomitantly receiving the CYP3A4 enzyme-inducing anticonvulsants phenytoin, phenobarbital or carbamazepine. The appropriate starting dose for patients taking these anticonvulsants has not been formally defined. The following drugs are also CYP3A4 inducers: rifampin, rifabutin. For patients requiring anticonvulsant treatment, consideration should be given to substituting non-enzyme inducing anticonvulsants at least 2 weeks prior to initiation of irinotecan therapy. Dexamethasone does not appear to alter the pharmacokinetics of irinotecan.
St. John’s Wort: St. John’s Wort is an inducer of CYP3A4 enzymes. Exposure to the active metabolite SN-38 is reduced in patients receiving concomitant St. John’s Wort. St. John’s Wort should be discontinued at least 2 weeks prior to the first cycle of irinotecan, and St. John’s Wort is contraindicated during irinotecan therapy.
Ketoconazole: Ketoconazole is a strong inhibitor of CYP3A4 enzymes. Patients receiving concomitant ketoconazole have increased exposure to irinotecan and its active metabolite SN-38. Patients should discontinue ketoconazole at least 1 week prior to starting irinotecan therapy and ketoconazole is contraindicated during irinotecan therapy.
Neuromuscular blocking agents: Interaction between irinotecan and neuromuscular blocking agents cannot be ruled out. Irinotecan has anticholinesterase activity, which may prolong the neuromuscular blocking effects of suxamethonium and the neuromuscular blockade of non-depolarizing drugs may be antagonized.
Atazanavir sulfate: Coadministration of atazanavir sulfate, a CYP3A4 and UGT1A1 inhibitor has the potential to increase systemic exposure of SN-38, the active metabolite of irinotecan. Physicians should take this into consideration when co-administering these drugs.
CLINICAL STUDIES
DOSAGE AND ADMINISTRATION
Second-Line Treatment for Recurrent or Progressive Metastatic Colorectal Cancer After 5-FU-Based Treatment
Weekly Dosage Schedule
222222
|
a Nine patients received 150 mg/m2 as a starting dose; two (22.2%) responded to irinotecan hydrochloride injection. b Relative dose intensity for irinotecan hydrochloride injection based on planned dose intensity of 100, 83.3, and 66.7 mg/m2/wk corresponding with 150, 125, and 100 mg/m2 starting doses, respectively. c Confirmed ≥ 4 to 6 weeks after first evidence of objective response. |
||||
| Study | ||||
| 1 | 2 | 3 | ||
| Number of Patients |
48 |
90 |
64 |
102 |
| Starting Dose (mg/m2/wk x 4) |
125a
|
125 |
125 |
100 |
|
Demographics and Treatment Administration
|
||||
| Female/Male (%) |
46/54 |
36/64 |
50/50 |
51/49 |
| Median Age in years (range) |
63 (29-78) |
63 (32-81) |
61 (42-84) |
64 (25-84) |
| Ethnic Origin (%) White African American Hispanic Oriental/Asian |
79 12 8 0 |
96 4 0 0 |
81 11 8 0 |
91 5 2 2 |
| Performance Status (%) 0 1 2 |
60 38 2 |
38 48 14 |
59 33 8 |
44 51 5 |
| Primary Tumor (%) Colon Rectum Unknown |
100 0 0 |
71 29 0 |
89 11 0 |
87 8 5 |
| Prior 5-FU Therapy (%) For Metastatic Disease ≤ 6 months after Adjuvant > 6 months after Adjuvant Classification Unknown |
81 15 2 2 |
66 7 16 12 |
73 27 0 0 |
68 28 2 3 |
| Prior Pelvic/Abdominal Irradiation (%) Yes Other None |
3 0 97 |
29 9 62 |
0 2 98 |
0 4 96 |
| Duration of Treatment with irinotecan hydrochloride injection (median, months) |
5 |
4 |
4 |
3 |
| Relative Dose Intensityb (median %) |
74 |
67 |
73 |
81 |
|
Efficacy
|
||||
| Confirmed Objective Response Rate (%)c
(95% CI) |
21 (9.3 - 32.3) |
13 (6.3 - 20.4) |
14 (5.5 - 22.6) |
9 (3.3 - 14.3) |
| Time to Response (median, months) |
2.6 |
1.5 |
2.8 |
2.8 |
| Response Duration (median, months) |
6.4 |
5.9 |
5.6 |
6.4 |
| Survival (median, months) |
10.4 |
8.1 |
10.7 |
9.3 |
| 1 Year Survival (%) |
46 |
31 |
45 |
43 |
In the intent-to-treat analysis of the pooled data across all three studies, 193 of the 304 patients began therapy at the recommended starting dose of 125 mg/m2. Among these 193 patients, 2 complete and 27 partial responses were observed, for an overall response rate of 15% (95% Confidence Interval [CI], 10% to 20.1%) at this starting dose. A considerably lower response rate was seen with a starting dose of 100 mg/m2. The majority of responses were observed within the first two cycles of therapy, but responses did occur in later cycles of treatment (one response was observed after the eighth cycle). The median response duration for patients beginning therapy at 125 mg/m2 was 5.8 months (range, 2.6 to 15.1 months). Of the 304 patients treated in the three studies, response rates to irinotecan hydrochloride injection were similar in males and females and among patients older and younger than 65 years. Rates were also similar in patients with cancer of the colon or cancer of the rectum and in patients with single and multiple metastatic sites. The response rate was 18.5% in patients with a performance status of 0 and 8.2% in patients with a performance status of 1 or 2. Patients with a performance status of 3 or 4 have not been studied. Over half of the patients responding to irinotecan hydrochloride injection had not responded to prior 5-FU. Patients who had received previous irradiation to the pelvis responded to irinotecan hydrochloride injection at approximately the same rate as those who had not previously received irradiation.
Once-Every-3-Week Dosage Schedule
Single-Arm Studies: Data from an open-label, single-agent, single-arm, multicenter, clinical study involving a total of 132 patients support a once every-3-week dosage schedule of irinotecan in the treatment of patients with metastatic cancer of the colon or rectum that recurred or progressed following treatment with 5-FU. Patients received a starting dose of 350 mg/m2 given by 30-minute intravenous infusion once every 3 weeks. Among the 132 previously treated patients in this trial, the intent-to-treat response rate was 12.1% (95% CI, 7% to 18.1%).
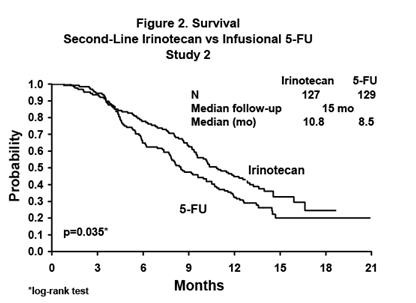
Randomized Trials: Two multicenter, randomized, clinical studies further support the use of irinotecan given by the once-every-3-week dosage schedule in patients with metastatic colorectal cancer whose disease has recurred or progressed following prior 5-FU therapy. In the first study, second-line irinotecan therapy plus best supportive care was compared with best supportive care alone. In the second study, second-line irinotecan therapy was compared with infusional 5-FU-based therapy. In both studies, irinotecan was administered intravenously at a starting dose of 350 mg/m2 over 90 minutes once every 3 weeks. The starting dose was 300 mg/m2 for patients who were 70 years and older or who had a performance status of 2. The highest total dose permitted was 700 mg. Dose reductions and/or administration delays were permitted in the event of severe hematologic and/or nonhematologic toxicities while on treatment. Best supportive care was provided to patients in both arms of Study 1 and included antibiotics, analgesics, corticosteroids, transfusions, psychotherapy, or any other symptomatic therapy as clinically indicated. In both studies, concomitant medications such as antiemetics, atropine, and loperamide were given to patients for prophylaxis and/or management of symptoms from treatment. If late diarrhea persisted for greater than 24 hours despite loperamide, a 7 day course of fluoroquinolone antibiotic prophylaxis was given. Patients in the control arm of the second study received one of the following 5-FU regimens: (1) LV, 200 mg/m2 IV over 2 hours; followed by 5-FU, 400 mg/m2 IV bolus; followed by 5-FU, 600 mg/m2 continuous IV infusion over 22 hours on days 1 and 2 every 2 weeks; (2) 5-FU, 250 to 300 mg/m2/day protracted continuous IV infusion until toxicity; (3) 5-FU, 2.6 to 3 g/m2 IV over 24 hours every week for 6 weeks with or without LV, 20 to 500 mg/m2/day every week IV for 6 weeks with 2-week rest between cycles. Patients were to be followed every 3 to 6 weeks for 1 year.
A total of 535 patients were randomized in the two studies at 94 centers. The primary endpoint in both studies was survival. The studies demonstrated a significant overall survival advantage for irinotecan compared with best supportive care (p=0.0001) and infusional 5-FU-based therapy (p=0.035) as shown in Figures 1 and 2. In Study 1, median survival for patients treated with irinotecan was 9.2 months compared with 6.5 months for patients receiving best supportive care. In Study 2, median survival for patients treated with irinotecan was 10.8 months compared with 8.5 months for patients receiving infusional 5-FU-based therapy. Multiple regression analyses determined that patients’ baseline characteristics also had a significant effect on survival. When adjusted for performance status and other baseline prognostic factors, survival among patients treated with irinotecan remained significantly longer than in the control populations (p=0.001 for Study 1 and p=0.017 for Study 2). Measurements of pain, performance status, and weight loss were collected prospectively in the two studies; however, the plan for the analysis of these data was defined retrospectively. When comparing irinotecan with best supportive care in Study 1, this analysis showed a statistically significant advantage for irinotecan, with longer time to development of pain (6.9 months versus 2 months), time to performance status deterioration (5.7 months versus 3.3 months), and time to >5% weight loss (6.4 months versus 4.2 months). Additionally, 33.3% (33/99) of patients with a baseline performance status of 1 or 2 showed an improvement in performance status when treated with irinotecan versus 11.3% (7/62) of patients receiving best supportive care (p=0.002). Because of the inclusion of patients with non-measurable disease, intent-to-treat response rates could not be assessed.

In the two randomized studies, the EORTC QLQ-C30 instrument was utilized. At the start of each cycle of therapy, patients completed a questionnaire consisting of 30 questions, such as “Did pain interfere with daily activities?” (1 = Not at All, to 4 = Very Much) and “Do you have any trouble taking a long walk?” (Yes or No). The answers from the 30 questions were converted into 15 subscales, that were scored from 0 to 100, and the global health status subscale that was derived from two questions about the patient’s sense of general well being in the past week. In addition to the global health status subscale, there were five functional (i.e., cognitive, emotional, social, physical, role) and nine symptom (i.e., fatigue, appetite loss, pain assessment, insomnia, constipation, dyspnea, nausea/vomiting, financial impact, diarrhea) subscales. The results as summarized in Table 4 are based on patients’ worst post-baseline scores. In Study 1, a multivariate analysis and univariate analyses of the individual subscales were performed and corrected for multivariate testing. Patients receiving irinotecan reported significantly better results for the global health status, on two of five functional subscales, and on four of nine symptom subscales. As expected, patients receiving irinotecan noted significantly more diarrhea than those receiving best supportive care. In Study 2, the multivariate analysis on all 15 subscales did not indicate a statistically significant difference between irinotecan and infusional 5-FU.
|
aBSC = best supportive care bRelative dose intensity for irinotecan based on planned dose intensity of 116.7 and 100 mg/m2/wk corresponding with 350 and 300 mg/m2 starting doses, respectively. |
||||
|
|
Study 1 |
Study 2 |
||
| Irinotecan |
BSCa
|
Irinotecan |
5-FU |
|
| Number of Patients |
189 |
90 |
127 |
129 |
|
Demographics and Treatment Administration
|
||||
| Female/Male (%) |
32/68 |
42/58 |
43/57 |
35/65 |
| Median Age in years (range) |
59 (22-75) |
62 (34-75) |
58 (30-75) |
58 (25-75) |
| Performance Status (%) 0 1 2 |
47 39 14 |
31 46 23 |
58 35 8 |
54 43 3 |
| Primary Tumor (%) Colon Rectum |
55 45 |
52 48 |
57 43 |
62 38 |
| Prior 5-FU Therapy (%) For Metastatic Disease As Adjuvant Treatment |
70 30 |
63 37 |
58 42 |
68 32 |
| Prior Irradiation (%) |
26 |
27 |
18 |
20 |
| Duration of Study Treatment (median, months) (Log-rank test) |
4.1 |
-- |
4.2 (p=0.02) |
2.8 |
| Relative Dose Intensity (median %)b
|
94 |
-- |
95 |
81-99 |
|
Survival
|
||||
| Survival (median, months) (Log-rank test) |
9.2 (p=0.0001) |
6.5 |
10.8 (p=0.035) |
8.5 |
| QLQ-C30 Subscale | Study 1 | Study 2 | ||||
|---|---|---|---|---|---|---|
| Irinotecan | BSC | p-value | Irinotecan | 5-FU | p-value | |
| a For the five functional subscales and global health status subscale, higher scores imply better functioning, whereas, on the nine symptom subscales, higher scores imply more severe symptoms. The subscale scores of each patient were collected at each visit until the patient dropped out of the study. | ||||||
| Global health Status | 47 | 37 | 0.03 | 53 | 52 | 0.9 |
| Functional Scales | ||||||
| Cognitive | 77 | 68 | 0.07 | 79 | 83 | 0.9 |
| Emotional | 68 | 64 | 0.4 | 64 | 68 | 0.9 |
| Social | 58 | 47 | 0.06 | 65 | 67 | 0.9 |
| Physical | 60 | 40 | 0.0003 | 66 | 66 | 0.9 |
| Role | 53 | 35 | 0.02 | 54 | 57 | 0.9 |
| Symptoms Scales | ||||||
| Fatigue | 51 | 63 | 0.03 | 47 | 46 | 0.9 |
| Appetite Loss | 37 | 57 | 0.0007 | 35 | 38 | 0.9 |
| Pain Assessment | 41 | 56 | 0.009 | 38 | 34 | 0.9 |
| Insomnia | 39 | 47 | 0.3 | 39 | 33 | 0.9 |
| Constipation | 28 | 41 | 0.03 | 25 | 19 | 0.9 |
| Dyspnea | 31 | 40 | 0.2 | 25 | 24 | 0.9 |
| Nausea/Vomiting | 27 | 29 | 0.5 | 25 | 16 | 0.09 |
| Financial Impact | 22 | 26 | 0.5 | 24 | 15 | 0.3 |
| Diarrhea | 32 | 19 | 0.01 | 32 | 22 | 0.2 |
IRINOTECAN HYDROCHLORIDE INDICATIONS AND USAGE
IRINOTECAN HYDROCHLORIDE CONTRAINDICATIONS
Irinotecan hydrochloride injection is contraindicated in patients with a known hypersensitivity to the drug or its excipients.
WARNINGS
General
Outside of a well-designed clinical study, Irinotecan hydrochloride injection should not be used in combination with the “Mayo Clinic” regimen of 5-FU/LV (administration for 4-5 consecutive days every 4 weeks) because of reports of increased toxicity, including toxic deaths. Irinotecan hydrochloride injection should be used as recommended (see DOSAGE AND ADMINISTRATION section ).
Diarrhea
Irinotecan hydrochloride injection can induce both early and late forms of diarrhea that appear to be mediated by different mechanisms. Early diarrhea (occurring during or shortly after infusion of irinotecan hydrochloride injection) is cholinergic in nature. It is usually transient and only infrequently is severe. It may be accompanied by symptoms of rhinitis, increased salivation, miosis, lacrimation, diaphoresis, flushing, and intestinal hyperperistalsis that can cause abdominal cramping. Early diarrhea and other cholinergic symptoms may be prevented or ameliorated by administration of atropine (see PRECAUTIONS, General, for dosing recommendations for atropine section ).
Late diarrhea (generally occurring more than 24 hours after administration of irinotecan hydrochloride injection) can be life threatening since it may be prolonged and may lead to dehydration, electrolyte imbalance, or sepsis. Late diarrhea should be treated promptly with loperamide (see PRECAUTIONS, Information for Patients, for dosing recommendations for loperamide, section ). Patients with diarrhea should be carefully monitored, should be given fluid and electrolyte replacement if they become dehydrated, and should be given antibiotic support if they develop ileus, fever, or severe neutropenia. After the first treatment, subsequent weekly chemotherapy treatments should be delayed in patients until return of pretreatment bowel function for at least 24 hours without need for antidiarrhea medication. If grade 2, 3, or 4 late diarrhea occurs subsequent doses of irinotecan hydrochloride injection should be decreased within the current cycle (see DOSAGE AND ADMINISTRATION section).
Neutropenia
Deaths due to sepsis following severe neutropenia have been reported in patients treated with irinotecan hydrochloride injection. Neutropenic complications should be managed promptly with antibiotic support (see PRECAUTIONS section). Therapy with irinotecan hydrochloride injection should be temporarily omitted during a cycle of therapy if neutropenic fever occurs or if the absolute neutrophil count drops <1000/mm3. After the patient recovers to an absolute neutrophil count ≥1000/mm3, subsequent doses of irinotecan hydrochloride injection should be reduced depending upon the level of neutropenia observed (see DOSAGE AND ADMINISTRATION section).
Routine administration of a colony-stimulating factor (CSF) is not necessary, but physicians may wish to consider CSF use in individual patients experiencing significant neutropenia.
Patients with Reduced UGT1A1 Activity
Individuals who are homozygous for the UGT1A1*28 allele (UGT1A1 7/7 genotype)are at increased risk for neutropenia following initiation of irinotecan hydrochloride injection treatment.
In a study of 66 patients who received single-agent irinotecan hydrochloride injection (350 mg/m2 once-every-3-weeks), the incidence of grade 4 neutropenia in patients homozygous for the UGT1A1*28 allele was 50%, and in patients heterozygous for this allele (UGT1A1 6/7 genotype) the incidence was 12.5%. No grade 4 neutropenia was observed in patients homozygous for the wild-type allele (UGT1A1 6/6 genotype).
When administered as a single-agent, a reduction in the starting dose by at least one level of irinotecan hydrochloride injection should be considered for patients known to be homozygous for the UGT1A1*28 allele. However, the precise dose reduction in this patient population is not known and subsequent dose modifications should be considered based on individual patient tolerance to treatment (see DOSAGE AND ADMINISTRATION and PRECAUTIONS, Laboratory Tests section ).
Hypersensitivity
Hypersensitivity reactions including severe anaphylactic or anaphylactoid reactions have been observed.
Colitis/Ileus
Cases of colitis complicated by ulceration, bleeding, ileus, and infection have been observed. Patients experiencing ileus should receive prompt antibiotic support (see PRECAUTIONS section).
Renal Impairment/Renal Failure
Rare cases of renal impairment and acute renal failure have been identified, usually in patients who became volume depleted from severe vomiting and/or diarrhea.
Thromboembolism
Thromboembolic events have been observed in patients receiving irinotecan-containing regimens; the specific cause of these events has not been determined.
Pulmonary Toxicity
Interstitial Pulmonary Disease (IPD)-like events, including fatalities, have been reported in patients receiving irinotecan (as monotherapy) for treatment of colorectal cancer and other advanced solid tumors. In the event of an acute onset of new or progressive, unexplained pulmonary symptoms such as dyspnea, cough, and fever, irinotecan and other co-prescribed chemotherapeutic agents should be interrupted pending diagnostic evaluation. If IPD is diagnosed, irinotecan and other chemotherapy should be discontinued and appropriate treatment instituted as needed (see ADVERSE REACTIONS: Overview of Adverse Events: Respiratory section ).
Pregnancy
14max2max22max22PRECAUTIONS
General
Care of Intravenous Site: Irinotecan hydrochloride injection is administered by intravenous infusion. Care should be taken to avoid extravasation, and the infusion site should be monitored for signs of inflammation. Should extravasation occur, flushing the site with sterile water and applications of ice are recommended.
Premedication with Antiemetics: Irinotecan is emetigenic. It is recommended that patients receive premedication with antiemetic agents. In clinical studies of the weekly dosage schedule, the majority of patients received 10 mg of dexamethasone given in conjunction with another type of antiemetic agent, such as a 5-HT3 blocker (e.g., ondansetron or granisetron). Antiemetic agents should be given on the day of treatment, starting at least 30 minutes before administration of irinotecan hydrochloride injection. Physicians should also consider providing patients with an antiemetic regimen (e.g., prochlorperazine) for subsequent use as needed.
Treatment of Cholinergic Symptoms: Prophylactic or therapeutic administration of 0.25 to 1 mg of intravenous or subcutaneous atropine should be considered (unless clinically contraindicated) in patients experiencing rhinitis, increased salivation, miosis, lacrimation, diaphoresis, flushing, abdominal cramping, or diarrhea (occurring during or shortly after infusion of irinotecan hydrochloride injection). These symptoms are expected to occur more frequently with higher irinotecan doses.
Immunosuppressant Effects/Increased Susceptibility to Infections: Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents including irinotecan hydrochloride injection, may result in serious or fatal infections. Avoid vaccination with a live vaccine in patients receiving irinotecan. Killed or inactivated vaccines may be administered; however, the response to such vaccines may be diminished.
Patients at Particular Risk: The use of irinotecan hydrochloride injection in patients with significant hepatic dysfunction has not been established. In clinical trials of either dosing schedule, irinotecan was not administered to patients with serum bilirubin >2 mg/dL, or transaminase >3 times the upper limit of normal if no liver metastasis, or transaminase >5 times the upper limit of normal with liver metastasis. In clinical trials of the weekly dosage schedule, patients with modestly elevated baseline serum total bilirubin levels (1 to 2 mg/dL) had a significantly greater likelihood of experiencing first-cycle, grade 3 or 4 neutropenia than those with bilirubin levels that were less than 1 mg/dL (50% [19/38] versus 18% [47/226]; p<0.001). (Also see CLINICAL PHARMACOLOGY: Pharmacokinetics in Special Populations: Hepatic Insufficiency, section ). Patients with deficient glucuronidation of bilirubin, such as those with Gilbert’s syndrome, may be at greater risk of myelosuppression when receiving therapy with irinotecan hydrochloride injection.
Ketoconazole, enzyme-inducing anticonvulsants and St. John’s Wort are known to have drug-drug interactions with irinotecan therapy. (See Drug-Drug Interactions sub-section under CLINICAL PHARMACOLOGY section )
Irinotecan commonly causes neutropenia, leucopenia, and anemia, any of which may be severe and therefore should not be used in patients with severe bone marrow failure. Patients must not be treated with irinotecan until resolution of the bowel obstruction. Patients with hereditary fructose intolerance should not be given Irinotecan hydrochloride injection, as this product contains sorbitol.
Information for Patients
Patients and patients’ caregivers should be informed of the expected toxic effects of irinotecan hydrochloride injection, particularly of its gastrointestinal complications, such as nausea, vomiting, abdominal cramping, diarrhea, and infection. Each patient should be instructed to have loperamide readily available and to begin treatment for late diarrhea (generally occurring more than 24 hours after administration of irinotecan hydrochloride injection) at the first episode of poorly formed or loose stools or the earliest onset of bowel movements more frequent than normally expected for the patient. One dosage regimen for loperamide used in clinical trials consisted of the following (Note: This dosage regimen exceeds the usual dosage recommendations for loperamide.): 4 mg at the first onset of late diarrhea and then 2 mg every 2 hours until the patient is diarrhea-free for at least 12 hours. Loperamide is not recommended to be used for more than 48 consecutive hours at these doses, because of the risk of paralytic ileus. During the night, the patient may take 4 mg of loperamide every 4 hours. Premedication with loperamide is not recommended. The use of drugs with laxative properties should be avoided because of the potential for exacerbation of diarrhea. Patients should be advised to contact their physician to discuss any laxative use.
Patients should be instructed to contact their physician or nurse if any of the following occur: diarrhea for the first time during treatment; black or bloody stools; symptoms of dehydration such as lightheadedness, dizziness, or faintness; inability to take fluids by mouth due to nausea or vomiting; inability to get diarrhea under control within 24 hours; or fever or evidence of infection.
Patients should be warned about the potential for dizziness or visual disturbances which may occur within 24 hours following the administration of irinotecan hydrochloride injection, and advised not to drive or operate machinery if these symptoms occur.
Patients should be alerted to the possibility of alopecia.
Laboratory Tests
Careful monitoring of the white blood cell count with differential, hemoglobin, and platelet count is recommended before each dose of irinotecan hydrochloride injection.
UGT1A1 Testing
WARNINGSDrug Interactions
The adverse effects of irinotecan hydrochloride injection, such as myelosuppression and diarrhea, would be expected to be exacerbated by other antineoplastic agents having similar adverse effects.
Patients who have previously received pelvic/abdominal irradiation are at increased risk of severe myelosuppression following the administration of irinotecan hydrochloride injection. The concurrent administration of irinotecan hydrochloride injection with irradiation has not been adequately studied and is not recommended.
Lymphocytopenia has been reported in patients receiving irinotecan hydrochloride injection, and it is possible that the administration of dexamethasone as antiemetic prophylaxis may have enhanced the likelihood of this effect. However, serious opportunistic infections have not been observed, and no complications have specifically been attributed to lymphocytopenia.
Hyperglycemia has also been reported in patients receiving irinotecan hydrochloride injection. Usually, this has been observed in patients with a history of diabetes mellitus or evidence of glucose intolerance prior to administration of irinotecan hydrochloride injection. It is probable that dexamethasone, given as antiemetic prophylaxis, contributed to hyperglycemia in some patients.
The incidence of akathisia in clinical trials of the weekly dosage schedule was greater (8.5%, 4/47 patients) when prochlorperazine was administered on the same day as irinotecan hydrochloride injection than when these drugs were given on separate days (1.3%, 1/80 patients). The 8.5% incidence of akathisia, however, is within the range reported for use of prochlorperazine when given as a premedication for other chemotherapies.
It would be expected that laxative use during therapy with irinotecan hydrochloride injection would worsen the incidence or severity of diarrhea, but this has not been studied.
In view of the potential risk of dehydration secondary to vomiting and/or diarrhea induced by irinotecan hydrochloride injection, the physician may wish to withhold diuretics during dosing with irinotecan hydrochloride injection and, certainly, during periods of active vomiting or diarrhea.
Drug-Laboratory Test Interactions
There are no known interactions between irinotecan hydrochloride injection and laboratory tests.
Carcinogenesis, Mutagenesis and Impairment of Fertility
max2in vitroin vivomax2max2
Pregnancy
WARNINGS
Nursing Mothers
Pediatric Use
The effectiveness of irinotecan in pediatric patients has not been established. Results from two open-label, single arm studies were evaluated. One hundred and seventy children with refractory solid tumors were enrolled in one phase 2 trial in which 50 mg/m2 of irinotecan was infused for 5 consecutive days every 3 weeks. Grade 3 to 4 neutropenia was experienced by 54 (31.8%) patients. Neutropenia was complicated by fever in 15 (8.8%) patients. Grade 3 to 4 diarrhea was observed in 35 (20.6%) patients. This adverse event profile was comparable to that observed in adults. In the second phase 2 trial of 21 children with previously untreated rhabdomyosarcoma, 20 mg/m2 of irinotecan was infused for 5 consecutive days on weeks 0, 1, 3 and 4. This single agent therapy was followed by multimodal therapy. Accrual to the single agent irinotecan phase was halted due to the high rate (28.6%) of progressive disease and the early deaths (14%). The adverse event profile was different in this study from that observed in adults; the most significant grade 3 or 4 adverse events were dehydration experienced by 6 patients (28.6%) associated with severe hypokalemia in 5 patients (23.8%) and hyponatremia in 3 patients (14.3%); in addition Grade 3 to 4 infection was reported in 5 patients (23.8%) (across all courses of therapy and irrespective of causal relationship).
Pharmacokinetic parameters for irinotecan and SN-38 were determined in 2 pediatric solid-tumor trials at dose levels of 50 mg/m2 (60 min infusion, n=48) and 125 mg/m2 (90 min infusion, n=6). Irinotecan clearance (mean ± S.D.) was 17.3 ± 6.7 L/h/m2 for the 50 mg/m2 dose and 16.2 ± 4.6 L/h/m2 for the 125 mg/m2 dose, which is comparable to that in adults. Dose-normalized SN-38 AUC values were comparable between adults and children. Minimal accumulation of irinotecan and SN-38 was observed in children on daily dosing regimens [daily x 5 every 3 weeks or (daily x 5) x 2 weeks every 3 weeks].
Geriatric Use
CLINICAL PHARMACOLOGY, Pharmacokinetics in Special Populations ADVERSE REACTIONS, Overview of Adverse Events, sections 2 DOSAGE AND ADMINISTRATION
IRINOTECAN HYDROCHLORIDE ADVERSE REACTIONS
Second-Line Single-Agent Therapy
Weekly Dosage Schedule
In three clinical studies evaluating the weekly dosage schedule, 304 patients with metastatic carcinoma of the colon or rectum that had recurred or progressed following 5-FU-based therapy were treated with irinotecan hydrochloride injection. Seventeen of the patients died within 30 days of the administration of irinotecan hydrochloride injection; in five cases (1.6%, 5/304), the deaths were potentially drug-related. These five patients experienced a constellation of medical events that included known effects of irinotecan hydrochloride injection. One of these patients died of neutropenic sepsis without fever. Neutropenic fever occurred in nine (3%) other patients; these patients recovered with supportive care.
One hundred nineteen (39.1%) of the 304 patients were hospitalized a total of 156 times because of adverse events; 81 (26.6%) patients were hospitalized for events judged to be related to administration of irinotecan hydrochloride injection. The primary reasons for drug-related hospitalization were diarrhea, with or without nausea and/or vomiting (18.4%); neutropenia/leukopenia, with or without diarrhea and/or fever (8.2%); and nausea and/or vomiting (4.9%).
Adjustments in the dose of irinotecan hydrochloride injection were made during the cycle of treatment and for subsequent cycles based on individual patient tolerance. The first dose of at least one cycle of irinotecan hydrochloride injection was reduced for 67% of patients who began the studies at the 125-mg/m2 starting dose. Within-cycle dose reductions were required for 32% of the cycles initiated at the 125-mg/m2 dose level. The most common reasons for dose reduction were late diarrhea, neutropenia, and leukopenia. Thirteen (4.3%) patients discontinued treatment with irinotecan hydrochloride injection because of adverse events. The adverse events in Table 5 are based on the experience of the 304 patients enrolled in the three studies described in the CLINICAL STUDIES, Studies Evaluating the Weekly Dosage Schedule, section.
| Body system and Event | % of Patients Reporting | |
|---|---|---|
| NCI Grades 1 to 4 | NCI Grades 3 and 4 | |
|
a Severity of adverse events based on NCI CTC (version 1.0) b Occurring > 24 hours after administration of irinotecan hydrochloride injection c Occurring ≤ 24 hours after administration of irinotecan hydrochloride injection d Primarily upper respiratory infections e Not applicable; complete hair loss = NCI grade 2 |
||
|
GASTROINTESTINAL
Diarrhea (late) b 7-9 stools/day (grade 3) ≥ 10 stools/day (grade 4) Nausea Vomiting Anorexia Diarrhea (early) c Constipation Flatulence Stomatitis Dyspepsia |
88 — — 86 67 55 51 30 12 12 10 |
31 (16) (14) 17 12 6 8 2 0 1 0 |
|
HEMATOLOGIC
Leukopenia Anemia Neutropenia 500 to <1000/ mm3 (grade 3) <500/ mm3 (grade 4) |
63 60 54 — — |
28 7 26 (15) (12) |
|
BODY AS A WHOLE
Asthenia Abdominal cramping/pain Fever Pain Headache Back pain Chills Minor infectiond Edema Abdominal enlargement |
76 57 45 24 17 14 14 14 10 10 |
12 16 1 2 1 2 0 0 1 0 |
|
METABOLIC and NUTRITIONAL
↓ Body weight Dehydration ↑ Alkaline phosphatase ↑ SGOT |
30 15 13 10 |
1 4 4 1 |
|
DERMATOLOGIC
Alopecia Sweating Rash |
60 16 13 |
NAe 0 1 |
|
RESPIRATORY
Dyspnea ↑ Coughing Rhinitis |
22 17 16 |
4 0 0 |
|
NEUROLOGIC
Insomnia Dizziness |
19 15 |
0 0 |
|
CARDIOVASCULAR
Vasodilation (flushing) |
11 |
0 |
Once-Every-3-Week Dosage Schedule
A total of 535 patients with metastatic colorectal cancer whose disease had recurred or progressed following prior 5-FU therapy participated in the two phase 3 studies: 316 received irinotecan, 129 received 5-FU, and 90 received best supportive care. Eleven (3.5%) patients treated with irinotecan died within 30 days of treatment. In three cases (1%, 3/316), the deaths were potentially related to irinotecan treatment and were attributed to neutropenic infection, grade 4 diarrhea, and asthenia, respectively. One (0.8%, 1/129) patient treated with 5-FU died within 30 days of treatment; this death was attributed to grade 4 diarrhea.
Hospitalizations due to serious adverse events (whether or not related to study treatment) occurred at least once in 60% (188/316) of patients who received irinotecan, 63% (57/90) who received best supportive care, and 39% (50/129) who received 5-FU-based therapy. Eight percent of patients treated with irinotecan and 7% treated with 5-FU-based therapy discontinued treatment due to adverse events.
Of the 316 patients treated with irinotecan, the most clinically significant adverse events (all grades, 1 to 4) were diarrhea (84%), alopecia (72%), nausea (70%), vomiting (62%), cholinergic symptoms (47%), and neutropenia (30%). Table 6 lists the grade 3 and 4 adverse events reported in the patients enrolled to all treatment arms of the two studies described in the CLINICAL STUDIES, Studies Evaluating the Once-Every-3-Week Dosage Schedule, section.
| Adverse Event | Study 1 | Study 2 | ||
|---|---|---|---|---|
|
Irinotecan N=189 |
BSCb
N=90 |
Irinotecan N=127 |
5-FU N=129 |
|
|
a Severity of adverse events based on NCI CTC (version 1.0) b BSC = best supportive care c Hepatic includes events such as ascites and jaundice d Cutaneous signs include events such as rash e Respiratory includes events such as dyspnea and cough f Neurologic includes events such as somnolence g Cardiovascular includes events such as dysrhythmias, ischemia, and mechanical cardiac dysfunction h Other includes events such as accidental injury, hepatomegaly, syncope, vertigo, and weight loss |
||||
|
TOTAL Grade 3/4 Adverse Events |
79 |
67 |
69 |
54 |
|
GASTROINTESTINAL
Diarrhea Vomiting Nausea Abdominal pain Constipation Anorexia Mucositis |
22 14 14 14 10 5 2 |
6 8 3 16 8 7 1 |
22 14 11 9 8 6 2 |
11 5 4 8 6 4 5 |
|
HEMATOLOGIC
Leukopenia/Neutropenia Anemia Hemorrhage Thrombocytopenia Infection without grade 3/4 neutropenia with grade 3/4 neutropenia Fever without grade 3/4 neutropenia with grade 3/4 neutropenia |
22 7 5 1 8 1 2 2 |
0 6 3 0 3 0 1 0 |
14 6 1 4 1 2 2 4 |
2 3 3 2 4 0 0 2 |
|
BODY AS A WHOLE
Pain Asthenia |
19 15 |
22 19 |
17 13 |
13 12 |
|
METABOLIC and NUTRITIONAL
Hepaticc |
9 |
7 |
9 |
6 |
|
DERMATOLOGIC
Hand and foot syndrome Cutaneous signsd |
0 2 |
0 0 |
0 1 |
5 3 |
|
RESPIRATORYe
|
10 |
8 |
5 |
7 |
|
NEUROLOGICf
|
12 |
13 |
9 |
4 |
|
CARDIOVASCULARg
|
9 |
3 |
4 |
2 |
|
OTHERh
|
32 |
28 |
12 |
14 |
Overview of Adverse Events
Gastrointestinal: Nausea, vomiting, and diarrhea are common adverse events following treatment with irinotecan hydrochloride injection and can be severe. When observed, nausea and vomiting usually occur during or shortly after infusion of irinotecan hydrochloride injection. An increased incidence of late diarrhea was observed in two studies, one using a 3-week schedule and the other using a weekly schedule. In the clinical studies testing the every 3-week-dosage schedule, the median time to the onset of late diarrhea was 5 days after irinotecan infusion. In the clinical studies evaluating the weekly dosage schedule, the median time to onset of late diarrhea was 11 days following administration of irinotecan hydrochloride injection. For patients starting treatment at the 125 mg/m2 weekly dose, the median duration of any grade of late diarrhea was 3 days. Among those patients treated at the 125 mg/m2 weekly dose who experienced grade 3 or 4 late diarrhea, the median duration of the entire episode of diarrhea was 7 days. The frequency of grade 3 or 4 late diarrhea was somewhat greater in patients starting treatment at 125 mg/m2 than in patients given a 100 mg/m2 weekly starting dose (34% [65/193] versus 23% [24/102]; p=0.08). The frequency of grade 3 and 4 late diarrhea by age was significantly greater in patients ≥65 years than in patients <65 years (40% [53/133] versus 23% [40/171]; p=0.002). In another study of 183 patients treated on the weekly schedule, the frequency of grade 3 or 4 late diarrhea in patients ≥65 years of age was 28.6% [26/91] and in patients <65 years of age was 23.9% [22/92].
In one study of the weekly dosage treatment, the frequency of grade 3 and 4 late diarrhea was significantly greater in male than in female patients (43% [25/58] versus 16% [5/32]; p=0.01), but there were no gender differences in the frequency of grade 3 and 4 late diarrhea in the other two studies of the weekly dosage treatment schedule. Colonic ulceration, sometimes with gastrointestinal bleeding, has been observed in association with administration of irinotecan hydrochloride injection.
Hematology: Irinotecan hydrochloride injection commonly causes neutropenia, leukopenia (including lymphocytopenia), and anemia. Serious thrombocytopenia is uncommon. When evaluated in the trials of weekly administration, the frequency of grade 3 and 4 neutropenia was significantly higher in patients who received previous pelvic/abdominal irradiation than in those who had not received such irradiation (48% [13/27] versus 24% [67/277]; p=0.04). In these same studies, patients with baseline serum total bilirubin levels of 1 mg/dL or more also had a significantly greater likelihood of experiencing first-cycle grade 3 or 4 neutropenia than those with bilirubin levels that were less than 1 mg/dL (50% [19/38] versus 18% [47/266]; p<0.001). There were no significant differences in the frequency of grade 3 and 4 neutropenia by age or gender. In the clinical studies evaluating the weekly dosage schedule, neutropenic fever (concurrent NCI grade 4 neutropenia and fever of grade 2 or greater) occurred in 3% of the patients; 6% of patients received G-CSF for the treatment of neutropenia. NCI grade 3 or 4 anemia was noted in 7% of the patients receiving weekly treatment; blood transfusions were given to 10% of the patients in these trials.
Body as a Whole: Asthenia, fever, and abdominal pain are generally the most common events of this type.
Cholinergic Symptoms: Patients may have cholinergic symptoms of rhinitis, increased salivation, miosis, lacrimation, diaphoresis, flushing, and intestinal hyperperistalsis that can cause abdominal cramping and early diarrhea. If these symptoms occur, they manifest during or shortly after drug infusion. They are thought to be related to the anticholinesterase activity of the irinotecan parent compound and are expected to occur more frequently with higher irinotecan doses.
Hepatic: In the clinical studies evaluating the weekly dosage schedule, NCI grade 3 or 4 liver enzyme abnormalities were observed in fewer than 10% of patients. These events typically occur in patients with known hepatic metastases.
Dermatologic: Alopecia has been reported during treatment with irinotecan hydrochloride injection. Rashes have also been reported but did not result in discontinuation of treatment.
Respiratory: Severe pulmonary events are infrequent. In the clinical studies evaluating the weekly dosage schedule, NCI grade 3 or 4 dyspnea was reported in 4% of patients. Over half the patients with dyspnea had lung metastases; the extent to which malignant pulmonary involvement or other preexisting lung disease may have contributed to dyspnea in these patients is unknown.
Interstitial pulmonary disease presenting as pulmonary infiltrates is uncommon during irinotecan therapy. Interstitial pulmonary disease can be fatal. Risk factors possibly associated with the development of interstitial pulmonary disease include pre-existing lung disease, use of pneumotoxic drugs, radiation therapy, and colony stimulating factors. Patients with risk factors should be closely monitored for respiratory symptoms before and during irinotecan therapy (see WARNINGS section).
Neurologic: Insomnia and dizziness can occur, but are not usually considered to be directly related to the administration of irinotecan hydrochloride injection. Dizziness may sometimes represent symptomatic evidence of orthostatic hypotension in patients with dehydration.
Cardiovascular: Vasodilation (flushing) may occur during administration of irinotecan hydrochloride injection. Bradycardia may also occur, but has not required intervention. These effects have been attributed to the cholinergic syndrome sometimes observed during or shortly after infusion of irinotecan hydrochloride injection. Thromboembolic events have been observed in patients receiving irinotecan hydrochloride injection; the specific cause of these events has not been determined.
Other Non-U.S. Clinical Trials
Post-Marketing Experience
The following events have been identified during post-marketing use of irinotecan hydrochloride injection in clinical practice. Myocardial ischemic events have been observed following irinotecan therapy. Infrequent cases of ulcerative and ischemic colitis have been observed. This can be complicated by ulceration, bleeding, ileus, obstruction, and infection, including typhlitis. Patients experiencing ileus should receive prompt antibiotic support (see PRECAUTIONS section). Cases of megacolon, intestinal perforation, symptomatic pancreatitis, and asymptomatic pancreatic enzyme elevation have been reported.
Hypersensitivity reactions including severe anaphylactic or anaphylactoid reactions have also been observed (see WARNINGS section).
Cases of hyponatremia mostly related with diarrhea and vomiting have been reported. Increases in serum levels of transaminases (i.e., AST and ALT) in the absence of progressive liver metastasis; transient increase of amylase and occasionally transient increase of lipase have been reported.
Infrequent cases of renal insufficiency including acute renal failure, hypotension or circulatory failure have been observed in patients who experienced episodes of dehydration associated with diarrhea and/or vomiting, or sepsis (see WARNINGS section).
Early effects such as muscular contraction or cramps and paresthesia have been reported.
Hiccups have been reported.
Transient dysarthria has been reported in patients treated with irinotecan hydrochloride injection; in some cases, the event was attributed to the cholinergic syndrome observed during or shortly after infusion of irinotecan.
OVERDOSAGE
22
IRINOTECAN HYDROCHLORIDE DOSAGE AND ADMINISTRATION
Single-Agent Dosage Schedules
Dosage Regimens
Irinotecan hydrochloride injection should be administered as an intravenous infusion over 90 minutes for both the weekly and once-every-3-week dosage schedules (see Preparation of Infusion Solution). Single-agent dosage regimens are shown in Table 7.
|
aSubsequent doses may be adjusted as high as 150 mg/m2 or to as low as 50 mg/m2 in 25 to 50 mg/m2 decrements depending upon individual patient tolerance. bSubsequent doses may be adjusted as low as 200 mg/m2 in 50 mg/m2 decrements depending upon individual patient tolerance. c Provided intolerable toxicity does not develop, treatment with additional cycles may be continued indefinitely as long as patients continue to experience clinical benefit. |
|||
|
Weekly Regimena
|
125 mg/m2 IV over 90 min, d 1,8,15,22 then 2-wk rest |
||
|
Starting Dose and Modified Dose Levelsc (mg/m2)
|
|||
| Starting Dose |
Dose Level-1 |
Dose Level-2 |
|
| 125 |
100 |
75 |
|
|
Once-Every-3-Week Regimenb
|
350 mg/m2 IV over 90 min, once every 3 wksc
|
||
|
Starting Dose and Modified Dose Levels (mg/m2)
|
|||
| Starting Dose |
Dose Level-1 |
Dose Level-2 |
|
| 350 |
300 |
250 |
|
A reduction in the starting dose by one dose level of irinotecan hydrochloride injection may be considered for patients with any of the following conditions: prior pelvic/abdominal radiotherapy, performance status of 2, or increased bilirubin levels. Dosing for patients with bilirubin >2 mg/dL cannot be recommended because there is insufficient information to recommend a dose in these patients.
It is recommended that patients receive premedication with antiemetic agents. Prophylactic or therapeutic administration of atropine should be considered in patients experiencing cholinergic symptoms. See PRECAUTIONS, General section.
Dose Modifications
Patients should be carefully monitored for toxicity and doses of irinotecan hydrochloride injection should be modified as necessary to accommodate individual patient tolerance to treatment. Based on recommended dose-levels described in Table 7, Single-Agent Regimens of irinotecan hydrochloride injection and Dose Modifications, subsequent doses should be adjusted as suggested in Table 8, Recommended Dose Modifications for Single-Agent Schedules. All dose modifications should be based on the worst preceding toxicity.
A new cycle of therapy should not begin until the toxicity has recovered to NCI grade 1 or less. Treatment may be delayed 1 to 2 weeks to allow for recovery from treatment-related toxicity. If the patient has not recovered, consideration should be given to discontinuing this combination therapy. Provided intolerable toxicity does not develop, treatment with additional cycles of irinotecan hydrochloride injection may be continued indefinitely as long as patients continue to experience clinical benefit.
| A new cycle of therapy should not begin until the granulocyte count has recovered to ≥1500/ mm3, and the platelet count has recovered to ≥100,000/ mm3, and treatment-related diarrhea is fully resolved. Treatment should be delayed 1 to 2 weeks to allow for recovery from treatment-related toxicities. If the patient has not recovered after a 2-week delay, consideration should be given to discontinuing irinotecan. | |||
|---|---|---|---|
|
aAll dose modifications should be based on the worst preceding toxicity bNational Cancer Institute Common Toxicity Criteria (version 1.0) cPretreatment dExcludes alopecia, anorexia, asthenia |
|||
|
Worst Toxicity NCI Gradeb(Value) |
During a Cycle of Therapy |
At the Start of the Next Cycles of Therapy (After Adequate Recovery), Compared with the Starting Dose in the Previous Cyclea |
|
| Weekly | Weekly | Once Every 3 Weeks | |
| No toxicity | Maintain dose level | ↑ 25 mg/m2 up to a maximum dose of 150 mg/mm2 |
Maintain dose level |
| Neutropenia | |||
| 1 (1500 to 1999/ mm3) | Maintain dose level | Maintain dose level | Maintain dose level |
| 2 (1000 to 1499/ mm3) | ↓ 25 mg/mm2 | Maintain dose level | Maintain dose level |
| 3 (500 to 999/ mm3) | Omit dose until resolved to ≤ grade 2, then ↓ 25 mg/mm2 | ↓ 25 mg/mm2 | ↓ 50 mg/mm2 |
| 4 (<500/ mm3) | Omit dose until resolved to ≤ grade 2, then ↓ 50 mg/mm2 | ↓ 50 mg/mm2
|
↓ 50 mg/mm2 |
| Neutropenic fever | Omit dose until resolved, then ↓ 50 mg/mm2 when resolved |
↓ 50 mg/mm2 | ↓ 50 mg/mm2 |
|
Other hematologic toxicities |
Dose modifications for leukopenia, thrombocytopenia, and anemia during a cycle of therapy and at the start of subsequent cycles of therapy are also based on NCI toxicity criteria and are the same as recommended for neutropenia above. | ||
| Diarrhea | |||
| 1 (2-3 stools/day > pretxc) | Maintain dose level | Maintain dose level | Maintain dose level |
| 2 (4-6 stools/day > pretx) | ↓ 25 mg/mm2 | Maintain dose level | Maintain dose level |
| 3 (7-9 stools/day > pretx) | Omit dose until resolved to ≤ grade 2, then ↓ 25 mg/mm2 | ↓ 25 mg/mm2 | ↓ 50 mg/mm2 |
| 4 (≥10 stools/day > pretx) | Omit dose until resolved to ≤ grade 2, then ↓ 50 mg/mm2 |
↓ 50 mg/mm2
|
↓ 50 mg/mm2 |
|
Other nonhematologicd toxicities |
|
|
|
| 1 | Maintain dose level | Maintain dose level | Maintain dose level |
| 2 | ↓ 25 mg/mm2 | ↓ 25 mg/mm2 | ↓ 50 mg/mm2 |
| 3 | Omit dose until resolved to ≤ grade 2, then ↓ 25 mg/mm2 | ↓ 25 mg/mm2
|
↓ 50 mg/mm2
|
| 4 | Omit dose until resolved to ≤ grade 2, then ↓ 50 mg/mm2 | ↓ 50 mg/m2 | ↓ 50 mg/mm2
|
Dosage in Patients with Reduced UGT1A1 Activity
When administered as a single-agent, a reduction in the starting dose by at least one level of irinotecan hydrochloride injection should be considered for patients known to be homozygous for the UGT1A1*28 allele (see CLINICAL PHARMACOLOGY and WARNINGS sections). However, the precise dose reduction in this patient population is not known and subsequent dose modifications should be considered based on individual patient tolerance to treatment (see tables 7 to 8).
Preparation and Administration Precautions
As with other potentially toxic anticancer agents, care should be exercised in the handling and preparation of infusion solutions prepared from irinotecan hydrochloride injection. The use of gloves is recommended. If a solution of irinotecan hydrochloride injection contacts the skin, wash the skin immediately and thoroughly with soap and water. If irinotecan hydrochloride injection contacts the mucous membranes, flush thoroughly with water.
Several published guidelines for handling and disposal of anticancer agents are available.1-4
Preparation of Infusion Solution
Inspect vial contents for particulate matter and repeat inspection when drug product is withdrawn from vial into syringe.
Irinotecan hydrochloride injection must be diluted prior to infusion. Irinotecan hydrochloride injection should be diluted in 5% Dextrose Injection, USP, (preferred) or 0.9% Sodium Chloride Injection, USP, to a final concentration range of 0.12 to 2.8 mg/mL. In most clinical trials, irinotecan hydrochloride injection was administered in 250 mL to 500 mL of 5% Dextrose Injection, USP.
The solution is physically and chemically stable for up to 24 hours at room temperature (approximately 25°C) and in ambient fluorescent lighting. Solutions diluted in 5% Dextrose Injection, USP, and stored at refrigerated temperatures (approximately 2° to 8°C), and protected from light are physically and chemically stable for 48 hours. Refrigeration of admixtures using 0.9% Sodium Chloride Injection, USP, is not recommended due to a low and sporadic incidence of visible particulates. Freezing irinotecan hydrochloride injection and admixtures of irinotecan hydrochloride injection may result in precipitation of the drug and should be avoided. Because of possible microbial contamination during dilution, it is advisable to use the admixture prepared with 5% Dextrose Injection, USP, within 24 hours if refrigerated (2° to 8°C, 36° to 46°F). In the case of admixtures prepared with 5% Dextrose Injection, USP, or Sodium Chloride Injection, USP, the solutions should be used within 6 hours if kept at room temperature (15° to 30°C, 59° to 86°F).
Other drugs should not be added to the infusion solution. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
HOW SUPPLIED
.
| Product No. | NDC No. | |
|---|---|---|
| 109302 |
63323-193-02 |
Irinotecan Hydrochloride Injection, 20 mg/mL in a 2 mL single dose amber glass vial packaged individually |
| 109305 |
63323-193-05 |
Irinotecan Hydrochloride Injection, 20 mg/mL in a 5 mL single dose amber glass vial packaged individually |
Store between 20° to 25°C (68° to 77°F) See USP Controlled Room Temperature, excursions permitted to 15° to 30°C (59° to 86°F). Protect from light. Retain in carton until time of use.
REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006; 63:1172-1193.
- Polovich, M., White, J. M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology Nursing Society.
Manufactured for:

APP Pharmaceuticals, LLC
Schaumburg, IL60173
Made in India
For Product Inquiry:
1-800-551-7176 or
www.APPpharma.com
Irinotecan HCl Injection 40 mg Carton Label
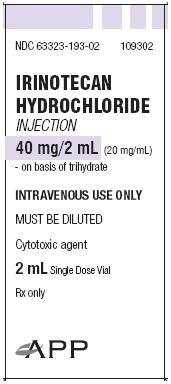
109302
IRINOTECAN
HYDROCHLORIDE
INJECTION
40 mg/2 mL (20 mg/mL)
- on basis of trihydrate
INTRAVENOUS USE ONLY
MUST BE DILUTED
Cytotoxic agent
2 mL Single Dose Vial
Rx only
Irinotecan HCl Injection 100 mg Carton Label
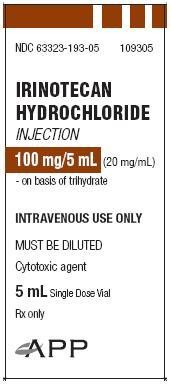
NDC 63323-193-05
109305
IRINOTECAN
HYDROCHLORIDE
INJECTION
100 mg/5 mL (20 mg/mL)
- on basis of trihydrate
INTRAVENOUS USE ONLY
MUST BE DILUTED
Cytotoxic agent
5 mL Single Dose Vial
Irinotecan HydrochlorideIrinotecan Hydrochloride INJECTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||