FLUXID
FLUXID™(FAMOTIDINE ORALLY DISINTEGRATING TABLETS)
FULL PRESCRIBING INFORMATION: CONTENTS*
- Description
- CLINICAL PHARMACOLOGY IN ADULTS
- FLUXID INDICATIONS AND USAGE
- FLUXID CONTRAINDICATIONS
- PRECAUTIONS
- FLUXID ADVERSE REACTIONS
- OVERDOSAGE
- FLUXID DOSAGE AND ADMINISTRATION
- Instructions for Use/Handling FLUXID™ Tablets
- Duodenal Ulcer
- Benign Gastric Ulcer
- Gastroesophageal Reflux Disease (GERD)
- Dosage for Pediatric Patients 6-16 years of age
- Pathological Hypersecretory Conditions (e.g., Zollinger-Ellison Syndrome, Multiple Endocrine Adenomas)
- Concomitant Use of Antacids
- Dosage Adjustment for Patients with Moderate or Severe Renal Insufficiency
- HOW SUPPLIED
FULL PRESCRIBING INFORMATION
Description
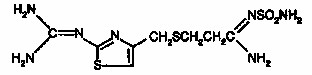
FLUXID™ (famotidine orally disintegrating tablets) is a histamine H2-receptor antagonist. Famotidine is N′-(aminosulfonyl)-3-[[[2-[(diaminomethylene)amino]-4-thiazolyl]methyl]thio] propanimidamide. The empirical formula of famotidine is C8H15N7O2S3 and its molecular weight is 337.45. Its structural formula is:
Famotidine is a white to pale yellow crystalline compound that is freely soluble in glacial acetic acid, slightly soluble in methanol, very slightly soluble in water, and practically insoluble in ethanol.
Each orally disintegrating tablet contains either 20 mg or 40 mg of famotidine and the following inactive ingredients: citric acid, colloidal silicon dioxide, corn starch, crospovidone, hypromellose, magnesium stearate, mannitol, methacrylic acid copolymer, microcrystalline cellulose, natural and artificial cherry flavor, sodium bicarbonate, sucralose and sucrose.
CLINICAL PHARMACOLOGY IN ADULTS
GI Effects
Famotidine is a competitive inhibitor of histamine H2-receptors. The primary clinically important pharmacologic activity of famotidine is inhibition of gastric secretion. Both the acid concentration and volume of gastric secretion are suppressed by famotidine, while changes in pepsin secretion are proportional to volume output.
In normal volunteers and hypersecretors, famotidine inhibited basal and nocturnal gastric secretion, as well as secretion stimulated by food and pentagastrin. After oral administration, the onset of the antisecretory effect occurred within one hour; the maximum effect was dose-dependent, occurring within one to three hours. Duration of inhibition of secretion by doses of
20 and 40 mg was 10 to 12 hours.
Single evening oral doses of 20 and 40 mg inhibited basal and nocturnal acid secretion in all subjects; mean nocturnal gastric acid secretion was inhibited by 86% and 94%, respectively, for a period of at least 10 hours. The same doses given in the morning suppressed food-stimulated acid secretion in all subjects. The mean suppression was 76% and 84%, respectively, 3 to 5 hours after administration, and 25% and 30%, respectively, 8 to 10 hours after administration. In some subjects who received the 20 mg dose, however, the antisecretory effect was dissipated within 6-8 hours. There was no cumulative effect with repeated doses. The nocturnal intragastric pH was raised by evening doses of 20 and 40 mg of famotidine to mean values of 5.0 and 6.4, respectively. When famotidine was given after breakfast, the basal daytime interdigestive pH at 3 and 8 hours after 20 or 40 mg of famotidine was raised to about 5.
Famotidine had little or no effect on fasting or postprandial serum gastrin levels. Gastric emptying and exocrine pancreatic function were not affected by famotidine.
Other Effects
Systemic effects of famotidine in the CNS, cardiovascular, respiratory or endocrine systems were not noted in clinical pharmacology studies. Also, no antiandrogenic effects were noted. (See ADVERSE REACTIONS.) Serum hormone levels, including prolactin, cortisol, thyroxine (T4), and testosterone, were not altered after treatment with famotidine.
Pharmacokinetics
Famotidine is incompletely absorbed. The bioavailability of oral doses is 40-45%. Bioavailability may be slightly increased by food, or slightly decreased by antacids; however, these effects are of no clinical consequence. Famotidine undergoes minimal first-pass metabolism. The peak plasma concentration is reached about 2½ hours after administration of FLUXID™. Plasma levels after multiple doses are similar to those after single doses. Fifteen to 20% of famotidine in plasma is protein bound. The elimination half-life of famotidine is approximately 5 hours after administration of FLUXID™. Famotidine is eliminated by renal (65-70%) and metabolic (30-35%) routes. Renal clearance is 250 - 450 mL/min, indicating some tubular excretion. Twenty-five to 30% of an oral dose and 65-70% of an intravenous dose are recovered in the urine as unchanged compound. The only metabolite identified in man is the S-oxide.
There is a close relationship between creatinine clearance values and the elimination half-life of famotidine. In patients with severe renal insufficiency, i.e., creatinine clearance less than
10 mL/min, the elimination half-life of famotidine may exceed 20 hours and adjustment of dose or dosing intervals in moderate and severe renal insufficiency may be necessary (see PRECAUTIONS, DOSAGE AND ADMINISTRATION).
In elderly patients, there are no clinically significant age-related changes in the pharmacokinetics of famotidine. However, in elderly patients with decreased renal function, the clearance of the drug may be decreased (see PRECAUTIONS, Geriatric Use).
Clinical Studies
Duodenal Ulcer
In a U.S. multicenter, double-blind study in outpatients with endoscopically confirmed duodenal ulcer, orally administered famotidine was compared to placebo. As shown in Table 1, 70% of patients treated with famotidine 40 mg h.s. were healed by week 4.
| Famotidine 40 mg h.s. (N=89) | Famotidine 20 mg b.i.d. (N=84) | Placebo h.s. (N=97) | |
| Week 2 |  |  | 17% |
| Week 4 |  |  | 31% |
Patients not healed by week 4 were continued in the study. By week 8, 83% of patients treated with famotidine had healed versus 45% of patients treated with placebo. The incidence of ulcer healing with famotidine was significantly higher than with placebo at each time point based on proportion of endoscopically confirmed healed ulcers.
In this study, time to relief of daytime and nocturnal pain was significantly shorter for patients receiving famotidine than for patients receiving placebo; patients receiving famotidine also took less antacid than the patients receiving placebo.
Long-Term Maintenance
Treatment of Duodenal Ulcers
Famotidine, 20 mg p.o. h.s. was compared to placebo h.s. as maintenance therapy in two double-blind, multicenter studies of patients with endoscopically confirmed healed duodenal ulcers. In the U.S. study, the observed ulcer incidence within 12 months in patients treated with placebo was 2.4 times greater than in the patients treated with famotidine. The 89 patients treated with famotidine had a cumulative observed ulcer incidence of 23.4% compared to an observed ulcer incidence of 56.6% in the 89 patients receiving placebo (p<0.01). These results were confirmed in an international study where the cumulative observed ulcer incidence within 12 months in the 307 patients treated with famotidine was 35.7%, compared to an incidence of 75.5% in the 325 patients treated with placebo (p<0.01).
Gastric Ulcer
In both a U.S. and an international multicenter, double-blind study in patients with endoscopically confirmed active benign gastric ulcer, orally administered famotidine, 40 mg h.s., was compared to placebo h.s. Antacids were permitted during the studies, but consumption was not significantly different between the famotidine and placebo groups. As shown in Table 2, the incidence of ulcer healing (dropouts counted as unhealed) with famotidine was statistically significantly better than placebo at weeks 6 and 8 in the U.S. study, and at weeks 4, 6 and 8 in the international study, based on the number of ulcers that healed, confirmed by endoscopy.
| U.S. Study | International Study | |||
| Famotidine 40 mg h.s. (N=74) | Placebo h.s. (N=75) | Famotidine 40 mg h.s. (N=149) | Placebo h.s. (N=145) | |
| Week 4 | 45% | 39% |  | 31% |
| Week 6 |  | 44% |  | 46% |
| Week 8 |  | 64% |  | 54% |
Time to complete relief of daytime and nighttime pain was statistically significantly shorter for patients receiving famotidine than for patients receiving placebo; however, in neither study was there a statistically significant difference in the proportion of patients whose pain was relieved by the end of the study (week 8).
Gastroesophageal Reflux Disease (GERD)
Orally administered famotidine was compared to placebo in a U.S. study that enrolled patients with symptoms of GERD and without endoscopic evidence of erosion or ulceration of the esophagus. Famotidine 20 mg b.i.d. was statistically significantly superior to 40 mg h.s. and to placebo in providing a successful symptomatic outcome, defined as moderate or excellent improvement of symptoms (Table 3).
| Famotidine 20 mg b.i.d. (N=154) | Famotidine 40 mg h.s. (N=149) | Placebo (N=73) | |
| Week 6 | 82 | 69 | 62 |
By two weeks of treatment symptomatic success was observed in a greater percentage of patients taking famotidine 20 mg b.i.d. compared to placebo (p<0.01).
Symptomatic improvement and healing of endoscopically verified erosion and ulceration were studied in two additional trials. Healing was defined as complete resolution of all erosions or ulcerations visible with endoscopy. The U.S. study comparing famotidine 40 mg p.o. b.i.d. to placebo and famotidine 20 mg p.o. b.i.d. showed a significantly greater percentage of healing for famotidine 40 mg b.i.d. at weeks 6 and 12 (Table 4).
| Famotidine 40 mg b.i.d. (N=127) | Famotidine 20 mg b.i.d. (N=125) | Placebo (N=66) | |
| Week 6 | 48  | 32 | 18 |
| Week 12 | 69  | 54 | 29 |
As compared to placebo, patients who received famotidine had faster relief of daytime and nighttime heartburn and a greater percentage of patients experienced complete relief of nighttime heartburn. These differences were statistically significant.
In the international study, when famotidine 40 mg p.o. b.i.d., was compared to ranitidine 150 mg p.o. b.i.d., a statistically significantly greater percentage of healing was observed with famotidine 40 mg b.i.d. at week 12 (Table 5). There was, however, no significant difference among treatments in symptom relief.
| Famotidine 40 mg b.i.d. (N=175) | Famotidine 20 mg b.i.d. (N=93) | Ranitidine 150 mg b.i.d. (N=172) | |
| Week 6 | 48 | 52 | 42 |
| Week 12 | 71 | 68 | 60 |
Pathological Hypersecretory Conditions (e.g., Zollinger-Ellison Syndrome, Multiple Endocrine Adenomas)
In studies of patients with pathological hypersecretory conditions such as Zollinger-Ellison Syndrome with or without multiple endocrine adenomas, famotidine significantly inhibited gastric acid secretion and controlled associated symptoms. Orally administered doses from 20 to 160 mg q 6 h maintained basal acid secretion below 10 mEq/hr; initial doses were titrated to the individual patient need and subsequent adjustments were necessary with time in some patients. Famotidine was well tolerated at these high dose levels for prolonged periods (greater than 12 months) in eight patients, and there were no cases reported of gynecomastia, increased prolactin levels, or impotence which were considered to be due to the drug.
Pharmacokinetics
Bioavailability studies of 8 pediatric patients (11-15 years of age) showed a mean oral bioavailability of 0.5 compared to adult values of 0.42 to 0.49. Oral doses of 0.5 mg/kg achieved an AUC of 580 + 60 ng-hr/mL in pediatric patients 11-15 years of age compared to 482 ± 181 ng-hr/mL in adults treated with 40 mg orally.
Pharmacodynamics
Pharmacodynamics of famotidine were evaluated in 5 pediatric patients 2 - 13 years of age using the sigmoid Emax model. These data suggest that the relationship between serum concentration of famotidine and gastric acid suppression is similar to that observed in one study of adults
(Table 6).
EC50(ng/mL) | |
| Pediatric Patients | 26 ± 13 |
| Data from one study | |
| a) healthy adult subjects | 26.5 ± 10.3 |
| b) adult patients with upper GI bleeding | 18.7 ± 10.8 |
In 4 pediatric patients 11 – 15 years of age given oral famotidine 0.5 mg/kg twice daily, gastric pH was greater than 5 for 5.0 + 1.1 hours.
FLUXID INDICATIONS AND USAGE
FLUXID™ is indicated in:
1. Short term treatment of active duodenal ulcer. Most adult patients heal within 4 weeks; there is rarely reason to use famotidine at full dosage for longer than 6 to 8 weeks. Studies have not assessed the safety of famotidine in uncomplicated active duodenal ulcer for periods of more than eight weeks.
2. Maintenance therapy for duodenal ulcer patients at reduced dosage after healing of an active ulcer. Controlled studies in adults have not extended beyond one year.
3. Short term treatment of active benign gastric ulcer. Most adult patients heal within 6 weeks. Studies have not assessed the safety or efficacy of famotidine in uncomplicated active benign gastric ulcer for periods of more than 8 weeks.
4. Short term treatment of gastroesophageal reflux disease (GERD). FLUXID™ is indicated for short term treatment of patients with symptoms of GERD (see CLINICAL PHARMACOLOGY IN ADULTS, Clinical Studies).
FLUXID™ is also indicated for the short term treatment of esophagitis due to GERD including erosive or ulcerative disease diagnosed by endoscopy (see CLINICAL PHARMACOLOGY IN ADULTS, Clinical Studies).
5. Treatment of pathological hypersecretory conditions (e.g., Zollinger-Ellison Syndrome, multiple endocrine adenomas) (see CLINICAL PHARMACOLOGY IN ADULTS, Clinical Studies).
FLUXID CONTRAINDICATIONS
Hypersensitivity to any component of this product. Cross sensitivity in this class of compounds has been observed. Therefore, FLUXID™ should not be administered to patients with a history of hypersensitivity to other H2-receptor antagonists.
PRECAUTIONS
General
Symptomatic response to therapy with famotidine does not preclude the presence of gastric malignancy.
Patients with Moderate or Severe Renal Insufficiency
Since CNS adverse effects have been reported in patients with moderate and severe renal insufficiency, longer intervals between doses or lower doses may need to be used in patients with moderate (creatinine clearance <50 mL/min) or severe (creatinine clearance <10 mL/min) renal insufficiency to adjust for the longer elimination half-life of famotidine (see CLINICAL PHARMACOLOGY IN ADULTS and DOSAGE AND ADMINISTRATION).
Information for patients
Patients should be instructed not to remove FLUXID™ Tablets from the bottle until just prior to dosing. With dry hands, the tablet should be removed from the bottle and immediately placed on the tongue to dissolve and be swallowed with the saliva. The tablet typically disintegrates in less than 2 minutes.
Drug interactions
No drug interactions have been identified. Studies with famotidine in man, in animal models, and in vitro have shown no significant interference with the disposition of compounds metabolized by the hepatic microsomal enzymes, e.g., cytochrome P450 system. Compounds tested in man include warfarin, theophylline, phenytoin, diazepam, aminopyrine and antipyrine. Indocyanine green as an index of hepatic drug extraction has been tested and no significant effects have been found.
Carcinogenesis, mutagenesis, impairment of fertility
In a 106 week study in rats and a 92 week study in mice given oral doses of up to
2000 mg/kg/day (approximately 405 times in rats, and 203 times in mice, the recommended maximum human dose based on body surface area), there was no evidence of carcinogenic potential for famotidine.
Famotidine was negative in the Ames test, the mouse micronucleus test and the mouse chromosomal aberration test.
In studies with rats given oral doses of up to 2000 mg/kg/day (approximately 405 times the recommended maximum human dose based on body surface area), fertility and reproductive performance were not affected.
Pregnancy. Teratogenic Effects: Pregnancy Category B
Reproductive studies have been performed at oral doses of up to 2000 mg/kg/day in rat (approximately 405 times the recommended maximum human dose based on body surface area) and 500 mg/kg/day in rabbit (approximately 203 times the recommended maximum human dose based on body surface area), and have revealed no significant evidence of impaired fertility or harm to the fetus due to famotidine. There are, however, no adequate or well-controlled studies in pregnant women. Because animal reproductive studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing mothers
Famotidine is detectable in human milk. Transient growth depression was observed in young rats suckling from mothers treated with famotidine. Because of the potential for serious adverse reactions in nursing infants from famotidine, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Patients 6-16 years of age
Use of famotidine in pediatric patients 6-16 years of age is supported by evidence from adequate and well-controlled studies of famotidine in adults, and by the following studies in pediatric patients: In published studies in small numbers of pediatric patients 1-15 years of age, clearance of famotidine was similar to that seen in adults. In pediatric patients 11-15 years of age, oral doses of 0.5 mg/kg were associated with a mean area under the curve (AUC) similar to that seen in adults treated orally with 40 mg. Limited published studies also suggest that the relationship between serum concentration and acid suppression is similar in pediatric patients 1-15 years of age as compared with adults. These studies suggest a starting dose for pediatric patients 6 - 16 years of age as follows:
Gastroesophageal Reflux Disease with or without esophagitis including erosions and
ulcerations - 1.0 mg/kg/day p.o. divided b.i.d. up to 40 mg b.i.d.
While published uncontrolled studies suggest effectiveness of famotidine in the treatment of gastroesophageal reflux disease, data in pediatric patients are insufficient to establish percent response with dose and duration of therapy. Therefore, treatment duration (initially based on adult duration recommendations) and dose should be individualized based on clinical response and/or pH determination (gastric or esophageal) and endoscopy. Published uncontrolled clinical studies in pediatric patients have employed doses up to 2 mg/kg/day for GERD with or without esophagitis including erosions and ulcerations.
Geriatric use
Of the 4,966 subjects in clinical studies who were treated with famotidine, 488 subjects (9.8%) were 65 and older, and 88 subjects (1.7%) were greater than 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. However, greater sensitivity of some older individuals cannot be ruled out.
No dosage adjustment is required based on age (see CLINICAL PHARMACOLOGY IN ADULTS, Pharmacokinetics). This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. Dosage adjustment in the case of moderate or severe renal impairment is necessary (see PRECAUTIONS, Patients with Moderate or Severe Renal Insufficiency and DOSAGE AND ADMINISTRATION, Dosage Adjustment for Patients with Moderate or Severe Renal Insufficiency).
FLUXID ADVERSE REACTIONS
The adverse reactions listed below have been reported during domestic and international clinical trials in approximately 2500 patients. In those controlled clinical trials in which famotidine tablets were compared to placebo, the incidence of adverse experiences in the group which received famotidine tablets, 40 mg at bedtime, was similar to that in the placebo group.
The following adverse reactions have been reported to occur in more than 1% of patients on therapy with famotidine in controlled clinical trials, and may be causally related to the drug: headache (4.7%), dizziness (1.3%), constipation (1.2%) and diarrhea (1.7%).
The following other adverse reactions have been reported infrequently in clinical trials or since the drug was marketed. The relationship to therapy with famotidine has been unclear in many cases. Within each category the adverse reactions are listed in order of decreasing severity:
Body as a Whole: fever, asthenia, fatigue
Cardiovascular: arrhythmia, AV block, palpitation
Gastrointestinal: cholestatic jaundice, liver enzyme abnormalities, vomiting, nausea, abdominal discomfort, anorexia, dry mouth
Hematologic: rare cases of agranulocytosis, pancytopenia, leukopenia, thrombocytopenia
Hypersensitivity: anaphylaxis, angioedema, orbital or facial edema, urticaria, rash, conjunctival injection
Musculoskeletal: musculoskeletal pain including muscle cramps, arthralgia
Nervous System/Psychiatric: grand mal seizure; psychic disturbances, which were reversible in cases for which follow-up was obtained, including hallucinations, confusion, agitation, depression, anxiety, decreased libido; paresthesia; insomnia; somnolence
Respiratory: bronchospasm
Skin: toxic epidermal necrolysis (very rare), alopecia, acne, pruritus, dry skin, flushing
Special Senses: tinnitus, taste disorder
Other: rare cases of impotence and rare cases of gynecomastia have been reported; however, in controlled clinical trials, the incidences were not greater than those seen with placebo.
The adverse experience profile seen with FLUXID™ was similar to that seen with famotidine tablets.
OVERDOSAGE
There is no experience to date with deliberate overdosage. Oral doses of up to 640 mg/day have been given to adult patients with pathological hypersecretory conditions with no serious adverse effects. In the event of overdosage, treatment should be symptomatic and supportive. Unabsorbed material should be removed from the gastrointestinal tract, the patient should be monitored, and supportive therapy should be employed.
Single oral doses of up to 3000 mg/kg in rats and mice and 2000 mg/kg in dogs were not lethal.
FLUXID DOSAGE AND ADMINISTRATION
Instructions for Use/Handling FLUXID™ Tablets
Just prior to administration, remove the tablet from the bottle with dry hands. Immediately place the FLUXID™ Tablet on top of the tongue, wait until it dissolves, then swallow with saliva. The tablet typically disintegrates in less than 2 minutes. Administration with liquid is not necessary.
Duodenal Ulcer
Acute Therapy
The recommended adult oral dosage for active duodenal ulcer is 40 mg once a day at bedtime. Most patients heal within 4 weeks; there is rarely reason to use famotidine at full dosage for longer than 6 to 8 weeks. A regimen of 20 mg b.i.d. is also effective
Maintenance Therapy
The recommended adult oral dose is 20 mg once a day at bedtime.
Benign Gastric Ulcer
Acute Therapy
The recommended adult oral dosage for active benign gastric ulcer is 40 mg once a day at bedtime.
Gastroesophageal Reflux Disease (GERD)
The recommended oral dosage for treatment of adult patients with symptoms of GERD is 20 mg b.i.d. for up to 6 weeks. The recommended oral dosage for the treatment of adult patients with esophagitis including erosions and ulcerations and accompanying symptoms due to GERD is 20 or 40 mg b.i.d. for up to 12 weeks (see CLINICAL PHARMACOLOGY IN ADULTS, Clinical Studies).
Dosage for Pediatric Patients 6-16 years of age
See PRECAUTIONS, Pediatric Patients 6-16 years of age.
The studies described in PRECAUTIONS, Pediatric Patients 6-16 years of age suggest the following starting doses in pediatric patients 6-16 years of age:
Gastroesophageal Reflux Disease with or without esophagitis including erosions and
ulcerations - 1.0 mg/kg/day p.o. divided b.i.d. up to 40 mg b.i.d.
Tablet should not be broken.
While published uncontrolled studies suggest effectiveness of famotidine in the treatment of gastroesophageal reflux disease, data in pediatric patients are insufficient to establish percent response with dose and duration of therapy. Therefore, treatment duration (initially based on adult duration recommendations) and dose should be individualized based on clinical response and/or pH determination (gastric or esophageal) and endoscopy. Published uncontrolled clinical studies in pediatric patients 1-16 years of age have employed doses up to 2 mg/kg/day for GERD with or without esophagitis including erosions and ulcerations.
Pathological Hypersecretory Conditions (e.g., Zollinger-Ellison Syndrome, Multiple Endocrine Adenomas)
The dosage of famotidine in patients with pathological hypersecretory conditions varies with the individual patient. The recommended adult oral starting dose for pathological hypersecretory conditions is 20 mg q 6 h. In some patients, a higher starting dose may be required. Doses should be adjusted to individual patient needs and should continue as long as clinically indicated. Doses up to 160 mg q 6 h have been administered to some adult patients with severe Zollinger-Ellison Syndrome.
Concomitant Use of Antacids
Antacids may be given concomitantly if needed.
Dosage Adjustment for Patients with Moderate or Severe Renal Insufficiency
In adult patients with moderate (creatinine clearance <50 mL/min) or severe (creatinine clearance <10 mL/min) renal insufficiency, the elimination half-life of famotidine is increased. For patients with severe renal insufficiency, it may exceed 20 hours, reaching approximately 24 hours in anuric patients. Since CNS adverse effects have been reported in patients with moderate and severe renal insufficiency, to avoid excess accumulation of the drug in patients with moderate or severe renal insufficiency, the dose of FLUXID™ may be reduced to half the dose or the dosing interval may be prolonged to 36-48 hours as indicated by the patient’s clinical response.
Based on the comparison of pharmacokinetic parameters for famotidine in adults and pediatric patients, dosage adjustment in pediatric patients with moderate or severe renal insufficiency should be considered.
HOW SUPPLIED
FLUXID™ (famotidine orally disintegrating tablets) 20 mg are white, round, biconvex, cherry-flavored and engraved “SP371” on one side and “20” on the other side. They are supplied as follows:
Bottles of 30 (unit-of-use)NDC 0091-3371-32
Bottles of 100NDC 0091-3371-01
FLUXID™ (famotidine orally disintegrating tablets) 40 mg are white, round, biconvex, cherry-flavored and engraved “SP372”on one side and “40” on the other side. They are supplied as follows:
Bottles of 30 (unit-of-use)NDC 0091-3372-32
Bottles of 100NDC 0091-3372-01
Store at 20° to 25°C (68° to 77°F); excursions permitted between 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature]. Protect from moisture.
Dispense in a tight container as defined in the USP/NF.
Manufactured for:
Milwaukee, WI 53201, USA
By: CIMA LABS INC.®
Eden Prairie, MN 55344, USA
FLUXID™ uses CIMA® U.S. Patent Nos. 6,024,981 and 6,221,392.
FLUXIDfamotidine TABLET, ORALLY DISINTEGRATING
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
FLUXIDfamotidine TABLET, ORALLY DISINTEGRATING
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||