Finasteride
Northstar Rx LLC
Actavis Totowa LLC
FULL PRESCRIBING INFORMATION
Finasteride, a synthetic 4-azasteroid compound, is a specific inhibitor of steroid Type II 5α-reductase, an intracellular enzyme that converts the androgen testosterone into 5α-dihydrotestosterone (DHT).
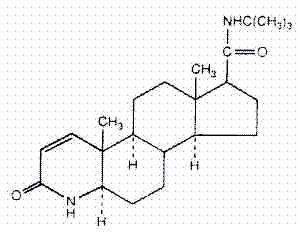
Finasteride is 4-azaandrost-1-ene-17-carboxamide, N-(1,1-dimethylethyl)-3-oxo-,(5α,17β)-. The empirical formula of finasteride is C23H36N2O2 and its molecular weight is 372.55. Its structural formula is:
Finasteride is a white crystalline powder with a melting point near 250°C. It is freely soluble in chloroform and in lower alcohol solvents, but is practically insoluble in water.
Finasteride tablets for oral administration are film-coated tablets that contain 5 mg of finasteride and the following inactive ingredients: FD&C Blue #2 Aluminum Lake, hypromellose, lactose monohydrate, lauryl macrogolglycerides, magnesium stearate, microcrystalline cellulose, polyethylene glycol, pregelatinized starch, sodium starch glycolate and titanium dioxide.
The development and enlargement of the prostate gland is dependent on the potent androgen, 5 α -dihydrotestosterone (DHT). Type II 5 α −reductase metabolizes testosterone to DHT in the prostate gland, liver and skin. DHT induces androgenic effects by binding to androgen receptors in the cell nuclei of these organs.
Finasteride is a competitive and specific inhibitor of Type II 5α-reductase with which it slowly forms a stable enzyme complex. Turnover from this complex is extremely slow (t½ ~30 days). This has been demonstrated both in vivo and in vitro. Finasteride has no affinity for the androgen receptor. In man, the 5 α -reduced steroid metabolites in blood and urine are decreased after administration of finasteride.
In man, a single 5-mg oral dose of finasteride produces a rapid reduction in serum DHT concentration, with the maximum effect observed 8 hours after the first dose. The suppression of DHT is maintained throughout the 24-hour dosing interval and with continued treatment. Daily dosing of finasteride at 5 mg/day for up to 4 years has been shown to reduce the serum DHT concentration by approximately 70%. The median circulating level of testosterone increased by approximately 10-20% but remained within the physiologic range.
Adult males with genetically inherited Type II 5 α -reductase deficiency also have decreased levels of DHT. Except for the associated urogenital defects present at birth, no other clinical abnormalities related to Type II 5 α -reductase deficiency have been observed in these individuals. These individuals have a small prostate gland throughout life and do not develop BPH.
In patients with BPH treated with finasteride (1-100 mg/day) for 7-10 days prior to prostatectomy, an approximate 80% lower DHT content was measured in prostatic tissue removed at surgery, compared to placebo; testosterone tissue concentration was increased up to 10 times over pretreatment levels, relative to placebo. Intraprostatic content of prostate-specific antigen (PSA) was also decreased.
In healthy male volunteers treated with finasteride for 14 days, discontinuation of therapy resulted in a return of DHT levels to pretreatment levels in approximately 2 weeks. In patients treated for three months, prostate volume, which declined by approximately 20%, returned to close to baseline value after approximately three months of discontinuation of therapy.
Absorption
In a study of 15 healthy young subjects, the mean bioavailability of finasteride 5-mg tablets was 63% (range 34-108%), based on the ratio of area under the curve (AUC) relative to an intravenous (IV) reference dose. Maximum finasteride plasma concentration averaged 37 ng/mL (range, 27-49 ng/mL) and was reached 1-2 hours postdose. Bioavailability of finasteride was not affected by food.
Distribution
Mean steady-state volume of distribution was 76 liters (range, 44-96 liters). Approximately 90% of circulating finasteride is bound to plasma proteins. There is a slow accumulation phase for finasteride after multiple dosing. After dosing with 5 mg/day of finasteride for 17 days, plasma concentrations of finasteride were 47 and 54% higher than after the first dose in men 45-60 years old (n=12) and ≥70 years old (n=12), respectively. Mean trough concentrations after 17 days of dosing were 6.2 ng/mL (range, 2.4-9.8 ng/mL) and 8.1 ng/mL (range, 1.8-19.7 ng/mL), respectively, in the two age groups. Although steady state was not reached in this study, mean trough plasma concentration in another study in patients with BPH (mean age, 65 years) receiving 5 mg/day was 9.4 ng/mL (range, 7.1-13.3 ng/mL; n=22) after over a year of dosing.
Finasteride has been shown to cross the blood brain barrier but does not appear to distribute preferentially to the CSF.
In 2 studies of healthy subjects (n=69) receiving finasteride 5 mg/day for 6-24 weeks, finasteride concentrations in semen ranged from undetectable (<0.1 ng/mL) to 10.54 ng/mL. In an earlier study using a less sensitive assay, finasteride concentrations in the semen of 16 subjects receiving finasteride 5 mg/day ranged from undetectable (<1.0 ng/mL) to 21 ng/mL. Thus, based on a 5-mL ejaculate volume, the amount of finasteride in semen was estimated to be 50- to 100-fold less than the dose of finasteride (5 µg) that had no effect on circulating DHT levels in men (see also PRECAUTIONS, Pregnancy).
Metabolism
Finasteride is extensively metabolized in the liver, primarily via the cytochrome P450 3A4 enzyme subfamily. Two metabolites, the t-butyl side chain monohydroxylated and monocarboxylic acid metabolites, have been identified that possess no more than 20% of the 5α-reductase inhibitory activity of finasteride.
Excretion
In healthy young subjects (n=15), mean plasma clearance of finasteride was 165 mL/min (range, 70-279 mL/min) and mean elimination half-life in plasma was 6 hours (range, 3-16 hours). Following an oral dose of 14C-finasteride in man (n=6), a mean of 39% (range, 32-46%) of the dose was excreted in the urine in the form of metabolites; 57% (range, 51-64%) was excreted in the feces.
The mean terminal half-life of finasteride in subjects ≥70 years of age was approximately 8 hours (range, 6-15 hours; n=12), compared with 6 hours (range, 4-12 hours; n=12) in subjects 45-60 years of age. As a result, mean AUC(0-24 hr) after 17 days of dosing was 15% higher in subjects ≥70 years of age than in subjects 45-60 years of age (p=0.02).
Special Populations
Pediatric: Finasteride pharmacokinetics have not been investigated in patients <18 years of age.
Gender: Finasteride pharmacokinetics in women are not available.
Geriatric: No dosage adjustment is necessary in the elderly. Although the elimination rate of finasteride is decreased in the elderly, these findings are of no clinical significance. See also Pharmacokinetics, Excretion, PRECAUTIONS, Geriatric Use and DOSAGE AND ADMINISTRATION.
Race: The effect of race on finasteride pharmacokinetics has not been studied.
Renal Insufficiency: No dosage adjustment is necessary in patients with renal insufficiency. In patients with chronic renal impairment, with creatinine clearances ranging from 9.0 to 55 mL/min, AUC, maximum plasma concentration, half-life, and protein binding after a single dose of 14C-finasteride were similar to values obtained in healthy volunteers. Urinary excretion of metabolites was decreased in patients with renal impairment. This decrease was associated with an increase in fecal excretion of metabolites. Plasma concentrations of metabolites were significantly higher in patients with renal impairment (based on a 60% increase in total radioactivity AUC). However, finasteride has been well tolerated in BPH patients with normal renal function receiving up to 80 mg/day for 12 weeks, where exposure of these patients to metabolites would presumably be much greater.
Hepatic Insufficiency: The effect of hepatic insufficiency on finasteride pharmacokinetics has not been studied. Caution should be used in the administration of finasteride in those patients with liver function abnormalities, as finasteride is metabolized extensively in the liver.
Drug Interactions
(also see PRECAUTIONS, Drug Interactions)
No drug interactions of clinical importance have been identified. Finasteride does not appear to affect the cytochrome P450-linked drug metabolism enzyme system. Compounds that have been tested in man have included antipyrine, digoxin, propranolol, theophylline, and warfarin, and no clinically meaningful interactions were found.
| Mean (± SD) | |
| *Range | |
| Bioavailability | 63% (34-108%)* |
| Clearance (mL/min) | 165 (55) |
| Volume of Distribution | 76 (14) |
| Half-Life (hours) | 6.2 (2.1) |
| Mean (± SD) | ||
| *First-dose values; all other parameters are last-dose values | ||
| 45-60 years old | ≥ 70 years old | |
| (n=12) | (n=12) | |
| AUC (ng•hr/mL) | 389 (98) | 463 (186) |
| Peak Concentration (ng/mL) | 46.2 (8.7) | 48.4 (14.7) |
| Time to Peak (hours) | 1.8 (0.7) | 1.8 (0.6) |
| Half-Life (hours)* | 6.0 (1.5) | 8.2 (2.5) |
Finasteride 5 mg/day was initially evaluated in patients with symptoms of BPH and enlarged prostates by digital rectal examination in two 1-year, placebo-controlled, randomized, double-blind studies and their 5-year open extensions.
Finasteride was further evaluated in a long-term efficacy and safety study, a double-blind, randomized, placebo-controlled, 4-year, multicenter study. 3040 patients between the ages of 45 and 78, with moderate to severe symptoms of BPH and an enlarged prostate upon digital rectal examination, were randomized into the study (1524 to finasteride, 1516 to placebo) and 3016 patients were evaluable for efficacy. 1883 patients completed the 4-year study (1000 in the finasteride group, 883 in the placebo group).
Effect on Symptom Score
Symptoms were quantified using a score similar to the American Urological Association Symptom Score, which evaluated both obstructive symptoms (impairment of size and force of stream, sensation of incomplete bladder emptying, delayed or interrupted urination) and irritative symptoms (nocturia, daytime frequency, need to strain or push the flow of urine) by rating on a 0 to 5 scale for six symptoms and a 0 to 4 scale for one symptom, for a total possible score of 34.
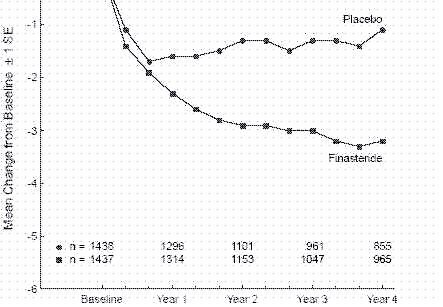
Patients in a long-term efficacy and safety study had moderate to severe symptoms at baseline (mean of approximately 15 points on a 0-34 point scale). Patients randomized to finasteride who remained on therapy for 4 years had a mean (± 1 SD) decrease in symptom score of 3.3 (± 5.8) points compared with 1.3 (± 5.6) points in the placebo group. (See Figure 1.) A statistically significant improvement in symptom score was evident at 1 year in patients treated with finasteride vs placebo (–2.3 vs –1.6), and this improvement continued through Year 4.
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Although an early improvement in urinary symptoms was seen in some patients, a therapeutic trial of at least 6 months was generally necessary to assess whether a beneficial response in symptom relief had been achieved. The improvement in BPH symptoms was seen during the first year and maintained throughout an additional 5 years of open extension studies.
Effect on the Need for Surgery
In a long-term efficacy and safety study, efficacy was also assessed by evaluating treatment failures. Treatment failure was prospectively defined as BPH-related urological events or clinical deterioration, lack of improvement and/or the need for alternative therapy. BPH-related urological events were defined as urological surgical intervention. Complete event information was available for 92% of the patients. The following table (Table 1) summarizes the results.
| All Treatment Failures in a long-term efficacy and safety study | |||||||
| Patients (%) | |||||||
| Event | Placebo | Finasteride | Relative | P | |||
| N=1503 | N=1513 | Risk** | 95 % CI | Value ** | |||
| * Patients with multiple events may be counted more than once for each type of event. | |||||||
| **Hazard ratio based on log rank test. | |||||||
| All Treatment Failures | 37.1 | 26.2 | 0.68 | (0.57 to 0.79) | <0.001 | ||
| Surgical Interventions for BPH | 10.1 | 4.6 | 0.45 | (0.32 to 0.63) | <0.001 | ||
| Two consecutive symptom scores >20 | 9.2 | 6.7 | |||||
| Bladder Stone | 0.4 | 0.5 | |||||
| Incontinence | 2.1 | 1.7 | |||||
| Renal Failure | 0.5 | 0.6 | |||||
| UTI | 5.7 | 4.9 | |||||
| Discontinuation due to worsening of BPH, lack of improvement, or to receive other medical treatment |
21.8 | 13.3 | |||||
Compared with placebo, finasteride was associated with a significantly lower need for BPH-related surgery [13.2% for placebo vs 6.6% for finasteride; 51% reduction in risk, 95% CI: (34 to 63%)]. Compared with placebo, finasteride was associated with a significantly lower risk for surgery [10.1% for placebo vs 4.6% for finasteride; 55% reduction in risk, 95% CI: (37 to 68%)]; see Figure 2.

| Placebo Group | ||||
| No. of events, cumulative | 37 | 89 | 121 | 162 |
| No. at risk per year | 1503 | 1454 | 1374 | 1314 |
| Finasteride Group | ||||
| No. of events, cumulative | 18 | 40 | 49 | 69 |
| No. at risk per year | 1513 | 1483 | 1438 | 1410 |
Effect on Maximum Urinary Flow Rate
In the patients in a long-term efficacy and safety study who remained on therapy for the duration of the study and had evaluable urinary flow data, finasteride increased maximum urinary flow rate by 1.9 mL/sec compared with 0.2 mL/sec in the placebo group.
There was a clear difference between treatment groups in maximum urinary flow rate in favor of finasteride by month 4 (1.0 vs 0.3 mL/sec) which was maintained throughout the study. In the earlier 1-year studies, increase in maximum urinary flow rate was comparable to a long-term efficacy and safety study and was maintained through the first year and throughout an additional 5 years of open extension studies.
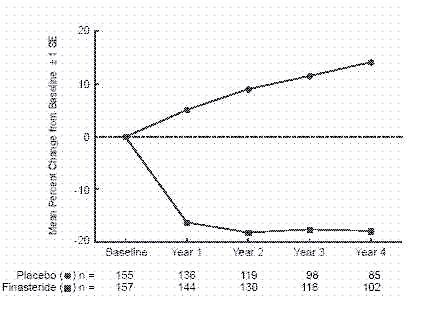
Effect on Prostate Volume
In a long-term efficacy and safety study, prostate volume was assessed yearly by magnetic resonance imaging (MRI) in a subset of patients. In patients treated with finasteride who remained on therapy, prostate volume was reduced compared with both baseline and placebo throughout the 4-year study. Finasteride decreased prostate volume by 17.9% (from 55.9 cc at baseline to 45.8 cc at 4 years) compared with an increase of 14.1% (from 51.3 cc to 58.5 cc) in the placebo group (p<0.001). (See Figure 3).
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Mean prostate volume at baseline ranged between 40-50 cc. The reduction in prostate volume was seen during the first year and maintained throughout an additional five years of open extension studies.
Prostate Volume as a Predictor of Therapeutic Response
A meta-analysis combining 1-year data from seven double-blind, placebo-controlled studies of similar design, including 4491 patients with symptomatic BPH, demonstrated that, in patients treated with finasteride, the magnitude of symptom response and degree of improvement in maximum urinary flow rate were greater in patients with an enlarged prostate at baseline.
Summary of Clinical Studies
The data from these studies, showing improvement in BPH-related symptoms, reduction in treatment failure (BPH-related urological events), increased maximum urinary flow rates, and decreasing prostate volume, suggest that finasteride arrests the disease process of BPH in men with an enlarged prostate.
Finasteride is indicated for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to:
- Improve symptoms
- Reduce the risk of the need for surgery including transurethral resection of the prostate (TURP) and prostatectomy.
Finasteride is contraindicated in the following:
Hypersensitivity to any component of this medication.
Pregnancy. Finasteride use is contraindicated in women when they are or may potentially be pregnant. Because of the ability of Type II 5α-reductase inhibitors to inhibit the conversion of testosterone to DHT, finasteride may cause abnormalities of the external genitalia of a male fetus of a pregnant woman who receives finasteride. If this drug is used during pregnancy, or if pregnancy occurs while taking this drug, the pregnant woman should be apprised of the potential hazard to the male fetus. (See also WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS and PRECAUTIONS, Information for Patients and Pregnancy.) In female rats, low doses of finasteride administered during pregnancy have produced abnormalities of the external genitalia in male offspring.
Finasteride is not indicated for use in pediatric patients (see PRECAUTIONS, Pediatric Use) or women (see also WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS; PRECAUTIONS, Information for Patients and Pregnancy; and HOW SUPPLIED).
Women should not handle crushed or broken finasteride tablets when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to a male fetus. Finasteride tablets are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets have not been broken or crushed. (See CONTRAINDICATIONS; PRECAUTIONS, Information for Patients and Pregnancy; and HOW SUPPLIED.)
Prior to initiating therapy with finasteride, appropriate evaluation should be performed to identify other conditions such as infection, prostate cancer, stricture disease, hypotonic bladder or other neurogenic disorders that might mimic BPH.
Patients with large residual urinary volume and/or severely diminished urinary flow should be carefully monitored for obstructive uropathy. These patients may not be candidates for finasteride therapy.
Caution should be used in the administration of finasteride in those patients with liver function abnormalities, as finasteride is metabolized extensively in the liver.
No clinical benefit has been demonstrated in patients with prostate cancer treated with finasteride. Patients with BPH and elevated PSA were monitored in controlled clinical studies with serial PSAs and prostate biopsies. In these BPH studies, finasteride did not appear to alter the rate of prostate cancer detection, and the overall incidence of prostate cancer was not significantly different in patients treated with finasteride or placebo.
Finasteride causes a decrease in serum PSA levels by approximately 50% in patients with BPH, even in the presence of prostate cancer. This decrease is predictable over the entire range of PSA values, although it may vary in individual patients. Analysis of PSA data from over 3000 patients in a long-term efficacy and safety study confirmed that in typical patients treated with finasteride for six months or more, PSA values should be doubled for comparison with normal ranges in untreated men. This adjustment preserves the sensitivity and specificity of the PSA assay and maintains its ability to detect prostate cancer.
Any sustained increases in PSA levels while on finasteride should be carefully evaluated, including consideration of non-compliance to therapy with finasteride.
Percent free PSA (free to total PSA ratio) is not significantly decreased by finasteride. The ratio of free to total PSA remains constant even under the influence of finasteride. If clinicians elect to use percent free PSA as an aid in the detection of prostate cancer in men undergoing finasteride therapy, no adjustment to its value appears necessary.
Women should not handle crushed or broken finasteride tablets when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to the male fetus (see CONTRAINDICATIONS; WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS; PRECAUTIONS, Pregnancy and HOW SUPPLIED).
Physicians should inform patients that the volume of ejaculate may be decreased in some patients during treatment with finasteride. This decrease does not appear to interfere with normal sexual function. However, impotence and decreased libido may occur in patients treated with finasteride (see ADVERSE REACTIONS).
Physicians should instruct their patients to promptly report any changes in their breasts such as lumps, pain or nipple discharge. Breast changes including breast enlargement, tenderness and neoplasm have been reported (see ADVERSE REACTIONS).
Physicians should instruct their patients to read the patient package insert before starting therapy with finasteride and to reread it each time the prescription is renewed so that they are aware of current information for patients regarding finasteride.
In patients with BPH, finasteride has no effect on circulating levels of cortisol, estradiol, prolactin, thyroid-stimulating hormone, or thyroxine. No clinically meaningful effect was observed on the plasma lipid profile (i.e., total cholesterol, low density lipoproteins, high density lipoproteins and triglycerides) or bone mineral density. Increases of about 10% were observed in luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in patients receiving finasteride, but levels remained within the normal range. In healthy volunteers, treatment with finasteride did not alter the response of LH and FSH to gonadotropin-releasing hormone indicating that the hypothalamic-pituitary-testicular axis was not affected.
Treatment with finasteride for 24 weeks to evaluate semen parameters in healthy male volunteers revealed no clinically meaningful effects on sperm concentration, mobility, morphology, or pH. A 0.6 mL (22.1%) median decrease in ejaculate volume with a concomitant reduction in total sperm per ejaculate was observed. These parameters remained within the normal range and were reversible upon discontinuation of therapy with an average time to return to baseline of 84 weeks.
No drug interactions of clinical importance have been identified. Finasteride does not appear to affect the cytochrome P450-linked drug metabolizing enzyme system. Compounds that have been tested in man have included antipyrine, digoxin, propranolol, theophylline, and warfarin and no clinically meaningful interactions were found.
Other Concomitant Therapy: Although specific interaction studies were not performed, finasteride was concomitantly used in clinical studies with acetaminophen, acetylsalicylic acid, angiotensin-converting enzyme (ACE) inhibitors, analgesics, anti-convulsants, beta-adrenergic blocking agents, diuretics, calcium channel blockers, cardiac nitrates, HMG-CoA reductase inhibitors, nonsteroidal anti-inflammatory drugs (NSAIDs), benzodiazepines, H2 antagonists and quinolone anti-infectives without evidence of clinically significant adverse interactions.
No evidence of a tumorigenic effect was observed in a 24-month study in Sprague-Dawley rats receiving doses of finasteride up to 160 mg/kg/day in males and 320 mg/kg/day in females. These doses produced respective systemic exposure in rats of 111 and 274 times those observed in man receiving the recommended human dose of 5 mg/day. All exposure calculations were based on calculated AUC(0-24 hr) for animals and mean AUC(0-24 hr) for man (0.4 µg•hr/mL).
In a 19-month carcinogenicity study in CD-1 mice, a statistically significant (p≤0.05) increase in the incidence of testicular Leydig cell adenomas was observed at a dose of 250 mg/kg/day (228 times the human exposure). In mice at a dose of 25 mg/kg/day (23 times the human exposure, estimated) and in rats at a dose of ≥40 mg/kg/day (39 times the human exposure) an increase in the incidence of Leydig cell hyperplasia was observed. A positive correlation between the proliferative changes in the Leydig cells and an increase in serum LH levels (2- to 3-fold above control) has been demonstrated in both rodent species treated with high doses of finasteride. No drug-related Leydig cell changes were seen in either rats or dogs treated with finasteride for 1 year at doses of 20 mg/kg/day and 45 mg/kg/day (30 and 350 times, respectively, the human exposure) or in mice treated for 19 months at a dose of 2.5 mg/kg/day (2.3 times the human exposure, estimated).
No evidence of mutagenicity was observed in an in vitro bacterial mutagenesis assay, a mammalian cell mutagenesis assay, or in an in vitro alkaline elution assay. In an in vitro chromosome aberration assay, using Chinese hamster ovary cells, there was a slight increase in chromosome aberrations. These concentrations correspond to 4000-5000 times the peak plasma levels in man given a total dose of 5 mg. In an in vivo chromosome aberration assay in mice, no treatment-related increase in chromosome aberration was observed with finasteride at the maximum tolerated dose of 250 mg/kg/day (228 times the human exposure) as determined in the carcinogenicity studies.
In sexually mature male rabbits treated with finasteride at 80 mg/kg/day (543 times the human exposure) for up to 12 weeks, no effect on fertility, sperm count, or ejaculate volume was seen. In sexually mature male rats treated with 80 mg/kg/day of finasteride (61 times the human exposure), there were no significant effects on fertility after 6 or 12 weeks of treatment; however, when treatment was continued for up to 24 or 30 weeks, there was an apparent decrease in fertility, fecundity and an associated significant decrease in the weights of the seminal vesicles and prostate. All these effects were reversible within 6 weeks of discontinuation of treatment. No drug-related effect on testes or on mating performance has been seen in rats or rabbits. This decrease in fertility in finasteride-treated rats is secondary to its effect on accessory sex organs (prostate and seminal vesicles) resulting in failure to form a seminal plug. The seminal plug is essential for normal fertility in rats and is not relevant in man.
Pregnancy Category X
See CONTRAINDICATIONS.
Finasteride is not indicated for use in women.
Administration of finasteride to pregnant rats at doses ranging from 100 µg/kg/day to 100 mg/kg/day (1-1000 times the recommended human dose of 5 mg/day) resulted in dose-dependent development of hypospadias in 3.6 to 100% of male offspring. Pregnant rats produced male offspring with decreased prostatic and seminal vesicular weights, delayed preputial separation and transient nipple development when given finasteride at ≥30 µg/kg/day (≥3/10 of the recommended human dose of 5 mg/day) and decreased anogenital distance when given finasteride at ≥3 µg/kg/day (≥3/100 of the recommended human dose of 5 mg/day). The critical period during which these effects can be induced in male rats has been defined to be days 16-17 of gestation. The changes described above are expected pharmacological effects of drugs belonging to the class of Type II 5α-reductase inhibitors and are similar to those reported in male infants with a genetic deficiency of Type II 5α-reductase. No abnormalities were observed in female offspring exposed to any dose of finasteride in utero.
No developmental abnormalities have been observed in first filial generation (F1) male or female offspring resulting from mating finasteride-treated male rats (80 mg/kg/day; 61 times the human exposure) with untreated females. Administration of finasteride at 3 mg/kg/day (30 times the recommended human dose of 5 mg/day) during the late gestation and lactation period resulted in slightly decreased fertility in F1 male offspring. No effects were seen in female offspring. No evidence of malformations has been observed in rabbit fetuses exposed to finasteride in utero from days 6-18 of gestation at doses up to 100 mg/kg/day (1000 times the recommended human dose of 5 mg/day). However, effects on male genitalia would not be expected since the rabbits were not exposed during the critical period of genital system development.
The in utero effects of finasteride exposure during the period of embryonic and fetal development were evaluated in the rhesus monkey (gestation days 20-100), a species more predictive of human development than rats or rabbits. Intravenous administration of finasteride to pregnant monkeys at doses as high as 800 ng/day (at least 60 to 120 times the highest estimated exposure of pregnant women to finasteride from semen of men taking 5 mg/day) resulted in no abnormalities in male fetuses. In confirmation of the relevance of the rhesus model for human fetal development, oral administration of a dose of finasteride (2 mg/kg/day; 20 times the recommended human dose of 5 mg/day or approximately 1-2 million times the highest estimated exposure to finasteride from semen of men taking 5 mg/day) to pregnant monkeys resulted in external genital abnormalities in male fetuses. No other abnormalities were observed in male fetuses and no finasteride-related abnormalities were observed in female fetuses at any dose.
Finasteride is not indicated for use in women.
It is not known whether finasteride is excreted in human milk.
Finasteride is not indicated for use in pediatric patients.
Safety and effectiveness in pediatric patients have not been established.
Of the total number of subjects included in a long-term efficacy and safety study, 1480 and 105 subjects were 65 and over and 75 and over, respectively. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients. No dosage adjustment is necessary in the elderly (see CLINICAL PHARMACOLOGY, Pharmacokinetics and Clinical Studies).
Finasteride is generally well tolerated; adverse reactions usually have been mild and transient.
4-Year Placebo-Controlled Study
In a long-term efficacy and safety study, 1524 patients treated with finasteride and 1516 patients treated with placebo were evaluated for safety over a period of 4 years. The most frequently reported adverse reactions were related to sexual function. 3.7% (57 patients) treated with finasteride and 2.1% (32 patients) treated with placebo discontinued therapy as a result of adverse reactions related to sexual function, which are the most frequently reported adverse reactions.
Table 2 presents the only clinical adverse reactions considered possibly, probably or definitely drug related by the investigator, for which the incidence on finasteride was ≥1% and greater than placebo over the 4 years of the study. In years 2-4 of the study, there was no significant difference between treatment groups in the incidences of impotence, decreased libido and ejaculation disorder.
| Drug-Related Adverse Experiences | ||||
| Year 1 | Years 2,3 and 4* | |||
| (%) | (%) | |||
| Finasteride | Placebo | Finasteride | Placebo | |
| *Combined Years 2-4 | ||||
| N = 1524 and 1516, finasteride vs placebo, respectively | ||||
| Impotence | 8.1 | 3.7 | 5.1 | 5.1 |
| Decreased Libido | 6.4 | 3.4 | 2.6 | 2.6 |
| Decreased Volume of Ejaculate | 3.7 | 0.8 | 1.5 | 0.5 |
| Ejaculation Disorder | 0.8 | 0.1 | 0.2 | 0.1 |
| Breast Enlargement | 0.5 | 0.1 | 1.8 | 1.1 |
| Breast Tenderness | 0.4 | 0.1 | 0.7 | 0.3 |
| Rash | 0.5 | 0.2 | 0.5 | 0.1 |
The adverse experience profile in the 1-year, placebo-controlled, Phase III studies, the 5-year open extensions, and a long-term efficacy and safety study were similar.
There is no evidence of increased adverse experiences with increased duration of treatment with finasteride. New reports of drug-related sexual adverse experiences decreased with duration of therapy.
During a 4- to 6-year placebo and comparator controlled study that enrolled 3047 men, there were 4 cases of breast cancer in men treated with finasteride but no cases in men not treated with finasteride. During the 4-year, placebo-controlled a long-term efficacy and safety study that enrolled 3040 men, there were 2 cases of breast cancer in placebo-treated men, but no cases were reported in men treated with finasteride. The relationship between long-term use of finasteride and male breast neoplasia is currently unknown.
In a 7-year placebo-controlled trial that enrolled 18,882 healthy men, 9060 had prostate needle biopsy data available for analysis. In the finasteride group, 280 (6.4%) men had prostate cancer with Gleason scores of 7-10 detected on needle biopsy vs. 237 (5.1%) men in the placebo group. Of the total cases of prostate cancer diagnosed in this study, approximately 98% were classified as intracapsular (stage T1 or T2). The clinical significance of these findings is unknown. This information from the literature (Thompson IM, Goodman PJ, Tangen CM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med 2003;349:213-22) is provided for consideration by physicians when finasteride is used as indicated (see INDICATIONS AND USAGE). Finasteride is not approved to reduce the risk of developing prostate cancer.
The following additional adverse effects have been reported in post-marketing experience:
- hypersensitivity reactions, including pruritus, urticaria, and swelling of the lips and face
- testicular pain.
Patients have received single doses of finasteride up to 400 mg and multiple doses of finasteride up to 80 mg/day for three months without adverse effects. Until further experience is obtained, no specific treatment for an overdose with finasteride can be recommended.
Significant lethality was observed in male and female mice at single oral doses of 1500 mg/m2 (500 mg/kg) and in female and male rats at single oral doses of 2360 mg/m2 (400 mg/kg) and 5900 mg/m2 (1000 mg/kg), respectively.
The recommended dose is 5 mg orally once a day.
Finasteride may be administered with or without meals. No dosage adjustment is necessary for patients with renal impairment or for the elderly (see CLINICAL PHARMACOLOGY, Pharmacokinetics).
Finasteride Tablets, USP 5 mg are blue, round, biconvex film-coated tablets, with “F5” on one side and “ ” on the other. Available in bottles of 30’s (NDC 16714-522-01), 90’s (NDC 16714-522-03), 100’s (NDC 16714-522-04) and 500’s (NDC 16714-522-05).
” on the other. Available in bottles of 30’s (NDC 16714-522-01), 90’s (NDC 16714-522-03), 100’s (NDC 16714-522-04) and 500’s (NDC 16714-522-05).
Store at 20 to 25°C (68 to 77°F) with excursions permitted between 15 to 30°C (59 to 86°F) [See USP Controlled Room Temperature].
Protect from light and keep container tightly closed.
Women should not handle crushed or broken finasteride tablets when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to the male fetus (see CONTRAINDICATIONS; WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS; PRECAUTIONS, Pregnancy and HOW SUPPLIED).
Physicians should inform patients that the volume of ejaculate may be decreased in some patients during treatment with finasteride. This decrease does not appear to interfere with normal sexual function. However, impotence and decreased libido may occur in patients treated with finasteride (see ADVERSE REACTIONS).
Physicians should instruct their patients to promptly report any changes in their breasts such as lumps, pain or nipple discharge. Breast changes including breast enlargement, tenderness and neoplasm have been reported (see ADVERSE REACTIONS).
Physicians should instruct their patients to read the patient package insert before starting therapy with finasteride and to reread it each time the prescription is renewed so that they are aware of current information for patients regarding finasteride.
Manufactured For:
-
Northstar Rx LLC
-
Memphis, TN 38141
Manufactured by:
Intas Pharmaceuticals Ltd.
Ahmedabad, India- 382210
Code: Guj/Drugs/1339
10 5425 1 624374
Rev. 07/10
ABOUT
FINASTERIDE TABLETS, USP 5 mg
(fin-AS-tur-eyed)
Finasteride is for use by men only.
Please read this leaflet before you start taking finasteride. Also, read it each time you renew your prescription, just in case anything has changed. Remember, this leaflet does not take the place of careful discussions with your doctor. You and your doctor should discuss finasteride when you start taking your medication and at regular checkups.
Why your doctor has prescribed finasteride?
Your doctor has prescribed finasteride because you have a medical condition called benign prostatic hyperplasia or BPH. This occurs only in men.
What is BPH?
BPH is an enlargement of the prostate gland. After age 50, most men develop enlarged prostates. The prostate is located below the bladder. As the prostate enlarges, it may slowly restrict the flow of urine. This can lead to symptoms such as:
- a weak or interrupted urinary stream
- a feeling that you cannot empty your bladder completely
- a feeling of delay or hesitation when you start to urinate
- a need to urinate often, especially at night
- a feeling that you must urinate right away.
In some men, BPH can lead to serious problems, including urinary tract infections, as well as the need for surgery.
Treatment options for BPH
There are three main treatment options for symptoms of BPH:
- Program of monitoring or “Watchful Waiting”. If a man has an enlarged prostate gland and no symptoms or if his symptoms do not bother him, he and his doctor may decide on a program of monitoring which would include regular checkups, instead of medication or surgery.
- Medication. Your doctor may prescribe finasteride for BPH. See “What finasteride does” below.
- Surgery. Some patients may need surgery. Your doctor can suggest several different surgical procedures for BPH. Which procedure is best depends on your symptoms and medical condition.
There are two main treatment options to reduce the risk of serious problems due to BPH:
- Medication. Your doctor may prescribe finasteride for BPH. See “What finasteride does” below.
- Surgery. Some patients may need surgery. Your doctor can suggest several different surgical procedures for BPH. Which procedure is best depends on your symptoms and medical condition.
What finasteride does
Finasteride lowers levels of a key hormone called DHT (dihydrotestosterone), which is a major cause of prostate growth. Lowering DHT leads to shrinkage of the enlarged prostate gland in most men. This can lead to gradual improvement in urine flow and symptoms over the next several months. Finasteride will help reduce the risk of the need for surgery. However, since each case of BPH is different, you should know that:
- Even though the prostate shrinks, you may NOT notice an improvement in urine flow or symptoms.
- You may need to take finasteride for six (6) months or more to see whether it improves your symptoms.
- Therapy with finasteride may reduce the need for surgery.
What you need to know while taking finasteride
• You must see your doctor regularly. While taking finasteride, you must have regular checkups.
Follow your doctor's advice about when to have these checkups.
• About side effects. Like all prescription drugs, finasteride may cause side effects. Side effects due to finasteride may include impotence (an inability to have an erection) or less desire for sex.
Some men taking finasteride may have changes or problems with ejaculation, such as a decrease in the amount of semen released during sex. This decrease in the amount of semen does not appear to interfere with normal sexual function. In some cases these side effects went away while the patient continued to take finasteride.
In addition, some men may have breast enlargement and/or tenderness. You should promptly report to your doctor any changes in your breasts such as lumps, pain or nipple discharge. Some men have reported allergic reactions such as rash, itching, hives, and swelling of the lips and face. Rarely, testicular pain has been reported.
You should discuss side effects with your doctor before taking finasteride and anytime you think you are having a side effect.
• Checking for prostate cancer. Your doctor has prescribed finasteride for symptomatic BPH and not for cancer — but a man can have BPH and prostate cancer at the same time. Doctors usually recommend that men be checked for prostate cancer once a year when they turn 50 (or 40 if a family member has had prostate cancer). These checks should continue while you take finasteride. Finasteride is not a treatment for prostate cancer.
• About Prostate-Specific Antigen (PSA).
Your doctor may have done a blood test called PSA. Finasteride can alter PSA values. For more information, talk to your doctor.
• A warning about finasteride and pregnancy.
Finasteride is for use by MEN only.
Women who are or may potentially be pregnant must not use finasteride. They should also not handle crushed or broken tablets of finasteride.
If a woman who is pregnant with a male baby absorbs the active ingredient in finasteride after oral use or through the skin, it may cause the male baby to be born with abnormalities of the sex organs.
Finasteride tablets are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets are not broken or crushed.
If a woman who is pregnant comes into contact with the active ingredient in finasteride, a doctor should be consulted.
Remember, these warnings apply only when the woman is pregnant or could potentially be pregnant.
How to take finasteride
Follow your doctor's advice about how to take finasteride. You must take it every day. You may take it with or between meals. To avoid forgetting to take finasteride, it may be helpful to take it at the same time every day.
Do not share finasteride with anyone else; it was prescribed only for you.
Keep finasteride and all medicines out of the reach of children.
FOR MORE INFORMATION ABOUT ‘finasteride’ AND BPH, TALK WITH YOUR DOCTOR.
IN ADDITION, TALK TO YOUR PHARMACIST OR OTHER HEALTH CARE PROVIDER.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1800-FDA-1088.
Manufactured For:
-
Northstar Rx LLC
-
Memphis, TN 38141
Manufactured by:
Intas Pharmaceuticals Ltd.
Ahmedabad, India- 382210
Code: Guj/Drugs/1339
10 5425 1 624374
Rev. 07/10

FinasterideFinasteride TABLET, FILM COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||