Doxazosin
FULL PRESCRIBING INFORMATION
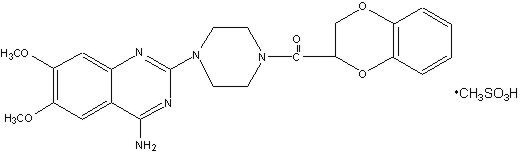
Doxazosin mesylate is a quinazoline compound that is a selective inhibitor of the alpha1 subtype of alpha adrenergic receptors. The chemical name of doxazosin mesylate is 1-(4-amino-6,7-dimethoxy-2-quinazolinyl)-4-(1,4-benzodioxan-2-ylcarbonyl) piperazine methanesulfonate. The molecular formula for doxazosin mesylate is C23H25N5O5 • CH4O3S and the molecular weight is 547.6. It has the following structure:
Doxazosin mesylate is freely soluble in dimethylsulfoxide, soluble in dimethylformamide, slightly soluble in methanol, ethanol, and water (0.8% at 25°C), and very slightly soluble in acetone and methylene chloride.
Benign prostatic hyperplasia (BPH) is a common cause of urinary outflow obstruction in aging males. Severe BPH may lead to urinary retention and renal damage. A static and a dynamic component contribute to the symptoms and reduced urinary flow rate associated with BPH. The static component is related to an increase in prostate size caused, in part, by a proliferation of smooth muscle cells in the prostatic stroma. However, the severity of BPH symptoms and the degree of urethral obstruction do not correlate well with the size of the prostate. The dynamic component of BPH is associated with an increase in smooth muscle tone in the prostate and bladder neck. The degree of tone in this area is mediated by the alpha1 adrenoceptor, which is present in high density in the prostatic stroma, prostatic capsule and bladder neck. Blockade of the alpha1 receptor decreases urethral resistance and may relieve the obstruction and BPH symptoms. In the human prostate, doxazosin antagonizes phenylephrine (alpha1 agonist)-induced contractions,in vitro, and binds with high affinity to the alpha1c adrenoceptor. The receptor subtype is thought to be the predominant functional type in the prostate. Doxazosin acts within 1 to 2 weeks to decrease the severity of BPH symptoms and improve urinary flow rate. Since alpha1 adrenoceptors are of low density in the urinary bladder (apart from the bladder neck), doxazosin should maintain bladder contractility.
In BPH patients (N = 450) treated for up to 2 years in open-label studies, doxazosin therapy resulted in significant improvement above baseline in urinary flow rates and BPH symptoms. The significant effects of doxazosin were maintained over the entire treatment period.
Although blockade of alpha1 adrenoceptors also lowers blood pressure in hypertensive patients with increased peripheral vascular resistance, doxazosin treatment of normotensive men with BPH did not result in a clinically significant blood pressure lowering effect (Table 2). The proportion of normotensive patients with a sitting systolic blood pressure less than 90 mmHg and/or diastolic blood pressure less than 60 mmHg at any time during treatment with doxazosin 1 to 8 mg once daily was 6.7% with doxazosin and not significantly different (statistically) from that with placebo (5%).
The mechanism of action of doxazosin mesylate is selective blockade of the alpha1 (postjunctional) subtype of adrenergic receptors. Studies in normal human subjects have shown that doxazosin competitively antagonized the pressor effects of phenylephrine (an alpha1 agonist) and the systolic pressor effect of norepinephrine. Doxazosin and prazosin have similar abilities to antagonize phenylephrine. The antihypertensive effect of doxazosin results from a decrease in systemic vascular resistance. The parent compound doxazosin is primarily responsible for the antihypertensive activity. The low plasma concentrations of known active and inactive metabolites of doxazosin (2-piperazinyl, 6'- and 7'-hydroxy and 6- and 7-O-desmethyl compounds) compared to parent drug indicate that the contribution of even the most potent compound (6'-hydroxy) to the antihypertensive effect of doxazosin in man is probably small. The 6'- and 7'-hydroxy metabolites have demonstrated antioxidant properties at concentrations of 5 mcM, in vitro.
Administration of doxazosin results in a reduction in systemic vascular resistance. In patients with hypertension there is little change in cardiac output. Maximum reductions in blood pressure usually occur 2 to 6 hours after dosing and are associated with a small increase in standing heart rate. Like other alpha1-adrenergic blocking agents, doxazosin has a greater effect on blood pressure and heart rate in the standing position.
In a pooled analysis of placebo-controlled hypertension studies with about 300 hypertensive patients per treatment group, doxazosin, at doses of 1 to 16 mg given once daily, lowered blood pressure at 24 hours by about 10/8 mmHg compared to placebo in the standing position and about 9/5 mmHg in the supine position. Peak blood pressure effects (1 to 6 hours) were larger by about 50 to 75% (i.e., trough values were about 55 to 70% of peak effect), with the larger peak-trough differences seen in systolic pressures. There was no apparent difference in the blood pressure response of caucasians and blacks or of patients above and below age 65. In these predominantly normocholesterolemic patients doxazosin produced small reductions in total serum cholesterol (2 to 3%), LDL cholesterol (4%), and a similarly small increase in HDL/total cholesterol ratio (4%). The clinical significance of these findings is uncertain. In the same patient population, patients receiving doxazosin gained a mean of 0.6 kg compared to a mean loss of 0.1 kg for placebo patients.
After oral administration of therapeutic doses, peak plasma levels of doxazosin mesylate occur at about 2 to 3 hours. Bioavailability is approximately 65%, reflecting first pass metabolism of doxazosin by the liver. The effect of food on the pharmacokinetics of doxazosin was examined in a crossover study with 12 hypertensive subjects. Reductions of 18% in mean maximum plasma concentration and 12% in the area under the concentration-time curve occurred when doxazosin was administered with food. Neither of these differences was statistically or clinically significant.
Doxazosin is extensively metabolized in the liver, mainly by O-demethylation of the quinazoline nucleus or hydroxylation of the benzodioxan moiety. Although several active metabolites of doxazosin have been identified, the pharmacokinetics of these metabolites have not been characterized. In a study of two subjects administered radiolabelled doxazosin 2 mg orally and 1 mg intravenously on two separate occasions, approximately 63% of the dose was eliminated in the feces and 9% of the dose was found in the urine. On average only 4.8% of the dose was excreted as unchanged drug in the feces and only a trace of the total radioactivity in the urine was attributed to unchanged drug. At the plasma concentrations achieved by therapeutic doses approximately 98% of the circulating drug is bound to plasma proteins.
Plasma elimination of doxazosin is biphasic, with a terminal elimination half-life of about 22 hours. Steady-state studies in hypertensive patients given doxazosin doses of 2 to 16 mg once daily showed linear kinetics and dose proportionality. In two studies, following the administration of 2 mg orally once daily, the mean accumulation ratios (steady-state AUC vs. first dose AUC) were 1.2 and 1.7. Enterohepatic recycling is suggested by secondary peaking of plasma doxazosin concentrations.
In a crossover study in 24 normotensive subjects, the pharmacokinetics and safety of doxazosin were shown to be similar with morning and evening dosing regimens. The area under the curve after morning dosing was, however, 11% less than that after evening dosing and the time to peak concentration after evening dosing occurred significantly later than that after morning dosing (5.6 hr vs. 3.5 hr).
Uses
Doxazosin tablets are indicated for the treatment of both the urinary outflow obstruction and obstructive and irritative symptoms associated with BPH: obstructive symptoms (hesitation, intermittency, dribbling, weak urinary stream, incomplete emptying of the bladder) and irritative symptoms (nocturia, daytime frequency, urgency, burning). Doxazosin may be used in all BPH patients whether hypertensive or normotensive. In patients with hypertension and BPH, both conditions were effectively treated with doxazosin monotherapy. Doxazosin provides rapid improvement in symptoms and urinary flow rate in 66 to 71% of patients. Sustained improvements with doxazosin were seen in patients treated for up to 14 weeks in double-blind studies and up to 2 years in open-label studies.
Doxazosin tablets are also indicated for the treatment of hypertension. Doxazosin may be used alone or in combination with diuretics, beta-adrenergic blocking agents, calcium channel blockers or angiotensin-converting enzyme inhibitors.
Doxazosin tablets are contraindicated in patients with a known sensitivity to quinazolines (e.g., prazosin, terazosin), doxazosin, or any of the inert ingredients.
Doxazosin, like other alpha-adrenergic blocking agents, can cause marked hypotension, especially in the upright position, with syncope and other postural symptoms such as dizziness. Marked orthostatic effects are most common with the first dose but can also occur when there is a dosage increase, or if therapy is interrupted for more than a few days. To decrease the likelihood of excessive hypotension and syncope, it is essential that treatment be initiated with the 1 mg dose. The 2, 4, and 8 mg tablets are not for initial therapy. Dosage should then be adjusted slowly (see DOSAGE AND ADMINISTRATION section) with evaluations and increases in dose every two weeks to the recommended dose. Additional antihypertensive agents should be added with caution.
Patients being titrated with doxazosin should be cautioned to avoid situations where injury could result should syncope occur, during both the day and night.
In an early investigational study of the safety and tolerance of increasing daily doses of doxazosin in normotensives beginning at 1 mg/day, only 2 of 6 subjects could tolerate more than 2 mg/day without experiencing symptomatic postural hypotension. In another study of 24 healthy normotensive male subjects receiving initial doses of 2 mg/day of doxazosin, seven (29%) of the subjects experienced symptomatic postural hypotension between 0.5 and 6 hours after the first dose necessitating termination of the study. In this study, 2 of the normotensive subjects experienced syncope. Subsequent trials in hypertensive patients always began doxazosin dosing at 1 mg/day resulting in a 4% incidence of postural side effects at 1 mg/day with no cases of syncope.
In multiple dose clinical trials in hypertension involving over 1,500 hypertensive patients with dose titration every one to two weeks, syncope was reported in 0.7% of patients. None of these events occurred at the starting dose of 1 mg and 1.2% (8/664) occurred at 16 mg/day.
In placebo-controlled, clinical trials in BPH, 3 out of 665 patients (0.5%) taking doxazosin reported syncope. Two of the patients were taking 1 mg doxazosin, while one patient was taking 2 mg doxazosin when syncope occurred. In the open-label, long-term extension follow-up of approximately 450 BPH patients, there were 3 reports of syncope (0.7%). One patient was taking 2 mg, one patient was taking 8 mg and one patient was taking 12 mg when syncope occurred. In a clinical pharmacology study, one subject receiving 2 mg experienced syncope.
If syncope occurs, the patient should be placed in a recumbent position and treated supportively as necessary.
Rarely (probably less frequently than once in every several thousand patients), alpha1 antagonists, including doxazosin, have been associated with priapism (painful penile erection, sustained for hours and unrelieved by sexual intercourse or masturbation). Because this condition can lead to permanent impotence if not promptly treated, patients must be advised about the seriousness of the condition (see PRECAUTIONS: Information for Patients).
Carcinoma of the prostate causes many of the symptoms associated with BPH and the two disorders frequently co-exist. Carcinoma of the prostate should therefore be ruled out prior to commencing therapy with doxazosin.
Intraoperative Floppy Iris Syndrome (IFIS) has been observed during cataract surgery in some patients on or previously treated with alpha1 blockers. This variant of small pupil syndrome is characterized by the combination of a flaccid iris that billows in response to intraoperative irrigation currents, progressive intraoperative miosis despite preoperative dilation with standard mydriatic drugs, and potential prolapse of the iris toward the phacoemulsification incisions. The patient's surgeon should be prepared for possible modifications to their surgical technique, such as the utilization of iris hooks, iris dilator rings, or viscoelastic substances. There does not appear to be a benefit of stopping alpha1 blocker therapy prior to cataract surgery.
While syncope is the most severe orthostatic effect of doxazosin, other symptoms of lowered blood pressure, such as dizziness, lightheadedness, or vertigo can occur, especially at initiation of therapy or at the time of dose increases.
These symptoms were common in clinical trials in hypertension, occurring in up to 23% of all patients treated and causing discontinuation of therapy in about 2%.
In placebo-controlled titration trials in hypertension, orthostatic effects were minimized by beginning therapy at 1 mg per day and titrating every two weeks to 2, 4, or 8 mg per day. There was an increased frequency of orthostatic effects in patients given 8 mg or more, 10%, compared to 5% at 1 to 4 mg and 3% in the placebo group.
In placebo-controlled trials in BPH, the incidence of orthostatic hypotension with doxazosin was 0.3% and did not increase with increasing dosage (to 8 mg/day). The incidence of discontinuations due to hypotensive or orthostatic symptoms was 3.3% with doxazosin and 1% with placebo. The titration interval in these studies was one to two weeks.
Patients in occupations in which orthostatic hypotension could be dangerous should be treated with particular caution. As alpha1 antagonists can cause orthostatic effects, it is important to evaluate standing blood pressure two minutes after standing and patients should be advised to exercise care when arising from a supine or sitting position.
If hypotension occurs, the patient should be placed in the supine position and, if this measure is inadequate, volume expansion with intravenous fluids or vasopressor therapy may be used. A transient hypotensive response is not a contraindication to further doses of doxazosin.
(See Patient Leaflet)
Patients should be made aware of the possibility of syncopal and orthostatic symptoms, especially at the initiation of therapy, and urged to avoid driving or hazardous tasks for 24 hours after the first dose, after a dosage increase, and after interruption of therapy when treatment is resumed. They should be cautioned to avoid situations where injury could result should syncope occur during initiation of doxazosin therapy. They should also be advised of the need to sit or lie down when symptoms of lowered blood pressure occur, although these symptoms are not always orthostatic, and to be careful when rising from a sitting or lying position. If dizziness, lightheadedness, or palpitations are bothersome they should be reported to the physician, so that dose adjustment can be considered. Patients should also be told that drowsiness or somnolence can occur with doxazosin or any selective alpha1 adrenoceptor antagonist, requiring caution in people who must drive or operate heavy machinery.
Patients should be advised about the possibility of priapism as a result of treatment with alpha1 antagonists. Patients should know that this adverse event is very rare. If they experience priapism, it should be brought to immediate medical attention for if not treated promptly it can lead to permanent erectile dysfunction (impotence).
Doxazosin does not affect the plasma concentration of prostate specific antigen in patients treated for up to 3 years. Both doxazosin, an alpha1 inhibitor, and finasteride, a 5-alpha reductase inhibitor, are highly protein bound and hepatically metabolized. There is no definitive controlled clinical experience on the concomitant use of alpha1 inhibitors and 5-alpha reductase inhibitors at this time.
Doxazosin should be administered with caution to patients with evidence of impaired hepatic function or to patients receiving drugs known to influence hepatic metabolism (see CLINICAL PHARMACOLOGY).
Analysis of hematologic data from hypertensive patients receiving doxazosin in controlled hypertension clinical trials showed that the mean WBC (N = 474) and mean neutrophil counts (N = 419) were decreased by 2.4% and 1%, respectively, compared to placebo, a phenomenon seen with other alpha blocking drugs. In BPH patients the incidence of clinically significant WBC abnormalities was 0.4% (2/459) with doxazosin and 0% (0/147) with placebo, with no statistically significant difference between the two treatment groups. A search through a data base of 2,400 hypertensive patients and 665 BPH patients revealed 4 hypertensives in which drug-related neutropenia could not be ruled out and one BPH patient in which drug-related leukopenia could not be ruled out. Two hypertensives had a single low value on the last day of treatment. Two hypertensives had stable, non-progressive neutrophil counts in the 1000/mm3 range over periods of 20 and 40 weeks. One BPH patient had a decrease from WBC count of 4800/mm3 to 2700/mm3 at the end of the study; there was no evidence of clinical impairment. In cases where follow-up was available the WBCs and neutrophil counts returned to normal after discontinuation of doxazosin. No patients became symptomatic as a result of the low WBC or neutrophil counts.
Most (98%) of plasma doxazosin is protein bound. In vitro data in human plasma indicate that doxazosin has no effect on protein binding of digoxin, warfarin, phenytoin or indomethacin. There is no information on the effect of other highly plasma protein bound drugs on doxazosin binding. Doxazosin has been administered without any evidence of an adverse drug interaction to patients receiving thiazide diuretics, beta-blocking agents, and nonsteroidal anti-inflammatory drugs. In a placebo-controlled trial in normal volunteers, the administration of a single 1 mg dose of doxazosin on day 1 of a 4-day regimen of oral cimetidine (400 mg twice daily) resulted in a 10% increase in mean AUC of doxazosin (p = 0.006), and a slight but not statistically significant increase in mean Cmax and mean half-life of doxazosin. The clinical significance of this increase in doxazosin AUC is unknown.
In clinical trials, doxazosin tablets have been administered to patients on a variety of concomitant medications; while no formal interaction studies have been conducted, no interactions were observed. Doxazosin tablets have been used with the following drugs or drug classes: 1) analgesic/anti-inflammatory (e.g., acetaminophen, aspirin, codeine and codeine combinations, ibuprofen, indomethacin); 2) antibiotics (e.g., erythromycin, trimethoprim and sulfamethoxazole, amoxicillin); 3) antihistamines (e.g., chlorpheniramine); 4) cardiovascular agents (e.g., atenolol, hydrochlorothiazide, propranolol); 5) corticosteroids; 6) gastrointestinal agents (e.g., antacids); 7) hypoglycemics and endocrine drugs; 8) sedatives and tranquilizers (e.g., diazepam); 9) cold and flu remedies.
An increased incidence of myocardial necrosis or fibrosis was displayed by Sprague-Dawley rats after 6 months of dietary administration at concentrations calculated to provide 80 mg doxazosin/kg/day and after 12 months of dietary administration at concentrations calculated to provide 40 mg doxazosin/kg/day (AUC exposure in rats 8 times the human AUC exposure with a 12 mg/day therapeutic dose). Myocardial fibrosis was observed in both rats and mice treated in the same manner with 40 mg doxazosin/kg/day for 18 months (exposure 8 times human AUC exposure in rats and somewhat equivalent to human Cmax exposure in mice). No cardiotoxicity was observed at lower doses (up to 10 or 20 mg/kg/day, depending on the study) in either species. These lesions were not observed after 12 months of oral dosing in dogs at maximum doses of 20 mg/kg/day [maximum plasma concentrations (Cmax) in dogs 14 times the Cmax exposure in humans receiving a 12 mg/day therapeutic dose] and in Wistar rats at doses of 100 mg/kg/day (Cmax exposures 15 times human Cmax exposure with a 12 mg/day therapeutic dose). There is no evidence that similar lesions occur in humans.
Chronic dietary administration (up to 24 months) of doxazosin mesylate at maximally tolerated doses of 40 mg/kg/day in rats and 120 mg/kg/day in mice revealed no evidence of carcinogenic potential. The highest doses evaluated in the rat and mouse studies are associated with AUCs (a measure of systemic exposure) that are 8 times and 4 times, respectively, the human AUC at a dose of 16 mg/day.
Mutagenicity studies revealed no drug- or metabolite-related effects at either chromosomal or subchromosomal levels.
Studies in rats showed reduced fertility in males treated with doxazosin at oral doses of 20 (but not 5 or 10) mg/kg/day, about 4 times the AUC exposures obtained with a 12 mg/day human dose. This effect was reversible within two weeks of drug withdrawal. There have been no reports of any effects of doxazosin on male fertility in humans.
Studies in pregnant rabbits and rats at daily oral doses of up to 41 and 20 mg/kg, respectively (plasma drug concentrations 10 and 4 times human Cmax and AUC exposures with a 12 mg/day therapeutic dose), have revealed no evidence of harm to the fetus. A dosage regimen of 82 mg/kg/day in the rabbit was associated with reduced fetal survival. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, doxazosin should be used during pregnancy only if clearly needed.
Radioactivity was found to cross the placenta following oral administration of labeled doxazosin to pregnant rats.
In peri-postnatal studies in rats, postnatal development at maternal doses of 40 or 50 mg/kg/day of doxazosin (8 times human AUC exposure with a 12 mg/day therapeutic dose) was delayed as evidenced by slower body weight gain and a slightly later appearance of anatomical features and reflexes.
Studies in lactating rats given a single oral dose of 1 mg/kg of [2-14C]-doxazosin indicate that doxazosin accumulates in rat breast milk with a maximum concentration about 20 times greater than the maternal plasma concentration. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when doxazosin is administered to a nursing mother.
The safety and effectiveness of doxazosin as an antihypertensive agent have not been established in pediatric patients.
The safety and effectiveness profile of doxazosin in BPH was similar in the elderly (age ≥ 65 years) and younger (age less 65 years) patients.
Clinical studies of doxazosin did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
The incidence of adverse events has been ascertained from worldwide clinical trials in 965 BPH patients. The incidence rates presented below (Table 3) are based on combined data from seven placebo-controlled trials involving once daily administration of doxazosin in doses of 1 to 16 mg in hypertensives and 0.5 to 8 mg in normotensives. The adverse events when the incidence in the doxazosin group was at least 1% are summarized in Table 3. No significant difference in the incidence of adverse events compared to placebo was seen except for dizziness, fatigue, hypotension, edema and dyspnea. Dizziness and dyspnea appeared to be dose-related.
Cardiovascular System:Urogenital System:Psychiatric Disorders:The majority of adverse experiences with doxazosin were mild.
Doxazosin mesylate has been administered to approximately 4,000 hypertensive patients, of whom 1,679 were included in the hypertension clinical development program. In that program, minor adverse effects were frequent, but led to discontinuation of treatment in only 7% of patients. In placebo-controlled studies adverse effects occurred in 49% and 40% of patients in the doxazosin and placebo groups, respectively, and led to discontinuation in 2% of patients in each group. The major reasons for discontinuation were postural effects (2%), edema, malaise/fatigue, and some heart rate disturbance, each about 0.7%.
In controlled hypertension clinical trials directly comparing doxazosin to placebo there was no significant difference in the incidence of side effects, except for dizziness (including postural), weight gain, somnolence and fatigue/malaise. Postural effects and edema appeared to be dose related. The prevalence rates presented below are based on combined data from placebo-controlled studies involving once daily administration of doxazosin at doses ranging from 1 to 16 mg. Table 4 summarizes those adverse experiences (possibly/probably related) reported for patients in these hypertension studies where the prevalence rate in the doxazosin group was at least 0.5% or where the reaction is of particular interest.
Experience with doxazosin overdosage is limited. Two adolescents who each intentionally ingested 40 mg doxazosin with diclofenac or acetaminophen, were treated with gastric lavage with activated charcoal and made full recoveries. A two-year-old child who accidentally ingested 4 mg doxazosin was treated with gastric lavage and remained normotensive during the five-hour emergency room observation period. A six-month-old child accidentally received a crushed 1 mg tablet of doxazosin and was reported to have been drowsy. A 32-year-old female with chronic renal failure, epilepsy and depression intentionally ingested 60 mg doxazosin (blood level 0.9 mcg/mL; normal values in hypertensives = 0.02 mcg/mL); death was attributed to a grand mal seizure resulting from hypotension. A 39-year-old female who ingested 70 mg doxazosin, alcohol and flurazepam developed hypotension which responded to fluid therapy.
The oral LD50 of doxazosin is greater than 1000 mg/kg in mice and rats. The most likely manifestation of overdosage would be hypotension, for which the usual treatment would be intravenous infusion of fluid. As doxazosin is highly protein bound, dialysis would not be indicated.
DOSAGE MUST BE INDIVIDUALIZED. The initial dosage of doxazosin tablets in patients with hypertension and/or BPH is 1 mg given once daily in the a.m. or p.m. This starting dose is intended to minimize the frequency of postural hypotension and first dose syncope associated with doxazosin. Postural effects are most likely to occur between 2 and 6 hours after a dose. Therefore blood pressure measurements should be taken during this time period after the first dose and with each increase in dose. If doxazosin tablets administration is discontinued for several days, therapy should be restarted using the initial dosing regimen.
The initial dosage of doxazosin is 1 mg, given once daily in the a.m. or p.m. Depending on the individual patient's urodynamics and BPH symptomatology, dosage may then be increased to 2 mg and thereafter to 4 mg and 8 mg once daily, the maximum recommended dose for BPH. The recommended titration interval is 1 to 2 weeks. Blood pressure should be evaluated routinely in these patients.
The initial dosage of doxazosin is 1 mg given once daily. Depending on the individual patient's standing blood pressure response (based on measurements taken at 2 to 6 hours post-dose and 24 hours post-dose), dosage may then be increased to 2 mg and thereafter if necessary to 4 mg, 8 mg and 16 mg to achieve the desired reduction in blood pressure. Increases in dose beyond 4 mg increase the likelihood of excessive postural effects including syncope, postural dizziness/vertigo and postural hypotension. At a titrated dose of 16 mg once daily the frequency of postural effects is about 12% compared to 3% for placebo.
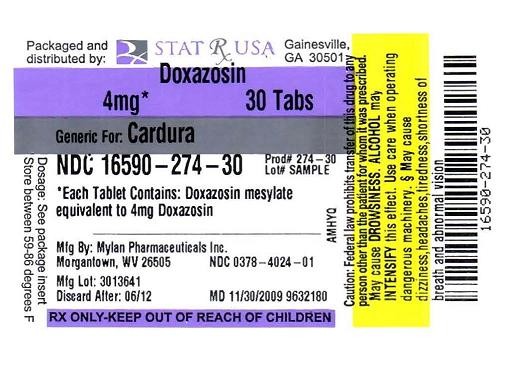
Doxazosin Tablets, USP are available as tablets for oral administration. Each tablet contains doxazosin mesylate equivalent to 1 mg, 2 mg, 4 mg or 8 mg of doxazosin.
The 1 mg are available as white to off-white, round, biconvex tablets debossed with M over D9 on one side of the tablet and scored on the other side. They are available as follows:
NDC 0378-4021-01
bottles of 100 tablets
The 2 mg are available as pink, round, biconvex tablets debossed with M over D10 on one side of the tablet and scored on the other side. They are available as follows:
NDC 0378-4022-01
bottles of 100 tablets
NDC 0378-4022-05
bottles of 500 tablets
The 4 mg are available as blue, round, biconvex tablets debossed with M over D11 on one side of the tablet and scored on the other side. They are available as follows:
NDC 0378-4024-01
bottles of 100 tablets
NDC 0378-4024-05
bottles of 500 tablets
The 8 mg are available as purple, round, biconvex tablets debossed with M over D12 on one side of the tablet and scored on the other side. They are available as follows:
NDC 0378-4028-01
bottles of 100 tablets
Store at 20° to 25°C (68° to 77°F). [See USP for Controlled Room Temperature.]
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
PHARMACIST: Detach Patient Information Leaflet at each perforation and give leaflet to patient.
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505
REVISED AUGUST 2007
DXZN:R6p
(See Patient Leaflet)
Patients should be made aware of the possibility of syncopal and orthostatic symptoms, especially at the initiation of therapy, and urged to avoid driving or hazardous tasks for 24 hours after the first dose, after a dosage increase, and after interruption of therapy when treatment is resumed. They should be cautioned to avoid situations where injury could result should syncope occur during initiation of doxazosin therapy. They should also be advised of the need to sit or lie down when symptoms of lowered blood pressure occur, although these symptoms are not always orthostatic, and to be careful when rising from a sitting or lying position. If dizziness, lightheadedness, or palpitations are bothersome they should be reported to the physician, so that dose adjustment can be considered. Patients should also be told that drowsiness or somnolence can occur with doxazosin or any selective alpha1 adrenoceptor antagonist, requiring caution in people who must drive or operate heavy machinery.
Patients should be advised about the possibility of priapism as a result of treatment with alpha1 antagonists. Patients should know that this adverse event is very rare. If they experience priapism, it should be brought to immediate medical attention for if not treated promptly it can lead to permanent erectile dysfunction (impotence).
Doxazosin does not affect the plasma concentration of prostate specific antigen in patients treated for up to 3 years. Both doxazosin, an alpha1 inhibitor, and finasteride, a 5-alpha reductase inhibitor, are highly protein bound and hepatically metabolized. There is no definitive controlled clinical experience on the concomitant use of alpha1 inhibitors and 5-alpha reductase inhibitors at this time.
Doxazosin should be administered with caution to patients with evidence of impaired hepatic function or to patients receiving drugs known to influence hepatic metabolism (see CLINICAL PHARMACOLOGY).
Analysis of hematologic data from hypertensive patients receiving doxazosin in controlled hypertension clinical trials showed that the mean WBC (N = 474) and mean neutrophil counts (N = 419) were decreased by 2.4% and 1%, respectively, compared to placebo, a phenomenon seen with other alpha blocking drugs. In BPH patients the incidence of clinically significant WBC abnormalities was 0.4% (2/459) with doxazosin and 0% (0/147) with placebo, with no statistically significant difference between the two treatment groups. A search through a data base of 2,400 hypertensive patients and 665 BPH patients revealed 4 hypertensives in which drug-related neutropenia could not be ruled out and one BPH patient in which drug-related leukopenia could not be ruled out. Two hypertensives had a single low value on the last day of treatment. Two hypertensives had stable, non-progressive neutrophil counts in the 1000/mm3 range over periods of 20 and 40 weeks. One BPH patient had a decrease from WBC count of 4800/mm3 to 2700/mm3 at the end of the study; there was no evidence of clinical impairment. In cases where follow-up was available the WBCs and neutrophil counts returned to normal after discontinuation of doxazosin. No patients became symptomatic as a result of the low WBC or neutrophil counts.
Most (98%) of plasma doxazosin is protein bound. In vitro data in human plasma indicate that doxazosin has no effect on protein binding of digoxin, warfarin, phenytoin or indomethacin. There is no information on the effect of other highly plasma protein bound drugs on doxazosin binding. Doxazosin has been administered without any evidence of an adverse drug interaction to patients receiving thiazide diuretics, beta-blocking agents, and nonsteroidal anti-inflammatory drugs. In a placebo-controlled trial in normal volunteers, the administration of a single 1 mg dose of doxazosin on day 1 of a 4-day regimen of oral cimetidine (400 mg twice daily) resulted in a 10% increase in mean AUC of doxazosin (p = 0.006), and a slight but not statistically significant increase in mean Cmax and mean half-life of doxazosin. The clinical significance of this increase in doxazosin AUC is unknown.
In clinical trials, doxazosin tablets have been administered to patients on a variety of concomitant medications; while no formal interaction studies have been conducted, no interactions were observed. Doxazosin tablets have been used with the following drugs or drug classes: 1) analgesic/anti-inflammatory (e.g., acetaminophen, aspirin, codeine and codeine combinations, ibuprofen, indomethacin); 2) antibiotics (e.g., erythromycin, trimethoprim and sulfamethoxazole, amoxicillin); 3) antihistamines (e.g., chlorpheniramine); 4) cardiovascular agents (e.g., atenolol, hydrochlorothiazide, propranolol); 5) corticosteroids; 6) gastrointestinal agents (e.g., antacids); 7) hypoglycemics and endocrine drugs; 8) sedatives and tranquilizers (e.g., diazepam); 9) cold and flu remedies.
An increased incidence of myocardial necrosis or fibrosis was displayed by Sprague-Dawley rats after 6 months of dietary administration at concentrations calculated to provide 80 mg doxazosin/kg/day and after 12 months of dietary administration at concentrations calculated to provide 40 mg doxazosin/kg/day (AUC exposure in rats 8 times the human AUC exposure with a 12 mg/day therapeutic dose). Myocardial fibrosis was observed in both rats and mice treated in the same manner with 40 mg doxazosin/kg/day for 18 months (exposure 8 times human AUC exposure in rats and somewhat equivalent to human Cmax exposure in mice). No cardiotoxicity was observed at lower doses (up to 10 or 20 mg/kg/day, depending on the study) in either species. These lesions were not observed after 12 months of oral dosing in dogs at maximum doses of 20 mg/kg/day [maximum plasma concentrations (Cmax) in dogs 14 times the Cmax exposure in humans receiving a 12 mg/day therapeutic dose] and in Wistar rats at doses of 100 mg/kg/day (Cmax exposures 15 times human Cmax exposure with a 12 mg/day therapeutic dose). There is no evidence that similar lesions occur in humans.
Chronic dietary administration (up to 24 months) of doxazosin mesylate at maximally tolerated doses of 40 mg/kg/day in rats and 120 mg/kg/day in mice revealed no evidence of carcinogenic potential. The highest doses evaluated in the rat and mouse studies are associated with AUCs (a measure of systemic exposure) that are 8 times and 4 times, respectively, the human AUC at a dose of 16 mg/day.
Mutagenicity studies revealed no drug- or metabolite-related effects at either chromosomal or subchromosomal levels.
Studies in rats showed reduced fertility in males treated with doxazosin at oral doses of 20 (but not 5 or 10) mg/kg/day, about 4 times the AUC exposures obtained with a 12 mg/day human dose. This effect was reversible within two weeks of drug withdrawal. There have been no reports of any effects of doxazosin on male fertility in humans.
Studies in pregnant rabbits and rats at daily oral doses of up to 41 and 20 mg/kg, respectively (plasma drug concentrations 10 and 4 times human Cmax and AUC exposures with a 12 mg/day therapeutic dose), have revealed no evidence of harm to the fetus. A dosage regimen of 82 mg/kg/day in the rabbit was associated with reduced fetal survival. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, doxazosin should be used during pregnancy only if clearly needed.
Radioactivity was found to cross the placenta following oral administration of labeled doxazosin to pregnant rats.
In peri-postnatal studies in rats, postnatal development at maternal doses of 40 or 50 mg/kg/day of doxazosin (8 times human AUC exposure with a 12 mg/day therapeutic dose) was delayed as evidenced by slower body weight gain and a slightly later appearance of anatomical features and reflexes.
Studies in lactating rats given a single oral dose of 1 mg/kg of [2-14C]-doxazosin indicate that doxazosin accumulates in rat breast milk with a maximum concentration about 20 times greater than the maternal plasma concentration. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when doxazosin is administered to a nursing mother.
The safety and effectiveness of doxazosin as an antihypertensive agent have not been established in pediatric patients.
The safety and effectiveness profile of doxazosin in BPH was similar in the elderly (age ≥ 65 years) and younger (age less 65 years) patients.
Clinical studies of doxazosin did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
doxazosin4mg
DoxazosinDoxazosin TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||