Crestor
Lake Erie Medical DBA Quality Care Products LLC
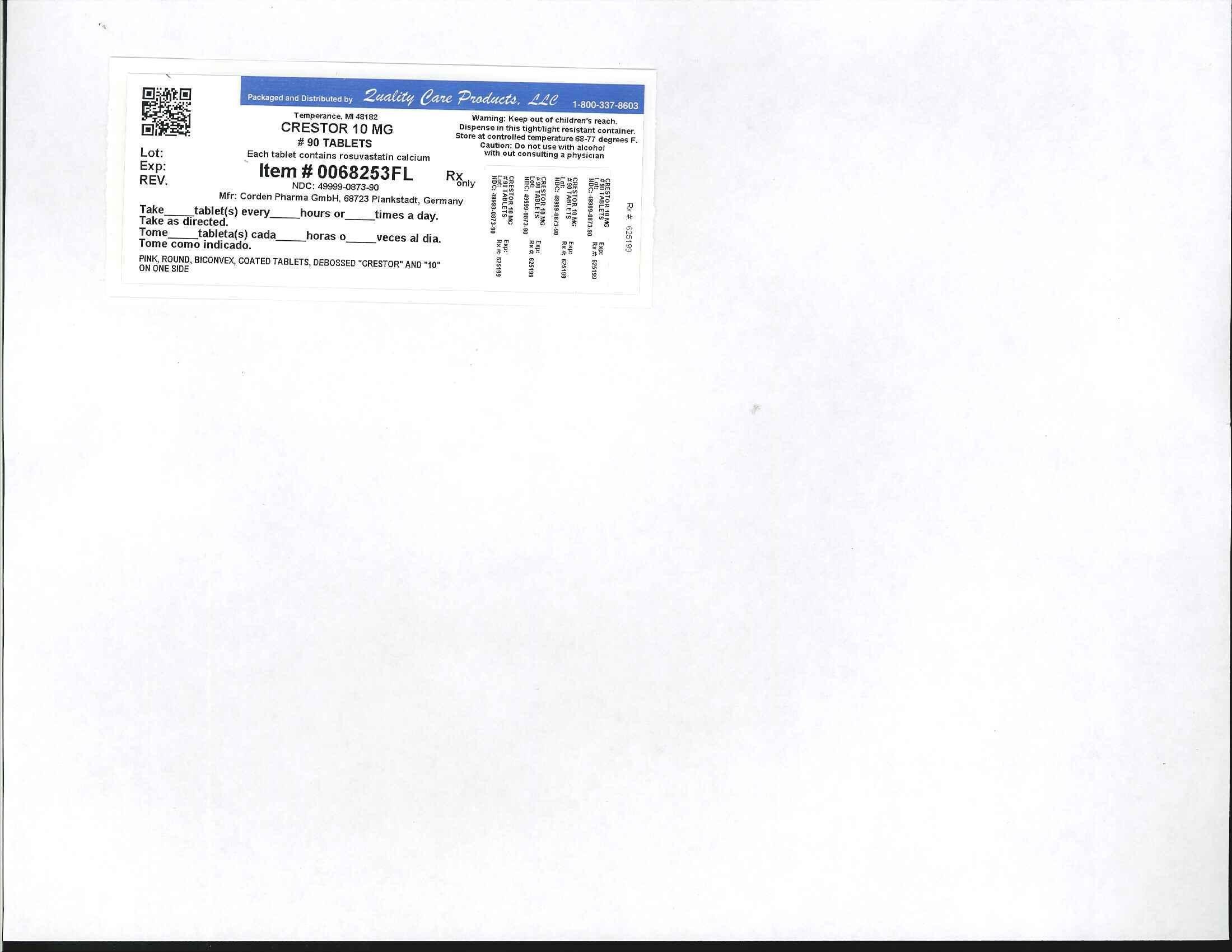
Crestor 10 MG
FULL PRESCRIBING INFORMATION
2227362
Inactive Ingredients: Each tablet contains: microcrystalline cellulose NF, lactose monohydrate NF, tribasic calcium phosphate NF, crospovidone NF, magnesium stearate NF, hypromellose NF, triacetin NF, titanium dioxide USP, yellow ferric oxide, and red ferric oxide NF.
CRESTOR is a selective and competitive inhibitor of HMG-CoA reductase, the rate-limiting enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A to mevalonate, a precursor of cholesterol. In vivo studies in animals, and in vitro studies in cultured animal and human cells have shown rosuvastatin to have a high uptake into, and selectivity for, action in the liver, the target organ for cholesterol lowering. In in vivo and in vitro studies, rosuvastatin produces its lipid-modifying effects in two ways. First, it increases the number of hepatic LDL receptors on the cell-surface to enhance uptake and catabolism of LDL. Second, rosuvastatin inhibits hepatic synthesis of VLDL, which reduces the total number of VLDL and LDL particles.
-
Absorption: In clinical pharmacology studies in man, peak plasma concentrations of rosuvastatin were reached 3 to 5 hours following oral dosing. Both Cmax and AUC increased in approximate proportion to CRESTOR dose. The absolute bioavailability of rosuvastatin is approximately 20%.
Administration of CRESTOR with food did not affect the AUC of rosuvastatin.
The AUC of rosuvastatin does not differ following evening or morning drug administration.
-
Distribution: Mean volume of distribution at steady-state of rosuvastatin is approximately 134 liters. Rosuvastatin is 88% bound to plasma proteins, mostly albumin. This binding is reversible and independent of plasma concentrations.
-
Metabolism: Rosuvastatin is not extensively metabolized; approximately 10% of a radiolabeled dose is recovered as metabolite. The major metabolite is N-desmethyl rosuvastatin, which is formed principally by cytochrome P450 2C9, and in vitro studies have demonstrated that N-desmethyl rosuvastatin has approximately one-sixth to one-half the HMG-CoA reductase inhibitory activity of the parent compound. Overall, greater than 90% of active plasma HMG-CoA reductase inhibitory activity is accounted for by the parent compound.
-
Excretion: Following oral administration, rosuvastatin and its metabolites are primarily excreted in the feces (90%). The elimination half-life (t1/2) of rosuvastatin is approximately 19 hours.
After an intravenous dose, approximately 28% of total body clearance was via the renal route, and 72% by the hepatic route.
-
Race: A population pharmacokinetic analysis revealed no clinically relevant differences in pharmacokinetics among Caucasian, Hispanic, and Black or Afro-Caribbean groups. However, pharmacokinetic studies, including one conducted in the US, have demonstrated an approximate 2-fold elevation in median exposure (AUC and Cmax) in Asian subjects when compared with a Caucasian control group.
-
Gender: There were no differences in plasma concentrations of rosuvastatin between men and women.
-
Geriatric: There were no differences in plasma concentrations of rosuvastatin between the nonelderly and elderly populations (age ≥65 years).
-
Renal Impairment: Mild to moderate renal impairment (CLcr greater than or equal to 30 mL/min/1.73 m2) had no influence on plasma concentrations of rosuvastatin. However, plasma concentrations of rosuvastatin increased to a clinically significant extent (about 3-fold) in patients with severe renal impairment (CLcr less than 30 mL/min/1.73 m2) not receiving hemodialysis compared with healthy subjects (CLcr greater than 80 mL/min/1.73 m2).
-
Hemodialysis: Steady-state plasma concentrations of rosuvastatin in patients on chronic hemodialysis were approximately 50% greater compared with healthy volunteer subjects with normal renal function.
-
Hepatic Impairment: In patients with chronic alcohol liver disease, plasma concentrations of rosuvastatin were modestly increased.
In patients with Child-Pugh A disease, Cmax and AUC were increased by 60% and 5%, respectively, as compared with patients with normal liver function. In patients with Child-Pugh B disease, Cmax and AUC were increased 100% and 21%, respectively, compared with patients with normal liver function.
Uses
CRESTOR is indicated as adjunctive therapy to diet to reduce elevated Total-C, LDL-C, ApoB, nonHDL-C, and triglycerides and to increase HDL-C in adult patients with primary hyperlipidemia or mixed dyslipidemia. Lipid-altering agents should be used in addition to a diet restricted in saturated fat and cholesterol when response to diet and nonpharmacological interventions alone has been inadequate.
Pediatric Patients 10 to 17 years of age with Heterozygous Familial Hypercholesterolemia (HeFH)
Adjunct to diet to reduce Total-C, LDL-C and ApoB levels in adolescent boys and girls, who are at least one year post-menarche, 10-17 years of age with heterozygous familial hypercholesterolemia if after an adequate trial of diet therapy the following findings are present: LDL-C > 190 mg/dL or > 160 mg/dL and there is a positive family history of premature cardiovascular disease (CVD) or two or more other CVD risk factors.CRESTOR is indicated as adjunctive therapy to diet for the treatment of adult patients with hypertriglyceridemia.
CRESTOR is indicated as an adjunct to diet for the treatment of patients with primary dysbetalipoproteinemia (Type III Hyperlipoproteinemia).
CRESTOR is indicated as adjunctive therapy to other lipid-lowering treatments (e.g., LDL apheresis) or alone if such treatments are unavailable to reduce LDL-C, Total-C, and ApoB in adult patients with homozygous familial hypercholesterolemia.
CRESTOR is indicated as adjunctive therapy to diet to slow the progression of atherosclerosis in adult patients as part of a treatment strategy to lower Total-C and LDL-C to target levels.
In individuals without clinically evident coronary heart disease but with an increased risk of cardiovascular disease based on age ≥ 50 years old in men and ≥ 60 years old in women, hsCRP ≥ 2 mg/L, and the presence of at least one additional cardiovascular disease risk factor such as hypertension, low HDL-C, smoking, or a family history of premature coronary heart disease, CRESTOR is indicated to:
-
reduce the risk of stroke
-
reduce the risk of myocardial infarction
-
reduce the risk of arterial revascularization procedures
CRESTOR has not been studied in Fredrickson Type I and V dyslipidemias.
CRESTOR is contraindicated in the following conditions:
-
Patients with a known hypersensitivity to any component of this product. Hypersensitivity reactions including rash, pruritus, urticaria and angioedema have been reported with CRESTOR [see Adverse Reactions (6.1)].
-
Patients with active liver disease, which may include unexplained persistent elevations of hepatic transaminase levels [see Warnings and Precautions (5.2)].
-
Women who are pregnant or may become pregnant. Because HMG-CoA reductase inhibitors decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, CRESTOR may cause fetal harm when administered to pregnant women. Additionally, there is no apparent benefit to therapy during pregnancy, and safety in pregnant women has not been established. If the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus and the lack of known clinical benefit with continued use during pregnancy [see Use in Specific Populations (8.1) and Nonclinical Toxicology (13.2)].
-
Nursing mothers. Because another drug in this class passes into breast milk, and because HMG-CoA reductase inhibitors have the potential to cause serious adverse reactions in nursing infants, women who require CRESTOR treatment should be advised not to nurse their infants [see Use in Specific Populations (8.3)].
The following serious adverse reactions are discussed in greater detail in other sections of the label:
-
Rhabdomyolysis with myoglobinuria and acute renal failure and myopathy (including myositis). [see Warnings and Precautions (5.1)]
-
Liver enzyme abnormalities [see Warnings and Precautions (5.2)]
In the CRESTOR controlled clinical trials database (placebo or active-controlled) of 5394 patients with a mean treatment duration of 15 weeks, 1.4% of patients discontinued due to adverse reactions. The most common adverse reactions that led to treatment discontinuation were:
-
myalgia
-
abdominal pain
-
nausea
The most commonly reported adverse reactions (incidence ≥ 2%) in the CRESTOR controlled clinical trial database of 5394 patients were:
-
headache
-
myalgia
-
abdominal pain
-
asthenia
-
nausea
see Warnings and Precautions
In the METEOR study, involving 981 participants treated with rosuvastatin 40 mg (n=700) or placebo (n=281) with a mean treatment duration of 1.7 years, 5.6% of subjects treated with CRESTOR versus 2.8% of placebo-treated subjects discontinued due to adverse reactions. The most common adverse reactions that led to treatment discontinuation were: myalgia, hepatic enzyme increased, headache, and nausea [see Clinical Studies (14.7)].
Adverse reactions reported in ≥ 2% of patients and at a rate greater than placebo are shown in Table 2.
In the JUPITER study, 17,802 participants were treated with rosuvastatin 20 mg (n=8901) or placebo (n=8901) for a mean duration of 2 years. A higher percentage of rosuvastatin-treated patients versus placebo-treated patients, 6.6% and 6.2%, respectively, discontinued study medication due to an adverse event, irrespective of treatment causality. Myalgia was the most common adverse reaction that led to treatment discontinuation.
In JUPITER, there was a significantly higher frequency of diabetes mellitus
reported in patients taking rosuvastatin (2.8%) versus patients taking placebo
(2.3%). Mean HbA1c was significantly increased by 0.1% in rosuvastatin-treated
patients compared to placebo-treated patients. The number of patients with a
HbA1c > 6.5% at the end of the trial was significantly higher in
rosuvastatin-treated versus placebo-treated patients [see
Warnings and Precautions (5.5) and Clinical
Studies (14.8)].
Adverse reactions reported in ≥ 2% of patients and at a rate greater than placebo are shown in Table 3.
In a 12-week controlled study in boys and postmenarchal girls,
the safety and tolerability profile of CRESTOR 5 to 20 mg daily was generally
similar to that of placebo [see Clinical Studies
(14.6) and Use in Special Populations, Pediatric
Use (8.4)].
However, elevations in serum creatine phosphokinase (CK) > 10 x ULN were observed more frequently in rosuvastatin compared with placebo-treated children. Four of 130 (3%) children treated with rosuvastatin (2 treated with 10 mg and 2 treated with 20 mg) had increased CK >10 x ULN, compared to 0 of 46 children on placebo.
The following adverse reactions have been identified during postapproval use of CRESTOR: arthralgia, hepatic failure, hepatitis, jaundice and memory loss. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There is no specific treatment in the event of overdose. In the event of overdose, the patient should be treated symptomatically and supportive measures instituted as required. Hemodialysis does not significantly enhance clearance of rosuvastatin.
Enter section text here
CRESTOR® (rosuvastatin calcium) Tablets are supplied as:
-
NDC 0310-0755-90: 5 mg. Yellow, round, biconvex, coated tablets. Debossed “CRESTOR” and “5” on one side; bottle of 90 tablets
-
NDC 0310-0751-90: 10 mg. Pink, round, biconvex, coated tablets. Debossed “CRESTOR” and “10” on one side; bottle of 90 tablets
-
NDC 0310-0751-39: 10 mg. Pink, round, biconvex, coated tablets. Debossed “CRESTOR” and “10” on one side; unit dose packages of 100
-
NDC 0310-0752-90: 20 mg. Pink, round, biconvex, coated tablets. Debossed “CRESTOR” and “20” on one side; bottles of 90
-
NDC 0310-0752-39: 20 mg. Pink, round, biconvex, coated tablets. Debossed “CRESTOR” and “20”on one side; unit dose packages of 100
-
NDC 0310-0754-30: 40 mg. Pink, oval, biconvex, coated tablets. Debossed “CRESTOR” on one side and “40” on the other side; bottles of 30
Patients should be advised to report promptly unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever.
When taking CRESTOR with an aluminum and magnesium hydroxide combination antacid, the antacid should be taken at least 2 hours after CRESTOR administration.
If the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus and the lack of known clinical benefit with continued use during pregnancy.
It is recommended that liver enzymes be checked before and at 12 weeks following both the initiation of therapy and any elevation of dose, and periodically (e.g., semiannually) thereafter.
CrestorRosuvastatin calcium TABLET, COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||