Clonidine
Lake Erie Medical DBA Quality Care Products LLC
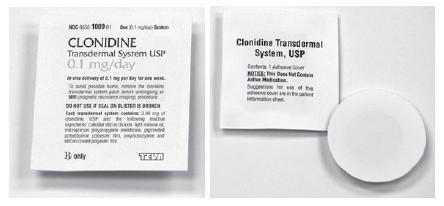
CLONIDINE Transdermal System USPProgrammed delivery in vivo of 0.1, 0.2, or 0.3 mg clonidine USP per day, for one week.
FULL PRESCRIBING INFORMATION: CONTENTS*
- CLONIDINE DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLONIDINE INDICATIONS AND USAGE
- CLONIDINE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- CLONIDINE ADVERSE REACTIONS
- OVERDOSAGE
- CLONIDINE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- STORAGE AND HANDLING
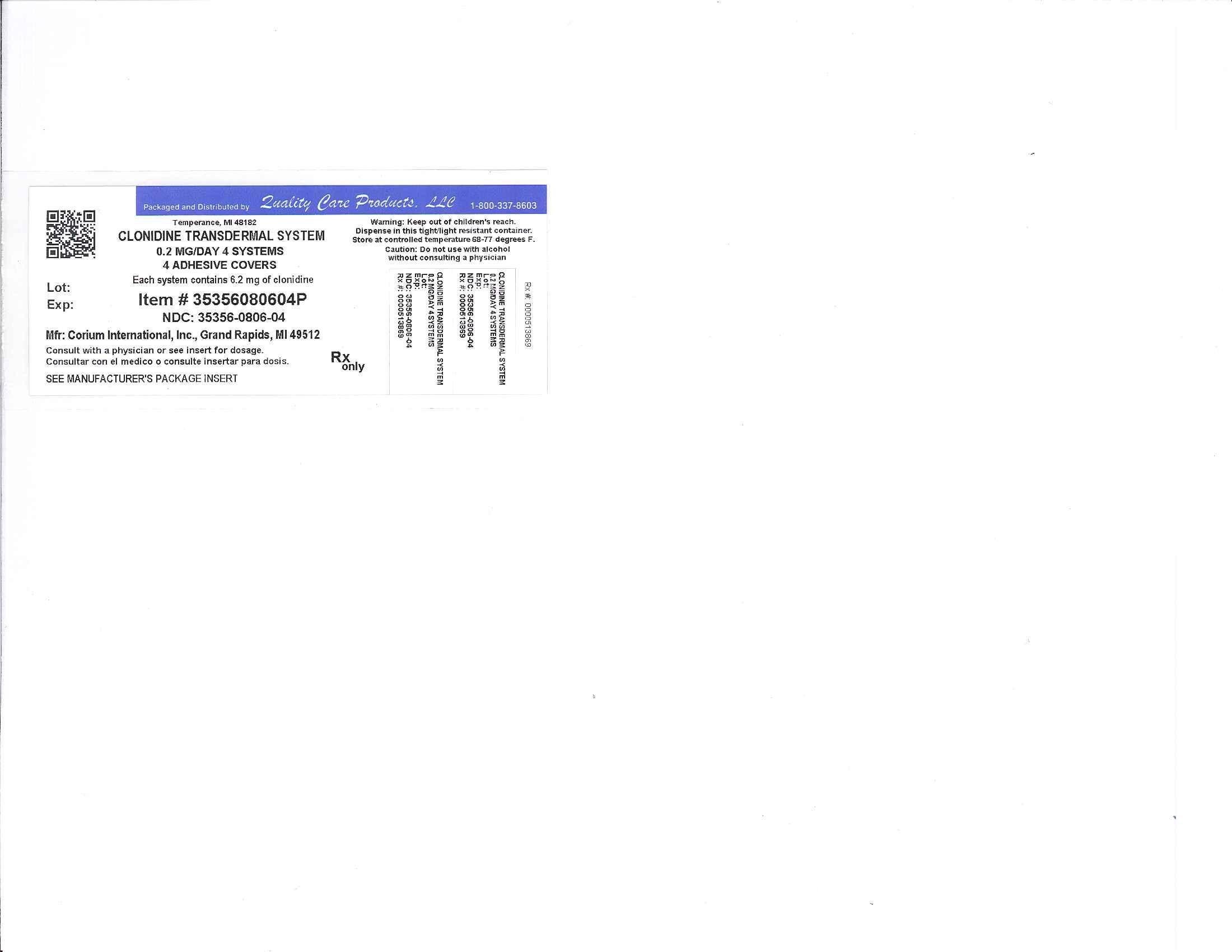
- Image of Label
FULL PRESCRIBING INFORMATION
CLONIDINE DESCRIPTION
Clonidine transdermal system USP provides continuous systemic delivery of clonidine USP for 7 days at an approximately constant rate. Clonidine USP is a centrally acting alpha-agonist hypotensive agent. It is an imidazoline derivative with the chemical name 2, 6-dichloro-N-2-imidazolidinylidenebenzenamine and has the following chemical structure:
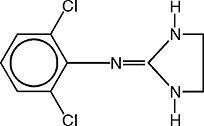
C9H9Cl2N3 M.W. 230.10
System Structure and Components
Clonidine transdermal system USP is a multi-layered film, 0.2 mm thick, containing clonidine USP as the active agent. The system areas are 4.33 cm2 (clonidine USP 0.1 mg per day), 8.67 cm2 (clonidine USP 0.2 mg per day) and 13 cm2 (clonidine USP 0.3 mg per day) and the amount of drug released is directly proportional to the area (see Release Rate Concept). The composition per unit area is the same for all three doses. The inactive ingredients are: colloidal silicon dioxide, light mineral oil, microporous polypropylene membrane, pigmented polyethylene polyester film, polyisobutylene and silicon coated polyester film.
Proceeding from the visible surface towards the surface attached to the skin, there are four consecutive layers: 1) a backing layer of polyester film; 2) a drug reservoir; 3) a microporous polypropylene membrane that controls the rate of delivery of clonidine USP from the system to the skin surface; 4) an adhesive formulation. Prior to use, a protective slit release liner of silicone coated polyester film that covers the adhesive layer is removed.
Cross Section of the System:

Release Rate Concept
Clonidine transdermal system USP is programmed to release clonidine USP at an approximately constant rate for 7 days. The energy for drug release is derived from the concentration gradient existing between a saturated solution of drug in the system and the much lower concentration prevailing in the skin. Clonidine USP flows in the direction of the lower concentration at a constant rate, limited by the rate-controlling membrane, so long as a saturated solution is maintained in the drug reservoir.
Following system application to intact skin, clonidine USP in the adhesive layer saturates the skin site below the system. Clonidine USP from the drug reservoir then begins to flow through the rate-controlling membrane and the adhesive layer of the system into the systemic circulation via the capillaries beneath the skin. Therapeutic plasma clonidine USP levels are achieved 2 to 3 days after initial application of clonidine transdermal system USP.
The 4.33, 8.67 and 13 cm2 systems deliver 0.1, 0.2, and 0.3 mg of clonidine USP per day, respectively. To ensure constant release of drug for 7 days, the total drug content of the system is higher than the total amount of drug delivered. Application of a new system to a fresh skin site at weekly intervals continuously maintains therapeutic plasma concentrations of clonidine USP. If the clonidine transdermal system USP is removed and not replaced with a new system, therapeutic plasma clonidine USP levels will persist for about 8 hours and then decline slowly over several days. Over this time period, blood pressure returns gradually to pretreatment levels.
CLINICAL PHARMACOLOGY
Clonidine stimulates alpha-adrenoreceptors in the brain stem. This action results in reduced sympathetic outflow from the central nervous system and in decreases in peripheral resistance, renal vascular resistance, heart rate, and blood pressure. Renal blood flow and glomerular filtration rate remain essentially unchanged. Normal postural reflexes are intact; therefore, orthostatic symptoms are mild and infrequent.
Acute studies with clonidine hydrochloride in humans have demonstrated a moderate reduction (15% to 20%) of cardiac output in the supine position with no change in the peripheral resistance; at a 45° tilt there is a smaller reduction in cardiac output and a decrease of peripheral resistance.
During long-term therapy, cardiac output tends to return to control values, while peripheral resistance remains decreased. Slowing of the pulse rate has been observed in most patients given clonidine, but the drug does not alter normal hemodynamic responses to exercise.
Tolerance to the antihypertensive effect may develop in some patients, necessitating a reevaluation of therapy.
Other studies in patients have provided evidence of a reduction in plasma renin activity and in the excretion of aldosterone and catecholamines. The exact relationship of these pharmacologic actions to the antihypertensive effect of clonidine has not been fully elucidated.
Clonidine acutely stimulates the release of growth hormone in children as well as adults but does not produce a chronic elevation of growth hormone with long-term use.
Pharmacokinetics
Clonidine transdermal system delivers clonidine at an approximately constant rate for 7 days. The absolute bioavailability of clonidine from the clonidine transdermal system dosage form is approximately 60%. Steady-state clonidine plasma levels are obtained within 3 days after transdermal application to the upper outer arm and increase linearly with increasing size of the transdermal patch. Mean steady-state plasma concentrations with the 4.33 cm2, 8.67 cm2 and 13 cm2 systems are approximately 0.4 ng/mL, 0.8 ng/mL, and 1.1 ng/mL, respectively. Similar clonidine steady-state concentrations are reached after application to the chest. Steady-state clonidine plasma levels remain constant after removal of one system and application of a new system of the same size.
Following intravenous administration, clonidine displays biphasic disposition with a distribution half-life of about 20 minutes and an elimination half-life ranging from 12 to 16 hours. The half-life increases up to 41 hours in patients with severe impairment of renal function. Clonidine has a total clearance of 177 mL/min and a renal clearance of 102 mL/min. The apparent volume of distribution (Vz) of clonidine is 197 L (2.9 L/kg). Clonidine crosses the placental barrier. It has been shown to cross the blood brain barrier in rats.
Following oral administration, about 40% to 60% of the absorbed dose is recovered in the urine as unchanged drug within 24 hours. About 50% of the absorbed dose is metabolized in the liver.
After removal of the clonidine transdermal system, clonidine plasma concentrations decline slowly with a half-life of approximately 20 hours.
CLONIDINE INDICATIONS AND USAGE
Clonidine transdermal system is indicated in the treatment of hypertension. It may be employed alone or concomitantly with other antihypertensive agents.
CLONIDINE CONTRAINDICATIONS
Clonidine transdermal system should not be used in patients with known hypersensitivity to clonidine or to any other component of the therapeutic system.
WARNINGS
Withdrawal
Patients should be instructed not to discontinue therapy without consulting their physician. Sudden cessation of clonidine treatment has, in some cases, resulted in symptoms such as nervousness, agitation, headache, tremor, and confusion accompanied or followed by a rapid rise in blood pressure and elevated catecholamine concentrations in the plasma. The likelihood of such reactions to discontinuation of clonidine therapy appears to be greater after administration of higher doses or continuation of concomitant beta-blocker treatment and special caution is therefore advised in these situations. Rare instances of hypertensive encephalopathy, cerebrovascular accidents and death have been reported after clonidine withdrawal. When discontinuing therapy with clonidine transdermal system, the physician should reduce the dose gradually over 2 to 4 days to avoid withdrawal symptomatology.
An excessive rise in blood pressure following discontinuation of clonidine transdermal system therapy can be reversed by administration of oral clonidine hydrochloride or by intravenous phentolamine. If therapy is to be discontinued in patients receiving a beta-blocker and clonidine concurrently, the beta-blocker should be withdrawn several days before the gradual discontinuation of clonidine transdermal system.
PRECAUTIONS
General
In patients who have developed localized contact sensitization to clonidine transdermal system, continuation of clonidine transdermal system or substitution of oral clonidine hydrochloride therapy may be associated with development of a generalized skin rash.
In patients who develop an allergic reaction to clonidine transdermal system, substitution of oral clonidine hydrochloride may also elicit an allergic reaction (including generalized rash, urticaria, or angioedema).
The sympatholytic action of clonidine may worsen sinus node dysfunction and atrioventricular (AV) block, especially in patients taking other sympatholytic drugs. There are postmarketing reports of patients with conduction abnormalities and/or taking other sympatholytic drugs who developed severe bradycardia requiring IV atropine, IV isoproterenol and temporary cardiac pacing while taking clonidine.
In hypertension caused by pheochromocytoma, no therapeutic effect of clonidine transdermal system can be expected.
In rare instances, loss of blood pressure control has been reported in patients using clonidine transdermal system according to the instructions for use.
Perioperative Use
Clonidine transdermal system therapy should not be interrupted during the surgical period. Blood pressure should be carefully monitored during surgery and additional measures to control blood pressure should be available if required. Physicians considering starting clonidine transdermal system therapy during the perioperative period must be aware that therapeutic plasma clonidine levels are not achieved until 2 to 3 days after initial application of clonidine transdermal system (see DOSAGE AND ADMINISTRATION).
Defibrillation or Cardioversion
The transdermal clonidine systems should be removed before attempting defibrillation or cardioversion because of the potential for altered electrical conductivity, which may increase the risk of arcing, a phenomenon associated with the use of defibrillators.
MRI
Skin burns have been reported at the patch site in several patients wearing an aluminized transdermal system during a magnetic resonance imaging scan (MRI). Because the clonidine transdermal system patch contains aluminum, it is recommended to remove the system before undergoing an MRI.
Information for Patients
Patients should be cautioned against interruption of clonidine transdermal system therapy without their physician’s advice.
Since patients may experience a possible sedative effect, dizziness, or accommodation disorder with use of clonidine, caution patients about engaging in activities such as driving a vehicle or operating appliances or machinery. Also, inform patients that this sedative effect may be increased by concomitant use of alcohol, barbiturates, or other sedating drugs.
Patients who wear contact lenses should be cautioned that treatment with clonidine transdermal system may cause dryness of eyes.
Patients should be instructed to consult their physicians promptly about the possible need to remove the patch if they observe moderate to severe localized erythema and/or vesicle formation at the site of application or generalized skin rash.
If a patient experiences isolated, mild localized skin irritation before completing 7 days of use, the system may be removed and replaced with a new system applied to a fresh skin site.
If the system should begin to loosen from the skin after application, the patient should be instructed to place the adhesive cover directly over the system to ensure adhesion during its
7 day use.
Used clonidine transdermal system patches contain a substantial amount of their initial drug content which may be harmful to infants and children if accidentally applied or ingested. THEREFORE, PATIENTS SHOULD BE CAUTIONED TO KEEP BOTH USED AND UNUSED CLONIDINE TRANSDERMAL SYSTEM PATCHES OUT OF THE REACH OF CHILDREN. After use, clonidine transdermal system should be folded in half with the adhesive sides together and discarded away from children’s reach.
Instructions for use, storage and disposal of the system are provided at the end of this brochure. These instructions are also included in each box of clonidine transdermal system.
Drug Interactions
Clonidine may potentiate the CNS-depressive effects of alcohol, barbiturates or other sedating drugs. If a patient receiving clonidine is also taking tricyclic antidepressants, the hypotensive effect of clonidine may be reduced, necessitating an increase in the clonidine dose. If a patient receiving clonidine is also taking neuroleptics, orthostatic regulation disturbances (e.g., orthostatic hypotension, dizziness, fatigue) may be induced or exacerbated.
Monitor heart rate in patients receiving clonidine concomitantly with agents known to affect sinus node function or AV nodal conduction, e.g., digitalis, calcium channel blockers, and beta-blockers. Sinus bradycardia resulting in hospitalization and pacemaker insertion has been reported in association with the use of clonidine concomitantly with diltiazem or verapamil.
Amitriptyline in combination with clonidine enhances the manifestation of corneal lesions in rats (see Toxicology).
Toxicology
In several studies with oral clonidine hydrochloride, a dose-dependent increase in the incidence and severity of spontaneous retinal degeneration was seen in albino rats treated for six months or longer. Tissue distribution studies in dogs and monkeys showed a concentration of clonidine in the choroid.
In view of the retinal degeneration seen in rats, eye examinations were performed during clinical trials in 908 patients before, and periodically after, the start of clonidine therapy. In 353 of these 908 patients, the eye examinations were carried out over periods of 24 months or longer. Except for some dryness of the eyes, no drug-related abnormal ophthalmological findings were recorded and, according to specialized tests such as electroretinography and macular dazzle, retinal function was unchanged.
In combination with amitriptyline, clonidine hydrochloride administration led to the development of corneal lesions in rats within 5 days.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Chronic dietary administration of clonidine was not carcinogenic to rats (132 weeks) or mice (78 weeks) dosed, respectively, at up to 46 to 70 times the maximum recommended daily human dose as mg/kg (9 or 6 times the MRDHD on a mg/m2 basis). There was no evidence of genotoxicity in the Ames test for mutagenicity or mouse micronucleus test for clastogenicity.
Fertility of male and female rats was unaffected by clonidine doses as high as 150 mcg/kg (approximately 3 times the MRDHD). In a separate experiment, fertility of female rats appeared to be affected at dose levels of 500 to 2000 mcg/kg (10 to 40 times the oral MRDHD on a mg/kg basis; 2 to 8 times the MRDHD on a mg/m2 basis).
Pregnancy
Teratogenic Effects
Reproduction studies performed in rabbits at doses up to approximately 3 times the oral maximum recommended daily human dose (MRDHD) of clonidine hydrochloride produced no evidence of a teratogenic or embryotoxic potential in rabbits. In rats, however, doses as low as 1/3 the oral MRDHD (1/15 the MRDHD on a mg/m2 basis) of clonidine were associated with increased resorptions in a study in which dams were treated continuously from 2 months prior to mating. Increased resorptions were not associated with treatment at the same or at higher dose levels (up to 3 times the oral MRDHD) when the dams were treated on gestation days 6 to 15. Increases in resorption were observed at much higher dose levels (40 times the oral MRDHD on a mg/kg basis; 4 to 8 times the MRDHD on a mg/m2 basis) in mice and rats treated on gestation days 1 to 14 (lowest dose employed in the study was 500 mcg/kg).
No adequate well-controlled studies have been conducted in pregnant women. Clonidine crosses the placental barrier (see CLINICAL PHARMACOLOGY, Pharmacokinetics). Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
As clonidine is excreted in human milk, caution should be exercised when clonidine transdermal system is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established in adequate and well-controlled trials.
CLONIDINE ADVERSE REACTIONS
Clinical Trial Experience With Clonidine Transdermal System
Most systemic adverse effects during clonidine transdermal system therapy have been mild and have tended to diminish with continued therapy. In a 3 month multi-clinic trial of clonidine transdermal system in 101 hypertensive patients, the systemic adverse reactions were: dry mouth (25 patients) and drowsiness (12), fatigue (6), headache (5), lethargy and sedation (3 each), insomnia, dizziness, impotence/sexual dysfunction, dry throat (2 each) and constipation, nausea, change in taste and nervousness (1 each).
In the above mentioned 3 month controlled clinical trial, as well as other uncontrolled clinical trials, the most frequent adverse reactions were dermatological and are described below.
In the 3 month trial, 51 of the 101 patients had localized skin reactions such as erythema (26 patients) and/or pruritus, particularly after using an adhesive cover throughout the 7 day dosage interval. Allergic contact sensitization to clonidine transdermal system was observed in 5 patients. Other skin reactions were localized vesiculation (7 patients), hyperpigmentation (5), edema (3), excoriation (3), burning (3), papules (1), throbbing (1), blanching (1), and a generalized macular rash (1).
In additional clinical experience, contact dermatitis resulting in treatment discontinuation was observed in 128 of 673 patients (about 19 in 100) after a mean duration of treatment of 37 weeks. The incidence of contact dermatitis was about 34 in 100 among white women, about 18 in 100 in white men, about 14 in 100 in black women, and approximately 8 in 100 in black men. Analysis of skin reaction data showed that the risk of having to discontinue clonidine transdermal system treatment because of contact dermatitis was greatest between treatment weeks 6 and 26, although sensitivity may develop either earlier or later in treatment.
In a large-scale clinical acceptability and safety study by 451 physicians in a total of 3539 patients, other allergic reactions were recorded for which a causal relationship to clonidine transdermal system was not established: maculopapular rash (10 cases); urticaria (2 cases); and angioedema of the face (2 cases), which also affected the tongue in one of the patients.
Marketing Experience With Clonidine Transdermal System
The following adverse reactions have been identified during post-approval use of clonidine transdermal system. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to clonidine transdermal system.
Body as a Whole: Fever; malaise; weakness; pallor; and withdrawal syndrome.
Cardiovascular: Congestive heart failure; cerebrovascular accident; electrocardiographic abnormalities (i.e., bradycardia, sick sinus syndrome disturbances and arrhythmias); chest pain; orthostatic symptoms; syncope; increases in blood pressure; sinus bradycardia and AV block with and without the use of concomitant digitalis; Raynaud’s phenomenon; tachycardia; bradycardia; and palpitations.
Central and Peripheral Nervous System/Psychiatric: Delirium; mental depression; hallucinations (including visual and auditory); localized numbness; vivid dreams or nightmares; restlessness; anxiety; agitation; irritability; other behavioral changes; and drowsiness.
Dermatological: Angioneurotic edema; localized or generalized rash; hives; urticaria; contact dermatitis; pruritus; alopecia; and localized hypo or hyper pigmentation.
Gastrointestinal: Anorexia and vomiting.
Genitourinary: Difficult micturition; loss of libido; and decreased sexual activity.
Metabolic: Gynecomastia or breast enlargement and weight gain.
Musculoskeletal: Muscle or joint pain; and leg cramps.
Ophthalmological: Blurred vision; burning of the eyes and dryness of the eyes.
Adverse Events Associated With Oral Clonidine Therapy
Most adverse effects are mild and tend to diminish with continued therapy. The most frequent (which appear to be dose-related) are dry mouth, occurring in about 40 of 100 patients; drowsiness, about 33 in 100; dizziness, about 16 in 100; constipation and sedation, each about 10 in 100. The following less frequent adverse experiences have also been reported in patients receiving clonidine hydrochloride USP tablets, but in many cases patients were receiving concomitant medication and a causal relationship has not been established.
Body as a Whole: Fatigue; fever; headache; pallor; weakness; and withdrawal syndrome. Also reported were a weakly positive Coombs’ test and increased sensitivity to alcohol.
Cardiovascular: Bradycardia; congestive heart failure; electrocardiographic abnormalities (i.e., sinus node arrest; junctional bradycardia; high degree AV block and arrhythmias); orthostatic symptoms; palpitations; Raynaud’s phenomenon; syncope; and tachycardia. Cases of sinus bradycardia and AV block have been reported, both with and without the use of concomitant digitalis.
Central Nervous System: Agitation; anxiety; delirium; delusional perception; hallucinations (including visual and auditory); insomnia; mental depression; nervousness; other behavioral changes; paresthesia; restlessness; sleep disorder; and vivid dreams or nightmares.
Dermatological: Alopecia; angioneurotic edema; hives; pruritus; rash; and urticaria.
Gastrointestinal: Abdominal pain; anorexia; constipation; hepatitis; malaise; mild transient abnormalities in liver function tests; nausea; parotitis; pseudo-obstruction (including colonic pseudo-obstruction); salivary gland pain; and vomiting.
Genitourinary: Decreased sexual activity; difficulty in micturition; erectile dysfunction; loss of libido; nocturia; and urinary retention.
Hematologic: Thrombocytopenia.
Metabolic: Gynecomastia; transient elevation of blood glucose or serum creatine phosphokinase; and weight gain.
Musculoskeletal: Leg cramps and muscle or joint pain.
Oro-otolaryngeal: Dryness of the nasal mucosa.
Ophthalmological: Accommodation disorder; blurred vision; burning of the eyes; decreased lacrimation; and dryness of the eyes.
OVERDOSAGE
Hypertension may develop early and may be followed by hypotension, bradycardia, respiratory depression, hypothermia, drowsiness, decreased or absent reflexes, weakness, irritability and miosis. The frequency of CNS depression may be higher in children than adults. Large overdoses may result in reversible cardiac conduction defects or dysrhythmias, apnea, coma and seizures. Signs and symptoms of overdose generally occur within 30 minutes to two hours after exposure. As little as 0.1 mg of clonidine has produced signs of toxicity in children.
If symptoms of poisoning occur following dermal exposure, remove all clonidine transdermal systems. After their removal, the plasma clonidine levels will persist for about 8 hours, then decline slowly over a period of several days. Rare cases of clonidine transdermal system poisoning due to accidental or deliberate mouthing or ingestion of the patch have been reported, many of them involving children.
There is no specific antidote for clonidine overdosage. Ipecac syrup-induced vomiting and gastric lavage would not be expected to remove significant amounts of clonidine following dermal exposure. If the patch is ingested, whole bowel irrigation may be considered and the administration of activated charcoal and/or cathartic may be beneficial. Supportive care may include atropine sulfate for bradycardia, intravenous fluids and/or vasopressor agents for hypotension and vasodilators for hypertension. Naloxone may be a useful adjunct for the management of clonidine-induced respiratory depression, hypotension and/or coma; blood pressure should be monitored since the administration of naloxone has occasionally resulted in paradoxical hypertension. Tolazoline administration has yielded inconsistent results and is not recommended as first-line therapy. Dialysis is not likely to significantly enhance the elimination of clonidine.
The largest overdose reported to date involved a 28-year-old male who ingested 100 mg of clonidine hydrochloride powder. This patient developed hypertension followed by hypotension, bradycardia, apnea, hallucinations, semicoma, and premature ventricular contractions. The patient fully recovered after intensive treatment. Plasma clonidine levels were 60 ng/mL after 1 hour, 190 ng/mL after 1.5 hours, 370 ng/mL after 2 hours, and 120 ng/mL after 5.5 and 6.5 hours. In mice and rats, the oral LD50 of clonidine is 206 and 465 mg/kg, respectively.
CLONIDINE DOSAGE AND ADMINISTRATION
Apply clonidine transdermal system USP once every 7 days to a hairless area of intact skin on the upper outer arm or chest. Each new application of clonidine transdermal system USP should be on a different skin site from the previous location. If the system loosens during 7 day wearing, the adhesive cover should be applied directly over the system to ensure good adhesion. There have been rare reports of the need for patch changes prior to 7 days to maintain blood pressure control.
To initiate therapy, clonidine transdermal system USP dosage should be titrated according to individual therapeutic requirements, starting with clonidine transdermal system USP 0.1 mg. If after one or two weeks the desired reduction in blood pressure is not achieved, increase the dosage by adding another clonidine transdermal system USP 0.1 mg or changing to a larger system. An increase in dosage above two clonidine transdermal system USP 0.3 mg is usually not associated with additional efficacy.
When substituting clonidine transdermal system USP for oral clonidine or for other antihypertensive drugs, physicians should be aware that the antihypertensive effect of clonidine transdermal system USP may not commence until 2 to 3 days after initial application. Therefore, gradual reduction of prior drug dosage is advised. Some or all previous antihypertensive treatment may have to be continued, particularly in patients with more severe forms of hypertension.
Renal Impairment
Patients with renal impairment may benefit from a lower initial dose. Patients should be carefully monitored. Since only a minimal amount of clonidine is removed during routine hemodialysis, there is no need to give supplemental clonidine following dialysis.
HOW SUPPLIED
Clonidine transdermal system USP 0.1 mg/day, 0.2 mg/day or 0.3 mg/day are available as 4 pouched systems and 4 adhesive covers per carton. Each system is a round corner, rectangular flexible transdermal system with a tan matte backing and clear membrane.
|
*Programmed Delivery - Clonidine in vivo Per Day Over 1 Week |
Debossed | Total Clonidine Content | Size |
NDC (for 4 systems) |
|
| Clonidine Transdermal System 0.1 mg/day | 0.1 mg | b 1009 | 3.09 mg | 4.33 cm2 | 0555-1009-16 |
| Clonidine Transdermal System 0.2 mg/day | 0.2 mg | b 1010 | 6.19 mg | 8.67 cm2 | 0555-1010-16 |
| Clonidine Transdermal System 0.3 mg/day | 0.3 mg | b 1011 | 9.28 mg | 13 cm2 | 0555-1011-16 |
STORAGE AND HANDLING
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
Manufactured By:
CORIUM INTERNATIONAL
Grand Rapids, MI 49512
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. C 8/2012
PATIENT INSTRUCTIONS
CLONIDINE Transdermal System USP
(Read the following instructions carefully before using this medication. If you have any questions, please consult with your doctor.)
General Information
Clonidine transdermal system is a round corner, rectangular flexible transdermal system with a tan matte backing and clear membrane, containing an active blood-pressure-lowering medication. It is designed to deliver the drug into the body through the skin smoothly and consistently for one full week. Normal exposure to water, as in showering, bathing, and swimming, should not affect the PATCH.
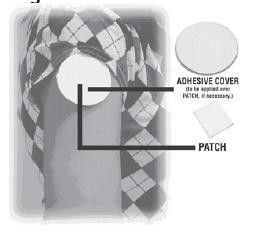
The optional ivory, round ADHESIVE COVER should be applied directly over the PATCH, should the PATCH begin to separate from the skin. The ivory, round ADHESIVE COVER ensures that the PATCH sticks to the skin. The clonidine transdermal system PATCH must be replaced with a new one on a fresh skin site if the one in use significantly loosens or falls off.
Figure 1:
Skin burns have been reported at the patch site in several patients wearing an aluminized transdermal system during a magnetic resonance imaging scan (MRI). Because the clonidine transdermal system contains aluminum, it is recommended to remove the system before undergoing an MRI.
How to Apply the Clonidine Transdermal System
1) Apply the tan, rectangular clonidine transdermal system PATCH once a week, preferably at a convenient time on the same day of the week (i.e., prior to bedtime on Tuesday of week one; prior to bedtime on Tuesday of week two, etc.).
Each carton contains two types of pouches:
Figure 2:
Contains PATCH with medication Contains ADHESIVE COVER for use
if the PATCH becomes loose.
2) Select a hairless area such as on the upper, outer arm or upper chest. The area chosen should
be free of cuts, abrasions, irritation, scars or calluses and should not be shaved before applying the clonidine transdermal system PATCH. Do not place the clonidine transdermal system PATCH on skin folds or under tight undergarments, since premature loosening may occur.
3) Wash hands with soap and water and thoroughly dry them.
4) Clean the area chosen with soap and water. Rinse and wipe dry with a clean, dry tissue.
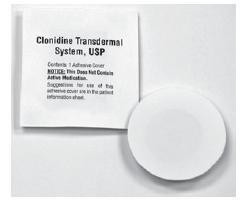
5) Select the pouch labeled “Clonidine Transdermal System USP” and open it as illustrated in Figure 3. Remove the tan, rectangular PATCH from the pouch.
Figure 3:

6) Remove the clear adhesive protective backing from the PATCH by gently peeling off one half of the backing at a time as shown in Figure 4. Avoid touching the sticky side of the clonidine transdermal system PATCH.
Figure 4:

7) Place the clonidine transdermal system PATCH on the prepared skin site (sticky side down) by applying firm pressure over the PATCH to ensure good contact with the skin, especially around the edges (Figure 5). Discard the clear adhesive protective backing and wash your hands with soap and water to remove any drug from your hands.
Figure 5:

8) After one week, remove the old PATCH and discard it (refer to Instructions for Disposal). After choosing a different skin site, repeat instructions 2 through 7 for the application of your next clonidine transdermal system PATCH.
What to do if your Clonidine Transdermal System PATCH becomes loose while wearing:
How to Apply the ADHESIVE COVER
Note: The ivory, round, ADHESIVE COVER does not contain any drug and should not be used alone. The COVER should be applied directly over the clonidine transdermal system PATCH only if the PATCH begins to separate from the skin, thereby ensuring that it sticks to the skin for seven full days.
Figure 6:
1) Wash hands with soap and water and thoroughly dry them.
2) Using a clean, dry tissue, make sure that the area around the tan, rectangular clonidine transdermal system PATCH is clean and dry. Press gently on the clonidine transdermal system PATCH to ensure that the edges are in good contact with the skin.
3) Take the ivory, round, ADHESIVE COVER (Figure 6) from the pouch and remove the paper liner backing from the COVER.
4) Carefully center the ivory, round, ADHESIVE COVER over the tan, rectangular clonidine transdermal system PATCH, and apply firm pressure, especially around the edges in contact with the skin.
Instructions for Disposal
During or even after use, a PATCH contains active medication which may be harmful to infants and children if accidentally applied or ingested. After use, fold in half with the sticky sides together. Dispose of carefully out of reach of children.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
Store at 20° to 25°C (68° to 77°F).
Manufactured By:
CORIUM INTERNATIONAL
Grand Rapids, MI 49512
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. A 2/2011
Image of Label
ClonidineClonidine PATCH, EXTENDED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||