Androgel
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use AndroGel safely and effectively. See full prescribing information for AndroGel.AndroGel (testosterone gel) 1% for topical use CIIIInitial U.S. Approval: 1953 BOXED WARNING WARNING: SECONDARY EXPOSURE TO TESTOSTERONE Virilization has been reported in children who were secondarily exposed to testosterone gel (5.2, 6.2). Children should avoid contact with unwashed or unclothed application sites in men using testosterone gel (5.2). Healthcare providers should advise patients to strictly adhere to recommended instructions for use (5.2). RECENT MAJOR CHANGES Boxed Warning 9/2009 WARNINGS AND PRECAUTIONS (5.2) 9/2009 INDICATIONS AND USAGEAndroGel is an androgen indicated for replacement therapy in males for conditions associated with a deficiency or absence of endogenous testosterone: Primary Hypogonadism (Congenital or Acquired) (1.1) Hypogonadotropic Hypogonadism (Congenital or Acquired) (1.1) DOSAGE AND ADMINISTRATION Recommended starting dose: 5 g for adult males, applied topically once daily (2.1). Apply to clean, dry, intact skin of shoulders and upper arms and/or abdomen. Do NOT apply AndroGel to the genitals (2.1). Dose adjustment for adult males: If serum testosterone level is below the normal range, adjust dose from 5 g to 7.5 g and from 7.5 g to 10 g (2.3). DOSAGE FORMS AND STRENGTHSAndroGel (testosterone gel) 1% for topical use is available as: 2 x 75 g pumps (each pump dispenses 60 metered 1.25 g doses) (3) 2.5 g packet or 5 g packet (3) CONTRAINDICATIONS Men with carcinoma of the breast or known or suspected prostate cancer (4, 5.1). Pregnant or breast feeding women. Testosterone may cause fetal harm (4). WARNINGS AND PRECAUTIONS Patients with benign prostatic hyperplasia (BPH) treated with androgens are at an increased risk for worsening of signs and symptoms of BPH (5.1). Secondary exposure to testosterone in children and women can occur with use of testosterone gel (5.2). Cases of secondary exposure resulting in virilization of children have been reported (6.2). Children and women should avoid contact with unwashed or unclothed application site(s) in men using testosterone gel. To minimize the potential for transfer to others, patients using AndroGel should apply the product as directed and strictly adhere to the following (5.2): Wash hands with soap and water after application. Cover the application site with clothing after the gel has dried. Wash the application site thoroughly with soap and water prior to any situation where skin-to-skin contact of the application site with another person is anticipated. Signs of virilization in children and women and the possibility of secondary exposure to testosterone gel should be brought to the attention of the healthcare provider. Testosterone gel should be promptly discontinued until the cause of the virilization is identified (5.2). Due to lack of controlled evaluations in women and potential virilizing effects, AndroGel is not indicated for use in women (5.3). Exogenous administration of androgens may lead to azoospermia (5.4). Edema may be a complication in patients with preexisting cardiac, renal, or hepatic disease (5.6, 6.2). Gynecomastia, enlargement of breast, may develop (5.7). Sleep apnea may occur in those with risk factors (5.8). Monitor serum testosterone, prostatic specific antigen, hemoglobin, hematocrit, liver function test, and lipid levels periodically (2.3, 5.1, 5.9). Alcohol-based gels are flammable until dry (5.10). Side EffectsMost common adverse reactions (incidence ≥ 5%) are acne, application site reaction, abnormal lab tests, and prostatic disorders (6). Cases of testosterone secondary exposure resulting in virilization of children have been reported (6.2). Reported signs and symptoms have included enlargement of the penis or clitoris, premature development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases with a reported outcome, these signs and symptoms were reported to have regressed with removal of the exposure to testosterone gel (5.2, 6.2). In a few cases, however, enlarged genitalia did not fully return to age-appropriate normal size and bone age remained modestly greater than chronological age. To report SUSPECTED ADVERSE REACTIONS, contact Abbott Laboratories at 1-800-241-1643 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . DRUG INTERACTIONS Androgens may decrease blood glucose, and therefore insulin requirement in diabetic patients (7.1). Use of testosterone with ACTH or corticosteroids may result in increased fluid retention. Use with caution, particularly in patients with cardiac, renal, or hepatic disease (7.2). Changes in anticoagulant activity may be seen with androgens. More frequent monitoring of INR and prothrombin time is recommended (7.3). USE IN SPECIFIC POPULATIONS Pregnancy: AndroGel may cause teratogenic effects. AndroGel should not be used in pregnant women (4, 8.1). Nursing mothers should not use AndroGel (4, 8.3). Safety and efficacy of AndroGel in males < 18 years old has not been established (8.4). There have not been sufficient numbers of geriatric patients involved in controlled clinical studies utilizing AndroGel to determine whether efficacy in those > 65 differs from younger subjects. Additionally, there is insufficient long-term safety data in geriatric patients to assess the potential risks of cardiovascular disease and prostate cancer (8.5). No formal studies were conducted involving patients with renal or hepatic insufficiencies (8.6).
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
- 1 ANDROGEL INDICATIONS AND USAGE
- 2 ANDROGEL DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 ANDROGEL CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
- 5.2 Potential for Secondary Exposure to Testosterone
- 5.3 Use in Women
- 5.4 Potential for Adverse Effects on Spermatogenesis
- 5.5 Hepatic Adverse Effects
- 5.6 Edema
- 5.7 Gynecomastia
- 5.8 Sleep Apnea
- 5.9 Laboratory Tests
- 5.10 Flammable Until Dry
- 6 ANDROGEL ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 ANDROGEL DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- FDA-Approved Medication Guide
FULL PRESCRIBING INFORMATION
WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
- Virilization has been reported in children who were secondarily exposed to testosterone gel [see Warnings and Precautions (5.2) and Adverse Reactions (6.2)] .
- Children should avoid contact with unwashed or unclothed application sites in men using testosterone gel [see Warnings and Precautions (5.2)] .
- Healthcare providers should advise patients to strictly adhere to recommended instructions for use [see Warnings and Precautions (5.2) ] .
1 INDICATIONS AND USAGE
1.1 Testosterone Replacement Therapy
AndroGel, an androgen, is indicated for replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone:
- Primary Hypogonadism (Congenital or Acquired) - testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchiectomy, Klinefelter's syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. These men usually have low serum testosterone levels and gonadotropins (FSH, LH) above the normal range.
- Hypogonadotropic Hypogonadism (Congenital or Acquired) - idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. These men have low testosterone serum levels but have gonadotropins in the normal or low range.
2 DOSAGE AND ADMINISTRATION
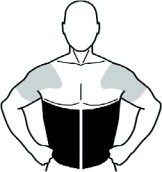
2.1 General Dosing
The recommended starting dose of AndroGel is 5 g once daily (preferably in the morning) to clean, dry, intact skin of the shoulders and upper arms and/or abdomen (area of application should be limited to the area that will be covered by the patient's short sleeve t-shirt). AndroGel must not be applied to the genitals. AndroGel is supplied as either a pump or in individual packets. After applying the gel, the application site should be allowed to dry for a few minutes prior to dressing. Avoid fire, flames or smoking until the gel has dried since alcohol based products, including AndroGel, are flammable. Hands should be washed with soap and water after AndroGel has been applied. [see Warnings and Precautions (5.2, 5.10)].
2.2 Administration
Multi-Dose Pump
Patients should be instructed to prime the pump before using it for the first time by fully depressing the pump mechanism (actuation) 3 times and discard this portion of the product to assure precise dose delivery. After the priming procedure, patients should completely depress the pump one time (actuation) for every 1.25 g (AndroGel Pump) of product required to achieve the daily prescribed dosage. The product may be delivered directly into the palm of the hand and then applied to the desired application sites, either one pump actuation at a time or upon completion of all pump actuations required for the daily dose. Alternatively, the product can be applied directly to the application sites. Application directly to the sites may prevent loss of product that may occur during transfer from the palm of the hand onto the application sites. Table 1 has specific dosing guidelines for adult males when the 75 g AndroGel Pump is used.
| Prescribed Daily Dose | Number of Pump Actuations in 75 g Pump |
|---|---|
| 5 g | 4 (once daily) |
| 7.5 g | 6 (once daily) |
| 10 g | 8 (once daily) |
Packets
The entire contents should be squeezed into the palm of the hand and immediately applied to the application sites. Alternately, patients may squeeze a portion of the gel from the packet into the palm of the hand and apply to application sites. Repeat until entire contents have been applied.
2.3 Dose Adjustment and Patient Assessments
- To ensure proper dosing, serum testosterone levels should be measured at intervals and replaced to serum testosterone levels in the normal range. If the serum testosterone concentration is below the normal range, the daily AndroGel dose may be increased from 5 g to 7.5 g and from 7.5 g to 10 g for adult males as instructed by the physician. If the serum testosterone concentration exceeds the normal range, the daily AndroGel dose may be decreased. If the serum testosterone concentration consistently exceeds the normal range at a daily dose of 5 g, AndroGel therapy should be discontinued.
The following is general advice for treating and monitoring adult patients on AndroGel. No specific recommendations can be made.
- Prescribers should be aware that testosterone is contraindicated in men with known or suspected prostate cancer. Therefore, evaluation for prostate cancer prior to initiation of AndroGel therapy is appropriate [see Contraindications (4)].
- Based on results from controlled studies, serum PSA may rise when taking AndroGel. Therefore, periodic assessment of serum PSA is recommended in patients taking AndroGel [see Adverse Reactions (6.1)].
- Based on results from controlled studies, worsening of BPH may occur in patients taking AndroGel [see Adverse Reactions (6.1)]. Therefore, periodic assessments for signs and symptoms of BPH are recommended in patients taking AndroGel.
- Hematocrit, serum lipid profile, and liver function test should be monitored in patients taking AndroGel [see Warnings and Precautions (5.9)].
3 DOSAGE FORMS AND STRENGTHS
AndroGel (testosterone gel) 1% for topical use is available in either unit-dose packets or multiple-dose pumps. The 75 g (60 metered-dose) pump delivers 1.25 g of product when the pump mechanism is fully depressed once.
AndroGel is available in the following three package containers:
- 2 x 75 g pumps (each pump dispenses 60 metered 1.25 g doses)
- 2.5 g packet
- 5 g packet
4 CONTRAINDICATIONS
AndroGel should not be used in any of the following patients:
- Men with carcinoma of the breast or known or suspected carcinoma of the prostate [see Warnings and Precautions (5.1), Adverse Reactions (6.1), and Nonclinical Toxicology (13.1)].
- Women who are or may become pregnant, or who are breastfeeding. AndroGel can cause fetal harm when administered to a pregnant woman. AndroGel may cause serious adverse reactions in nursing infants. Exposure of a female fetus or nursing infant to androgens may result in varying degrees of virilization. Pregnant women or those who may become pregnant need to be aware of the potential for transfer of testosterone from men treated with AndroGel [see Warnings and Precautions (5.2) and Use in Specific Populations (8.1, 8.3)].
- Men with known hypersensitivity to any of its ingredients, including alcohol and soy products.
5 WARNINGS AND PRECAUTIONS
5.1 Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
- Patients with BPH treated with androgens are at an increased risk for worsening of signs and symptoms of BPH.
- Patients treated with androgens may be at increased risk for prostate cancer. Evaluation of the patient for prostate cancer prior to initiating and during treatment with androgens is appropriate.
- Increases in serum PSA from baseline values were seen in approximately 18% of individuals in an open label study of 162 hypogonadal men treated with AndroGel for up to 42 months. Most of these increases were seen within the first year of therapy [see Contraindications (4), Warnings and Precautions (5.9), Adverse Reactions (6.1), and Nonclinical Toxicology (13.1)].
5.2 Potential for Secondary Exposure to Testosterone
Secondary exposure to testosterone in children and women can occur with testosterone gel use in men [see Clinical Studies (14.3)]. Cases of secondary exposure resulting in virilization of children have been reported in postmarketing surveillance. Signs and symptoms have included enlargement of the penis or clitoris, development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases, these signs and symptoms regressed with removal of the exposure to testosterone gel. In a few cases, however, enlarged genitalia did not fully return to age-appropriate normal size, and bone age remained modestly greater than chronological age. The risk of transfer was increased in some of these cases by not adhering to precautions for the appropriate use of testosterone gel.
Inappropriate changes in genital size or development of pubic hair or libido in children, or changes in body hair distribution, significant increase in acne, or other signs of virilization in adult women should be brought to the attention of a physician and the possibility of secondary exposure to testosterone gel should also be brought to the attention of a physician. Testosterone gel should be promptly discontinued until the cause of virilization has been identified.
Testosterone may cause fetal harm in a pregnant woman due to virilization of a female fetus [see Use in Specific Populations (8.1)].
Strict adherence to the following precautions is advised in order to minimize the potential for secondary exposure to testosterone from AndroGel-treated skin:
- Children and women should avoid contact with unwashed or unclothed application site(s) of men using testosterone gel.
- AndroGel should only be applied to the shoulders, upper arms, and/or abdomen (area of application should be limited to the area that will be covered by the patient's short sleeve t-shirt).
- Patients should wash their hands immediately with soap and water after applying AndroGel.
- Patients should cover the application site(s) with clothing (e.g., a shirt) after the gel has dried.
- Prior to any situation in which skin-to-skin contact with the application site is anticipated, patients should wash the application site(s) thoroughly with soap and water to remove any testosterone residue.
- In the event that unwashed or unclothed skin to which AndroGel has been applied comes in direct contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible. Studies show that residual testosterone is removed from the skin surface by washing with soap and water.
5.3 Use in Women
Due to lack of controlled evaluations in women and potential virilizing effects, AndroGel is not indicated for use in women [see Use in Specific Populations (8.1, 8.3)].
5.4 Potential for Adverse Effects on Spermatogenesis
At large doses of exogenous androgens, spermatogenesis may be suppressed through feedback inhibition of pituitary follicle-stimulating hormone (FSH) which could possibly lead to adverse effects on semen parameters including sperm count.
5.5 Hepatic Adverse Effects
Prolonged use of high doses of orally active 17-alpha-alkyl androgens (e.g., methyltestosterone) has been associated with serious hepatic adverse effects (peliosis hepatis, hepatic neoplasms, cholestatic hepatitis, and jaundice). Peliosis hepatis can be a life-threatening or fatal complication. Long-term therapy with intramuscular testosterone enanthate has produced multiple hepatic adenomas. AndroGel is not known to produce these adverse effects.
There are rare reports of hepatocellular carcinoma in patients receiving long-term oral therapy with androgens in high doses. Withdrawal of the drugs did not lead to regression of the tumors in all cases.
5.6 Edema
Drugs in the androgen class may promote retention of sodium and water. Edema with or without congestive heart failure may be a serious complication in patients with preexisting cardiac, renal, or hepatic disease [see Adverse Reactions (6.2)].
5.7 Gynecomastia
Gynecomastia may develop and may persist in patients being treated with androgens, including AndroGel, for hypogonadism.
5.8 Sleep Apnea
The treatment of hypogonadal men with testosterone products may potentiate sleep apnea in some patients, especially those with risk factors such as obesity or chronic lung diseases [see Adverse Reactions (6.2)].
5.9 Laboratory Tests
- Increases in hematocrit, reflective of increases in red blood cell mass, may require lowering or discontinuation of testosterone. Increase in red blood cell mass may increase the risk for a thromboembolic event.
- Changes in serum lipid profile may require dose adjustment or discontinuation of testosterone therapy.
- Androgens may decrease levels of thyroxin-binding globulin, resulting in decreased total T4 serum levels and increased resin uptake of T3 and T4. Free thyroid hormone levels remain unchanged, however, and there is no clinical evidence of thyroid dysfunction.
- Androgens should be used with caution in cancer patients at risk of hypercalcemia (and associated hypercalciuria). Regular monitoring of serum calcium concentrations is recommended in these patients.
5.10 Flammable Until Dry
- Alcohol Based Products including AndroGel are flammable; therefore avoid fire, flame or smoking until the gel has dried.
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials in Hypogonadal Men
Table 2 shows the incidence of all adverse events judged by the investigator to be at least possibly related to treatment with AndroGel and reported by >1% of patients in a 180 Day, Phase 3 study.
|
*Lab test abnormal occurred in nine patients with one or more of the following events reported: elevated hemoglobin or hematocrit, hyperlipidemia, elevated triglycerides, hypokalemia, decreased HDL, elevated glucose, elevated creatinine, elevated total bilirubin. |
|||
|
**Prostate disorders included five patients with enlarged prostate, one with BPH, and one with elevated PSA results. |
|||
|
***Testis disorders were reported in two patients: one with left varicocele and one with slight sensitivity of left testis. |
|||
| Adverse Event | Dose of AndroGel | ||
| 5 g | 7.5 g | 10 g | |
| N = 77 | N = 40 | N = 78 | |
| Acne | 1% | 3% | 8% |
| Alopecia | 1% | 0% | 1% |
| Application Site Reaction | 5% | 3% | 4% |
| Asthenia | 0% | 3% | 1% |
| Depression | 1% | 0% | 1% |
| Emotional Lability | 0% | 3% | 3% |
| Gynecomastia | 1% | 0% | 3% |
| Headache | 4% | 3% | 0% |
| Hypertension | 3% | 0% | 3% |
| Lab Test Abnormal* | 6% | 5% | 3% |
| Libido Decreased | 0% | 3% | 1% |
| Nervousness | 0% | 3% | 1% |
| Pain Breast | 1% | 3% | 1% |
| Prostate Disorder** | 3% | 3% | 5% |
| Testis Disorder*** | 3% | 0% | 0% |
Other less common adverse reactions, reported in fewer than 1% of patients included: amnesia, anxiety, discolored hair, dizziness, dry skin, hirsutism, hostility, impaired urination, paresthesia, penis disorder, peripheral edema, sweating, and vasodilation.
In this 180 day clinical trial, skin reactions at the site of application were reported with AndroGel, but none was severe enough to require treatment or discontinuation of drug.
Six patients (4%) in this trial had adverse events that led to discontinuation of AndroGel. These events included: cerebral hemorrhage, convulsion (neither of which were considered related to AndroGel administration), depression, sadness, memory loss, elevated prostate specific antigen, and hypertension. No AndroGel patient discontinued due to skin reactions.
In a separate uncontrolled pharmacokinetic study of 10 patients, two had adverse events associated with AndroGel; these were asthenia and depression in one patient and increased libido and hyperkinesia in the other.
In a 3 year, flexible dose, extension study, the incidence of all adverse events judged by the investigator to be at least possibly related to treatment with AndroGel and reported by > 1% of patients is shown in Table 3.
| Adverse Event | Percent of Subjects |
|---|---|
| (N = 162) | |
|
+Lab test abnormal occurred in 15 patients with one or more of the following events reported: elevated AST, elevated ALT, elevated testosterone, elevated hemoglobin or hematocrit, elevated cholesterol, elevated cholesterol/LDL ratio, elevated triglycerides, elevated HDL, elevated serum creatinine. |
|
|
*Urinary symptoms included nocturia, urinary hesitancy, urinary incontinence, urinary retention, urinary urgency and weak urinary stream. |
|
|
**Testis disorders included three patients. There were two with a non-palpable testis and one with slight right testicular tenderness. |
|
| Lab Test Abnormal+ | 9.3 |
| Skin dry | 1.9 |
| Application Site Reaction | 5.6 |
| Acne | 3.1 |
| Pruritus | 1.9 |
| Enlarged Prostate | 11.7 |
| Carcinoma of Prostate | 1.2 |
| Urinary Symptoms* | 3.7 |
| Testis Disorder** | 1.9 |
| Gynecomastia | 2.5 |
| Anemia | 2.5 |
Two patients reported serious adverse events considered possibly related to treatment: deep vein thrombosis (DVT) and prostate disorder requiring a transurethral resection of the prostate (TURP).
Discontinuation for adverse events in this study included: two patients with application site reactions, one with kidney failure, and five with prostate disorders (including increase in serum PSA in 4 patients, and increase in PSA with prostate enlargement in a fifth patient).
Increases in Serum PSA Observed in Clinical Trials of Hypogonadal Men
During the initial 6-month study, the mean change in PSA values had a statistically significant increase of 0.26 ng/mL. Serum PSA was measured every 6 months thereafter in the 162 hypogonadal men on AndroGel in the 3-year extension study. There was no additional statistically significant increase observed in mean PSA from 6 months through 36 months. However, there were increases in serum PSA observed in approximately 18% of individual patients. The overall mean change from baseline in serum PSA values for the entire group from month 6 to 36 was 0.11 ng/mL.
Twenty-nine patients (18%) met the per-protocol criterion for increase in serum PSA, defined as >2X the baseline or any single serum PSA >6 ng/mL. Most of these (25/29) met this criterion by at least doubling of their PSA from baseline. In most cases where PSA at least doubled (22/25), the maximum serum PSA value was still <2 ng/mL. The first occurrence of a pre-specified, post-baseline increase in serum PSA was seen at or prior to Month 12 in most of the patients who met this criterion (23 of 29; 79%).
Four patients met this criterion by having a serum PSA >6 ng/mL and in these, maximum serum PSA values were 6.2 ng/mL, 6.6 ng/mL, 6.7 ng/mL, and 10.7 ng/mL. In two of these patients, prostate cancer was detected on biopsy. The first patient's PSA levels were 4.7 ng/mL and 6.2 ng/mL at baseline and at Month 6/Final, respectively. The second patient's PSA levels were 4.2 ng/mL, 5.2 ng/mL, 5.8 ng/mL, and 6.6 ng/mL at baseline, Month 6, Month 12, and Final, respectively.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of AndroGel. Because the reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Secondary Exposure to Testosterone in Children
Cases of secondary exposure to testosterone resulting in virilization of children have been reported in postmarket surveillance. Signs and symptoms of these reported cases have included enlargement of the clitoris (with surgical intervention) or the penis, development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases with a reported outcome, these signs and symptoms were reported to have regressed with removal of the testosterone gel exposure. In a few cases, however, enlarged genitalia did not fully return to age appropriate normal size, and bone age remained modestly greater than chronological age. In some of the cases, direct contact with the sites of application on the skin of men using testosterone gel was reported. In at least one reported case, the reporter considered the possibility of secondary exposure from items such as the testosterone gel user's shirts and/or other fabric, such as towels and sheets [see Warnings and Precautions (5.2)].
Hypogonadal Men
Table 4 includes adverse reactions that have been identified postmarketing.
| Blood and the lymphatic system disorders: | Elevated Hgb, Hct (polycythemia) |
| Endocrine disorders: | Hirsutism |
| Gastrointestinal disorders: | Nausea |
| General disorders and administration site reactions: | Asthenia, edema, malaise |
| Genitourinary disorders: | Impaired urination |
| Hepatobiliary disorders: | Abnormal liver function tests (e.g. transaminases, elevated GGTP, bilirubin) |
| Investigations: | Elevated PSA, electrolyte changes (nitrogen, calcium, potassium, phosphorus, sodium), changes in serum lipids (hyperlipidemia, elevated triglycerides, decreased HDL), impaired glucose tolerance, fluctuating testosterone levels, weight increase |
| Neoplasms benign, malignant and unspecified (cysts and polyps): | Prostate cancer |
| Nervous system: | Headache, dizziness, sleep apnea, insomnia |
| Psychiatric disorders: | Depression, emotional lability, decreased libido, nervousness, hostility, amnesia, anxiety |
| Reproductive system and breast disorders: | Gynecomastia, mastodynia, prostatic enlargement, testicular atrophy, oligospermia, priapism (frequent or prolonged erections) |
| Respiratory disorders: | Dyspnea |
| Skin and subcutaneous tissue disorders: | Acne, alopecia, application site reaction (pruritus, dry skin, erythema, rash, discolored hair, paresthesia), sweating |
| Vascular disorders: | Hypertension, vasodilation (hot flushes) |
7 DRUG INTERACTIONS
7.1 Insulin
Changes in insulin sensitivity or glycemic control may occur in patients treated with androgens. In diabetic patients, the metabolic effects of androgens may decrease blood glucose and, therefore, insulin requirements.
7.2 Corticosteroids
The concurrent use of testosterone with ACTH or corticosteroids may result in increased fluid retention and should be monitored cautiously, particularly in patients with cardiac, renal or hepatic disease.
7.3 Oral Anticoagulants
Changes in anticoagulant activity may be seen with androgens. More frequent monitoring of INR and prothrombin time are recommended in patients taking anticoagulants, especially at the initiation and termination of androgen therapy.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X: AndroGel is contraindicated during pregnancy or in women who may become pregnant. It is teratogenic and may cause fetal harm [see Contraindications (4)]. Exposure of a female fetus to androgens may result in varying degrees of virilization. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
8.3 Nursing Mothers
Although it is not known how much testosterone transfers into human milk, AndroGel is contraindicated in nursing women because of the potential for serious adverse reactions in nursing infants [see Contraindications (4)].
Testosterone and other androgens may adversely affect lactation.
8.4 Pediatric Use
Safety and efficacy of AndroGel in males < 18 years old has not been established. Improper use may result in acceleration of bone age and premature closure of epiphyses.
8.5 Geriatric Use
There have not been sufficient numbers of geriatric patients involved in controlled clinical studies utilizing AndroGel to determine whether efficacy in those over 65 years of age differs from younger subjects. Additionally, there is insufficient long-term safety data in geriatric patients to assess the potential risks of cardiovascular disease and prostate cancer.
8.6 Renal or Hepatic Impairment
No formal studies were conducted involving patients with renal or hepatic insufficiencies.
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
AndroGel contains testosterone, a Schedule III controlled substance as defined by the Anabolic Steroids Control Act.
Oral ingestion of AndroGel will not result in clinically significant serum testosterone concentrations due to extensive first-pass metabolism.
10 OVERDOSAGE
There is one report of acute overdosage with use of an approved injectable testosterone product: this subject had serum testosterone levels of up to 11,400 ng/dL with a cerebrovascular accident. Treatment of overdosage would consist of discontinuation of AndroGel together with appropriate symptomatic and supportive care.
11 DESCRIPTION
AndroGel (testosterone gel) 1% is a clear, colorless hydroalcoholic gel containing 1% testosterone. Topical administration of AndroGel 5 g, 7.5 g, or 10 g contains 50 mg, 75 mg, or 100 mg of testosterone, respectively, is to be applied daily to the skin's surface. Approximately 10% of the applied testosterone dose is absorbed across skin of average permeability during a 24-hour period.
The active pharmacologic ingredient in AndroGel is testosterone. Testosterone USP is a white to practically white crystalline powder chemically described as 17-beta hydroxyandrost-4-en-3-one. The structural formula is:
Inactive ingredients in AndroGel are carbomer 980, ethanol 67.0%, isopropyl myristate, purified water, and sodium hydroxide. These ingredients are not pharmacologically active.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Endogenous androgens, including testosterone and dihydrotestosterone (DHT), are responsible for the normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of prostate, seminal vesicles, penis and scrotum; the development of male hair distribution, such as facial, pubic, chest and axillary hair; laryngeal enlargement, vocal chord thickening, alterations in body musculature and fat distribution. Testosterone and DHT are necessary for the normal development of secondary sex characteristics. Male hypogonadism results from insufficient secretion of testosterone and is characterized by low serum testosterone concentrations. Signs/symptoms associated with male hypogonadism include erectile dysfunction and decreased sexual desire, fatigue and loss of energy, mood depression, regression of secondary sexual characteristics and osteoporosis.
Male hypogonadism has two main etiologies. Primary hypogonadism is caused by defects of the gonads, such as Klinefelter's Syndrome or Leydig cell aplasia, whereas secondary hypogonadism is the failure of the hypothalamus (or pituitary) to produce sufficient gonadotropins (FSH, LH).
12.3 Pharmacokinetics
Adult Males
Absorption
AndroGel delivers physiologic amounts of testosterone, producing circulating testosterone concentrations that approximate normal levels (298 – 1043 ng/dL) seen in healthy men. AndroGel provides continuous transdermal delivery of testosterone for 24 hours following a single application to intact, clean, dry skin of the shoulders, upper arms and/or abdomen.
AndroGel is a hydroalcoholic formulation that dries quickly when applied to the skin surface. The skin serves as a reservoir for the sustained release of testosterone into the systemic circulation. Approximately 10% of the testosterone dose applied on the skin surface from AndroGel is absorbed into systemic circulation. Therefore, 5 g and 10 g of AndroGel systemically deliver approximately 5 mg and 10 mg of testosterone, respectively. In a study with 10 g of AndroGel, all patients showed an increase in serum testosterone within 30 minutes, and eight of nine patients had a serum testosterone concentration within normal range by 4 hours after the initial application. Absorption of testosterone into the blood continues for the entire 24-hour dosing interval. Serum concentrations approximate the steady-state level by the end of the first 24 hours and are at steady state by the second or third day of dosing.
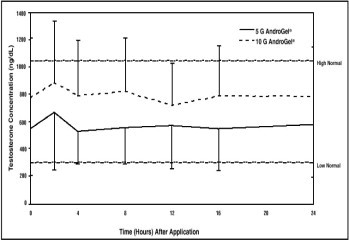
With single daily applications of AndroGel, follow-up measurements 30, 90 and 180 days after starting treatment have confirmed that serum testosterone concentrations are generally maintained within the eugonadal range. Figure 1 summarizes the 24-hour pharmacokinetic profiles of testosterone for hypogonadal men (<300 ng/dL) maintained on 5 g or 10 g of AndroGel for 30 days. The average (± SD) daily testosterone concentration produced by AndroGel 10 g on Day 30 was 792 (± 294) ng/dL and by AndroGel 5 g 566 (± 262) ng/dL.
Figure 1: Mean (± SD) Steady-State Serum Testosterone Concentrations on Day 30 in Patients Applying AndroGel Once Daily
When AndroGel treatment is discontinued after achieving steady state, serum testosterone levels remain in the normal range for 24 to 48 hours but return to their pretreatment levels by the fifth day after the last application.
Distribution
Circulating testosterone is primarily bound in the serum to sex hormone-binding globulin (SHBG) and albumin. Approximately 40% of testosterone in plasma is bound to SHBG, 2% remains unbound (free) and the rest is bound to albumin and other proteins.
Metabolism
There is considerable variation in the half-life of testosterone as reported in the literature, ranging from 10 to 100 minutes. Testosterone is metabolized to various 17-keto steroids through two different pathways. The major active metabolites of testosterone are estradiol and DHT.
DHT concentrations increased in parallel with testosterone concentrations during AndroGel treatment. After 180 days of treatment in adult males, mean DHT concentrations were within the normal range with 5 g AndroGel and were about 7% above the normal range after a 10 g dose. The mean steady-state DHT/T ratio during 180 days of AndroGel treatment remained within normal limits and ranged from 0.23 to 0.29 (5 g/day) and from 0.27 to 0.33 (10 g/day).
Excretion
About 90% of a dose of testosterone given intramuscularly is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and its metabolites; about 6% of a dose is excreted in the feces, mostly in the unconjugated form. Inactivation of testosterone occurs primarily in the liver.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Testosterone has been tested by subcutaneous injection and implantation in mice and rats. In mice, the implant induced cervical-uterine tumors, which metastasized in some cases. There is suggestive evidence that injection of testosterone into some strains of female mice increases their susceptibility to hepatoma. Testosterone is also known to increase the number of tumors and decrease the degree of differentiation of chemically induced carcinomas of the liver in rats.
14 CLINICAL STUDIES
14.1 Clinical Trials in Adult Hypogonadal Males
AndroGel was evaluated in a multi-center, randomized, parallel-group, active-controlled, 180-day trial in 227 hypogonadal men. The study was conducted in 2 phases. During the Initial Treatment Period (Days 1-90), 73 patients were randomized to AndroGel 5 g daily, 78 patients to AndroGel 10 g daily, and 76 patients to a non-scrotal testosterone transdermal system. The study was double-blind for dose of AndroGel but open-label for active control. Patients who were originally randomized to AndroGel and who had single-sample serum testosterone levels above or below the normal range on Day 60 were titrated to 7.5 g daily on Day 91. During the Extended Treatment Period (Days 91-180), 51 patients continued on AndroGel 5 g daily, 52 patients continued on AndroGel 10 g daily, 41 patients continued on a non-scrotal testosterone transdermal system (5 mg daily), and 40 patients received AndroGel 7.5 g daily. Upon completion of the initial study, 163 enrolled and 162 patients received treatment in an open-label extension study of AndroGel for an additional period of up to 3 years.
Mean peak, trough and average serum testosterone concentrations within the normal range (298-1043 ng/dL) were achieved on the first day of treatment with doses of 5 g and 10 g. In patients continuing on AndroGel 5 g and 10 g, these mean testosterone levels were maintained within the normal range for the 180-day duration of the original study. Figure 2 summarizes the 24-hour pharmacokinetic profiles of testosterone administered as AndroGel for 30, 90 and 180 days. Testosterone concentrations were maintained as long as the patient continued to properly apply the prescribed AndroGel treatment.
Figure 2: Mean Steady-State Testosterone Concentrations in Patients with Once-Daily AndroGel Therapy
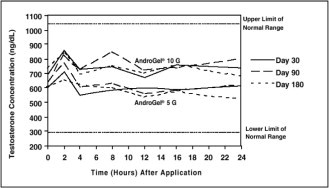
Table 5 summarizes the mean testosterone concentrations on Treatment Day 180 for patients receiving 5 g, 7.5 g, or 10 g of AndroGel. The 7.5 g dose produced mean concentrations intermediate to those produced by 5 g and 10 g of AndroGel.
| 5 g | 7.5 g | 10 g | |
| N = 44 | N = 37 | N = 48 | |
| Cavg | 555 ± 225 | 601 ± 309 | 713 ± 209 |
| Cmax | 830 ± 347 | 901 ± 471 | 1083 ± 434 |
| Cmin | 371 ± 165 | 406 ± 220 | 485 ± 156 |
Of 129 hypogonadal men who were appropriately titrated with AndroGel and who had sufficient data for analysis, 87% achieved an average serum testosterone level within the normal range on Treatment Day 180.
In patients treated with AndroGel, there were no observed differences in the average daily serum testosterone concentrations at steady-state based on age, cause of hypogonadism, or body mass index.
AndroGel 5 g/day and 10 g/day resulted in significant increases over time in total body mass and total body lean mass, while total body fat mass and the percent body fat decreased significantly. These changes were maintained for 180 days of treatment during the original study. Changes in the 7.5 g dose group were similar. Bone mineral density in both hip and spine increased significantly from Baseline to Day 180 with 10 g AndroGel.
AndroGel treatment at 5 g/day and 10 g/day for 90 days produced significant improvement in libido (measured by sexual motivation, sexual activity and enjoyment of sexual activity as assessed by patient responses to a questionnaire). The degree of penile erection as subjectively estimated by the patients, increased with AndroGel treatment, as did the subjective score for “satisfactory duration of erection.” AndroGel treatment at 5 g/day and 10 g/day produced positive effects on mood and fatigue. Similar changes were seen after 180 days of treatment and in the group treated with the 7.5 g dose. DHT concentrations increased in parallel with testosterone concentrations at AndroGel doses of 5 g/day and 10 g/day, but the DHT/T ratio stayed within the normal range, indicating enhanced availability of the major physiologically active androgen. Serum estradiol (E2) concentrations increased significantly within 30 days of starting treatment with AndroGel 5 or 10 g/day and remained elevated throughout the treatment period but remained within the normal range for eugonadal men. Serum levels of SHBG decreased very slightly (1 to 11%) during AndroGel treatment. In men with hypergonadotropic hypogonadism, serum levels of LH and FSH fell in a dose- and time-dependent manner during treatment with AndroGel.
14.2 Phototoxicity in Humans
The phototoxic potential of AndroGel was evaluated in a double-blind, single-dose study in 27 subjects with photosensitive skin types. The Minimal Erythema Dose (MED) of ultraviolet radiation was determined for each subject. A single 24 (+1) hour application of duplicate patches containing test articles (placebo gel, testosterone gel, or saline) was made to naive skin sites on Day 1. On Day 2, each subject received five exposure times of ultraviolet radiation, each exposure being 25% greater than the previous one. Skin evaluations were made on Days 2 to 5. Exposure of test and control article application sites to ultraviolet light did not produce increased inflammation relative to non-irradiated sites, indicating no phototoxic effect.
14.3 Testosterone Transfer from Male Patients to Female Partners
The potential for dermal testosterone transfer following AndroGel use was evaluated in a clinical study between males dosed with AndroGel and their untreated female partners. Two (2) to 12 hours after AndroGel (10 g) application by the male subjects, the couples (N = 38 couples) engaged in daily, 15-minute sessions of vigorous skin-to-skin contact so that the female partners gained maximum exposure to the AndroGel application sites. Under these study conditions, all unprotected female partners had a serum testosterone concentration >2 times the baseline value at some time during the study. When a shirt covered the application site(s), the transfer of testosterone from the males to the female partners was completely prevented.
16 HOW SUPPLIED/STORAGE AND HANDLING
AndroGel is supplied in non-aerosol, metered-dose pumps. The pump is composed of plastic and stainless steel and an LDPE/aluminum foil inner liner encased in rigid plastic with a polypropylene cap. Each 88 g AndroGel Pump in the twin package is capable of dispensing 75 g or 60 metered 1.25 g doses.
AndroGel is also supplied in unit-dose aluminum foil packets in cartons of 30. Each packet of 2.5 g or 5 g gel contains 25 mg or 50 mg testosterone, respectively.
| NDC Number | Package Size |
| 54868-5814-0 | 2 x 75 g pumps (each pump dispenses 60 metered 1.25 g doses) |
| 54868-4792-0 | 30 packets (2.5 g per packet) |
| 54868-4810-0 | 30 packets (5 g per packet) |
Keep AndroGel out of the reach of children.
Storage
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Disposal
Used AndroGel pumps or used AndroGel packets should be discarded in household trash in a manner that prevents accidental application or ingestion by children or pets.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Medication Guide
17.1 Men with known or suspected prostate or breast cancer should not use AndroGel
17.2 Potential for Secondary Exposure to Testosterone and Steps to Prevent Secondary Exposure
Secondary exposure to testosterone in children and women can occur with the use of testosterone gel in men. Cases of secondary exposure to testosterone have been reported in children with signs and symptoms including enlargement of the penis or clitoris, premature development of pubic hair, increased erections, and aggressive behavior.
- Physicians should advise patients of the reported signs and symptoms of secondary exposure which may include the following:
- In children; unexpected sexual development including inappropriate enlargement of the penis or clitoris, premature development of pubic hair, increased erections, and aggressive behavior
- In women; changes in hair distribution, increase in acne, or other signs of testosterone effects
- The possibility of secondary exposure to testosterone gel should be brought to the attention of a healthcare provider
- Testosterone gel should be promptly discontinued until the cause of virilization is identified
Strict adherence to the following precautions is advised to minimize the potential for secondary exposure to testosterone from testosterone gel in men [see FDA-Approved Medication Guide] :
- Children and women should avoid contact with unwashed or unclothed application site(s) of men using testosterone gel
-
To minimize the potential for transfer to others, patients using AndroGel should apply the product as directed and strictly adhere to the following:
- Wash hands with soap and water after application
- Cover the application site(s) with clothing after the gel has dried
- Wash the application site(s) thoroughly with soap and water prior to any situation where skin-to-skin contact of the application site with another person is anticipated
- In the event that unwashed or unclothed skin to which testosterone gel has been applied comes in contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible.
17.3 Potential Side Effects with Androgens
Patients should be informed that treatment with androgens may lead to adverse reactions which include:
- Changes in urinary habits such as increased urination at night, trouble starting your urine stream, passing urine many times during the day, having an urge that you have to go to the bathroom right away, having a urine accident, being unable to pass urine and weak urine flow.
- Breathing disturbances, including those associated with sleep, or excessive daytime sleepiness.
- Too frequent or persistent erections of the penis.
- Nausea, vomiting, changes in skin color, or ankle swelling.
17.4 Patients Should Be Advised
- To read the Medication Guide before starting AndroGel therapy and to reread it each time the prescription is renewed
- Of the appropriate application and use of AndroGel to maximize the benefits and to minimize the risk of secondary exposure in children and women
- To keep AndroGel out of the reach of children
- That AndroGel is an alcohol based product and is flammable; therefore avoid fire, flame or smoking until the gel has dried
- Of the importance of adhering to all recommended monitoring
- To report any changes in their state of health, such as changes in urinary habits, breathing, sleep, and mood
- To wait 5 hours before showering or swimming. This will ensure that the greatest amount of AndroGel is absorbed into their system.
Marketed By:
Abbott Laboratories
North Chicago, IL 60064, U.S.A.
U.S. Patent No. 6,503,894
© 2011 Abbott Laboratories
53267/53268 5E Rev Nov 2011
Additional barcode label applied by:
Physicians Total Care, Inc.
Tulsa, Oklahoma 74146
FDA-Approved Medication Guide
Medication Guide
AndroGel ® (AN DROW JEL) CIII
(testosterone gel) 1%
Read the Medication Guide that comes with AndroGel before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about AndroGel?
1. Early signs and symptoms of puberty have happened in young children who were accidentally exposed to testosterone through contact with men using AndroGel.
Signs and symptoms of early puberty in a child may include:
- enlarged penis or clitoris
- early development of pubic hair
- increased erections or sex drive
- aggressive behavior
AndroGel can transfer from your body to others.
2. Women and children should avoid contact with the unwashed or unclothed area where AndroGel has been applied to your skin.
Stop using AndroGel and call your healthcare provider right away if you see any signs and symptoms in a child or a woman that may have occurred through accidental exposure to AndroGel.
Signs and symptoms of exposure to AndroGel in children may include:
- enlarged penis or clitoris
- early development of pubic hair
- increased erections or sex drive
- aggressive behavior
Signs and symptoms of exposure to AndroGel in women may include:
- changes in body hair
- a large increase in acne
To lower the risk of transfer of AndroGel from your body to others, you should follow these important instructions:
- Apply AndroGel only to areas that will be covered by a short sleeve T-shirt. These areas are your shoulders and upper arms, or stomach area (abdomen), or shoulders, upper arms and stomach area.
- Wash your hands right away with soap and water after applying AndroGel.
- After the gel has dried, cover the application area with clothing. Keep the area covered until you have washed the application area well or have showered.
- If you expect to have skin-to-skin contact with another person, first wash the application area well with soap and water.
- If a woman or child makes contact with the AndroGel application area, that area on the woman or child should be washed well with soap and water right away.
What is AndroGel?
AndroGel is a prescription medicine that contains testosterone. AndroGel is used to treat adult males who have low or no testosterone.
It is not known if AndroGel is safe or effective in children younger than 18 years old. Improper use of AndroGel may affect bone growth in children.
AndroGel is a controlled substance (CIII) because it contains testosterone that can be a target for people who abuse prescription medicines. Keep your AndroGel in a safe place to protect it. Never give your AndroGel to anyone else, even if they have the same symptoms you have. Selling or giving away this medicine may harm others and is against the law.
AndroGel is not meant for use in women.
Who should not use AndroGel?
Do not use AndroGel if you:
- have breast cancer
- have or might have prostate cancer
- are pregnant or may become pregnant or breast-feeding. AndroGel may harm your unborn or breast-feeding baby.
Women who are pregnant or who may become pregnant should avoid contact with the area of skin where AndroGel has been applied.
- are allergic to testosterone or any of the ingredients in AndroGel including soy. See the end of this Medication Guide for a complete list of ingredients in AndroGel.
Talk to your healthcare provider before taking this medicine if you have any of the above conditions.
What should I tell my healthcare provider before using AndroGel?
Before you use AndroGel, tell your healthcare provider if you:
- have breast cancer or prostate cancer
- have urinary problems due to an enlarged prostate
- have heart problems
- have liver or kidney problems
- have problems breathing while you sleep (sleep apnea)
- have any other medical conditions
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Using AndroGel with certain other medicines can affect each other.
Especially, tell your healthcare provider if you take:
- insulin
- corticosteroids
- medicines that decrease blood clotting
Ask your healthcare provider or pharmacist for a list of these medicines, if you are not sure.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I use AndroGel?
- It is important that you apply AndroGel exactly as prescribed by your healthcare provider. Your healthcare provider will tell you how much AndroGel to apply and when to apply it.
- Your healthcare provider may change your AndroGel dose. Do not change your AndroGel dose without talking to your healthcare provider.
- AndroGel is for skin use only.
- Do not allow others to apply AndroGel to your body.
- Applying AndroGel:
-
AndroGel comes in a pump or in packets. -
- Before using the pump for the first time, you will need to prime the pump. To prime AndroGel, fully push down on the pump 3 times. Do not use any AndroGel that came out while priming. Wash it down the sink or throw it in the trash to avoid accidental exposure to others. Your AndroGel pump is ready to use now.
- Your healthcare provider will tell you the number of times to press the pump for each dose.
-
- Tear open the packet completely at the dotted line.
- Squeeze all of the AndroGel out of the packet into the palm of your hand. Squeeze from the bottom of the packet to the top.
- Throw away the packet in the trash out of the reach of children to avoid accidental exposure.
-
- Squeeze the medicine into the palm of your hand and apply to clean dry, intact skin at the same time each day.
- You may also apply AndroGel from the pump or packet directly to your skin.
-
Apply AndroGel only to areas that will be covered by a short sleeve t-shirt, as shown in the shaded areas in the figure below. These areas are your shoulders and upper arms, or stomach area, or shoulders, upper arm and stomach area.
- Do not apply AndroGel to your penis or scrotum.
- Wash your hands with soap and water right after you apply AndroGel.
- Let the application areas dry for a few minutes before putting on a shirt.
- To prevent transfer of AndroGel to others, clothes (such as a t-shirt) should always be worn to cover the AndroGel application areas until you have washed the application areas well with soap and water.
- Wait 5 hours before showering or swimming. This will ensure that the greatest amount of AndroGel is absorbed into your system.
- AndroGel is flammable until dry. Let the gel dry before smoking or going near an open flame.
Your healthcare provider will test your blood before you start and while you take AndroGel.
What are the possible side effects of AndroGel?
AndroGel can cause serious side effects including:
See “What is the most important information I should know about AndroGel?”
- If you already have enlargement of your prostate gland your signs and symptoms can get worse while using AndroGel. This can include:
- increased urination at night
- trouble starting your urine stream
- having to pass urine many times during the day
- having an urge that you have to go to the bathroom right away
- having a urine accident
- being unable to pass urine or weak urine flow
- Possible increased risk of prostate cancer. Your healthcare provider should check you for prostate cancer or any other prostate problems before you start and while you use AndroGel.
- In large doses AndroGel may lower your sperm count.
- Swelling of your ankles, feet, or body, with or without heart failure.
- Enlarged or painful breasts.
- Have problems breathing while you sleep (sleep apnea).
- Blood clots in the legs. This can include pain, swelling or redness of your legs.
Call your healthcare provider right away if you have any of the serious side effects listed above.
The most common side effects of AndroGel include:
- acne
- skin irritation where AndroGel is applied
- increased cholesterol levels
- increased prostate specific antigen (a test used to screen for prostate cancer)
- increased red blood cell count
- increased liver function tests
Other side effects include more erections than are normal for you or erections that last a long time.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of AndroGel. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store AndroGel?
- Store AndroGel between 59ºF to 86ºF (15ºC to 30ºC).
- Safely throw away used AndroGel in household trash. Be careful to prevent accidental exposure of children or pets.
- Keep AndroGel away from fire.
Keep AndroGel and all medicines out of the reach of children.
General information about AndroGel
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use AndroGel for a condition for which it was not prescribed. Do not give AndroGel to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about AndroGel. If you would like more information, talk to your healthcare provider. You can ask your pharmacist or healthcare provider for information about AndroGel that is written for health professionals.
For more information, go to www.ANDROGEL.com or call 1-800-241-1643.
What are the ingredients in AndroGel?
Active ingredient: testosterone
Inactive ingredients: carbomer 980, ethyl alcohol 67.0%, isopropyl myristate, purified water and sodium hydroxide.
© 2011 Abbott Laboratories
Marketed by:
Abbott Laboratories
North Chicago, IL 60064, U.S.A.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Issued Nov 2011
NDC 54868-4792-0

CIII
AndroGel® (testosterone gel) 1%
30 Unit-dose Packets
Contains 2.5 grams per unit dose
Clear, colorless gel provides transdermal delivery of testosterone through the skin of the shoulders, upper arms, or abdomen.*
Rx Only
Dispense the enclosed Medication Guide to each patient.
* See accompanying package insert.
NDC 54868-4810-0

CIII
AndroGel® (testosterone gel 1%)
30 Unit-dose Packets
Contains 5 grams per unit dose
Clear, colorless gel provides transdermal delivery of testosterone through the skin of the shoulders, upper arms, or abdomen.*
Dispense the enclosed Medication guide to each patient.
*See accompanying package insert.
Rx Only
NDC 54868-5814-0

CIII
AndroGel® (testosterone 1% Pump
This package contains 2 multi-dose pumps. Each pump is capable of dispensing 75g doses each.
Clear, colorless gel provides transdermal delivery of testosterone through the skin of the shoulders, upper arms, or abdomen.*
Dispense the enclosed Medication Guide to each patient.
Rx Only
AndrogelTestosterone GEL
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
AndrogelTestosterone GEL
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
AndrogelTestosterone GEL
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||