Temozolomide
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Temozolomide Capsules safely and effectively. See full prescribing information for Temozolomide Capsules.Temozolomide Capsules for oral use Initial U.S. Approval: 1999INDICATIONS AND USAGETemozolomide Capsules are an alkylating drug indicated for the treatment of adult patients with: Newly diagnosed glioblastoma multiforme (GBM) concomitantly with radiotherapy and then as maintenance treatment. (1.1) Refractory anaplastic astrocytoma patients who have experienced disease progression on a drug regimen containing nitrosourea and procarbazine. (1.2) DOSAGE AND ADMINISTRATION Newly Diagnosed GBM: 75 mg/m2 for 42 days concomitant with focal radiotherapy followed by initial maintenance dose of 150 mg/m2 once daily for Days 1 to 5 of a 28 day cycle of temozolomide for 6 cycles. (2.1) Refractory Anaplastic Astrocytoma: Initial dose 150 mg/m2 once daily for 5 consecutive days per 28 day treatment cycle. (2.1) DOSAGE FORMS AND STRENGTHS 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, and 250 mg capsules. (3) CONTRAINDICATIONS Known hypersensitivity to any temozolomide capsules component or to dacarbazine (DTIC). (4.1) WARNINGS AND PRECAUTIONS Myelosuppression - monitor Absolute Neutrophil Count (ANC) and platelet count prior to dosing and throughout treatment. Geriatric patients and women have a higher risk of developing myelosuppression. (5.1) Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukemia, have been observed. (5.2) Pneumocystis carinii pneumonia (PCP) - prophylaxis required for all patients receiving concomitant temozolomide and radiotherapy for the 42 day regimen for the treatment of newly diagnosed glioblastoma multiforme. (5.3) All patients, particularly those receiving steroids, should be observed closely for the development of lymphopenia and PCP. (5.4) Complete blood counts should be obtained throughout the treatment course as specified. (5.4) Fetal harm can occur when administered to a pregnant woman. Women should be advised to avoid becoming pregnant when receiving temozolomide. (5.5) Side Effects The most common adverse reactions (≥ 10% incidence) are: alopecia, fatigue, nausea, vomiting, headache, constipation, anorexia, convulsions, rash, hemiparesis, diarrhea, asthenia, fever, dizziness, coordination abnormal, viral infection, amnesia, and insomnia. (6.1) The most common Grade 3 to 4 hematologic laboratory abnormalities (≥ 10% incidence) that have developed during treatment with temozolomide are: lymphopenia, thrombocytopenia, neutropenia, and leukopenia. (6.1) Allergic reactions have also been reported. (6) To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537 or drug.safety@tevapharm.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Valproic acid: decreases oral clearance of temozolomide. (7.1) USE IN SPECIFIC POPULATIONS Nursing mothers: Not recommended. (8.3) Pediatric use: No established use. (8.4) Hepatic/Renal Impairment: Caution should be exercised when temozolomide is administered to patients with severe renal or hepatic impairment. (8.6, 8.7)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 TEMOZOLOMIDE INDICATIONS AND USAGE
- 2 TEMOZOLOMIDE DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 TEMOZOLOMIDE CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 TEMOZOLOMIDE ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 TEMOZOLOMIDE DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- Principal Display Panel
- Principal Display Panel
- Principal Display Panel
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Newly Diagnosed Glioblastoma Multiforme
Temozolomide Capsules are indicated for the treatment of adult patients with newly diagnosed glioblastoma multiforme concomitantly with radiotherapy and then as maintenance treatment.
1.2 Refractory Anaplastic Astrocytoma
Temozolomide Capsules are indicated for the treatment of adult patients with refractory anaplastic astrocytoma, i.e., patients who have experienced disease progression on a drug regimen containing nitrosourea and procarbazine.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing and Dose Modification Guidelines
Dosage of temozolomide must be adjusted according to nadir neutrophil and platelet counts in the previous cycle and the neutrophil and platelet counts at the time of initiating the next cycle. For temozolomide dosage calculations based on body surface area (BSA) see Table 5. For suggested capsule combinations on a daily dose see Table 6.
Patients with Newly Diagnosed High Grade Glioma
Concomitant Phase
Temozolomide is administered at 75 mg/m2 daily for 42 days concomitant with focal radiotherapy (60 Gy administered in 30 fractions) followed by maintenance temozolomide for 6 cycles. Focal RT includes the tumor bed or resection site with a 2 to 3 cm margin. No dose reductions are recommended during the concomitant phase; however, dose interruptions or discontinuation may occur based on toxicity. The temozolomide dose should be continued throughout the 42 day concomitant period up to 49 days if all of the following conditions are met: absolute neutrophil count greater than or equal to 1.5 x 109/L, platelet count greater than or equal to 100 x 109/L, common toxicity criteria (CTC) nonhematological toxicity less than or equal to Grade 1 (except for alopecia, nausea, and vomiting). During treatment a complete blood count should be obtained weekly. Temozolomide dosing should be interrupted or discontinued during concomitant phase according to the hematological and nonhematological toxicity criteria as noted in Table 1. Pneumocystis carinii pneumonia (PCP) prophylaxis is required during the concomitant administration of temozolomide and radiotherapy, and should be continued in patients who develop lymphocytopenia until recovery from lymphocytopenia (CTC Grade less than or equal to 1).
| TMZ = temozolomide; CTC = Common Toxicity Criteria. | ||
| Toxicity |
TMZ Interruption |
TMZ Discontinuation |
| Absolute Neutrophil Count | greater than or equal to 0.5 and less than 1.5 x 109/L |
less than 0.5 x 109/L |
| Platelet Count | greater than or equal to 10 and less than 100 x 109/L |
less than 10 x 109/L |
| CTC Nonhematological Toxicity (except for alopecia, nausea, vomiting) |
CTC Grade 2 |
CTC Grade 3 or 4 |
Maintenance Phase
Cycle 1
Four weeks after completing the temozolomide + RT phase, temozolomide is administered for an additional 6 cycles of maintenance treatment. Dosage in Cycle 1 (maintenance) is 150 mg/m2 once daily for 5 days followed by 23 days without treatment.
Cycles 2 to 6
At the start of Cycle 2, the dose can be escalated to 200 mg/m2, if the CTC nonhematologic toxicity for Cycle 1 is Grade less than or equal to 2 (except for alopecia, nausea, and vomiting), absolute neutrophil count (ANC) is greater than or equal to 1.5 x 109/L, and the platelet count is greater than or equal to 100 x 109/L. The dose remains at 200 mg/m2 per day for the first 5 days of each subsequent cycle except if toxicity occurs. If the dose was not escalated at Cycle 2, escalation should not be done in subsequent cycles.
Dose Reduction or Discontinuation During Maintenance
Dose reductions during the maintenance phase should be applied according to Tables 2 and 3.
During treatment, a complete blood count should be obtained on Day 22 (21 days after the first dose of temozolomide) or within 48 hours of that day, and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). The next cycle of temozolomide should not be started until the ANC and platelet count exceed these levels. Dose reductions during the next cycle should be based on the lowest blood counts and worst nonhematologic toxicity during the previous cycle. Dose reductions or discontinuations during the maintenance phase should be applied according to Tables 2 and 3.
| Dose Level | Dose (mg/m2/day) | Remarks |
| -1 | 100 | Reduction for prior toxicity |
| 0 | 150 | Dose during Cycle 1 |
| 1 | 200 | Dose during Cycles 2 to 6 in absence of toxicity |
| TMZ = temozolomide; CTC = Common Toxicity Criteria. | ||
| Toxicity |
Reduce TMZ by 1 Dose Level |
Discontinue TMZ |
| Absolute Neutrophil Count | less than 1 x 109/L | See footnote |
| Platelet Count | less than 50 x 109/L | See footnote |
| CTC Nonhematological Toxicity (except for alopecia, nausea, vomiting) |
CTC Grade 3 |
CTC Grade 4  |
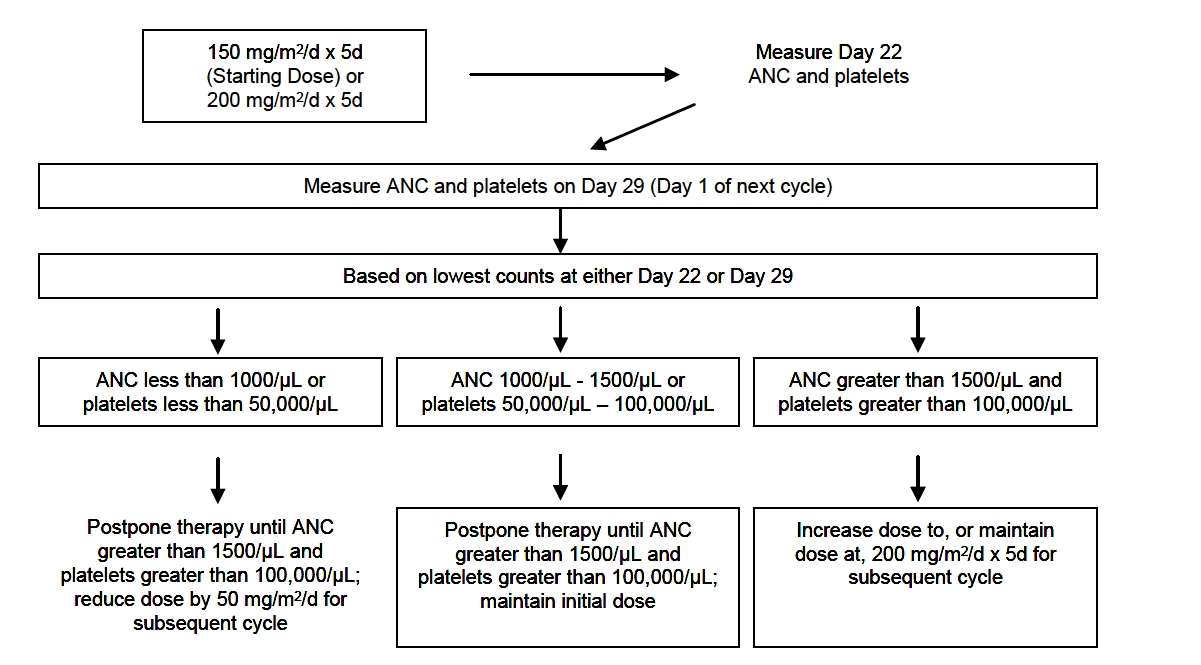
Patients with Refractory Anaplastic Astrocytoma
For adults the initial dose is 150 mg/m2 once daily for 5 consecutive days per 28 day treatment cycle. For adult patients, if both the nadir and day of dosing (Day 29, Day 1 of next cycle) ANC are greater than or equal to 1.5 x 109/L (1500/μL) and both the nadir and Day 29, Day 1 of next cycle platelet counts are greater than or equal to 100 x 109/L (100,000/μL), the temozolomide dose may be increased to 200 mg/m2/day for 5 consecutive days per 28 day treatment cycle. During treatment, a complete blood count should be obtained on Day 22 (21 days after the first dose) or within 48 hours of that day, and weekly until the ANC is above 1.5 x 109/L (1500/μL) and the platelet count exceeds 100 x 109/L (100,000/μL). The next cycle of temozolomide should not be started until the ANC and platelet count exceed these levels. If the ANC falls to less than 1 x 109/L (1000/μL) or the platelet count is less than 50 x 109/L (50,000/μL) during any cycle, the next cycle should be reduced by 50 mg/m2, but not below 100 mg/m2, the lowest recommended dose (see Table 4). Temozolomide therapy can be continued until disease progression. In the clinical trial, treatment could be continued for a maximum of 2 years, but the optimum duration of therapy is not known.
|
Total BSA (m2) |
75 mg/m2 (mg daily) |
150 mg/m2 (mg daily) |
200 mg/m2 (mg daily) |
| 1 | 75 | 150 | 200 |
| 1.1 | 82.5 | 165 | 220 |
| 1.2 | 90 | 180 | 240 |
| 1.3 | 97.5 | 195 | 260 |
| 1.4 | 105 | 210 | 280 |
| 1.5 | 112.5 | 225 | 300 |
| 1.6 | 120 | 240 | 320 |
| 1.7 | 127.5 | 255 | 340 |
| 1.8 | 135 | 270 | 360 |
| 1.9 | 142.5 | 285 | 380 |
| 2 | 150 | 300 | 400 |
| 2.1 | 157.5 | 315 | 420 |
| 2.2 | 165 | 330 | 440 |
| 2.3 | 172.5 | 345 | 460 |
| 2.4 | 180 | 360 | 480 |
| 2.5 | 187.5 | 375 | 500 |
| Number of Daily Capsules by Strength (mg) | ||||||
| Total Daily Dose (mg) | 250 mg | 180 mg | 140 mg | 100 mg | 20 mg | 5 mg |
| 75 | 0 | 0 | 0 | 0 | 3 | 3 |
| 82.5 | 0 | 0 | 0 | 0 | 4 | 0 |
| 90 | 0 | 0 | 0 | 0 | 4 | 2 |
| 97.5 | 0 | 0 | 0 | 1 | 0 | 0 |
| 105 | 0 | 0 | 0 | 1 | 0 | 1 |
| 112.5 | 0 | 0 | 0 | 1 | 0 | 2 |
| 120 | 0 | 0 | 0 | 1 | 1 | 0 |
| 127.5 | 0 | 0 | 0 | 1 | 1 | 1 |
| 135 | 0 | 0 | 0 | 1 | 1 | 3 |
| 142.5 | 0 | 0 | 1 | 0 | 0 | 0 |
| 150 | 0 | 0 | 1 | 0 | 0 | 2 |
| 157.5 | 0 | 0 | 1 | 0 | 1 | 0 |
| 165 | 0 | 0 | 1 | 0 | 1 | 1 |
| 172.5 | 0 | 0 | 1 | 0 | 1 | 2 |
| 180 | 0 | 1 | 0 | 0 | 0 | 0 |
| 187.5 | 0 | 1 | 0 | 0 | 0 | 1 |
| 195 | 0 | 1 | 0 | 0 | 0 | 3 |
| 200 | 0 | 1 | 0 | 0 | 1 | 0 |
| 210 | 0 | 0 | 0 | 2 | 0 | 2 |
| 220 | 0 | 0 | 0 | 2 | 1 | 0 |
| 225 | 0 | 0 | 0 | 2 | 1 | 1 |
| 240 | 0 | 0 | 1 | 1 | 0 | 0 |
| 255 | 1 | 0 | 0 | 0 | 0 | 1 |
| 260 | 1 | 0 | 0 | 0 | 0 | 2 |
| 270 | 1 | 0 | 0 | 0 | 1 | 0 |
| 280 | 0 | 0 | 2 | 0 | 0 | 0 |
| 285 | 0 | 0 | 2 | 0 | 0 | 1 |
| 300 | 0 | 0 | 0 | 3 | 0 | 0 |
| 315 | 0 | 0 | 0 | 3 | 0 | 3 |
| 320 | 0 | 1 | 1 | 0 | 0 | 0 |
| 330 | 0 | 1 | 1 | 0 | 0 | 2 |
| 340 | 0 | 1 | 1 | 0 | 1 | 0 |
| 345 | 0 | 1 | 1 | 0 | 1 | 1 |
| 360 | 0 | 2 | 0 | 0 | 0 | 0 |
| 375 | 0 | 2 | 0 | 0 | 0 | 3 |
| 380 | 0 | 1 | 0 | 2 | 0 | 0 |
| 400 | 0 | 0 | 0 | 4 | 0 | 0 |
| 420 | 0 | 0 | 3 | 0 | 0 | 0 |
| 440 | 0 | 0 | 3 | 0 | 1 | 0 |
| 460 | 0 | 2 | 0 | 1 | 0 | 0 |
| 480 | 0 | 1 | 0 | 3 | 0 | 0 |
| 500 | 2 | 0 | 0 | 0 | 0 | 0 |
2.2 Preparation and Administration
Temozolomide Capsules
In clinical trials, temozolomide was administered under both fasting and nonfasting conditions; however, absorption is affected by food [see Clinical Pharmacology (12.3)], and consistency of administration with respect to food is recommended. There are no dietary restrictions with temozolomide. To reduce nausea and vomiting, temozolomide should be taken on an empty stomach. Bedtime administration may be advised. Antiemetic therapy may be administered prior to and/or following administration of temozolomide.
Temozolomide Capsules should not be opened or chewed. They should be swallowed whole with a glass of water. If capsules are accidentally opened or damaged, precautions should be taken to avoid inhalation or contact with the skin or mucous membranes [see How Supplied/Storage and Handling (16.1)].
3 DOSAGE FORMS AND STRENGTHS
- Temozolomide Capsules for oral administration
| 5 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with white to off-white powder. Imprinted in green ink stylized barr over 5 mg on one piece and 1078 on the other piece. |
| 20 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with white to off-white powder. Imprinted in brown ink stylized barr over 20 mg on one piece and 1077 on the other piece. |
| 100 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in blue ink stylized barr over 100 mg on one piece and 1076 on the other piece. |
| 140 mg: |
Two-piece hard gelatin capsule with blue opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 140 mg on one piece and 1159 on the other piece. |
| 180 mg: |
Two-piece hard gelatin capsule with dark orange opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 180 mg on one piece and 1160 on the other piece. |
| 250 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 250 mg on one piece and 1075 on the other piece. |
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Temozolomide is contraindicated in patients who have a history of hypersensitivity reaction (such as urticaria, allergic reaction including anaphylaxis, toxic epidermal necrolysis, and Stevens-Johnson syndrome) to any of its components. Temozolomide is also contraindicated in patients who have a history of hypersensitivity to dacarbazine (DTIC), since both drugs are metabolized to 5-(3-methyltriazen-1-yl)-imidazole-4-carboxamide (MTIC).
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
Patients treated with temozolomide may experience myelosuppression, including prolonged pancytopenia, which may result in aplastic anemia, which in some cases has resulted in a fatal outcome. In some cases, exposure to concomitant medications associated with aplastic anemia, including carbamazepine, phenytoin, and sulfamethoxazole/trimethoprim, complicates assessment. Prior to dosing, patients must have an absolute neutrophil count (ANC) ≥ 1.5 x 109/L and a platelet count ≥ 100 x 109/L. A complete blood count should be obtained on Day 22 (21 days after the first dose) or within 48 hours of that day, and weekly until the ANC is above 1.5 x 109/L and platelet count exceeds 100 x 109/L. Geriatric patients and women have been shown in clinical trials to have a higher risk of developing myelosuppression.
5.2 Myelodysplastic Syndrome
Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukemia, have been observed.
5.3 Pneumonia
For treatment of newly diagnosed glioblastoma multiforme: Prophylaxis against Pneumocystis carinii pneumonia (PCP) is required for all patients receiving concomitant temozolomide and radiotherapy for the 42 day regimen.
There may be a higher occurrence of PCP when temozolomide is administered during a longer dosing regimen. However, all patients receiving temozolomide, particularly patients receiving steroids, should be observed closely for the development of PCP regardless of the regimen.
5.4 Laboratory Tests
For the concomitant treatment phase with RT, a complete blood count should be obtained prior to initiation of treatment and weekly during treatment.
For the 28 day treatment cycles, a complete blood count should be obtained prior to treatment on Day 1 and on Day 22 (21 days after the first dose) of each cycle. Blood counts should be performed weekly until recovery if the ANC falls below 1.5 x 109/L and the platelet count falls below 100 x 109/L [ see Recommended Dosing and Dose Modification Guidelines (2.1) ].
5.5 Use in Pregnancy
Temozolomide can cause fetal harm when administered to a pregnant woman. Administration of temozolomide to rats and rabbits during organogenesis at 0.38 and 0.75 times the maximum recommended human dose (75 and 150 mg/m2), respectively, caused numerous fetal malformations of the external organs, soft tissues, and skeleton in both species [ see Use in Specific Populations (8.1) ].
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Newly Diagnosed Glioblastoma Multiforme
During the concomitant phase (temozolomide + radiotherapy), adverse reactions including thrombocytopenia, nausea, vomiting, anorexia, and constipation were more frequent in the temozolomide + RT arm. The incidence of other adverse reactions was comparable in the two arms. The most common adverse reactions across the cumulative temozolomide experience were alopecia, nausea, vomiting, anorexia, headache, and constipation (see Table 7). Forty-nine percent (49%) of patients treated with temozolomide reported one or more severe or life-threatening reactions, most commonly fatigue (13%), convulsions (6%), headache (5%), and thrombocytopenia (5%). Overall, the pattern of reactions during the maintenance phase was consistent with the known safety profile of temozolomide.
| RT + TMZ = radiotherapy plus temozolomide; NOS = not otherwise specified.
Note: Grade 5 (fatal) adverse reactions are included in the Grade ≥ 3 column. |
||||||
|
Concomitant Phase RT Alone (n = 285) |
Concomitant Phase RT + TMZ (n = 288) |
Maintenance Phase TMZ (n = 224) |
||||
| All | Grade ≥3 | All | Grade ≥3 | All | Grade ≥3 | |
| Subjects Reporting any Adverse Reaction | 258 (91) | 74 (26) | 266 (92) | 80 (28) | 206 (92) | 82 (37) |
| Body as a Whole – General Disorders | ||||||
| Anorexia | 25 (9) | 1 (< 1) | 56 (19) | 2 (1) | 61 (27) | 3 (1) |
| Dizziness | 10 (4) | 0 | 12 (4) | 2 (1) | 12 (5) | 0 |
| Fatigue | 139 (49) | 15 (5) | 156 (54) | 19 (7) | 137 (61) | 20 (9) |
| Headache | 49 (17) | 11 (4) | 56 (19) | 5 (2) | 51 (23) | 9 (4) |
| Weakness | 9 (3) | 3 (1) | 10 (3) | 5 (2) | 16 (7) | 4 (2) |
| Central and Peripheral Nervous System Disorders | ||||||
| Confusion | 12 (4) | 6 (2) | 11 (4) | 4 (1) | 12 (5) | 4 (2) |
| Convulsions | 20 (7) | 9 (3) | 17 (6) | 10 (3) | 25 (11) | 7 (3) |
| Memory Impairment | 12 (4) | 1 (< 1) | 8 (3) | 1 (< 1) | 16 (7) | 2 (1) |
| Disorders of the Eye | ||||||
| Vision Blurred | 25 (9) | 4 (1) | 26 (9) | 2 (1) | 17 (8) | 0 |
| Disorders of the Immune System | ||||||
| Allergic Reaction | 7 (2) | 1 (< 1) | 13 (5) | 0 | 6 (3) | 0 |
| Gastrointestinal System Disorders | ||||||
| Abdominal Pain | 2 (1) | 0 | 7 (2) | 1 (<1) | 11 (5) | 1 (<1) |
| Constipation | 18 (6) | 0 | 53 (18) | 3 (1) | 49 (22) | 0 |
| Diarrhea | 9 (3) | 0 | 18 (6) | 0 | 23 (10) | 2 (1) |
| Nausea | 45 (16) | 1 (< 1) | 105 (36) | 2 (1) | 110 (49) | 3 (1) |
| Stomatitis | 14 (5) | 1 (< 1) | 19 (7) | 0 | 20 (9) | 3 (1) |
| Vomiting | 16 (6) | 1 (< 1) | 57 (20) | 1 (< 1) | 66 (29) | 4 (2) |
| Injury and Poisoning | ||||||
| Radiation Injury NOS | 11 (4) | 1 (< 1) | 20 (7) | 0 | 5 (2) | 0 |
| Musculoskeletal System Disorders | ||||||
| Arthralgia | 2 (1) | 0 | 7 (2) | 1 (<1) | 14 (6) | 0 |
| Platelet, Bleeding and Clotting Disorders | ||||||
| Thrombocytopenia | 3 (1) | 0 | 11 (4) | 8 (3) | 19 (8) | 8 (4) |
| Psychiatric Disorders | ||||||
| Insomnia | 9 (3) | 1 (<1) | 14 (5) | 0 | 9 (4) | 0 |
| Respiratory System Disorders | ||||||
| Coughing | 3 (1) | 0 | 15 (5) | 2 (1) | 19 (8) | 1 (<1) |
| Dyspnea | 9 (3) | 4 (1) | 11 (4) | 5 (2) | 12 (5) | 1 (<1) |
| Skin and Subcutaneous Tissue Disorders | ||||||
| Alopecia | 179 (63) | 0 | 199 (69) | 0 | 124 (55) | 0 |
| Dry Skin | 6 (2) | 0 | 7 (2) | 0 | 11 (5) | 1 (<1) |
| Erythema | 15 (5) | 0 | 14 (5) | 0 | 2 (1) | 0 |
| Pruritus | 4 (1) | 0 | 11 (4) | 0 | 11 (5) | 0 |
| Rash | 42 (15) | 0 | 56 (19) | 3 (1) | 29 (13) | 3 (1) |
| Special Senses Other, Disorders | ||||||
| Taste Perversion | 6 (2) | 0 | 18 (6) | 0 | 11 (5) | 0 |
Myelosuppression (neutropenia and thrombocytopenia), which is a known dose-limiting toxicity for most cytotoxic agents, including temozolomide, was observed. When laboratory abnormalities and adverse reactions were combined, Grade 3 or Grade 4 neutrophil abnormalities including neutropenic reactions were observed in 8% of the patients, and Grade 3 or Grade 4 platelet abnormalities, including thrombocytopenic reactions, were observed in 14% of the patients treated with temozolomide.
Refractory Anaplastic Astrocytoma
Tables 8 and 9 show the incidence of adverse reactions in the 158 patients in the anaplastic astrocytoma study for whom data are available. In the absence of a control group, it is not clear in many cases whether these reactions should be attributed to temozolomide or the patients' underlying conditions, but nausea, vomiting, fatigue, and hematologic effects appear to be clearly drug-related. The most frequently occurring adverse reactions were nausea, vomiting, headache, and fatigue. The adverse reactions were usually NCI Common Toxicity Criteria (CTC) Grade 1 or 2 (mild to moderate in severity) and were self-limiting, with nausea and vomiting readily controlled with antiemetics. The incidence of severe nausea and vomiting (CTC Grade 3 or 4) was 10% and 6%, respectively. Myelosuppression (thrombocytopenia and neutropenia) was the dose-limiting adverse reaction. It usually occurred within the first few cycles of therapy and was not cumulative.
Myelosuppression occurred late in the treatment cycle and returned to normal, on average, within 14 days of nadir counts. The median nadirs occurred at 26 days for platelets (range: 21 to 40 days) and 28 days for neutrophils (range: 1 to 44 days). Only 14% (22/158) of patients had a neutrophil nadir and 20% (32/158) of patients had a platelet nadir, which may have delayed the start of the next cycle. Less than 10% of patients required hospitalization, blood transfusion, or discontinuation of therapy due to myelosuppression.
In clinical trial experience with 110 to 111 women and 169 to 174 men (depending on measurements), there were higher rates of Grade 4 neutropenia (ANC < 500 cells/μL) and thrombocytopenia (< 20,000 cells/μL) in women than men in the first cycle of therapy (12% vs. 5% and 9% vs. 3%, respectively).
In the entire safety database for which hematologic data exist (N = 932), 7% (4/61) and 9.5% (6/63) of patients over age 70 experienced Grade 4 neutropenia or thrombocytopenia in the first cycle, respectively. For patients less than or equal to age 70, 7% (62/871) and 5.5% (48/879) experienced Grade 4 neutropenia or thrombocytopenia in the first cycle, respectively. Pancytopenia, leukopenia, and anemia have also been reported.
| No. (%) of Temozolomide Patients (N = 158) | ||
| All Reactions | Grade 3/4 | |
| Any Adverse Reaction | 153 (97) | 79 (50) |
| Body as a Whole | ||
| Headache | 65 (41) | 10 (6) |
| Fatigue | 54 (34) | 7 (4) |
| Asthenia | 20 (13) | 9 (6) |
| Fever | 21 (13) | 3 (2) |
| Back pain | 12 (8) | 4 (3) |
| Cardiovascular | ||
| Edema peripheral | 17 (11) | 1 (1) |
| Central and Peripheral Nervous System | ||
| Convulsions | 36 (23) | 8 (5) |
| Hemiparesis | 29 (18) | 10 (6) |
| Dizziness | 19 (12) | 1 (1) |
| Coordination abnormal | 17 (11) | 2 (1) |
| Amnesia | 16 (10) | 6 (4) |
| Insomnia | 16 (10) | 0 |
| Paresthesia | 15 (9) | 1 (1) |
| Somnolence | 15 (9) | 5 (3) |
| Paresis | 13 (8) | 4 (3) |
| Urinary incontinence | 13 (8) | 3 (2) |
| Ataxia | 12 (8) | 3 (2) |
| Dysphasia | 11 (7) | 1 (1) |
| Convulsions local | 9 (6) | 0 |
| Gait abnormal | 9 (6) | 1 (1) |
| Confusion | 8 (5) | 0 |
| Endocrine | ||
| Adrenal hypercorticism | 13 (8) | 0 |
| Gastrointestinal System | ||
| Nausea | 84 (53) | 16 (10) |
| Vomiting | 66 (42) | 10 (6) |
| Constipation | 52 (33) | 1 (1) |
| Diarrhea | 25 (16) | 3 (2) |
| Abdominal pain | 14 (9) | 2 (1) |
| Anorexia | 14 (9) | 1 (1) |
| Metabolic | ||
| Weight increase | 8 (5) | 0 |
| Musculoskeletal System | ||
| Myalgia | 8 (5) | |
| Psychiatric Disorders | ||
| Anxiety | 11 (7) | 1 (1) |
| Depression | 10 (6) | 0 |
| Reproductive Disorders | ||
| Breast pain, female | 4 (6) | |
| Resistance Mechanism Disorders | ||
| Infection viral | 17 (11) | 0 |
| Respiratory System | ||
| Upper respiratory tract infection | 13 (8) | 0 |
| Pharyngitis | 12 (8) | 0 |
| Sinusitis | 10 (6) | 0 |
| Coughing | 8 (5) | 0 |
| Skin and Appendages | ||
| Rash | 13 (8) | 0 |
| Pruritus | 12 (8) | 2 (1) |
| Urinary System | ||
| Urinary tract infection | 12 (8) | 0 |
| Micturition increased frequency | 9 (6) | 0 |
| Vision | ||
| Diplopia | 8 (5) | 0 |
Vision abnormal |
8 (5) | |
Temozolomide |
|
| Hemoglobin | 7/158 (4%) |
| Lymphopenia | 83/152 (55%) |
| Neutrophils | 20/142 (14%) |
| Platelets | 29/156 (19%) |
| WBC | 18/158 (11%) |
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of temozolomide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the drug exposure.
Temozolomide Capsules: allergic reactions, including anaphylaxis, have been reported. Erythema multiforme has been reported, which resolved after discontinuation of temozolomide and, in some cases, recurred upon rechallenge. Cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported.
There have been reported cases of hepatotoxicity, including elevations of liver enzymes, hyperbilirubinemia, cholestasis, and hepatitis.
Opportunistic infections including Pneumocystis carinii pneumonia (PCP) have also been reported. Cases of interstitial pneumonitis/pneumonitis, alveolitis, and pulmonary fibrosis have been reported. Prolonged pancytopenia, which may result in aplastic anemia, has been reported, and in some cases has resulted in a fatal outcome.
7 DRUG INTERACTIONS
7.1 Valproic Acid
Administration of valproic acid decreases oral clearance of temozolomide by about 5%. The clinical implication of this effect is not known [ see Clinical Pharmacology (12.3) ].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category D
See Warnings and Precautions section.
Temozolomide can cause fetal harm when administered to a pregnant woman. Five consecutive days of oral temozolomide administration of 0.38 and 0.75 times the highest recommended human dose (75 and 150 mg/m2) in rats and rabbits, respectively, during the period of organogenesis caused numerous malformations of the external and internal soft tissues and skeleton in both species. Doses equivalent to 0.75 times the highest recommended human dose (150 mg/m2) caused embryolethality in rats and rabbits as indicated by increased resorptions. There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus. Women of childbearing potential should be advised to avoid becoming pregnant during therapy with temozolomide.
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants and tumorigenicity shown for temozolomide in animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of temozolomide to the mother.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Temozolomide capsules have been studied in 2 open-label studies in pediatric patients (aged 3-18 years) at a dose of 160 to 200 mg/m2 daily for 5 days every 28 days. In one trial, 29 patients with recurrent brain stem glioma and 34 patients with recurrent high grade astrocytoma were enrolled. All patients had recurrence following surgery and radiation therapy, while 31% also had disease progression following chemotherapy. In a second study conducted by the Children's Oncology Group (COG), 122 patients were enrolled, including patients with medulloblastoma/PNET (29), high grade astrocytoma (23), low grade astrocytoma (22), brain stem glioma (16), ependymoma (14), other CNS tumors (9), and non-CNS tumors (9). The temozolomide toxicity profile in pediatric patients is similar to adults. Table 10 shows the adverse reactions in 122 children in the COG study.
|
No. (%) of Temozolomide Patients (N = 122)  |
||
|
Body System/Organ Class Adverse Reaction |
All Reactions | Grade 3/4 |
| Subjects Reporting an AE | 107 (88) | 69 (57) |
| Body as a Whole | ||
| Central and Peripheral Nervous System | ||
| Central cerebral CNS cortex | 22 (18) | 13 (11) |
| Gastrointestinal System | ||
| Nausea | 56 (46) | 5 (4) |
| Vomiting | 62 (51) | 4 (3) |
| Platelet, Bleeding and Clotting | ||
| Thrombocytopenia | 71 (58) | 31 (25) |
| Red Blood Cell Disorders | ||
| Decreased Hemoglobin | 62 (51) | 7 (6) |
| White Cell and RES Disorders | ||
| Decreased WBC | 71 (58) | 21 (17) |
| Lymphopenia | 73 (60) | 48 (39) |
| Neutropenia | 62 (51) | 24 (20) |
8.5 Geriatric Use
Clinical studies of temozolomide did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
In the anaplastic astrocytoma study population, patients 70 years of age or older had a higher incidence of Grade 4 neutropenia and Grade 4 thrombocytopenia (2/8; 25%, P = 0.31 and 2/10; 20%, P = 0.09, respectively) in the first cycle of therapy than patients under 70 years of age [ see Warnings and Precautions (5) and Adverse Reactions (6.1) ].
In newly diagnosed patients with glioblastoma multiforme, the adverse reaction profile was similar in younger patients (< 65 years) vs. older (≥ 65 years).
8.6 Renal Impairment
Caution should be exercised when temozolomide is administered to patients with severe renal impairment [ see Clinical Pharmacology (12.3) ].
8.7 Hepatic Impairment
Caution should be exercised when temozolomide is administered to patients with severe hepatic impairment [ see Clinical Pharmacology ( 12.3 ) ].
10 OVERDOSAGE
Doses of 500, 750, 1000, and 1250 mg/m2 (total dose per cycle over 5 days) have been evaluated clinically in patients. Dose-limiting toxicity was hematologic and was reported with any dose but is expected to be more severe at higher doses. An overdose of 2000 mg per day for 5 days was taken by one patient and the adverse reactions reported were pancytopenia, pyrexia, multi-organ failure, and death. There are reports of patients who have taken more than 5 days of treatment (up to 64 days), with adverse reactions reported including bone marrow suppression, which in some cases was severe and prolonged, and infections and resulted in death. In the event of an overdose, hematologic evaluation is needed. Supportive measures should be provided as necessary.
11 DESCRIPTION
Temozolomide Capsules for oral administration contain temozolomide, an imidazotetrazine derivative. The chemical name of temozolomide is 3,4-dihydro-3-methyl-4-oxoimidazo[5,1-d]-as-tetrazine-8-carboxamide. The structural formula is:
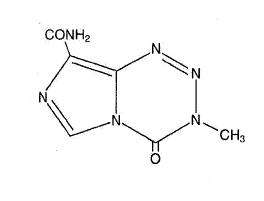
The material is a white to light tan/light pink powder. The molecule is stable at acidic pH (< 5) and labile at pH >7; hence temozolomide can be administered orally. The prodrug, temozolomide, is rapidly hydrolyzed to the active 5-(3-methyltriazen-1-yl) imidazole-4-carboxamide (MTIC) at neutral and alkaline pH values, with hydrolysis taking place even faster at alkaline pH.
Each capsule contains either 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, or 250 mg of temozolomide. The inactive ingredients for Temozolomide Capsules are anhydrous lactose, colloidal silicon dioxide, povidone, sodium starch glycolate, stearic acid, and tartaric acid. The 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, and 250 mg capsule shells contain D&C yellow no. 10, FD&C red no. 40, FD&C yellow no. 6, gelatin, and titanium dioxide. The 140 mg capsule shell also contains D&C red no. 28, FD&C blue no. 1, and FD&C green no. 3. The 180 mg capsule shell also contains FD&C blue no. 1. The 5 mg imprinting ink contains ammonium hydroxide, black iron oxide, D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, propylene glycol, and shellac. The 20 mg imprinting ink contains ammonium hydroxide, black iron oxide, propylene glycol, red iron oxide, shellac, and yellow iron oxide. The 100 mg imprinting ink contains FD&C blue no. 1 aluminum lake, polyvinylpyrrolidone, propylene glycol, shellac, sodium hydroxide, and titanium dioxide. The 140 mg, 180 mg, and 250 mg imprinting ink contains black iron oxide, D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, FD&C blue no. 2 aluminum lake, FD&C red no. 40 aluminum lake, propylene glycol, and shellac.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Temozolomide is not directly active but undergoes rapid nonenzymatic conversion at physiologic pH to the reactive compound 5-(3-methyltriazen-1-yl)-imidazole-4-carboxamide (MTIC). The cytotoxicity of MTIC is thought to be primarily due to alkylation of DNA. Alkylation (methylation) occurs mainly at the O6 and N7 positions of guanine.
12.3 Pharmacokinetics
Absorption
Temozolomide is rapidly and completely absorbed after oral administration with a peak plasma concentration (Cmax) achieved in a median Tmax of 1 hour. Food reduces the rate and extent of temozolomide absorption. Mean peak plasma concentration and AUC decreased by 32% and 9%, respectively, and median Tmax increased by 2-fold (from 1-2.25 hours) when temozolomide was administered after a modified high-fat breakfast.
A pharmacokinetic study comparing oral and intravenous temozolomide in 19 patients with primary CNS malignancies showed that 150 mg/m2 temozolomide for injection administered over 90 minutes is bioequivalent to 150 mg/m2 temozolomide oral capsules with respect to both Cmax and AUC of temozolomide and MTIC. Following a single 90-minute intravenous infusion of 150 mg/m2, the geometric mean Cmax values for temozolomide and MTIC were 7.3 mcg/mL and 276 ng/mL, respectively. Following a single oral dose of 150 mg/m2, the geometric mean Cmax values for temozolomide and MTIC were 7.5 mcg/mL and 282 ng/mL, respectively. Following a single 90-minute intravenous infusion of 150 mg/m2, the geometric mean AUC values for temozolomide and MTIC were 24.6 mcg•hr/mL and 891 ng•hr/mL, respectively. Following a single oral dose of 150 mg/m2, the geometric mean AUC values for temozolomide and MTIC were 23.4 mcg•hr/mL and 864 ng•hr/mL, respectively.
Distribution
Temozolomide has a mean apparent volume of distribution of 0.4 L/kg (%CV = 13%). It is weakly bound to human plasma proteins; the mean percent bound of drug-related total radioactivity is 15%.
Metabolism and Elimination
Temozolomide is spontaneously hydrolyzed at physiologic pH to the active species, MTIC and to temozolomide acid metabolite. MTIC is further hydrolyzed to 5-amino-imidazole-4-carboxamide (AIC), which is known to be an intermediate in purine and nucleic acid biosynthesis, and to methylhydrazine, which is believed to be the active alkylating species. Cytochrome P450 enzymes play only a minor role in the metabolism of temozolomide and MTIC. Relative to the AUC of temozolomide, the exposure to MTIC and AIC is 2.4% and 23%, respectively.
Excretion
About 38% of the administered temozolomide total radioactive dose is recovered over 7 days: 37.7% in urine and 0.8% in feces. The majority of the recovery of radioactivity in urine is unchanged temozolomide (5.6%), AIC (12%), temozolomide acid metabolite (2.3%), and unidentified polar metabolite(s) (17%). Overall clearance of temozolomide is about 5.5 L/hr/m2. Temozolomide is rapidly eliminated, with a mean elimination half-life of 1.8 hours, and exhibits linear kinetics over the therapeutic dosing range of 75 to 250 mg/m2/day.
Effect of Age
A population pharmacokinetic analysis indicated that age (range: 19-78 years) has no influence on the pharmacokinetics of temozolomide.
Effect of Gender
A population pharmacokinetic analysis indicated that women have an approximately 5% lower clearance (adjusted for body surface area) for temozolomide than men.
Effect of Race
The effect of race on the pharmacokinetics of temozolomide has not been studied.
Tobacco Use
A population pharmacokinetic analysis indicated that the oral clearance of temozolomide is similar in smokers and nonsmokers.
Effect of Renal Impairment
A population pharmacokinetic analysis indicated that creatinine clearance over the range of 36 to 130 mL/min/m2 has no effect on the clearance of temozolomide after oral administration. The pharmacokinetics of temozolomide have not been studied in patients with severely impaired renal function (CLcr <36 mL/min/m2). Caution should be exercised when temozolomide is administered to patients with severe renal impairment [see Use in Specific Populations (8.6)]. Temozolomide has not been studied in patients on dialysis.
Effect of Hepatic Impairment
A study showed that the pharmacokinetics of temozolomide in patients with mild-to-moderate hepatic impairment (Child-Pugh Class I - II) were similar to those observed in patients with normal hepatic function. Caution should be exercised when temozolomide is administered to patients with severe hepatic impairment [see Use in Specific Populations (8.7) ].
Effect of Other Drugs on Temozolomide Pharmacokinetics
In a multiple-dose study, administration of temozolomide capsules with ranitidine did not change the Cmax or AUC values for temozolomide or MTIC.
A population analysis indicated that administration of valproic acid decreases the clearance of temozolomide by about 5% [see Drug Interactions (7.1)].
A population analysis did not demonstrate any influence of coadministered dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, H2-receptor antagonists, or phenobarbital on the clearance of orally administered temozolomide.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Temozolomide is carcinogenic in rats at doses less than the maximum recommended human dose. Temozolomide induced mammary carcinomas in both males and females at doses 0.13 to 0.63 times the maximum human dose (25 to 125 mg/m2) when administered orally on 5 consecutive days every 28 days for 6 cycles. Temozolomide also induced fibrosarcomas of the heart, eye, seminal vesicles, salivary glands, abdominal cavity, uterus, and prostate, carcinomas of the seminal vesicles, schwannomas of the heart, optic nerve, and harderian gland, and adenomas of the skin, lung, pituitary, and thyroid at doses 0.5 times the maximum daily dose. Mammary tumors were also induced following 3 cycles of temozolomide at the maximum recommended daily dose.
Temozolomide is a mutagen and a clastogen. In a reverse bacterial mutagenesis assay (Ames assay), temozolomide increased revertant frequency in the absence and presence of metabolic activation. Temozolomide was clastogenic in human lymphocytes in the presence and absence of metabolic activation.
Temozolomide impairs male fertility. Temozolomide caused syncytial cells/immature sperm formation at 0.25 and 0.63 times the maximum recommended human dose (50 and 125 mg/m2) in rats and dogs, respectively, and testicular atrophy in dogs at 0.63 times the maximum recommended human dose (125 mg/m2).
13.2 Animal Toxicology and/or Pharmacology
Toxicology studies in rats and dogs identified a low incidence of hemorrhage, degeneration, and necrosis of the retina at temozolomide doses equal to or greater than 0.63 times the maximum recommended human dose (125 mg/m2). These changes were most commonly seen at doses where mortality was observed.
14 CLINICAL STUDIES
14.1 Newly Diagnosed Glioblastoma Multiforme
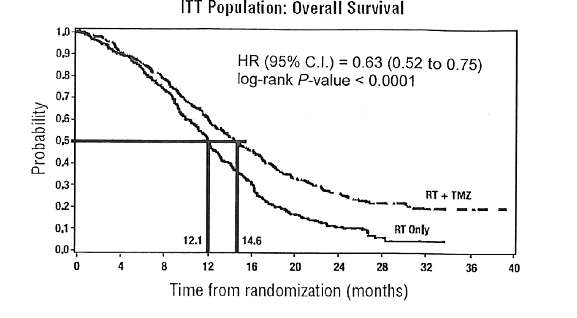
Five hundred and seventy-three patients were randomized to receive either temozolomide (TMZ) + Radiotherapy (RT) (n = 287) or RT alone (n = 286). Patients in the temozolomide + RT arm received concomitant temozolomide (75 mg/m2) once daily, starting the first day of RT until the last day of RT, for 42 days (with a maximum of 49 days). This was followed by 6 cycles of temozolomide alone (150 or 200 mg/m2) on Days 1 to 5 of every 28 day cycle, starting 4 weeks after the end of RT. Patients in the control arm received RT only. In both arms, focal radiation therapy was delivered as 60 Gy/30 fractions. Focal RT includes the tumor bed or resection site with a 2 to 3 cm margin. Pneumocystis carinii pneumonia (PCP) prophylaxis was required during the TMZ + RT, regardless of lymphocyte count, and was to continue until recovery of lymphocyte count to less than or equal to Grade 1.
At the time of disease progression, temozolomide was administered as salvage therapy in 161 patients of the 282 (57%) in the RT alone arm, and 62 patients of the 277 (22%) in the temozolomide + RT arm.
The addition of concomitant and maintenance temozolomide to radiotherapy in the treatment of patients with newly diagnosed GBM showed a statistically significant improvement in overall survival compared to radiotherapy alone (Figure 1). The hazard ratio (HR) for overall survival was 0.63 (95% CI for HR = 0.52 to 0.75) with a log-rank p < 0.0001 in favor of the temozolomide arm. The median survival was increased by 2.5 months in the temozolomide arm.
14.2 Refractory Anaplastic Astrocytoma
A single-arm, multicenter study was conducted in 162 patients who had anaplastic astrocytoma at first relapse and who had a baseline Karnofsky performance status of 70 or greater. Patients had previously received radiation therapy and may also have previously received a nitrosourea with or without other chemotherapy. Fifty-four patients had disease progression on prior therapy with both a nitrosourea and procarbazine, and their malignancy was considered refractory to chemotherapy (refractory anaplastic astrocytoma population). Median age of this subgroup of 54 patients was 42 years (19 to 76). Sixty-five percent were male. Seventy-two percent of patients had a KPS of >80. Sixty-three percent of patients had surgery other than a biopsy at the time of initial diagnosis. Of those patients undergoing resection, 73% underwent a subtotal resection and 27% underwent a gross total resection. Eighteen percent of patients had surgery at the time of first relapse. The median time from initial diagnosis to first relapse was 13.8 months (4.2 to 75.4).
Temozolomide capsules were given for the first 5 consecutive days of a 28 day cycle at a starting dose of 150 mg/m2/day. If the nadir and day of dosing (Day 29, Day 1 of next cycle) absolute neutrophil count was ≥ 1.5 x 109/L (1500/μL) and the nadir and Day 29, Day 1 of next cycle platelet count was ≥ 100 x 109/L (100,000/μL), the temozolomide dose was increased to 200 mg/m2/day for the first 5 consecutive days of a 28 day cycle.
In the refractory anaplastic astrocytoma population, the overall tumor response rate (CR + PR) was 22% (12/54 patients) and the complete response rate was 9% (5/54 patients). The median duration of all responses was 50 weeks (range: 16-114 weeks) and the median duration of complete responses was 64 weeks (range: 52-114 weeks). In this population, progression-free survival at 6 months was 45% (95% CI: 31%-58%) and progression-free survival at 12 months was 29% (95% CI: 16%-42%). Median progression-free survival was 4.4 months. Overall survival at 6 months was 74% (95% CI: 62%-86%) and 12-month overall survival was 65% (95% CI: 52%-78%). Median overall survival was 15.9 months.
15 REFERENCES
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999.
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006; 63:1172-1193.
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165. [3]
- Polovich, M., White, J.M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Safe Handling and Disposal
Care should be exercised in the handling and preparation of temozolomide. Capsules should not be opened. If capsules are accidentally opened or damaged, rigorous precautions should be taken with the contents to avoid inhalation or contact with the skin or mucous membranes. The use of gloves and safety glasses is recommended to avoid exposure in case of breakage of the capsules. Procedures for proper handling and disposal of anticancer drugs should be considered1 to 4. Several guidelines on this subject have been published.
16.2 How Supplied
Temozolomide Capsules
|
5 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with white to off-white powder. Imprinted in green ink stylized barr over 5 mg on one piece and 1078 on the other piece. Available in bottles of 5 and 14. |
| 20 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with white to off-white powder. Imprinted in brown ink stylized barr over 20 mg on one piece and 1077 on the other piece. Available in bottles of 5 and 14. |
| 100 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in blue ink stylized barr over 100 mg on one piece and 1076 on the other piece. Available in bottles of 5 and 14. |
| 140 mg: |
Two-piece hard gelatin capsule with blue opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 140 mg on one piece and 1159 on the other piece. Available in bottles of 5 and 14. |
| 180 mg: |
Two-piece hard gelatin capsule with dark orange opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 180 mg on one piece and 1160 on the other piece. Available in bottles of 5 and 14. |
| 250 mg: |
Two-piece hard gelatin capsule with off-white opaque cap and off-white opaque body filled with off-white or light tan/light pink powder. Imprinted in black ink stylized barr over 250 mg on one piece and 1075 on the other piece. Available in bottles of 5. |
16.3 Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container or retain in original bottle.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling (Patient Information).
17.1 Information for the Patient
Physicians should discuss the following with their patients:
- Nausea and vomiting are the most frequently occurring adverse reactions. Nausea and vomiting are usually either self-limiting or readily controlled with standard antiemetic therapy.
- Capsules should not be opened. If capsules are accidentally opened or damaged, rigorous precautions should be taken with the capsule contents to avoid inhalation or contact with the skin or mucous membranes.
- The medication should be kept away from children and pets.
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. C 1/2013
TEMOZOLOMIDE (tem-oh zoe-loe-mide)
Capsules
PHARMACIST
Dispense enclosed Patient Package Insert to each patient.
Rx only
PHARMACIST INFORMATION SHEET
IMPORTANT DISPENSING INFORMATION
For every patient, temozolomide must be dispensed in its original package making sure each container lists the strength per capsule and that patients take the appropriate number of capsules from each package.
Please see the dispensing instructions below for more information.
What is temozolomide?
Temozolomide is an oral alkylating agent for the treatment of newly diagnosed glioblastoma multiforme and refractory anaplastic astrocytoma.
How is temozolomide dosed?
The daily dose of temozolomide capsules for a given patient is calculated by the physician, based on the patient’s body surface area (BSA). The resulting dose is then rounded off to the nearest 5 mg. An example of the dosing may be as follows: the initial daily dose of temozolomide in milligrams is the BSA multiplied by mg/m2/day, (a patient with a BSA of 1.84 is 1.84 x 75 mg = 138, or 140 mg/day). The dose for subsequent cycles may be adjusted according to nadir neutrophil and platelet counts in the previous cycle and at the time of initiating the next cycle.
How might the dose of temozolomide be modified for Refractory Anaplastic Astrocytoma?
Dosage of temozolomide must be adjusted according to nadir neutrophil and platelet counts in the previous cycle and neutrophil and platelet counts at the time of initiating the next cycle. The initial dose is 150 mg/m2 orally once daily for 5 consecutive days per 28 day treatment cycle. If both the nadir and day of dosing (Day 29, Day 1 of next cycle) absolute neutrophil counts (ANC) are greater than or equal to 1.5 x 109/L (1500/µL) and both the nadir and Day 29, Day 1 of next cycle platelet counts are greater than or equal to 100 x 109/L (100,000/µL), the temozolomide dose may be increased to 200 mg/m2/day for 5 consecutive days per 28 day treatment cycle. During treatment, a complete blood count should be obtained on Day 22 (21 days after the first dose) or within 48 hours of that day, and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). The next cycle of temozolomide should not be started until the ANC and platelet count exceed these levels. If the ANC falls to less than 1 x 109/L (1,000/µL) or the platelet count is less than 50 x 109/L (50,000/µL) during any cycle, the next cycle should be reduced by 50 mg/m2, but not below 100 mg/m2, the lowest recommended dose (see Table 1).
What is the temozolomide capsules treatment regimen?
Temozolomide is given for 5 consecutive days on a 28 day cycle. Patients should continue taking temozolomide until their physician determines that their disease has progressed, up to 2 years, or until unacceptable side effects or toxicities occur. Physicians may alter the treatment regimen for a given patient.
Newly Diagnosed Concomitant Phase Treatment Schedule
Temozolomide is administered orally at 75 mg/m2 daily for 42 days concomitant with focal radiotherapy (60 Gy administered in 30 fractions), followed by maintenance temozolomide for 6 cycles. No dose reductions are recommended; however, dose interruptions may occur based on patient tolerance. The temozolomide dose can be continued throughout the 42 day concomitant period up to 49 days if all of the following conditions are met: absolute neutrophil count greater than or equal to 1.5 x 109/L, platelet count greater than or equal to 100 x109/L, common toxicity criteria (CTC) nonhematological toxicity less than or equal to Grade 1 (except for alopecia, nausea and vomiting). During treatment a complete blood count should be obtained weekly. Temozolomide dosing should be interrupted or discontinued during concomitant phase according to the hematological and nonhematological toxicity criteria as noted in Table 2. Pneumocystis carinii pneumonia (PCP) prophylaxis is required during the concomitant administration of temozolomide and radiotherapy, and should be continued in patients who develop lymphocytopenia until recovery from lymphocytopenia (CTC grade less than or equal to 1).
| TMZ = temozolomide; CTC = Common Toxicity Criteria. | ||
| Toxicity |
TMZ Interruption |
TMZ Discontinuation |
| Absolute Neutrophil Count | greater than or equal to 0.5 and less than 1.5 x 109/L |
less than 0.5 x 109/L |
| Platelet Count | greater than or equal to 10 and less than 100 x 109/L | less than 10 x 109/L |
| CTC Nonhematological Toxicity (except for alopecia, nausea, vomiting) |
CTC Grade 2 |
CTC Grade 3 or 4 |
Maintenance Phase Treatment Schedule
Four weeks after completing the temozolomide + RT phase, temozolomide is administered for an additional 6 cycles of maintenance treatment. Dosage in Cycle 1 (maintenance) is 150 mg/m2 once daily for 5 days followed by 23 days without treatment. At the start of Cycle 2, the dose is escalated to 200 mg/m2, if the CTC nonhematologic toxicity for Cycle 1 is Grade less than or equal to 2 (except for alopecia, nausea and vomiting), absolute neutrophil count (ANC) is greater than or equal to 1.5 x 109/L, and the platelet count is greater than or equal to 100 x 109/L. If the dose was not escalated at Cycle 2, escalation should not be done in subsequent cycles. The dose remains at 200 mg/m2 per day for the first 5 days of each subsequent cycle except if toxicity occurs.
During treatment a complete blood count should be obtained on Day 22 (21 days after the first dose) or within 48 hours of that day, and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). The next cycle of temozolomide should not be started until the ANC and platelet count exceed these levels. Dose reductions during the next cycle should be based on the lowest blood counts and worst nonhematologic toxicity during the previous cycle. Dose reductions or discontinuations during the maintenance phase should be applied according to Tables 3 and 4.
| Dose Level | Dose (mg/m2/day) | Remarks |
| -1 | 100 | Reduction for prior toxicity |
| 0 | 150 | Dose during Cycle 1 |
| 1 | 200 | Dose during Cycles 2 to 6 in absence of toxicity |
| TMZ = temozolomide; CTC = Common Toxicity Criteria. | ||
| Toxicity |
Reduce TMZ by 1 Dose Level |
Discontinue TMZ |
| Absolute Neutrophil Count | less than 1 x 109/L | See footnote |
| Platelet Count | less than 50 x 109/L | See footnote |
|
CTC Nonhematological Toxicity (except for alopecia, nausea, vomiting) |
CTC Grade 3 |
CTC Grade 4  |
How is temozolomide taken?
Patients should take each day’s dose with a full glass of water at the same time each day. Taking the medication on an empty stomach or at bedtime may help ease nausea. If patients are also taking antinausea or other medications to relieve the side effects associated with temozolomide, they should be advised to take these medications 30 minutes before they take temozolomide. Temozolomide causes the rapid appearance of malignant tumors in rats. Patients SHOULD NOT open or split the capsules. If capsules are accidentally opened or damaged, rigorous precautions should be taken with the capsule contents to avoid inhalation or contact with the skin or mucous membranes. The medication should be kept away from children and pets. The temozolomide capsules should be swallowed whole and NEVER CHEWED.
What should the patient avoid during treatment with temozolomide?
There are no dietary restrictions for patients taking temozolomide. Temozolomide may affect testicular function, so male patients should exercise adequate birth control measures. Temozolomide may cause birth defects. Female patients should avoid becoming pregnant while receiving this drug. Women who are nursing prior to receiving temozolomide should discontinue nursing. It is not known whether temozolomide is excreted into breast milk. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants and tumorigenicity shown for temozolomide in animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of temozolomide to the mother.
What are the side effects of temozolomide?
Nausea and vomiting are the most common side effects associated with temozolomide. Noncumulative myelosuppression is the dose-limiting toxicity. Patients should be evaluated periodically by their physician to monitor blood counts.
Other commonly reported side effects reported by patients taking temozolomide are fatigue, constipation, alopecia, anorexia, and headache.
How is temozolomide supplied?
Temozolomide capsules are available in 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, and 250 mg strengths. The 5 mg, 20 mg, 100 mg, and 250 mg capsules contain an off-white capsule body with an off-white cap. The 140 mg capsules contain an off-white capsule body with a blue cap. The 180 mg capsules contain an off-white capsule body with a dark orange cap. Each capsule contains color-coded printing or a different color cap according to strength.
| Temozolomide Capsule Strength | Color |
| 5 mg | Green Imprint |
| 20 mg | Brown Imprint |
| 100 mg | Blue Imprint |
| 140 mg | Blue Cap |
| 180 mg | Dark Orange Cap |
| 250 mg | Black Imprint |
The 5 mg, 20 mg, 100 mg, 140 mg, and 180 mg capsule strengths are available in 5 count and 14 count packages. The 250 mg capsule strength is available in a 5 count package.
How is temozolomide dispensed?
Each strength of temozolomide must be dispensed in its original package (one strength per one container). Follow the instructions below:
Based on the dose prescribed, determine the number of each strength of temozolomide capsules needed for the full 42 or 5 day cycle as prescribed by the physician. For example, in a 5 day cycle, 275 mg/day would be dispensed as five 250 mg capsules, five 20 mg capsules and five 5 mg capsules. Label each container with the appropriate number of capsules to be taken each day. Dispense to the patient, making sure each container lists the strength (mg) per capsule and that he or she understands to take the appropriate number of capsules of temozolomide from each package to equal the total daily dose prescribed by the physician.
How can temozolomide be ordered?
Temozolomide can be ordered from your wholesaler. It is important to understand if temozolomide is being used as part of a 42 day regimen or as part of a 5 day course. Remember to order enough temozolomide for the appropriate cycle.
For example:
- a 5 day course of 360 mg/day would require the following to be ordered: two 5 count packages of 180 mg capsules.
- a 42 day course of 140 mg/day would require the following to be ordered: three 14 count packages of 140 mg capsules.
For examples of other dosing regimens, please refer to the full Prescribing Information (Table 6).
| Temozolomide Product | NDC Number |
| Bottles | |
| 5 mg capsules (5 count) | 0093-7599-57 |
| 5 mg capsules (14 count) | 0093-7599-41 |
| 20 mg capsules (5 count) | 0093-7600-57 |
| 20 mg capsules (14 count) | 0093-7600-41 |
| 100 mg capsules (5 count) | 0093-7601-57 |
| 100 mg capsules (14 count) | 0093-7601-41 |
| 140 mg capsules (5 count) | 0093-7638-57 |
| 140 mg capsules (14 count) | 0093-7638-41 |
| 180 mg capsules (5 count) | 0093-7639-57 |
| 180 mg capsules (14 count) | 0093-7639-41 |
| 250 mg capsules (5 count) | 0093-7602-57 |
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. C 1/2013
TEMOZOLOMIDE (tem-oh zoe-loe-mide)
Capsules
Rx only
What is the most important information I should know about temozolomide?
- Temozolomide may cause birth defects. Male and female patients who take temozolomide should use effective birth control. Female patients and female partners of male patients should avoid becoming pregnant while taking temozolomide.
See the section “What are the possible side effects of temozolomide?” for more information about side effects.
What is temozolomide?
Temozolomide is a prescription medicine used to treat adults with certain brain cancer tumors. Temozolomide blocks cell growth, especially cells that grow fast, such as cancer cells. Temozolomide may decrease the size of certain brain tumors in some patients.
It is not known if temozolomide is safe and effective in children.
Who should not take temozolomide?
Do not take temozolomide if you:
- have had an allergic reaction to dacarbazine (DTIC), another cancer medicine.
- have had a red itchy rash, or a severe allergic reaction, such as trouble breathing, swelling of the face, throat, or tongue, or severe skin reaction to temozolomide or any of the ingredients in temozolomide. If you are not sure, ask your doctor. See the end of the leaflet for a list of ingredients in temozolomide.
What should I tell my doctor before taking temozolomide?
Tell your doctor about all your medical conditions, including if you:
- are allergic to dacarbazine (DTIC) or have had a severe allergic reaction to temozolomide. See “Who should not take temozolomide?”
- have kidney problems
- have liver problems
- are pregnant. See “What is the most important information I should know about temozolomide?”
- are breastfeeding. It is not known whether temozolomide passes into breast milk. You and your doctor should decide if you will breastfeed or take temozolomide. You should not do both without talking with your doctor.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take a medicine that contains valproic acid (Stavzor®, Depakene®).
Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine.
How should I take temozolomide?
Temozolomide may be taken by mouth as a capsule at home.
There are two common dosing schedules for taking temozolomide.
- Some people take temozolomide for 42 days in a row (possibly 49 days depending on side effects) with radiation treatment. This is one cycle of treatment. After this, you may have “maintenance” treatment. Your doctor may prescribe 6 more cycles of temozolomide capsules. For each of these cycles, you take temozolomide capsules one time each day for 5 days in a row and then you stop taking it for the next 23 days. This is a 28 day maintenance treatment cycle.
- Another way to take temozolomide capsules is to take it one time each day for 5 days in a row only, and then you stop taking it for the next 23 days. This is one cycle of treatment (28 days). Your doctor will watch your progress on temozolomide capsules and decide how long you should take it. You might take temozolomide capsules until your tumor gets worse or for possibly up to 2 years.
- Your dose is based on your height and weight, and the number of treatment cycles will depend on how you respond to and tolerate this treatment.
- Your doctor may modify your schedule based on how you tolerate the treatment.
- If your doctor prescribes a treatment regimen that is different from the information in this leaflet, make sure you follow the specific instructions given to you by your doctor.
Temozolomide Capsules
- Take temozolomide capsules exactly as prescribed.
- Temozolomide capsules come in different strengths. Each capsule strength has a different color-coded printing or a different color cap. Your doctor may prescribe more than one strength of temozolomide capsules for you, so it is important that you understand how to take your medicine the right way. Be sure that you understand exactly how many capsules you need to take on each day of your treatment, and what strengths to take. This may be different whenever you start a new cycle.
- Talk to your doctor before you take your dose if you are not sure how much to take. This will help to prevent taking too much temozolomide and decrease your chances of getting serious side effects.
- Take each day’s dose of temozolomide capsules at one time, with a full glass of water.
- Swallow temozolomide capsules whole. Do not chew, open, or split the capsules.
- If temozolomide capsules are accidentally opened or damaged, be careful not to breathe in (inhale) the powder from the capsules or get the powder on your skin or mucous membranes (for example, in your nose or mouth). If contact with any of these areas happens, flush the area with water.
- If you vomit temozolomide capsules, do not take any more capsules. Wait and take your next planned dose.
- The medicine is used best by your body if you take it at the same time every day in relation to a meal.
- To lessen nausea, try to take temozolomide on an empty stomach or at bedtime. Your doctor may prescribe medicine to prevent or treat nausea, or other medicines to lessen side effects with temozolomide.
- See your doctor regularly to check your progress. Your doctor will check you for side effects that you might not notice.
- If you miss a dose of temozolomide, talk with your doctor for instructions about when to take your next dose of temozolomide.
- Call your doctor right away if you take more than the prescribed amount of temozolomide. It is important that you do not take more than the amount of temozolomide prescribed for you.
What should I avoid while taking temozolomide?
- Female patients and female partners of male patients should avoid becoming pregnant while taking temozolomide. See “What is the most important information I should know about temozolomide?”
What are the possible side effects of temozolomide?
Temozolomide can cause serious side effects.
- See “What is the most important information I should know about temozolomide?”
-
Decreased blood cells. Temozolomide affects cells that grow rapidly, including bone marrow cells. This can cause you to have a decrease in blood cells. Your doctor can monitor your blood for these effects.
- White blood cells are needed to fight infections. Neutrophils are a type of white blood cell that help prevent bacterial infections. Decreased neutrophils can lead to serious infections that can lead to death. Other white blood cells called lymphocytes may also be decreased.
- Platelets are blood cells needed for normal blood clotting. Low platelet counts can lead to bleeding. Tell your doctor about any unusual bruising or bleeding.
Your doctor will check your blood regularly while you are taking temozolomide to see if these side effects are happening. Your doctor may need to change the dose of temozolomide or when you get it depending on your blood cell counts. People who are age 70 or older and women may be more likely to have their blood cells affected.
- Pneumocystis carinii Pneumonia (PCP). PCP is an infection that people can get when their immune system is weak. Temozolomide decreases white blood cells, which makes your immune system weaker and can increase your risk of getting PCP. All patients taking temozolomide will be watched carefully by their doctor for this infection, especially patients who take steroids. Tell your doctor if you have any of the following signs and symptoms of PCP infection: shortness of breath and/or fever, chills, dry cough.
- Secondary cancers. Blood problems such as myelodysplastic syndrome and secondary cancers, such as a certain kind of leukemia, can happen in people who take temozolomide. Your doctor will watch you for this.
- Convulsions. Convulsions may be severe or life-threatening in people who take temozolomide.
Common side effects with temozolomide include:
- nausea and vomiting. Your doctor can prescribe medicines that may help reduce these symptoms.
- headache
- feeling tired
- loss of appetite
- hair loss
- constipation
- bruising
- rash
- paralysis on one side of the body
- diarrhea
- weakness
- fever
- dizziness
- coordination problems
- viral infection
- sleep problems
- memory loss
- bruising or small red or purple spots under the skin
Tell your doctor about any side effect that bothers you or that does not go away.
These are not all the possible side effects with temozolomide. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store temozolomide capsules?
- Store temozolomide capsules at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
- Keep temozolomide capsules out of the reach of children and pets.
General information about temozolomide.
Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use temozolomide for a condition for which it was not prescribed. Do not give temozolomide to other people, even if they have the same symptoms that you have. It may harm them.
This leaflet summarizes the most important information about temozolomide. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about temozolomide that is written for health professionals.
For more information, call Medical Affairs at 1-866-832-8537.
How are temozolomide capsules supplied?
The 5 mg, 20 mg, 100 mg and 250 mg temozolomide capsules contain an off-white capsule body with an off-white cap. The 140 mg capsules contain an off-white capsule body with a blue cap. The 180 mg capsules contain an off-white capsule body with a dark orange cap. Each capsule contains color-coded printing or a different color cap according to strength. The capsules are available in six different strengths.
| Temozolomide Capsule Strength | Color |
| 5 mg | Green Imprint |
| 20 mg | Brown Imprint |
| 100 mg | Blue Imprint |
| 140 mg | Blue Cap |
| 180 mg | Dark Orange Cap |
| 250 mg | Black Imprint |
What are the ingredients in temozolomide?
Temozolomide Capsules
Active ingredient: temozolomide.
Inactive ingredients: anhydrous lactose, colloidal silicon dioxide, povidone, sodium starch glycolate, stearic acid, and tartaric acid. The 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, and 250 mg capsule shells contain D&C yellow no. 10, FD&C red no. 40, FD&C yellow no. 6, gelatin, and titanium dioxide. The 140 mg capsule shell also contains D&C red no. 28, FD&C blue no. 1, and FD&C green no. 3. The 180 mg capsule shell also contains FD&C blue no. 1. The 5 mg imprinting ink contains ammonium hydroxide, black iron oxide, D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, propylene glycol, and shellac. The 20 mg imprinting ink contains ammonium hydroxide, black iron oxide, propylene glycol, red iron oxide, shellac, and yellow iron oxide. The 100 mg imprinting ink contains FD&C blue no. 1 aluminum lake, polyvinylpyrrolidone, propylene glycol, shellac, sodium hydroxide, and titanium dioxide. The 140 mg, 180 mg, and 250 mg imprinting ink contains black iron oxide, D&C yellow no. 10 aluminum lake, FD&C blue no. 1 aluminum lake, FD&C blue no. 2 aluminum lake, FD&C red no. 40 aluminum lake, propylene glycol, and shellac.
All brand names listed are the registered trademarks of their respective owners and are not trademarks of Teva Pharmaceuticals USA.
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. C 1/2013
Principal Display Panel

Temozolomide Capsules 5 mg 5s Label Text
NDC 0093-7599-57
TEMOZOLOMIDE
Capsules
5 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA
Principal Display Panel
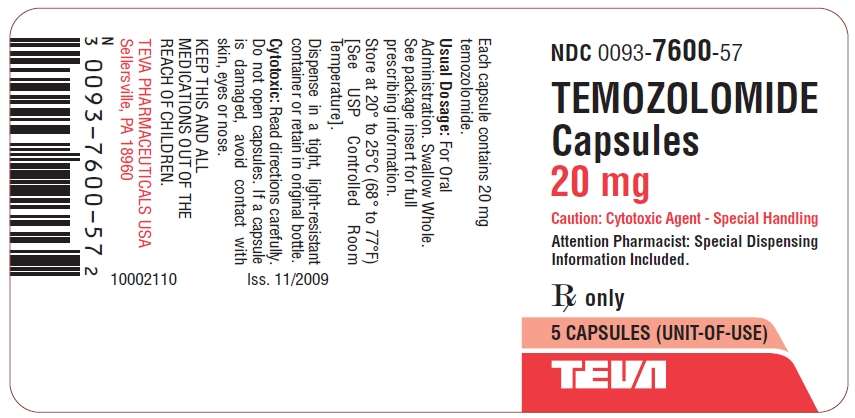
Temozolomide Capsules 20 mg 5s Label Text
NDC 0093-7600-57
TEMOZOLOMIDE
Capsules
20 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA
Principal Display Panel
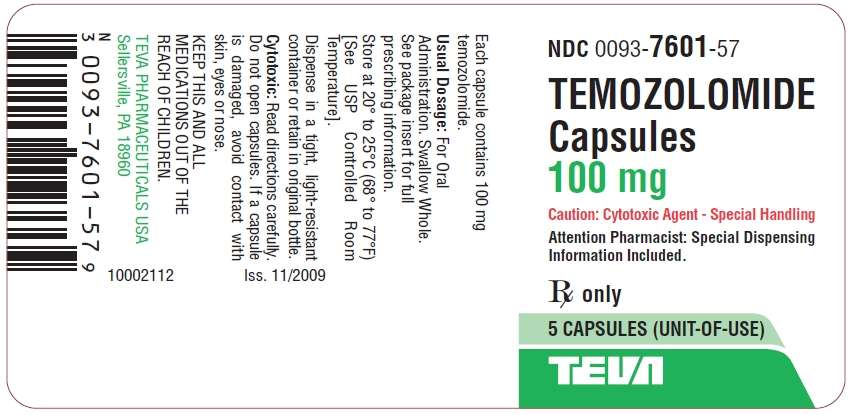
Temozolomide Capsules 100 mg 5s Label Text
NDC 0093-7601-57
TEMOZOLOMIDE
Capsules
100 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA
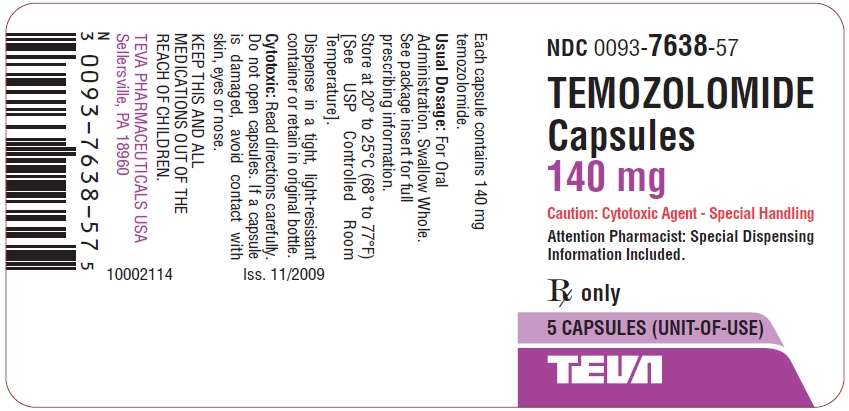
Temozolomide Capsules 140 mg 5s Label Text
NDC 0093-7638-57
TEMOZOLOMIDE
Capsules
140 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA

Temozolomide Capsules 180 mg 5s Label Text
NDC 0093-7639-57
TEMOZOLOMIDE
Capsules
180 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA
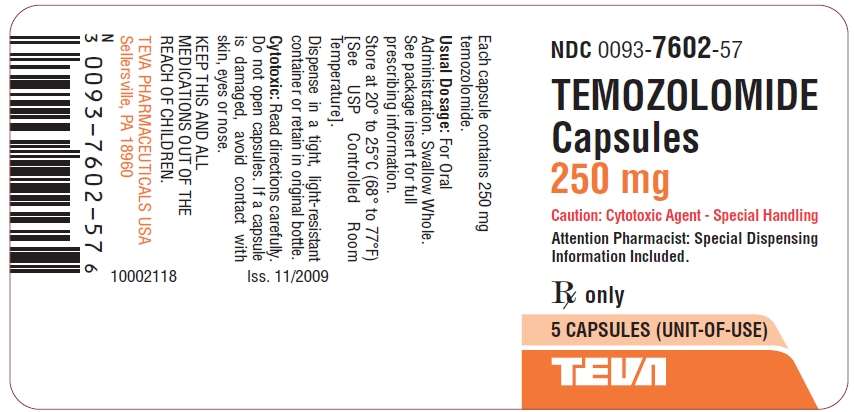
Temozolomide Capsules 250 mg 5s Label Text
NDC 0093-7602-57
TEMOZOLOMIDE
Capsules
250 mg
Caution: Cytotoxic Agent - Special Handling
Attention Pharmacist: Special Dispensing
Information Included.
Rx only
5 CAPSULES (UNIT-OF-USE)
TEVA
TemozolomideTemozolomide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TemozolomideTemozolomide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TemozolomideTemozolomide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TemozolomideTemozolomide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TemozolomideTemozolomide CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TemozolomideTemozolomide CAPSULE
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||