Ramipril
Exelan Pharmaceuticals, Inc.
InvaGen Pharmaceuticals, Inc.
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use ramipril capsules safely and effectively. See full prescribing information for ramipril capsules.Ramipril Capsules, USP, Oral Initial U.S. Approval: 1991 RECENT MAJOR CHANGES WARNINGS AND PRECAUTIONS Dual Blockade of the Renin-Angiotensin- Aldosterone System: Telmisartan (5.7) 10/2010 BOXED WARNINGWARNING: AVOID USE IN PREGNANCY See full prescribing information for complete boxed warning When used in pregnancy, ACE inhibitors can cause injury and death to the developing fetus. When pregnancy is detected, discontinue ramipril as soon as possible (5.6). INDICATIONS AND USAGE Ramipril capsules, USP are indicated for the treatment of hypertension. It may be used alone or in combination with thiazide diuretics. (1.1). DOSAGE AND ADMINISTRATION Hypertension: Initial dose is 2.5 mg to 20 mg once daily. Adjust dosage according to blood pressure response after 2 to 4 weeks of treatment. The usual maintenance dose following titration is 2.5 mg to 20 mg daily as a single dose or equally divided doses (2.1). Dosage adjustment: See respective sections pertaining to dosage adjustment in special situations (2.5). DOSAGE FORMS AND STRENGTHSCapsule: 1.25 mg, 2.5 mg, 5 mg, 10 mg (3) CONTRAINDICATIONSAngioedema related to previous treatment with an ACE inhibitor, or a history of hereditary or idiopathic angioedema.(4). WARNINGS AND PRECAUTIONSACE inhibitor use has been associated with the following: Angioedema, with increased risk in patients with a prior history (5.1) Hypotension and hyperkalemia (5.5, 5.8) Renal impairment: monitor renal function during therapy (5.3) Increased risk of renal impairment when combined with another blocker of the renin-angiotensin-aldosterone system (5.7) Rare cholestatic jaundice and hepatic failure (5.2) Rare neutropenia and agranulocytosis (5.4) Side EffectsThe most common adverse reactions in patients with hypertension included headache, dizziness, fatigue, and cough (6.1). To report SUSPECTED ADVERSE REACTIONS, contact Exelan Pharmaceuticals, Inc. at 1-877-397-6028 or www.exelanpharma.com or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Diuretics: Possibility of excessive hypotension (7.1). Lithium: Use with caution (7.3). Gold: Nitritoid reactions have been reported (7.4). USE IN SPECIFIC POPULATIONS Pregnancy: Discontinue drug if pregnancy is detected (5.6, 8.1). Nursing mothers: Ramipril use is not recommended in nursing mothers (8.3).
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: USE IN PREGNANCY
- 1 RAMIPRIL INDICATIONS AND USAGE
- 2 RAMIPRIL DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 RAMIPRIL CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 RAMIPRIL ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 RAMIPRIL DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
WARNING: USE IN PREGNANCY
- When used in pregnancy during the second and third trimesters, ACE inhibitors can cause injury and even death to the developing fetus. When pregnancy is detected, discontinue ramipril as soon as possible (5.6).
1 INDICATIONS AND USAGE
1.1 Hypertension
Ramipril Capsules, USP are indicated for the treatment of hypertension. They may be used alone or in combination with thiazide diuretics.
2 DOSAGE AND ADMINISTRATION
2.1 Hypertension
The recommended initial dose for patients not receiving a diuretic is 2.5 mg once a day. Adjust dose according to blood pressure response. The usual maintenance dosage range is 2.5 mg to 20 mg per day administered as a single dose or in two equally divided doses. In some patients treated once daily, the antihypertensive effect may diminish toward the end of the dosing interval. In such patients, consider an increase in dosage or twice daily administration. If blood pressure is not controlled with ramipril capsules alone, a diuretic can be added.
2.4 General Dosing Information
Generally, swallow ramipril capsules whole. The ramipril capsule can also be opened and the contents sprinkled on a small amount (about 4 oz.) of applesauce or mixed in 4 oz. (120 mL) of water or apple juice. To be sure that ramipril is not lost when such a mixture is used, consume the mixture in its entirety. The described mixtures can be pre-prepared and stored for up to 24 hours at room temperature or up to 48 hours under refrigeration. Concomitant administration of ramipril capsules with potassium supplements, potassium salt substitutes, or potassium-sparing diuretics can lead to increases of serum potassium [see Warnings and Precautions ( 5.8 )]
2.5 Dosage Adjustment
Renal Impairment
Establish baseline renal function in patients initiating ramipril capsules. Usual regimens of therapy with ramipril capsules may be followed in patients with estimated creatinine clearance > 40 mL/min. However, in patients with worse impairment, 25% of the usual dose of ramipril is expected to produce full therapeutic levels of ramiprilat [see Use in Specific Population (8.6 )].
Hypertension
For patients with hypertension and renal impairment, the recommended initial dose is 1.25 mg ramipril capsules once daily. Dosage may be titrated upward until blood pressure is controlled or to a maximum total daily dose of 5 mg.
Volume Depletion or Renal Artery Stenosis
Blood pressure decreases associated with any dose of ramipril capsules depend, in part, on the presence or absence of volume depletion (e.g., past and current diuretic use) or the presence or absence of renal artery stenosis. If such circumstances are suspected to be present, initiate dosing at 1.25 mg once daily. Adjust dosage according to blood pressure response.
3 DOSAGE FORMS AND STRENGTHS
Ramipril capsules are supplied as hard gelatin capsules containing 1.25 mg, 2.5 mg, 5 mg, and 10 mg of ramipril.
4 CONTRAINDICATIONS
Ramipril capsules are contraindicated in patients who are hypersensitive to this product or any other ACE inhibitor (e.g., a patient who has experienced angioedema during therapy with any other ACE inhibitor).
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylactoid and Possibly Related Reactions
Presumably because drugs that act directly on the renin-angiotensin-aldosterone system (e.g., ACE inhibitors) affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving these drugs (including ramipril) may be subject to a variety of adverse reactions, some of them serious.
Angioedema
Head and Neck Angioedema
Patients with a history of angioedema unrelated to ACE inhibitor therapy may be at increased risk of angioedema while receiving an ACE inhibitor.
Angioedema of the face, extremities, lips, tongue, glottis, and larynx has been reported in patients treated with ACE inhibitors. Angioedema associated with laryngeal edema can be fatal. If laryngeal stridor or angioedema of the face, tongue, or glottis occurs, discontinue treatment with ramipril and institute appropriate therapy immediately. Where there is involvement of the tongue, glottis, or larynx likely to cause airway obstruction, administer appropriate therapy (e.g., subcutaneous epinephrine solution 1:1000 [0.3 mL to 0.5 mL]) promptly [see ADVERSE REACTIONS ( 6 )].
In considering the use of ramipril, note that in controlled clinical trials ACE inhibitors cause a higher rate of angioedema in Black patients than in non-Black patients.
In a large U.S. postmarketing study, angioedema (defined as reports of angio, face, larynx, tongue, or throat edema) was reported in 3/1523 (0.20%) Black patients and in 8/8680 (0.09%) non-Black patients. These rates were not different statistically.
Intestinal Angioedema
Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Include intestinal angioedema in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Anaphylactoid Reactions During Desensitization
Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid Reactions During Membrane Exposure
Anaphylactoid reactions have been reported in patients dialyzed with high-flux membranes and treated concomitantly with an ACE inhibitor. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
5.2 Hepatic Failure and Impaired Liver Function
Rarely, ACE inhibitors, including ramipril, have been associated with a syndrome that starts with cholestatic jaundice and progresses to fulminant hepatic necrosis and sometimes death. The mechanism of this syndrome is not understood. Discontinue ramipril if patient develops jaundice or marked elevations of hepatic enzymes.
As ramipril is primarily metabolized by hepatic esterases to its active moiety, ramiprilat, patients with impaired liver function could develop markedly elevated plasma levels of ramipril. No formal pharmacokinetic studies have been carried out in hypertensive patients with impaired liver function.
5.3 Renal Impairment
As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible individuals. In patients whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with ACE inhibitors, including ramipril, may be associated with oliguria or progressive azotemia and rarely with acute renal failure or death.
In hypertensive patients with unilateral or bilateral renal artery stenosis, increases in blood urea nitrogen and serum creatinine may occur. Experience with another ACE inhibitor suggests that these increases would be reversible upon discontinuation of ramipril and/or diuretic therapy. In such patients, monitor renal function during the first few weeks of therapy. Some hypertensive patients with no apparent preexisting renal vascular disease have developed increases in blood urea nitrogen and serum creatinine, usually minor and transient, especially when ramipril has been given concomitantly with a diuretic. This is more likely to occur in patients with preexisting renal impairment. Dosage reduction of ramipril and/or discontinuation of the diuretic may be required.
5.4 Neutropenia and Agranulocytosis
In rare instances, treatment with ACE inhibitors may be associated with mild reductions in red blood cell count and hemoglobin content, blood cell or platelet counts. In isolated cases, agranulocytosis, pancytopenia, and bone marrow depression may occur. Hematological reactions to ACE inhibitors are more likely to occur in patients with collagen-vascular disease (e.g., systemic lupus erythematosus, scleroderma) and renal impairment. Consider monitoring white blood cell counts in patients with collagen-vascular disease, especially if the disease is associated with impaired renal function.
5.5 Hypotension
General Considerations
Ramipril can cause symptomatic hypotension, after either the initial dose or a later dose when the dosage has been increased. Like other ACE inhibitors, ramipril, has been only rarely associated with hypotension in uncomplicated hypertensive patients. Symptomatic hypotension is most likely to occur in patients who have been volume- and/or salt-depleted as a result of prolonged diuretic therapy, dietary salt restriction, dialysis, diarrhea, or vomiting. Correct volume-and salt-depletion before initiating therapy with ramipril.
If excessive hypotension occurs, place the patient in a supine position and, if necessary, treat with intravenous infusion of physiological saline. Ramipril treatment usually can be continued following restoration of blood pressure and volume.
Heart Failure Post-Myocardial Infarction
In patients with heart failure post-myocardial infarction who are currently being treated with a diuretic, symptomatic hypotension occasionally can occur following the initial dose of ramipril.
Congestive Heart Failure
In patients with congestive heart failure, with or without associated renal insufficiency, ACE inhibitor therapy may cause excessive hypotension, which may be associated with oliguria or azotemia and rarely, with acute renal failure and death.
Surgery and Anesthesia
In patients undergoing surgery or during anesthesia with agents that produce hypotension, ramipril may block angiotensin II formation that would otherwise occur secondary to compensatory renin release. Hypotension that occurs as a result of this mechanism can be corrected by volume expansion.
5.6 Fetal/Neonatal Morbidity and Mortality
Angiotensin converting enzyme inhibitors can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature. When pregnancy is detected, discontinue ACE inhibitors as soon as possible.
The use of ACE inhibitors during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal renal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation, and hypoplastic lung development. Prematurity, intrauterine growth retardation, and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were caused by the ACE inhibitor exposure.
In a published retrospective epidemiological study, infants whose mothers had taken an ACE inhibitor during their first trimester of pregnancy appeared to have an increased risk of major congenital malformations compared with infants whose mothers had not undergone first trimester exposure to ACE inhibitor drugs. The number of cases of birth defects is small and the findings of this study have not yet been confirmed.
Rarely (probably less than once in every thousand pregnancies), no alternative to a drug acting on the renin-angiotensin-aldosterone system will be found. In these rare cases, inform mothers about the potential hazards to their fetuses, and perform serial ultrasound examinations to assess the intraamniotic environment.
If oligohydramnios is observed, discontinue ramipril unless it is considered life-saving for the mother. Contraction stress testing, a nonstress test, or biophysical profiling may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Closely observe infants with histories of in utero exposure to ACE inhibitors for hypotension, oliguria, and hyperkalemia. If oliguria occurs, direct attention towards support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as a means of reversing hypotension and/or substituting for disordered renal function. Ramipril, which crosses the placenta, can be removed from the neonatal circulation by these means, but limited experience has not shown that such removal is central to the treatment of these infants.
5.7 Dual Blockade of the Renin-Angiotensin-Aldosterone System
Telmisartan
The ONTARGET trial enrolled 25,620 patients >55 years old with atherosclerotic disease or diabetes with end-organ damage, randomized them to telmisartan only, ramipril only, or the combination, and followed them for a median of 56 months. Patients receiving the combination of telmisartan and ramipril did not obtain any benefit compared to monotherapy, but experienced an increased incidence of clinically important renal dysfunction (death, doubling of serum creatinine, or dialysis) compared with groups receiving telmisartan alone or ramipril alone. Concomitant use of telmisartan and ramipril is not recommended.
5.8 Hyperkalemia
In clinical trials with ramipril, hyperkalemia (serum potassium > 5.7 mEq/L) occurred in approximately 1% of hypertensive patients receiving ramipril. In most cases, these were isolated values, which resolved despite continued therapy. None of these patients were discontinued from the trials because of hyperkalemia. Risk factors for the development of hyperkalemia include renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salt substitutes, which should be used cautiously, if at all, with ramipril [see Drug Interactions ( 7.1 )].
5.9 Cough
Presumably caused by inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with all ACE inhibitors, always resolving after discontinuation of therapy. Consider the possibility of angiotensin converting enzyme inhibitor induced-cough in the differential diagnosis of cough.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Hypertension
Ramipril has been evaluated for safety in over 4000 patients with hypertension; of these, 1230 patients were studied in U.S. controlled trials, and 1107 were studied in foreign controlled trials. Almost 700 of these patients were treated for at least one year. The overall incidence of reported adverse events was similar in ramipril and placebo patients. The most frequent clinical side effects (possibly or probably related to study drug) reported by patients receiving ramipril in placebo-controlled trials were: headache (5.4%), dizziness (2.2%), and fatigue or asthenia (2.0%), but only the last one was more common in ramipril patients than in patients given placebo. Generally the side effects were mild and transient, and there was no relation to total dosage within the range of 1.25 mg to 20 mg. Discontinuation of therapy because of a side effect was required in approximately 3% of U.S. patients treated with ramipril. The most common reasons for discontinuation were: cough (1.0%), dizziness (0.5%), and impotence (0.4%).Of observed side effects considered possibly or probably related to study drug that occurred in U.S. placebo-controlled trials in more than 1% of patients treated with ramipril, only asthenia (fatigue) was more common on ramipril than placebo (2% [n = 13/651] vs. 1% [n = 2/286], respectively).
In placebo-controlled trials, there was also an excess of upper respiratory infection and flu syndrome in the ramipril group, not attributed at that time to ramipril. As these studies were carried out before the relationship of cough to ACE inhibitors was recognized, some of these events may represent ramipril-induced cough. In a later 1 year study, increased cough was seen in almost 12% of ramipril patients, with about 4% of patients requiring discontinuation of treatment.
Other Adverse Reactions
Other adverse reactions reported in controlled clinical trials (in less than 1% of ramipril patients), or rarer events seen in post-marketing experience, include the following (in some, a causal relationship to drug is uncertain):
Body as a whole: Anaphylactoid reactions [see Warnings and Precautions ( 5.1 )].
Cardiovascular: Symptomatic hypotension (reported in 0.5% of patients in U.S. trials) [see Warnings and Precautions( 5.5 )], syncope, and palpitations.
Hematologic: Pancytopenia, hemolytic anemia, and thrombocytopenia. Decreases in hemoglobin or hematocrit (a low value and a decrease of 5 g/dL or 5%, respectively) were rare, occurring in 0.4% of patients receiving ramipril alone and in 1.5% of patients receiving ramipril plus a diuretic.
Renal: Acute renal failure. Some hypertensive patients with no apparent preexisting renal disease have developed minor, usually transient, increases in blood urea nitrogen and serum creatinine when taking ramipril, particularly when ramipril was given concomitantly with a diuretic [see Warnings and Precautions ( 5.3 )].
Angioneurotic edema: Angioneurotic edema has been reported in 0.3% of patients in U.S. clinical trials of ramipril [seeWarnings and Precautions (5.1 )].
Gastrointestinal: Hepatic failure, hepatitis, jaundice, pancreatitis, abdominal pain (sometimes with enzyme changes suggesting pancreatitis), anorexia, constipation, diarrhea, dry mouth, dyspepsia, dysphagia, gastroenteritis, increased salivation, and taste disturbance.
Dermatologic: Apparent hypersensitivity reactions (manifested by urticaria, pruritus, or rash, with or without fever), photosensitivity, purpura, onycholysis, pemphigus, pemphigoid, erythema multiforme, toxic epidermal necrolysis, and Stevens-Johnson syndrome.
Neurologic and Psychiatric: Anxiety, amnesia, convulsions, depression, hearing loss, insomnia, nervousness, neuralgia, neuropathy, paresthesia, somnolence, tinnitus, tremor, vertigo, and vision disturbances.
Miscellaneous: As with other ACE inhibitors, a symptom complex has been reported which may include a positive ANA, an elevated erythrocyte sedimentation rate, arthralgia/arthritis, myalgia, fever, vasculitis, eosinophilia, photosensitivity, rash and other dermatologic manifestations. Additionally, as with other ACE inhibitors, eosinophilic pneumonitis has been reported.
Other: Arthralgia, arthritis, dyspnea, edema, epistaxis, impotence, increased sweating, malaise, myalgia, and weight gain.
6.2 Post-marketing Experience
In addition to adverse reactions reported from clinical trials, there have been rare reports of hypoglycemia reported during ramipril therapy when given to patients concomitantly taking oral hypoglycemic agents or insulin. The causal relationship is unknown.
6.3 Clinical Laboratory Test Findings
Creatinine and Blood Urea Nitrogen: Increases in creatinine levels occurred in 1.2% of patients receiving ramipril alone, and in 1.5% of patients receiving ramipril and a diuretic. Increases in blood urea nitrogen levels occurred in 0.5% of patients receiving ramipril alone and in 3% of patients receiving ramipril with a diuretic. None of these increases required discontinuation of treatment. Increases in these laboratory values are more likely to occur in patients with renal insufficiency or those pretreated with a diuretic and, based on experience with other ACE inhibitors, would be expected to be especially likely in patients with renal artery stenosis [see Warnings and Precautions (5.3 )]. As ramipril decreases aldosterone secretion, elevation of serum potassium can occur. Use potassium supplements and potassium sparing diuretics with caution, and monitor the patient’s serum potassium frequently [see Warnings and Precautions (5.8 )].
Hemoglobin and Hematocrit: Decreases in hemoglobin or hematocrit (a low value and a decrease of 5 g/dL or 5%, respectively) were rare, occurring in 0.4% of patients receiving ramipril alone and in 1.5% of patients receiving ramipril plus a diuretic. No U.S. patients discontinued treatment because of decreases in hemoglobin or hematocrit.
Other (causal relationships unknown): Clinically important changes in standard laboratory tests were rarely associated with ramipril administration. Elevations of liver enzymes, serum bilirubin, uric acid, and blood glucose have been reported, as have cases of hyponatremia and scattered incidents of leucopenia, eosinophilia, and proteinuria. In U.S. trials, less than 0.2% of patients discontinued treatment for laboratory abnormalities; all of these were cases of proteinuria or abnormal liver-function tests.
7 DRUG INTERACTIONS
7.1 Diuretics
Patients on diuretics, especially those in whom diuretic therapy was recently instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with ramipril. The possibility of hypotensive effects with ramipril can be minimized by either decreasing or discontinuing the diuretic or increasing the salt intake prior to initiation of treatment with ramipril. If this is not possible, reduce the starting dose [see DOSAGE AND ADMINISTRATION ( 2 )].
Ramipril can attenuate potassium loss caused by thiazide diuretics. Potassium-sparing diuretics (spironolactone, amiloride, triamterene, and others) or potassium supplements can increase the risk of hyperkalemia. Therefore, if concomitant use of such agents is indicated, monitor the patient’s serum potassium frequently.
7.2 Other Antihypertensive Agents
Limited experience in controlled and uncontrolled trials combining ramipril with a calcium channel blocker, a loop diuretic, or triple therapy (beta-blocker, vasodilator, and a diuretic) indicate no unusual drug-drug interactions. Other ACE inhibitors have had less than additive effects with beta adrenergic blockers, presumably because both drug classes lower blood pressure by inhibiting parts of the renin-angiotensin-aldosterone system.
The combination of ramipril and propranolol showed no adverse effects on dynamic parameters (blood pressure and heart rate).
In a large-scale, long-term clinical efficacy study, the combination of telmisartan and ramipril resulted in an increased incidence of clinically important renal dysfunction (death, doubling of serum creatinine, dialysis) compared with groups receiving either drug alone. Therefore, concomitant use of telmisartan and ramipril is not recommended [see Dual Blockade of the Renin-Angiotensin-Aldosterone System (5.7 )].
7.3 Lithium
Increased serum lithium levels and symptoms of lithium toxicity have been reported in patients receiving ACE inhibitors during therapy with lithium; therefore, frequent monitoring of serum lithium levels is recommended. If a diuretic is also used, the risk of lithium toxicity may be increased.
7.4 Gold
Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy including ramipril.
7.5 Other
Neither ramipril nor its metabolites have been found to interact with food, digoxin, antacid, furosemide, cimetidine, indomethacin, and simvastatin. The co-administration of ramipril and warfarin did not adversely affect the anticoagulation effects of the latter drug. Additionally, coadministration of ramipril with phenprocoumon did not affect minimum phenprocoumon levels or interfere with the patients’ state of anticoagulation. Rarely, concomitant treatment with ACE inhibitors and non-steroidal anti-inflammatory agents have been associated with worsening of renal failure and an increase in serum potassium.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Categories C (first trimester) and D (second and third trimesters) [see Warnings and Precautions (5.6 )].
8.3 Nursing Mothers
Ingestion of a single 10 mg oral dose of ramipril resulted in undetectable amounts of ramipril and its metabolites in breast milk. However, because multiple doses may produce low milk concentrations that are not predictable from a single dose, do not use ramipril in nursing mothers.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Irreversible kidney damage has been observed in very young rats given a single dose of ramipril.
8.5 Geriatric Use
Of the total number of patients who received ramipril in U.S. clinical studies of ramipril, 11.0% were ≥ 65 years of age while 0.2% were ≥ 75 years of age. No overall differences in effectiveness or safety were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but a greater sensitivity of some older individuals cannot be ruled out.
One pharmacokinetic study conducted in hospitalized elderly patients indicated that peak ramiprilat levels and area under the plasma concentration-time curve (AUC) for ramiprilat are higher in older patients.
8.6 Renal Impairment
A single-dose pharmacokinetic study was conducted in hypertensive patients with varying degrees of renal impairment who received a single 10 mg dose of ramipril. Patients were stratified into four groups based on initial estimates of creatinine clearance: normal (>80 mL/min), mild impairment (40 to 80 mL/min), moderate impairment (15 to 40 mL/min), and severe impairment (< 15 mL/min). On average, the AUC0-24h for ramiprilat was approximately 1.7 fold higher, 3.0 fold higher, and 3.2-fold higher in the groups with mild, moderate, and severe renal impairment, respectively, compared to the group with normal renal function. Overall, the results suggest that the starting dose of ramipril should be adjusted downward in patients with moderate-to-severe renal impairment.
10 OVERDOSAGE
Single oral doses of ramipril in rats and mice of 10 g/kg to 11 g/kg resulted in significant lethality. In dogs, oral doses as high as 1 g/kg induced only mild gastrointestinal distress. Limited data on human overdosage are available. The most likely clinical manifestations would be symptoms attributable to hypotension.
Laboratory determinations of serum levels of ramipril and its metabolites are not widely available, and such determinations have, in any event, no established role in the management of ramipril overdose.
No data are available to suggest physiological maneuvers (e.g., maneuvers to change the pH of the urine) that might accelerate elimination of ramipril and its metabolites. Similarly, it is not known which, if any, of these substances can be effectively removed from the body by hemodialysis.
Angiotensin II could presumably serve as a specific antagonist-antidote in the setting of ramipril overdose, but angiotensin II is essentially unavailable outside of scattered research facilities. Because the hypotensive effect of ramipril is achieved through vasodilation and effective hypovolemia, it is reasonable to treat ramipril overdose by infusion of normal saline solution.
11 DESCRIPTION
Ramipril is a 2-aza-bicyclo[3.3.0]-octane-3-carboxylic acid derivative. It is a white or almost white crystalline powder soluble in polar organic solvents and buffered aqueous solutions. Ramipril melts between 105°C and 112°C.
The CAS Registry Number is 87333-19-5. Ramipril's chemical name is (2S ,3aS ,6aS)-1[(S)-N-[(S)-1-carboxy-3-phenylpropyl] alanyl]octahydrocyclopenta[b]pyrrole-2-carboxylic acid, 1-ethyl ester.
Ramipril capsules, USP are supplied as hard shell capsules for oral administration containing 1.25 mg, 2.5 mg, 5 mg, and 10 mg of ramipril. The inactive ingredients present are pregelatinized starch NF, gelatin, and titanium dioxide. The 1.25 mg capsule shell contains D&C Yellow # 10 and FD&C Yellow # 6 the 2.5 mg capsule shell contains D&C Red # 28, D&C Yellow # 10 and FD&C Red #40, the 5 mg capsule shell contains D&C Red # 28, D&C Red # 33, D&C Yellow # 10 and FD&C Blue #1, and the 10 mg capsule shell contains D&C Red # 28, and FD&C Blue #1. Capsule shells are imprinted with ink containing Shellac and Black iron oxide.
The structural formula for ramipril is:
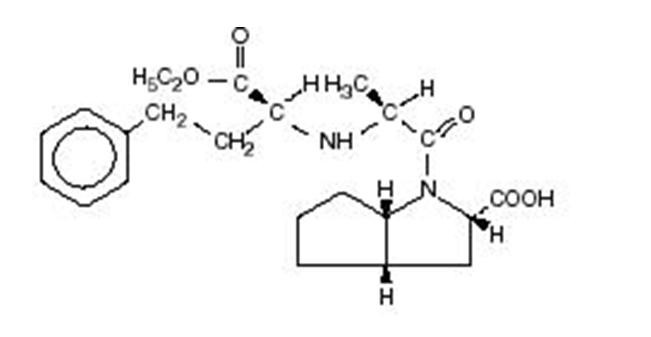
Its empirical formula is C23H32N2O5 and its molecular weight is 416.5.
Ramiprilat, the diacid metabolite of ramipril, is a non-sulfhydryl ACE inhibitor. Ramipril is converted to ramiprilat by hepatic cleavage of the ester group.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ramipril and ramiprilat inhibit ACE in human subjects and animals. Angiotensin converting enzyme is a peptidyl dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also stimulates aldosterone secretion by the adrenal cortex. Inhibition of ACE results in decreased plasma angiotensin II, which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a small increase of serum potassium. In hypertensive patients with normal renal function treated with ramipril alone for up to 56 weeks, approximately 4% of patients during the trial had an abnormally high serum potassium and an increase from baseline greater than 0.75 mEq/L, and none of the patients had an abnormally low potassium and a decrease from baseline greater than 0.75 mEq/L. In the same study, approximately 2% of patients treated with ramipril and hydrochlorothiazide for up to 56 weeks had abnormally high potassium values and an increase from baseline of 0.75 mEq/L or greater; and approximately 2% had abnormally low values and decreases from baseline of 0.75 mEq/L or greater [see Warnings and Precautions (5.8 )]. Removal of angiotensin II negative feedback on renin secretion leads to increased plasma renin activity.
The effect of ramipril on hypertension appears to result at least in part from inhibition of both tissue and circulating ACE activity, thereby reducing angiotensin II formation in tissue and plasma.
Angiotensin converting enzyme is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasopressor peptide, play a role in the therapeutic effects of ramipril remains to be elucidated.
While the mechanism through which ramipril lowers blood pressure is believed to be primarily suppression of the renin-angiotensin-aldosterone system, ramipril has an antihypertensive effect even in patients with low-renin hypertension. Although ramipril was antihypertensive in all races studied, Black hypertensive patients (usually a low-renin hypertensive population) had a blood pressure lowering response to monotherapy, albeit a smaller average response, than non-Black patients.
12.2 Pharmacodynamics
Single doses of ramipril of 2.5 mg to 20 mg produce approximately 60% to 80% inhibition of ACE activity 4 hours after dosing with approximately 40% to 60% inhibition after 24 hours. Multiple oral doses of ramipril of 2.0 mg or more cause plasma ACE activity to fall by more than 90% 4 hours after dosing, with over 80% inhibition of ACE activity remaining 24 hours after dosing. The more prolonged effect of even small multiple doses presumably reflects saturation of ACE binding sites by ramiprilat and relatively slow release from those sites.
12.3 Pharmacokinetics
Absorption
Following oral administration of ramipril, peak plasma concentrations (Cmax) of ramipril are reached within 1 hour. The extent of absorption is at least 50% to 60%, and is not significantly influenced by the presence of food in the gastrointestinal tract, although the rate of absorption is reduced.
In a trial in which subjects received ramipril capsules or the contents of identical capsules dissolved in water, dissolved in apple juice, or suspended in applesauce, serum ramiprilat levels were essentially unrelated to the use or non-use of the concomitant liquid or food.
Distribution
Cleavage of the ester group (primarily in the liver) converts ramipril to its active diacid metabolite, ramiprilat. Peak plasma concentrations of ramiprilat are reached 2 to 4 hours after drug intake. The serum protein binding of ramipril is about 73% and that of ramiprilat about 56%; in vitro, these percentages are independent of concentration over the range of 0.01 mcg/mL to 10 mcg/mL.
Metabolism
Ramipril is almost completely metabolized to ramiprilat, which has about 6 times the ACE inhibitory activity of ramipril, and to the diketopiperazine ester, the diketopiperazine acid, and the glucuronides of ramipril and ramiprilat, all of which are inactive.
Plasma concentrations of ramipril and ramiprilat increase with increased dose, but are not strictly dose-proportional. The 24-hour AUC for ramiprilat, however, is dose-proportional over the 2.5 mg to 20 mg dose range. The absolute bioavailabilities of ramipril and ramiprilat were 28% and 44%, respectively, when 5 mg of oral ramipril was compared with the same dose of ramipril given intravenously.
After once-daily dosing, steady-state plasma concentrations of ramiprilat are reached by the fourth dose. Steady-state concentrations of ramiprilat are somewhat higher than those seen after the first dose of ramipril, especially at low doses (2.5 mg), but the difference is clinically insignificant.
Plasma concentrations of ramiprilat decline in a triphasic manner (initial rapid decline, apparent elimination phase, terminal elimination phase). The initial rapid decline, which represents distribution of the drug into a large peripheral compartment and subsequent binding to both plasma and tissue ACE, has a half-life of 2 to 4 hours. Because of its potent binding to ACE and slow dissociation from the enzyme, ramiprilat shows two elimination phases. The apparent elimination phase corresponds to the clearance of free ramiprilat and has a half-life of 9 to 18 hours. The terminal elimination phase has a prolonged half-life (> 50 hours) and probably represents the binding/dissociation kinetics of the ramiprilat/ACE complex. It does not contribute to the accumulation of the drug. After multiple daily doses of ramipril 5 mg to 10 mg, the half-life of ramiprilat concentrations within the therapeutic range was 13 to 17 hours.
In patients with creatinine clearance < 40 mL/min/1.73 m2, peak levels of ramiprilat are approximately doubled, and trough levels may be as much as quintupled. In multiple-dose regimens, the total exposure to ramiprilat (AUC) in these patients is 3 to 4 times as large as it is in patients with normal renal function who receive similar doses.
In patients with impaired liver function, the metabolism of ramipril to ramiprilat appears to be slowed, possibly because of diminished activity of hepatic esterases, and plasma ramipril levels in these patients are increased about 3 fold. Peak concentrations of ramiprilat in these patients, however, are not different from those seen in subjects with normal hepatic function, and the effect of a given dose on plasma ACE activity does not vary with hepatic function.
Excretion
After oral administration of ramipril, about 60% of the parent drug and its metabolites are eliminated in the urine, and about 40% is found in the feces. Drug recovered in the feces may represent both biliary excretion of metabolites and/or unabsorbed drug, however the proportion of a dose eliminated by the bile has not been determined. Less than 2% of the administered dose is recovered in urine as unchanged ramipril.
The urinary excretion of ramipril, ramiprilat, and their metabolites is reduced in patients with impaired renal function. Compared to normal subjects, patients with creatinine clearance < 40 mL/min/1.73 m2 had higher peak and trough ramiprilat levels and slightly longer times to peak concentrations.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
No evidence of a tumorigenic effect was found when ramipril was given by gavage to rats for up to 24 months at doses of up to 500 mg/kg/day or to mice for up to 18 months at doses of up to 1000 mg/kg/day. (For either species, these doses are about 200 times the maximum recommended human dose when compared on the basis of body surface area.) No mutagenic activity was detected in the Ames test in bacteria, the micronucleus test in mice, unscheduled DNA synthesis in a human cell line, or a forward gene-mutation assay in a Chinese hamster ovary cell line. Several metabolites and degradation products of ramipril were also negative in the Ames test. A study in rats with dosages as great as 500 mg/kg/day did not produce adverse effects on fertility.
No teratogenic effects of ramipril were seen in studies of pregnant rats, rabbits, and cynomolgus monkeys. On a body surface area basis, the doses used were up to approximately 400 times (in rats and monkeys) and 2 times (in rabbits) the recommended human dose.
14 CLINICAL STUDIES
14.1 Hypertension
Ramipril has been compared with other ACE inhibitors, beta-blockers, and thiazide diuretics as monotherapy for hypertension. It was approximately as effective as other ACE inhibitors and as atenolol.
Administration of ramipril to patients with mild to moderate hypertension results in a reduction of both supine and standing blood pressure to about the same extent with no compensatory tachycardia. Symptomatic postural hypotension is infrequent, although it can occur in patients who are salt- and/or volume-depleted [see Warnings and Precautions (5.5 )]. Use of ramipril in combination with thiazide diuretics gives a blood pressure lowering effect greater than that seen with either agent alone.
In single-dose studies, doses of 5 mg to 20 mg of ramipril lowered blood pressure within 1 to 2 hours, with peak reductions achieved 3 to 6 hours after dosing. The antihypertensive effect of a single dose persisted for 24 hours. In longer term (4 to 12 weeks) controlled studies, once-daily doses of 2.5 mg to 10 mg were similar in their effect, lowering supine or standing systolic and diastolic blood pressures 24 hours after dosing by about 6/4 mmHg more than placebo. In comparisons of peak vs. trough effect, the trough effect represented about 50 to 60% of the peak response. In a titration study comparing divided (bid) vs. qd treatment, the divided regimen was superior, indicating that for some patients, the antihypertensive effect with once-daily dosing is not adequately maintained.
In most trials, the antihypertensive effect of ramipril increased during the first several weeks of repeated measurements. The antihypertensive effect of ramipril has been shown to continue during long-term therapy for at least 2 years. Abrupt withdrawal of ramipril has not resulted in a rapid increase in blood pressure. Ramipril has been compared with other ACE inhibitors, beta-blockers, and thiazide diuretics. Ramipril was approximately as effective as other ACE inhibitors and as atenolol. In both Caucasians and Blacks, hydrochlorothiazide (25 or 50 mg) was significantly more effective than ramipril. Ramipril was less effective in Blacks than in Caucasians. The effectiveness of ramipril was not influenced by age, sex, or weight.
In a baseline controlled study of 10 patients with mild essential hypertension, blood pressure reduction was accompanied by a 15% increase in renal blood flow. In healthy volunteers, glomerular filtration rate was unchanged.
16 HOW SUPPLIED/STORAGE AND HANDLING
Ramipril capsules, USP are available as 1.25 mg, 2.5 mg, 5 mg, and 10 mg in hard gelatin capsules.
Ramipril 1.25 mg capsules are hard gelatin capsules size "4", yellow opaque body with yellow opaque cap imprinted with IG271 on cap and 1.25 mg on body in black ink, filled with white to off-white powder and supplied in bottles of 100 (NDC 76282-271-01), 500 (76282-271-05) and 1000 (NDC 76282-271-10).
Ramipril 2.5 mg capsules are hard gelatin capsules size "4", orange opaque body with orange opaque cap imprinted with IG272 on cap and 2.5 mg on body in black ink, filled with white to off-white powder and supplied in bottles of 100 (NDC 76282-272-01), 500 (NDC 76282-272-05) and 1000 (NDC 76282-272-10).
Ramipril 5 mg capsules are hard gelatin capsules size "4", red opaque body with red opaque cap imprinted with IG273 on cap and 5 mg on body in black ink, filled with white to off-white powder and supplied in bottles of 100 (NDC 76282-273-01), 500 (NDC 76282-273-05) and 1000 (NDC 76282-273-10).
Ramipril 10 mg capsules are hard gelatin capsules size "4", blue opaque body with blue opaque cap imprinted with IG274 on cap and 10 mg on body in black ink, filled with white to off-white powder and supplied in bottles of 100 (NDC 76282-274-01), 500 (NDC 76282-274-05) and 1000 (NDC 76282-274-10).
Dispense in well-closed container with safety closure.
Store at controlled room temperature between 20° and 25°C (68° and 77°F) (See USP).
17 PATIENT COUNSELING INFORMATION
17.1 Angioedema
Angioedema, including laryngeal edema, can occur rarely with treatment with ACE inhibitors, especially following the first dose. Advise patients to report immediately any signs or symptoms suggesting angioedema (swelling of face, eyes, lips, or tongue, or difficulty in breathing) and to take no more drug until they have consulted with the prescribing physician.
17.2 Neutropenia
Advise patients to report promptly any indication of infection (e.g., sore throat, fever), which could be a sign of neutropenia.
17.3 Symptomatic Hypotension
Inform patients that light-headedness can occur, especially during the first days of therapy, and it should be reported.
Advise patients to discontinue ramipril if syncope (fainting) occurs, and to follow up with their health care providers. Inform patients that inadequate fluid intake or excessive perspiration, diarrhea, or vomiting while taking ramipril can lead to an excessive fall in blood pressure, with the same consequences of lightheadedness and possible syncope.
17.4 Pregnancy
Inform female patients of childbearing age about the consequences of exposure to ACE inhibitors during pregnancy. Advise these patients to report pregnancies to their physicians as soon as possible.
17.5 Hyperkalemia
Advise patients not to use salt substitutes containing potassium without consulting their physician.
Manufactured for:
Exelan Pharmaceuticals, Inc.
Peachtree City, GA 30269
Manufactured by:
InvaGen Pharmaceuticals, Inc.
Hauppauge, NY11788
Rev: 07/11
Barcode:
271-07-2011
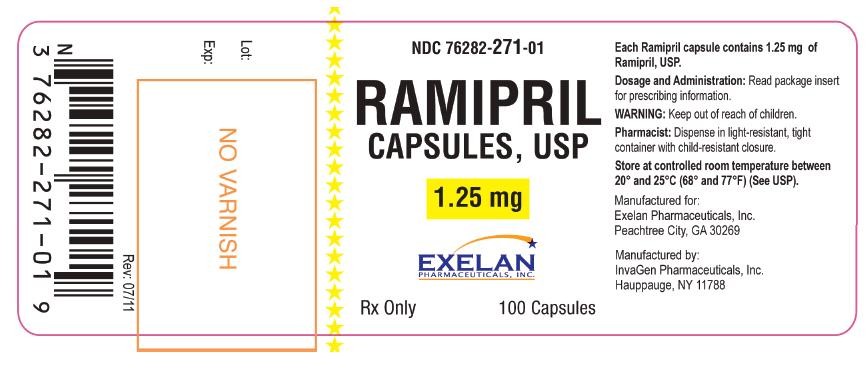
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL 1.25 mg
NDC 76282-271-01
RAMIPRIL
CAPSULES, USP
1.25 mg
EXCELAN PHARMACEUTICALS, INC.
Rx Only
100 Capsules
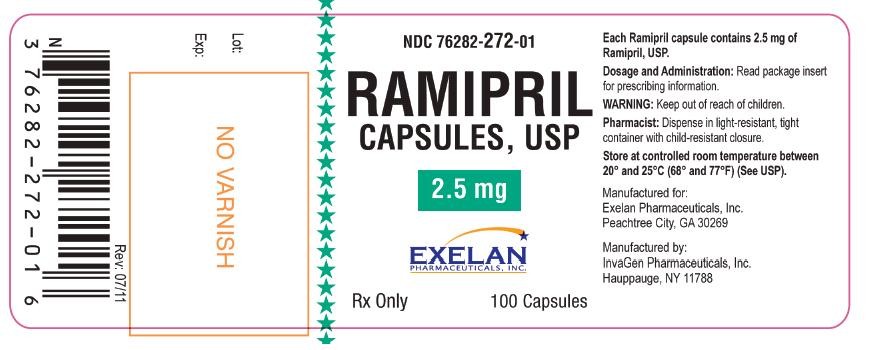
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL 2.5 mg
NDC 76282-272-01
RAMIPRIL
CAPSULES, USP
2.5 mg
EXCELAN PHARMACEUTICALS, INC.
Rx Only
100 Capsules
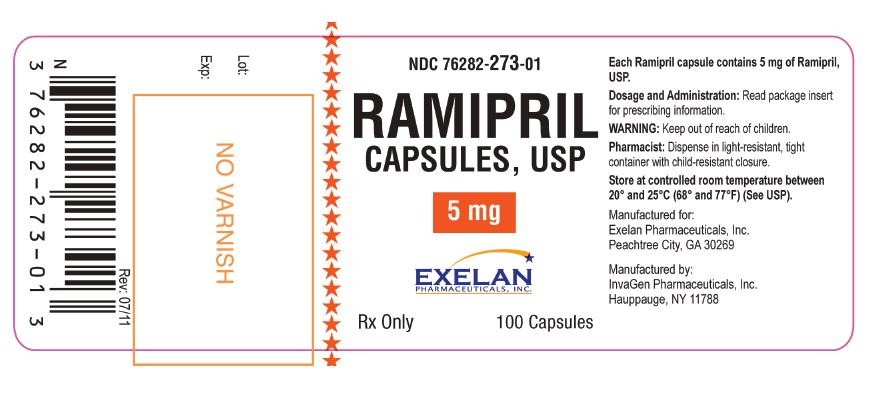
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL 5 mg
NDC 76282-273-01
RAMIPRIL
CAPSULES, USP
5 mg
EXCELAN PHARMACEUTICALS, INC.
Rx Only
100 Capsules
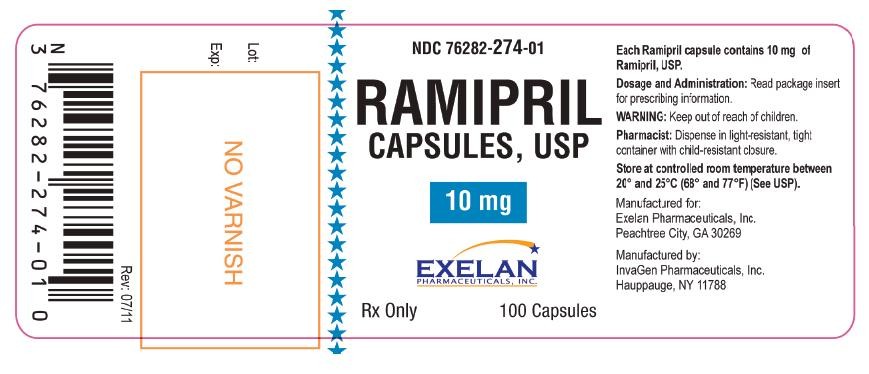
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL 10 mg
NDC 76282-274-01
RAMIPRIL
CAPSULES, USP
10 mg
EXCELAN PHARMACEUTICALS, INC.
Rx Only
100 Capsules
RamiprilRamipril CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
RamiprilRamipril CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
RamiprilRamipril CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
RamiprilRamipril CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||