Rabeprazole Sodium
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use rabeprazole sodium delayed-release tablets safely and effectively. See full prescribing information for rabeprazole sodium delayed-release tablets.RABEPRAZOLE sodium delayed-release tablets, for oral use Initial U.S. Approval: 1999RECENT MAJOR CHANGESWarnings and Precautions, Clostridium difficile Associated Diarrhea (5.3) 10/2012Warnings and Precautions, Concomitant Use of Rabeprazole With Methotrexate (5.6) 05/2012INDICATIONS AND USAGERabeprazole sodium delayed-release tablets are a proton-pump inhibitor (PPI) indicated in adults for: Healing of Erosive or Ulcerative Gastroesophageal Reflux Disease (GERD) (1.1) Maintenance of Healing of Erosive or Ulcerative GERD (1.2) Treatment of Symptomatic GERD (1.3) Healing of Duodenal Ulcers (1.4) Helicobacter pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence (1.5) Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome (1.6) In adolescent patients 12 years of age and older for: Short-term treatment of Symptomatic GERD (1.7) DOSAGE AND ADMINISTRATIONRabeprazole sodium delayed-release tablets should be swallowed whole. The tablets should not be chewed, crushed or split (2.10). Healing of Erosive or Ulcerative Gastroesophageal Reflux Disease (GERD) (2.1) 20 mg once daily Maintenance of Healing of Erosive or Ulcerative GERD (2.2) 20 mg once daily Treatment of Symptomatic GERD in Adults (2.3) 20 mg once daily Healing of Duodenal Ulcers (2.4) 20 mg once daily after morning meal Helicobacter pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence (2.5) Three Drug Regimen: All three medications should be taken twice daily with morning and evening meals for 7 days Rabeprazole sodium delayed-release 20 mg Amoxicillin 1000 mg Clarithromycin 500 mg Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome (2.6) Starting dose 60 mg once daily then adjust to patient needs Treatment of Symptomatic GERD in Adolescents 12 Years of Age and Older (2.7) 20 mg once daily DOSAGE FORMS AND STRENGTHSDelayed-Release Tablets: 20 mg (3)CONTRAINDICATIONS History of hypersensitivity to rabeprazole (4) WARNINGS AND PRECAUTIONS Symptomatic response to therapy with rabeprazole does not preclude the presence of gastric malignancy (5.1) Use with warfarin: monitor for increases in INR and prothrombin time (5.2) PPI therapy may be associated with increased risk of Clostridium difficile associated diarrhea (5.3) Bone fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine (5.4) Hypomagnesemia has been reported rarely with prolonged treatment with PPIs (5.5) Side Effects In the adult studies (4 to 8 weeks), adverse reactions that occurred at a rate greater than 2% and greater than placebo included pain, pharyngitis, flatulence, infection and constipation (6.1) In studies of adolescent patients (ages 12 to 16 years, and up to 36 weeks exposure) adverse reactions that occurred at a rate of ≥ 5% of patients included abdominal pain, diarrhea and headache (6.1) To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537 or drug.safety@tevapharm.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Increased INR and prothrombin times have been reported with concomitant use with warfarin. Patients need to be monitored (7.2) Rabeprazole has been shown to inhibit cyclosporine metabolism in vitro (7.3) Rabeprazole inhibits gastric acid secretion and may interfere with the absorption of drugs where gastric pH is an important determinant of bioavailability (e.g., ketoconazole, iron salts and digoxin) (7.4) Rabeprazole may reduce the plasma levels of atazanavir (7.4) Methotrexate: Rabeprazole may increase serum level of methotrexate (7.7) USE IN SPECIFIC POPULATIONS Studies conducted do not support the use of rabeprazole sodium delayed-release tablets for the treatment of GERD in pediatric patients younger than 12 years of age (8.4). The safety and efficacy of rabeprazole sodium delayed-release tablets for GERD have not been established for pediatric patients less than 12 years of age (8.4).
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 RABEPRAZOLE SODIUM INDICATIONS AND USAGE
- 1.1 Healing of Erosive or Ulcerative GERD in Adults
- 1.2 Maintenance of Healing of Erosive or Ulcerative GERD in Adults
- 1.3 Treatment of Symptomatic GERD in Adults
- 1.4 Healing of Duodenal Ulcers in Adults
- 1.5 Eradication to Reduce the Risk of Duodenal Ulcer Recurrence in Adults
- 1.6 Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
- 1.7 Short-Term Treatment of Symptomatic GERD in Adolescent Patients 12 Years of Age and Older
- 2 RABEPRAZOLE SODIUM DOSAGE AND ADMINISTRATION
- 2.1 Healing of Erosive or Ulcerative GERD in Adults
- 2.2 Maintenance of Healing of Erosive or Ulcerative GERD in Adults
- 2.3 Treatment of Symptomatic GERD in Adults
- 2.4 Healing of Duodenal Ulcers in Adults
- 2.5 Eradication to Reduce the Risk of Duodenal Ulcer Recurrence in Adults
- 2.6 Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
- 2.7 Short-Term Treatment of Symptomatic GERD in Adolescent Patients 12 Years of Age and Older
- 2.9 Elderly, Renal and Hepatic Impaired Patients
- 2.10 Administration Recommendations
- 3 DOSAGE FORMS AND STRENGTHS
- 4 RABEPRAZOLE SODIUM CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 RABEPRAZOLE SODIUM ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 10 OVERDOSAGE
- 11 RABEPRAZOLE SODIUM DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 14.1 Healing of Erosive or Ulcerative GERD in Adults
- 14.2 Long-Term Maintenance of Healing of Erosive or Ulcerative GERD in Adults
- 14.3 Treatment of Symptomatic GERD in Adults
- 14.4 Healing of Duodenal Ulcers in Adults
- 14.5 Eradication in Patients With Peptic Ulcer Disease or Symptomatic Non-Ulcer Disease in Adults
- 14.6 Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
- 14.7 Pediatric GERD
- 15 REFERENCES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- MEDICATION GUIDE
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Healing of Erosive or Ulcerative GERD in Adults
Rabeprazole sodium delayed-release tablets are indicated for short-term (4 to 8 weeks) treatment in the healing and symptomatic relief of erosive or ulcerative gastroesophageal reflux disease (GERD). For those patients who have not healed after 8 weeks of treatment, an additional 8 week course of rabeprazole sodium delayed-release tablets may be considered.
1.2 Maintenance of Healing of Erosive or Ulcerative GERD in Adults
Rabeprazole sodium delayed-release tablets are indicated for maintaining healing and reduction in relapse rates of heartburn symptoms in patients with erosive or ulcerative gastroesophageal reflux disease (GERD Maintenance). Controlled studies do not extend beyond 12 months.
1.3 Treatment of Symptomatic GERD in Adults
Rabeprazole sodium delayed-release tablets are indicated for the treatment of daytime and nighttime heartburn and other symptoms associated with GERD in adults.
1.4 Healing of Duodenal Ulcers in Adults
Rabeprazole sodium delayed-release tablets are indicated for short-term (up to four weeks) treatment in the healing and symptomatic relief of duodenal ulcers. Most patients heal within four weeks.
1.5 Eradication to Reduce the Risk of Duodenal Ulcer Recurrence in Adults
Rabeprazole sodium delayed-release tablets in combination with amoxicillin and clarithromycin as a three drug regimen, is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or history within the past 5 years) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Clinical Studies (14.5) and Dosage and Administration (2.5)].
In patients who fail therapy, susceptibility testing should be done. If resistance to clarithromycin is demonstrated or susceptibility testing is not possible, alternative antimicrobial therapy should be instituted [see Clinical Pharmacology (12.2) and the clarithromycin package insert, Clinical Pharmacology (12.2)].
1.6 Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
Rabeprazole sodium delayed-release tablets are indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison syndrome.
1.7 Short-Term Treatment of Symptomatic GERD in Adolescent Patients 12 Years of Age and Older
Rabeprazole sodium delayed-release tablets are indicated for the treatment of symptomatic GERD in adolescents 12 years of age and above for up to 8 weeks.
2 DOSAGE AND ADMINISTRATION
2.1 Healing of Erosive or Ulcerative GERD in Adults
The recommended adult oral dose is one rabeprazole sodium 20 mg delayed-release tablet to be taken once daily for four to eight weeks [see Indications and Usage (1.1)]. For those patients who have not healed after 8 weeks of treatment, an additional 8 week course of rabeprazole sodium delayed-release tablets may be considered.
2.2 Maintenance of Healing of Erosive or Ulcerative GERD in Adults
The recommended adult oral dose is one rabeprazole sodium 20 mg delayed-release tablet to be taken once daily [see Indications and Usage (1.2)].
2.3 Treatment of Symptomatic GERD in Adults
The recommended adult oral dose is one rabeprazole sodium 20 mg delayed-release tablet to be taken once daily for 4 weeks [see Indications and Usage (1.3)]. If symptoms do not resolve completely after 4 weeks, an additional course of treatment may be considered. The recommended adolescent dosing is one rabeprazole sodium 20 mg delayed-release tablet to be taken once daily for 8 weeks.
2.4 Healing of Duodenal Ulcers in Adults
The recommended adult oral dose is one rabeprazole sodium 20 mg delayed-release tablet to be taken once daily after the morning meal for a period up to four weeks [see Indications and Usage (1.5)]. Most patients with duodenal ulcer heal within four weeks. A few patients may require additional therapy to achieve healing.
2.5 Eradication to Reduce the Risk of Duodenal Ulcer Recurrence in Adults
| Rabeprazole Sodium Delayed-Release Tablet | 20 mg | Twice Daily for 7 Days |
| Amoxicillin | 1000 mg | Twice Daily for 7 Days |
| Clarithromycin | 500 mg | Twice Daily for 7 Days |
| All three medications should be taken twice daily with the morning and evening meals. | ||
2.6 Treatment of Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
The dosage of rabeprazole sodium delayed-release tablets in patients with pathologic hypersecretory-conditions varies with the individual patient. The recommended adult oral starting dose is 60 mg once daily. Doses should be adjusted to individual patient needs and should continue for as long as clinically indicated. Some patients may require divided doses. Doses up to 100 mg QD and 60 mg BID have been administered. Some patients with Zollinger-Ellison syndrome have been treated continuously with rabeprazole sodium delayed-release tablets for up to one year.
2.7 Short-Term Treatment of Symptomatic GERD in Adolescent Patients 12 Years of Age and Older
The recommended oral dose for adolescents 12 years of age and older is one 20 mg delayed-release tablet once daily for up to 8 weeks [see Use in Specific Populations (8.4) and Clinical Studies (14.7)].
2.9 Elderly, Renal and Hepatic Impaired Patients
No dosage adjustment is necessary in elderly patients, in patients with renal disease or in patients with mild to moderate hepatic impairment. Administration of rabeprazole to patients with mild to moderate liver impairment resulted in increased exposure and decreased elimination. Due to the lack of clinical data on rabeprazole in patients with severe hepatic impairment, caution should be exercised in those patients.
2.10 Administration Recommendations
| Formulation | Population | Instructions |
| Delayed-Release Tablet | Adults and adolescents 12 years of age and older |
Swallow tablets whole. Do not chew, crush or split tablets. Tablets can be taken with or without food. |
3 DOSAGE FORMS AND STRENGTHS
Rabeprazole sodium delayed-release tablets are provided in strength of 20 mg.
4 CONTRAINDICATIONS
Rabeprazole is contraindicated in patients with known hypersensitivity to rabeprazole, substituted benzimidazoles or to any component of the formulation.
For information about contraindications of antibacterial agents (clarithromycin and amoxicillin) indicated in combination with rabeprazole sodium delayed-release tablets, refer to the Contraindications section of their package inserts.
5 WARNINGS AND PRECAUTIONS
5.1 Presence of Gastric Malignancy
Symptomatic response to therapy with rabeprazole does not preclude the presence of gastric malignancy.
Patients with healed GERD were treated for up to 40 months with rabeprazole and monitored with serial gastric biopsies. Patients without H. pylori infection (221 of 326 patients) had no clinically important pathologic changes in the gastric mucosa. Patients with H. pylori infection at baseline (105 of 326 patients) had mild or moderate inflammation in the gastric body or mild inflammation in the gastric antrum. Patients with mild grades of infection or inflammation in the gastric body tended to change to moderate, whereas those graded moderate at baseline tended to remain stable. Patients with mild grades of infection or inflammation in the gastric antrum tended to remain stable. At baseline 8% of patients had atrophy of glands in the gastric body and 15% had atrophy in the gastric antrum. At endpoint, 15% of patients had atrophy of glands in the gastric body and 11% had atrophy in the gastric antrum. Approximately 4% of patients had intestinal metaplasia at some point during follow-up, but no consistent changes were seen.
5.2 Concomitant Use With Warfarin
Steady state interactions of rabeprazole and warfarin have not been adequately evaluated in patients. There have been reports of increased INR and prothrombin time in patients receiving a proton pump inhibitor and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with a proton pump inhibitor and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Published observational studies suggest that PPI therapy like rabeprazole may be associated with an increased risk of Clostridium difficile associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2)].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents. For more information specific to antibacterial agents (clarithromycin and amoxicillin) indicated for use in combination with rabeprazole, refer to Warnings and Precautions sections of those package inserts.
5.4 Bone Fracture
Several published observational studies in adults suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2) and Adverse Reactions (6.2)].
5.5 Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), healthcare professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].
Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (7.7)].
6 ADVERSE REACTIONS
Worldwide, over 2900 patients have been treated with rabeprazole in Phase II-III clinical trials involving various dosages and durations of treatment.
Because clinical trials are conducted under varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Clinical Studies Experience
Adults
The data described below reflect exposure to rabeprazole in 1064 adult patients exposed for up to 8 weeks. The studies were primarily placebo- and active-controlled trials in adult patients with Erosive or Ulcerative Gastroesophageal Reflux Disease (GERD), Duodenal Ulcers and Gastric Ulcers. The population had a mean age of 53 years (range 18 to 89 years) and had a ratio of approximately 60% male: 40% female. The racial distribution was 86% Caucasian, 8% African American, 2% Asian and 5% other. Most patients received either 10 mg, 20 mg or 40 mg/day of rabeprazole.
An analysis of adverse reactions appearing in ≥ 2% of rabeprazole patients (n = 1064) and with a greater frequency than placebo (n = 89) in controlled North American and European acute treatment trials, revealed the following adverse reactions: pain (3% vs. 1%), pharyngitis (3% vs. 2%), flatulence (3% vs. 1%), infection (2% vs. 1%), and constipation (2% vs. 1%).
Three long-term maintenance studies consisted of a total of 740 adult patients; at least 54% of adult patients were exposed to rabeprazole for 6 months and at least 33% were exposed for 12 months. Of the 740 adult patients, 247 (33%) and 241 (33%) patients received 10 mg and 20 mg of rabeprazole, respectively, while 169 (23%) patients received placebo and 83 (11%) received omeprazole.
The safety profile of rabeprazole in the maintenance studies in adults was consistent with what was observed in the acute studies.
Other adverse reactions seen in controlled clinical trials, which do not meet the above criteria (≥ 2% of rabeprazole treated patients and greater than placebo) and for which there is a possibility of a causal relationship to rabeprazole, include the following: headache, abdominal pain, diarrhea, dry mouth, dizziness, peripheral edema, hepatic enzyme increase, hepatitis, hepatic encephalopathy, myalgia, and arthralgia.
Combination Treatment with Amoxicillin and Clarithromycin: In clinical trials using combination therapy with rabeprazole plus amoxicillin and clarithromycin (RAC), no adverse reactions unique to this drug combination were observed. In the U.S. multicenter study, the most frequently reported drug related adverse reactions for patients who received RAC therapy for 7 or 10 days were diarrhea (8% and 7%) and taste perversion (6% and 10%), respectively.
No clinically significant laboratory abnormalities particular to the drug combinations were observed.
For more information on adverse reactions or laboratory changes with amoxicillin or clarithromycin, refer to their respective package prescribing information, Adverse Reactions section.
Pediatric
In a multicenter, open-label study of adolescent patients 12 to 16 years of age with a clinical diagnosis of symptomatic GERD or endoscopically proven GERD, the adverse event profile was similar to that of adults. The adverse reactions reported without regard to relationship to rabeprazole that occurred in ≥ 2% of 111 patients were headache (9.9%), diarrhea (4.5%), nausea (4.5%), vomiting (3.6%), and abdominal pain (3.6%). The related reported adverse reactions that occurred in ≥ 2% of patients were headache (5.4%) and nausea (1.8%). There were no adverse reactions reported in this study that were not previously observed in adults.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of rabeprazole. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: sudden death; coma, hyperammonemia; jaundice; rhabdomyolysis; disorientation and delirium; anaphylaxis; angioedema; bullous and other drug eruptions of the skin; severe dermatologic reactions, including toxic epidermal necrolysis (some fatal), Stevens-Johnson syndrome, and erythema multiforme; interstitial pneumonia; interstitial nephritis; TSH elevations; bone fractures; hypomagnesemia and Clostridium difficile associated diarrhea. In addition, agranulocytosis, hemolytic anemia, leukopenia, pancytopenia, and thrombocytopenia have been reported. Increases in prothrombin time/INR in patients treated with concomitant warfarin have been reported.
7 DRUG INTERACTIONS
7.1 Drugs Metabolized by CYP450
Rabeprazole is metabolized by the cytochrome P450 (CYP450) drug metabolizing enzyme system. Studies in healthy subjects have shown that rabeprazole does not have clinically significant interactions with other drugs metabolized by the CYP450 system, such as warfarin and theophylline given as single oral doses, diazepam as a single intravenous dose, and phenytoin given as a single intravenous dose (with supplemental oral dosing). Steady state interactions of rabeprazole and other drugs metabolized by this enzyme system have not been studied in patients.
7.2 Warfarin
There have been reports of increased INR and prothrombin time in patients receiving proton pump inhibitors, including rabeprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death [see Warnings and Precautions (5.2)].
7.3 Cyclosporine
In vitro incubations employing human liver microsomes indicated that rabeprazole inhibited cyclosporine metabolism with an IC50 of 62 micromolar, a concentration that is over 50 times higher than the Cmax in healthy volunteers following 14 days of dosing with 20 mg of rabeprazole. This degree of inhibition is similar to that by omeprazole at equivalent concentrations.
7.4 Compounds Dependent on Gastric pH for Absorption
Rabeprazole produces sustained inhibition of gastric acid secretion. An interaction with compounds which are dependent on gastric pH for absorption may occur due to the magnitude of acid suppression observed with rabeprazole. For example, in normal subjects, coadministration of rabeprazole 20 mg QD resulted in an approximately 30% decrease in the bioavailability of ketoconazole and increases in the AUC and Cmax for digoxin of 19% and 29%, respectively. Therefore, patients may need to be monitored when such drugs are taken concomitantly with rabeprazole. Coadministration of rabeprazole and antacids produced no clinically relevant changes in plasma rabeprazole concentrations.
Concomitant use of atazanavir and proton pump inhibitors is not recommended. Coadministration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and thereby reduce its therapeutic effect.
7.5 Drugs Metabolized by CYP2C19
In a clinical study in Japan evaluating rabeprazole in adult patients categorized by CYP2C19 genotype (n = 6 per genotype category), gastric acid suppression was higher in poor metabolizers as compared to extensive metabolizers. This could be due to higher rabeprazole plasma levels in poor metabolizers. Whether or not interactions of rabeprazole sodium with other drugs metabolized by CYP2C19 would be different between extensive metabolizers and poor metabolizers has not been studied.
7.6 Combined Administration With Clarithromycin
Combined administration consisting of rabeprazole, amoxicillin, and clarithromycin resulted in increases in plasma concentrations of rabeprazole and 14-hydroxyclarithromycin [see Clinical Pharmacology (12.3)].
Concomitant administration of clarithromycin with other drugs can lead to serious adverse reactions due to drug interactions [see Warnings and Precautions in prescribing information for clarithromycin]. Because of these drug interactions, clarithromycin is contraindicated for coadministration with certain drugs [see Contraindications in prescribing information for clarithromycin] [see Drug Interactions in prescribing information for amoxicillin].
7.7 Methotrexate
Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of methotrexate with PPIs have been conducted [see Warnings and Precautions (5.6)].
7.8 Clopidogrel
Concomitant administration of rabeprazole and clopidogrel in healthy subjects had no clinically meaningful effect on exposure to the active metabolite of clopidogrel [see Clinical Pharmacology (12.3)]. No dose adjustment of clopidogrel is necessary when administered with an approved dose of rabeprazole.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy category B
Risk Summary
There are no adequate and well-controlled studies with rabeprazole in pregnant women. No evidence of teratogenicity was seen in animal reproduction studies with rabeprazole at 13 and 8 times the human exposure at the recommended dose for GERD, in rats and rabbits, respectively. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Animal Data
Embryo-fetal developmental studies have been performed in rats at intravenous doses of rabeprazole up to 50 mg/kg/day (plasma AUC of 11.8 mcg•hr/mL, about 13 times the human exposure at the recommended oral dose for GERD) and rabbits at intravenous doses up to 30 mg/kg/day (plasma AUC of 7.3 mcg•hr/mL, about 8 times the human exposure at the recommended oral dose for GERD) and have revealed no evidence of harm to the fetus due to rabeprazole.
Administration of rabeprazole to rats in late gestation and during lactation at an oral dose of 400 mg/kg/day (about 195 times the human oral dose based on mg/m2) resulted in decreases in body weight gain of the pups.
8.3 Nursing Mothers
It is not known if rabeprazole is excreted in human milk; however, rabeprazole is present in rat milk. Because many drugs are excreted in milk, caution should be exercised when rabeprazole is administered to a nursing woman.
8.4 Pediatric Use
Symptomatic GERD in Adolescent Patients Greater or Equal to 12 Years of Age
In a multicenter, randomized, open-label, parallel-group study, 111 adolescent patients 12 to 16 years of age with a clinical diagnosis of symptomatic GERD, or suspected or endoscopically proven GERD were randomized and treated with either rabeprazole 10 mg or rabeprazole 20 mg once daily for up to 8 weeks for the evaluation of safety and efficacy. The adverse event profile in adolescent patients was similar to that of adults. The related reported adverse reactions that occurred in ≥ 2% of patients were headache (5.4%) and nausea (1.8%). There were no adverse reactions reported in these studies that were not previously observed in adults.
8.5 Geriatric Use
Of the total number of subjects in clinical studies of rabeprazole, 19% were 65 years and over, while 4% were 75 years and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Gender
Duodenal ulcer and erosive esophagitis healing rates in women are similar to those in men. Adverse reactions and laboratory test abnormalities in women occurred at rates similar to those in men.
10 OVERDOSAGE
Because strategies for the management of overdose are continually evolving, it is advisable to contact a Poison Control Center to determine the latest recommendations for the management of an overdose of any drug. There has been no experience with large overdoses with rabeprazole. Seven reports of accidental overdosage with rabeprazole have been received. The maximum reported overdose was 80 mg. There were no clinical signs or symptoms associated with any reported overdose. Patients with Zollinger-Ellison syndrome have been treated with up to 120 mg rabeprazole QD. No specific antidote for rabeprazole is known. Rabeprazole is extensively protein bound and is not readily dialyzable. In the event of overdosage, treatment should be symptomatic and supportive.
Single oral doses of rabeprazole at 786 mg/kg and 1024 mg/kg were lethal to mice and rats, respectively. The single oral dose of 2000 mg/kg was not lethal to dogs. The major symptoms of acute toxicity were hypoactivity, labored respiration, lateral or prone position and convulsion in mice and rats and watery diarrhea, tremor, convulsion and coma in dogs.
11 DESCRIPTION
The active ingredient in rabeprazole sodium delayed-release tablets is rabeprazole sodium, which is a proton pump inhibitor. It is a substituted benzimidazole known chemically as 2-[[[4-(3-methoxypropoxy)-3-methyl-2-pyridinyl]-methyl]sulfinyl]-1H–benzimidazole sodium salt. Rabeprazole sodium is a white to slightly yellowish-white solid. It is very soluble in water and methanol, freely soluble in ethanol, chloroform and ethyl acetate and insoluble in ether and n-hexane. The stability of rabeprazole sodium is a function of pH; it is rapidly degraded in acid media, and is more stable under alkaline conditions. The structural formula is:

C18H20N3NaO3S M.W. 381.43
Rabeprazole is available for oral administration as delayed-release, enteric-coated tablets containing 20 mg of rabeprazole sodium.
Inactive ingredients of the 20 mg tablet are D&C Yellow #10 Lake, FD&C Yellow #6 Lake, hydroxypropyl cellulose, hypromellose, hypromellose phthalate, iron oxide black, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium oxide, magnesium stearate, mannitol, microcrystalline cellulose, polyethylene glycol, propylene glycol, shellac glaze, stearic acid, titanium dioxide, and triethyl citrate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Rabeprazole belongs to a class of antisecretory compounds (substituted benzimidazole proton-pump inhibitors) that do not exhibit anticholinergic or histamine H2-receptor antagonist properties, but suppress gastric acid secretion by inhibiting the gastric H+, K+ATPase at the secretory surface of the gastric parietal cell. Because this enzyme is regarded as the acid (proton) pump within the parietal cell, rabeprazole has been characterized as a gastric proton-pump inhibitor. Rabeprazole blocks the final step of gastric acid secretion.
In gastric parietal cells, rabeprazole is protonated, accumulates, and is transformed to an active sulfenamide. When studied in vitro, rabeprazole is chemically activated at pH 1.2 with a half-life of 78 seconds. It inhibits acid transport in porcine gastric vesicles with a half-life of 90 seconds.
12.2 Pharmacodynamics
Antisecretory Activity
The antisecretory effect begins within one hour after oral administration of 20 mg rabeprazole. The median inhibitory effect of rabeprazole on 24 hour gastric acidity is 88% of maximal after the first dose. Rabeprazole 20 mg inhibits basal and peptone meal-stimulated acid secretion versus placebo by 86% and 95%, respectively, and increases the percent of a 24 hour period that the gastric pH > 3 from 10% to 65% (see table below). This relatively prolonged pharmacodynamic action compared to the short pharmacokinetic half-life (1 to 2 hours) reflects the sustained inactivation of the H+, K+ATPase.
| Parameter | Rabeprazole (20 mg QD) | Placebo |
| Basal Acid Output (mmol/hr) | 0.4 |
2.8 |
| Stimulated Acid Output (mmol/hr) | 0.6 |
13.3 |
| % Time Gastric pH > 3 | 65 |
10 |
Compared to placebo, rabeprazole, 10 mg, 20 mg, and 40 mg, administered once daily for 7 days significantly decreased intragastric acidity with all doses for each of four meal-related intervals and the 24 hour time period overall. In this study, there were no statistically significant differences between doses; however, there was a significant dose-related decrease in intragastric acidity. The ability of rabeprazole to cause a dose-related decrease in mean intragastric acidity is illustrated below.
| AUC interval (hrs) | Treatment | |||
|
10 mg RBP (N = 24) |
20 mg RBP (N = 24) |
40 mg RBP (N = 24) |
Placebo (N = 24) |
|
| 08:00 to 13:00 | 19.6 ± 21.5 |
12.9 ± 23 |
7.6 ± 14.7 |
91.1 ± 39.7 |
| 13:00 to 19:00 | 5.6 ± 9.7 |
8.3 ± 29.8 |
1.3 ± 5.2 |
95.5 ± 48.7 |
| 19:00 to 22:00 | 0.1 ± 0.1 |
0.1 ± 0.06 |
0.0 ± 0.02 |
11.9 ± 12.5 |
| 22:00 to 08:00 | 129.2 ± 84 |
109.6 ± 67.2 |
76.9 ± 58.4 |
479.9 ± 165 |
| AUC 0-24 hours | 155.5 ± 90.6 |
130.9 ± 81 |
85.8 ± 64.3 |
678.5 ± 216 |
After administration of 20 mg rabeprazole tablets once daily for eight days, the mean percent of time that gastric pH > 3 or gastric pH > 4 after a single dose (Day 1) and multiple doses (Day 8) was significantly greater than placebo (see table below). The decrease in gastric acidity and the increase in gastric pH observed with 20 mg rabeprazole tablets administered once daily for eight days were compared to the same parameters for placebo, as illustrated below:
| Parameter | Rabeprazole 20 mg QD | Placebo | ||
| Day 1 | Day 8 | Day 1 | Day 8 | |
| Mean AUC0-24 Acidity | 340.8 |
176.9 |
925.5 | 862.4 |
Median trough pH (23 hr) |
3.77 | 3.51 | 1.27 | 1.38 |
% Time Gastric pH > 3 |
54.6 |
68.7 |
19.1 | 21.7 |
% Time Gastric pH > 4 |
44.1 |
60.3 |
7.6 | 11.0 |
Effects on Esophageal Acid Exposure
In patients with gastroesophageal reflux disease (GERD) and moderate to severe esophageal acid exposure, rabeprazole 20 mg and 40 mg tablets per day decreased 24 hour esophageal acid exposure. After seven days of treatment, the percentage of time that esophageal pH < 4 decreased from baselines of 24.7% for 20 mg and 23.7% for 40 mg, to 5.1% and 2.0%, respectively. Normalization of 24 hour intraesophageal acid exposure was correlated to gastric pH > 4 for at least 35% of the 24 hour period; this level was achieved in 90% of subjects receiving rabeprazole 20 mg and in 100% of subjects receiving rabeprazole 40 mg. With rabeprazole 20 mg and 40 mg per day, significant effects on gastric and esophageal pH were noted after one day of treatment, and more pronounced after seven days of treatment.
Effects on Serum Gastrin
In patients given daily doses of rabeprazole for up to eight weeks to treat ulcerative or erosive esophagitis and in patients treated for up to 52 weeks to prevent recurrence of disease the median fasting gastrin level increased in a dose-related manner. The group median values stayed within the normal range.
In a group of subjects treated daily with rabeprazole 20 mg tablets for 4 weeks a doubling of mean serum gastrin concentrations were observed. Approximately 35% of these treated subjects developed serum gastrin concentrations above the upper limit of normal. In a study of CYP2C19 genotyped subjects in Japan, poor metabolizers developed statistically significantly higher serum gastrin concentrations than extensive metabolizers.
Effects on Enterochromaffin-like (ECL) Cells
Increased serum gastrin secondary to antisecretory agents stimulates proliferation of gastric ECL cells which, over time, may result in ECL cell hyperplasia in rats and mice and gastric carcinoids in rats, especially in females [see Nonclinical Toxicology (13.1)].
In over 400 patients treated with rabeprazole tablets (10 or 20 mg/day) for up to one year, the incidence of ECL cell hyperplasia increased with time and dose, which is consistent with the pharmacological action of the proton-pump inhibitor. No patient developed the adenomatoid, dysplastic or neoplastic changes of ECL cells in the gastric mucosa. No patient developed the carcinoid tumors observed in rats.
Endocrine Effects
Studies in humans for up to one year have not revealed clinically significant effects on the endocrine system. In healthy male volunteers treated with rabeprazole for 13 days, no clinically relevant changes have been detected in the following endocrine parameters examined: 17 β-estradiol, thyroid stimulating hormone, tri-iodothyronine, thyroxine, thyroxine-binding protein, parathyroid hormone, insulin, glucagon, renin, aldosterone, follicle-stimulating hormone, luteotrophic hormone, prolactin, somatotrophic hormone, dehydroepiandrosterone, cortisol-binding globulin, and urinary 6β-hydroxycortisol, serum testosterone and circadian cortisol profile.
Other Effects
In humans treated with rabeprazole for up to one year, no systemic effects have been observed on the central nervous, lymphoid, hematopoietic, renal, hepatic, cardiovascular, or respiratory systems. No data are available on long-term treatment with rabeprazole and ocular effects.
Microbiology
The following in vitro data are available but the clinical significance is unknown.
Rabeprazole sodium, amoxicillin and clarithromycin as a three drug regimen has been shown to be active against most strains of Helicobacter pylori in vitro and in clinical infections as described in the Clinical Studies (14) and Indications and Usage (1) sections.
Helicobacter pylori
Susceptibility testing of H. pylori isolates was performed for amoxicillin and clarithromycin using agar dilution methodology1, and minimum inhibitory concentrations (MICs) were determined.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures.
Incidence of Antibiotic-Resistant Organisms Among Clinical Isolates
Pretreatment Resistance: Clarithromycin pretreatment resistance rate (MIC ≥ 1 mcg/mL) to H. pylori was 9% (51/ 560) at baseline in all treatment groups combined. A total of > 99% (558/560) of patients had H. pylori isolates which were considered to be susceptible (MIC ≤ 0.25 mcg/mL) to amoxicillin at baseline. Two patients had baseline H. pylori isolates with an amoxicillin MIC of 0.5 mcg/mL.
For susceptibility testing information about Helicobacter pylori, see Microbiology section in prescribing information for clarithromycin and amoxicillin.
| Days of RAC Therapy | Clarithromycin Pretreatment Results | Total Number | H. pylori Negative (Eradicated) | H. pylori Positive (Persistent) Post-Treatment Susceptibility Results | |||
S |
I |
R |
No MIC | ||||
| 7 | Susceptible |
129 | 103 | 2 | 0 | 1 | 23 |
| 7 | Intermediate |
0 | 0 | 0 | 0 | 0 | 0 |
| 7 | Resistant |
16 | 5 | 2 | 1 | 4 | 4 |
| 10 | Susceptible |
133 | 111 | 3 | 1 | 2 | 16 |
| 10 | Intermediate |
0 | 0 | 0 | 0 | 0 | 0 |
| 10 | Resistant |
9 | 1 | 0 | 0 | 5 | 3 |
Patients with persistent H. pylori infection following rabeprazole, amoxicillin, and clarithromycin therapy will likely have clarithromycin resistant clinical isolates. Therefore, clarithromycin susceptibility testing should be done when possible. If resistance to clarithromycin is demonstrated or susceptibility testing is not possible, alternative antimicrobial therapy should be instituted.
Amoxicillin Susceptibility Test Results and Clinical/Bacteriological Outcomes: In the U.S. multicenter study, a total of > 99% (558/560) of patients had H. pylori isolates which were considered to be susceptible (MIC ≤ 0.25 mcg/mL) to amoxicillin at baseline. The other 2 patients had baseline H. pylori isolates with an amoxicillin MIC of 0.5 mcg/mL, and both isolates were clarithromycin-resistant at baseline; in one case the H. pylori was eradicated. In the 7 and 10 day treatment groups 75% (107/145) and 79% (112/142), respectively, of the patients who had pretreatment amoxicillin susceptible MICs (≤ 0.25 mcg/mL) were eradicated of H. pylori. No patients developed amoxicillin-resistant H. pylori during therapy.
12.3 Pharmacokinetics
Rabeprazole sodium delayed-release tablets are enteric-coated to allow rabeprazole sodium, which is acid labile, to pass through the stomach relatively intact.
After oral administration of 20 mg rabeprazole tablet, peak plasma concentrations (Cmax) of rabeprazole occur over a range of 2.0 to 5.0 hours (Tmax). The rabeprazole Cmax and AUC are linear over an oral dose range of 10 mg to 40 mg. There is no appreciable accumulation when doses of 10 mg to 40 mg are administered every 24 hours; the pharmacokinetics of rabeprazole is not altered by multiple dosing.
Absorption: Absolute bioavailability for a 20 mg oral tablet of rabeprazole (compared to intravenous administration) is approximately 52%. When rabeprazole tablets are administered with a high fat meal, Tmax is variable; which concomitant food intake may delay the absorption up to 4 hours or longer. However, the Cmax and the extent of rabeprazole absorption (AUC) are not significantly altered. Thus rabeprazole tablets may be taken without regard to timing of meals.
Distribution: Rabeprazole is 96.3% bound to human plasma proteins.
Metabolism: Rabeprazole is extensively metabolized. A significant portion of rabeprazole is metabolized via systemic nonenzymatic reduction to a thioether compound. Rabeprazole is also metabolized to sulphone and desmethyl compounds via cytochrome P450 in the liver. The thioether and sulphone are the primary metabolites measured in human plasma. These metabolites were not observed to have significant antisecretory activity. In vitro studies have demonstrated that rabeprazole is metabolized in the liver primarily by cytochromes P450 3A (CYP3A) to a sulphone metabolite and cytochrome P450 2C19 (CYP2C19) to desmethyl rabeprazole. CYP2C19 exhibits a known genetic polymorphism due to its deficiency in some sub-populations (e.g., 3 to 5% of Caucasians and 17 to 20% of Asians). Rabeprazole metabolism is slow in these sub-populations, therefore, they are referred to as poor metabolizers of the drug.
Elimination: Following a single 20 mg oral dose of 14C-labeled rabeprazole, approximately 90% of the drug was eliminated in the urine, primarily as thioether carboxylic acid; its glucuronide, and mercapturic acid metabolites. The remainder of the dose was recovered in the feces. Total recovery of radioactivity was 99.8%. No unchanged rabeprazole was recovered in the urine or feces.
Geriatric: In 20 healthy elderly subjects administered 20 mg rabeprazole tablet once daily for seven days, AUC values approximately doubled and the Cmax increased by 60% compared to values in a parallel younger control group. There was no evidence of drug accumulation after once daily administration [see Use in Specific Populations (8.5)].
Pediatric: The pharmacokinetics of rabeprazole was studied in pediatric patients with GERD aged up to 16 years in four separate clinical studies.
Patients 12 to 16 Years of Age
The pharmacokinetics of rabeprazole was studied in 12 adolescent patients with GERD 12 to 16 years of age, in a multicenter study. Patients received rabeprazole 20 mg tablets once daily for five or seven days. An approximate 40% increase in exposure was noted following 5 to 7 days of dosing compared with the exposure after 1 day dosing. Pharmacokinetic parameters in adolescent patients with GERD 12 to 16 years of age were within the range observed in healthy adult volunteers.
Gender and Race: In analyses adjusted for body mass and height, rabeprazole pharmacokinetics showed no clinically significant differences between male and female subjects. In studies that used different formulations of rabeprazole, AUC0-∞ values for healthy Japanese men were approximately 50 to 60% greater than values derived from pooled data from healthy men in the United States.
Renal Disease: In 10 patients with stable end-stage renal disease requiring maintenance hemodialysis (creatinine clearance ≤ 5 mL/min/1.73 m2), no clinically significant differences were observed in the pharmacokinetics of rabeprazole after a single 20 mg oral dose when compared to 10 healthy volunteers [see Dosage and Administration (2.9)].
Hepatic Disease: In a single dose study of 10 patients with chronic mild to moderate compensated cirrhosis of the liver who were administered a 20 mg dose of rabeprazole, AUC0-24 was approximately doubled, the elimination half-life was 2 to 3 fold higher, and total body clearance was decreased to less than half compared to values in healthy men.
In a multiple dose study of 12 patients with mild to moderate hepatic impairment administered 20 mg rabeprazole once daily for eight days, AUC0-∞ and Cmax values increased approximately 20% compared to values in healthy age- and gender-matched subjects. These increases were not statistically significant.
No information exists on rabeprazole disposition in patients with severe hepatic impairment. Please refer to the Dosage and Administration (2.9) for information on dosage adjustment in patients with hepatic impairment.
Combined Administration with Antimicrobials: Sixteen healthy volunteers genotyped as extensive metabolizers with respect to CYP2C19 were given 20 mg rabeprazole sodium, 1000 mg amoxicillin, 500 mg clarithromycin, or all 3 drugs in a four-way crossover study. Each of the four regimens was administered twice daily for 6 days. The AUC and Cmax for clarithromycin and amoxicillin were not different following combined administration compared to values following single administration. However, the rabeprazole AUC and Cmax increased by 11% and 34%, respectively, following combined administration. The AUC and Cmax for 14-hydroxyclarithromycin (active metabolite of clarithromycin) also increased by 42% and 46%, respectively. This increase in exposure to rabeprazole and 14-hydroxyclarithromycin is not expected to produce safety concerns.
Concomitant Use with Clopidogrel: Clopidogrel is metabolized to its active metabolite in part by CYP2C19. A study of healthy subjects including CYP2C19 extensive and intermediate metabolizers receiving once daily administration of clopidogrel 75 mg concomitantly with placebo or with rabeprazole 20 mg (n = 36), for 7 days was conducted. The mean AUC of the active metabolite of clopidogrel was reduced by approximately 12% (mean AUC ratio was 88%, with 90% CI of 81.7 to 95.5%) when rabeprazole was coadministered compared to administration of clopidogrel with placebo.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 88/104 week carcinogenicity study in CD-1 mice, rabeprazole at oral doses up to 100 mg/kg/day did not produce any increased tumor occurrence. The highest tested dose produced a systemic exposure to rabeprazole (AUC) of 1.40 mcg•hr/mL which is 1.6 times the human exposure (plasma AUC0-∞ = 0.88 mcg•hr/mL) at the recommended dose for GERD (20 mg/day). In a 28 week carcinogenicity study in p53+/- transgenic mice, rabeprazole at oral doses of 20, 60, and 200 mg/kg/day did not cause an increase in the incidence rates of tumors but produced gastric mucosal hyperplasia at all doses. The systemic exposure to rabeprazole at 200 mg/kg/day is about 17 to 24 times the human exposure at the recommended dose for GERD. In a 104 week carcinogenicity study in Sprague-Dawley rats, males were treated with oral doses of 5, 15, 30 and 60 mg/kg/day and females with 5, 15, 30, 60 and 120 mg/kg/day. Rabeprazole produced gastric enterochromaffin-like (ECL) cell hyperplasia in male and female rats and ECL cell carcinoid tumors in female rats at all doses including the lowest tested dose. The lowest dose (5 mg/kg/day) produced a systemic exposure to rabeprazole (AUC) of about 0.1 mcg•hr/mL which is about 0.1 times the human exposure at the recommended dose for GERD. In male rats, no treatment related tumors were observed at doses up to 60 mg/kg/day producing a rabeprazole plasma exposure (AUC) of about 0.2 mcg•hr/mL (0.2 times the human exposure at the recommended dose for GERD).
Rabeprazole was positive in the Ames test, the Chinese hamster ovary cell (CHO/HGPRT) forward gene mutation test and the mouse lymphoma cell (L5178Y/TK+/–) forward gene mutation test. Its demethylated-metabolite was also positive in the Ames test. Rabeprazole was negative in the in vitro Chinese hamster lung cell chromosome aberration test, the in vivo mouse micronucleus test, and the in vivo and ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) tests.
Rabeprazole at intravenous doses up to 30 mg/kg/day (plasma AUC of 8.8 mcg•hr/mL, about 10 times the human exposure at the recommended dose for GERD) was found to have no effect on fertility and reproductive performance of male and female rats.
13.2 Animal Toxicology and/or Pharmacology
Studies in juvenile and young adult rats and dogs were performed. In juvenile animal studies rabeprazole sodium was administered orally to rats for up to 5 weeks and to dogs for up to 13 weeks, each commencing on Day 7 postpartum and followed by a 13 week recovery period. Rats were dosed at 5, 25 or 150 mg/kg/day and dogs were dosed at 3, 10 or 30 mg/kg/day. The data from these studies were comparable to those reported for young adult animals. Pharmacologically mediated changes, including increased serum gastrin levels and stomach changes, were observed at all dose levels in both rats and dogs. These observations were reversible over the 13 week recovery periods. Although body weights and/or crown-rump lengths were minimally decreased during dosing, no effects on the development parameters were noted in either juvenile rats or dogs.
14 CLINICAL STUDIES
14.1 Healing of Erosive or Ulcerative GERD in Adults
In a U.S., multicenter, randomized, double-blind, placebo-controlled study, 103 patients were treated for up to eight weeks with placebo, 10 mg, 20 mg or 40 mg rabeprazole QD. For this and all studies of GERD healing, only patients with GERD symptoms and at least grade 2 esophagitis (modified Hetzel-Dent grading scale) were eligible for entry. Endoscopic healing was defined as grade 0 or 1. Each rabeprazole dose was significantly superior to placebo in producing endoscopic healing after four and eight weeks of treatment. The percentage of patients demonstrating endoscopic healing was as follows:
| Week | 10 mg Rabeprazole QD | 20 mg Rabeprazole QD | 40 mg Rabeprazole QD | Placebo |
| N = 27 | N = 25 | N= 26 | N = 25 | |
| 4 | 63% |
56% |
54% |
0% |
| 8 | 93% |
84% |
85% |
12% |
In addition, there was a statistically significant difference in favor of the rabeprazole 10 mg, 20 mg, and 40 mg doses compared to placebo at Weeks 4 and 8 regarding complete resolution of GERD heartburn frequency (p ≤ 0.026). All rabeprazole groups reported significantly greater rates of complete resolution of GERD daytime heartburn severity compared to placebo at Weeks 4 and 8 (p ≤ 0.036). Mean reductions from baseline in daily antacid dose were statistically significant for all rabeprazole groups when compared to placebo at both Weeks 4 and 8 (p ≤ 0.007).
In a North American multicenter, randomized, double-blind, active-controlled study of 336 patients, rabeprazole was statistically superior to ranitidine with respect to the percentage of patients healed at endoscopy after four and eight weeks of treatment (see table below):
| Week | Rabeprazole 20 mg QD | Ranitidine 150 mg QID |
| N = 167 | N = 169 | |
| 4 | 59% |
36% |
| 8 | 87% |
66% |
Rabeprazole 20 mg once daily was significantly more effective than ranitidine 150 mg QID in the percentage of patients with complete resolution of heartburn at Weeks 4 and 8 (p < 0.001). Rabeprazole 20 mg once daily was also more effective in complete resolution of daytime heartburn (p ≤ 0.025), and nighttime heartburn (p ≤ 0.012) at both Weeks 4 and 8, with significant differences by the end of the first week of the study.
14.2 Long-Term Maintenance of Healing of Erosive or Ulcerative GERD in Adults
The long-term maintenance of healing in patients with erosive or ulcerative GERD previously healed with gastric antisecretory therapy was assessed in two U.S., multicenter, randomized, double-blind, placebo-controlled studies of identical design of 52 weeks duration. The two studies randomized 209 and 285 patients, respectively, to receive either 10 mg or 20 mg of rabeprazole QD or placebo. As demonstrated in the tables below, rabeprazole was significantly superior to placebo in both studies with respect to the maintenance of healing of GERD and the proportions of patients remaining free of heartburn symptoms at 52 weeks:
| Rabeprazole 10 mg | Rabeprazole 20 mg | Placebo | |
| Study 1 | N = 66 | N = 67 | N = 70 |
| Week 4 | 83% |
96% |
44% |
| Week 13 | 79% |
93% |
39% |
| Week 26 | 77% |
93% |
31% |
| Week 39 | 76% |
91% |
30% |
| Week 52 | 73% |
90% |
29% |
| Study 2 | N = 93 | N = 93 | N = 99 |
| Week 4 | 89% |
94% |
40% |
| Week 13 | 86% |
91% |
33% |
| Week 26 | 85% |
89% |
30% |
| Week 39 | 84% |
88% |
29% |
| Week 52 | 77% |
86% |
29% |
| COMBINED STUDIES | N = 159 | N = 160 | N = 169 |
| Week 4 | 87% |
94% |
42% |
| Week 13 | 83% |
92% |
36% |
| Week 26 | 82% |
91% |
31% |
| Week 39 | 81% |
89% |
30% |
| Week 52 | 75% |
87% |
29% |
| Rabeprazole 10 mg | Rabeprazole 20 mg | Placebo | |
| Heartburn Frequency | |||
| Study 1 | 46/55 (84%) |
48/52 (92%) |
17/45 (38%) |
| Study 2 | 50/72 (69%) |
57/72 (79%) |
22/79 (28%) |
| Daytime Heartburn Severity | |||
| Study 1 | 61/64 (95%) |
60/62 (97%) |
42/61 (69%) |
| Study 2 | 73/84 (87%) |
82/87 (94%) |
67/90 (74%) |
| Nighttime Heartburn Severity | |||
| Study 1 | 57/61 (93%) |
60/61 (98%) |
37/56 (66%) |
| Study 2 | 67/80 (84%) | 79/87 (91%) |
64/87 (74%) |
14.3 Treatment of Symptomatic GERD in Adults
Two U.S., multicenter, double-blind, placebo controlled studies were conducted in 316 adult patients with daytime and nighttime heartburn. Patients reported 5 or more periods of moderate to very severe heartburn during the placebo treatment phase the week prior to randomization. Patients were confirmed by endoscopy to have no esophageal erosions.
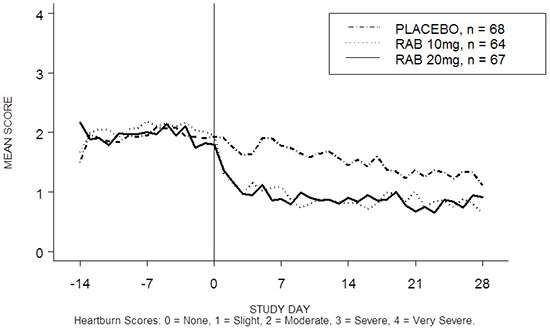
The percentage of heartburn free daytime and/or nighttime periods was greater with rabeprazole 20 mg compared to placebo over the 4 weeks of study in Study RAB-USA-2 (47% vs. 23%) and Study RAB-USA-3 (52% vs. 28%). The mean decreases from baseline in average daytime and nighttime heartburn scores were significantly greater for rabeprazole 20 mg as compared to placebo at week 4. Graphical displays depicting the daily mean daytime and nighttime scores are provided in Figures 2 to 5.
In addition, the combined analysis of these two studies showed rabeprazole 20 mg significantly improved other GERD-associated symptoms (regurgitation, belching and early satiety) by week 4 compared with placebo (all p values < 0.005).
Rabeprazole 20 mg also significantly reduced daily antacid consumption versus placebo over 4 weeks (p < 0.001).
14.4 Healing of Duodenal Ulcers in Adults
In a U.S., randomized, double-blind, multicenter study assessing the effectiveness of 20 mg and 40 mg of rabeprazole QD versus placebo for healing endoscopically defined duodenal ulcers, 100 patients were treated for up to four weeks. Rabeprazole was significantly superior to placebo in producing healing of duodenal ulcers. The percentages of patients with endoscopic healing are presented below:
| Week |
Rabeprazole 20 mg QD N = 34 |
Rabeprazole 40 mg QD N = 33 |
Placebo N = 33 |
| 2 | 44% | 42% | 21% |
| 4 | 79% |
91% |
39% |
At Weeks 2 and 4, significantly more patients in the rabeprazole 20 and 40 mg groups reported complete resolution of ulcer pain frequency (p ≤ 0.018), daytime pain severity (p ≤ 0.023), and nighttime pain severity (p ≤ 0.035) compared with placebo patients. The only exception was the rabeprazole 40 mg group versus placebo at Week 2 for duodenal ulcer pain frequency (p = 0.094). Significant differences in resolution of daytime and nighttime pain were noted in both rabeprazole groups relative to placebo by the end of the first week of the study. Significant reductions in daily antacid use were also noted in both rabeprazole groups compared to placebo at Weeks 2 and 4 (p < 0.001).
An international randomized, double-blind, active-controlled trial was conducted in 205 patients comparing 20 mg rabeprazole QD with 20 mg omeprazole QD. The study was designed to provide at least 80% power to exclude a difference of at least 10% between rabeprazole and omeprazole, assuming four-week healing response rates of 93% for both groups. In patients with endoscopically defined duodenal ulcers treated for up to four weeks, rabeprazole was comparable to omeprazole in producing healing of duodenal ulcers. The percentages of patients with endoscopic healing at two and four weeks are presented below:
| Week |
Rabeprazole 20 mg QD N = 102 |
Omeprazole 20 mg QD N = 103 |
95% Confidence Interval for the Treatment Difference (Rabeprazole - Omeprazole) |
| 2 | 69% | 61% | (–6%, 22%) |
| 4 | 98% | 93% | (–3%, 15%) |
Rabeprazole and omeprazole were comparable in providing complete resolution of symptoms.
14.5 Eradication in Patients With Peptic Ulcer Disease or Symptomatic Non-Ulcer Disease in Adults
The U.S. multicenter study was a double-blind, parallel-group comparison of rabeprazole, amoxicillin, and clarithromycin for 3, 7, or 10 days vs. omeprazole, amoxicillin and clarithromycin for 10 days. Therapy consisted of rabeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily (RAC) or omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily (OAC). Patients with H. pylori infection were stratified in a 1:1 ratio for those with peptic ulcer disease (active or a history of ulcer in the past five years) [PUD] and those who were symptomatic but without peptic ulcer disease [NPUD], as determined by upper gastrointestinal endoscopy. The overall H. pylori eradication rates, defined as negative 13C-UBT for H. pylori ≥ 6 weeks from the end of the treatment are shown in the following table. The eradication rates in the 7 day and 10 day RAC regimens were found to be similar to 10 day OAC regimen using either the Intent-to-Treat (ITT) or Per-Protocol (PP) populations. Eradication rates in the RAC 3 day regimen were inferior to the other regimens.
| Treatment Group Percent (%) of Patients Cured (Number of Patients) | Difference (RAC – OAC) [95% Confidence Interval] | ||
7-day RAC |
10-day OAC | ||
Per Protocol |
84.3% (N = 166) | 81.6% (N = 179) | 2.8 [-5.2, 10.7] |
Intent-to-Treat |
77.3% (N = 194) | 73.3% (N = 206) | 4.0 [-4.4, 12.5] |
10-day RAC |
10-day OAC | ||
Per Protocol |
86.0% (N = 171) | 81.6% (N = 179) | 4.4 [-3.3, 12.1] |
Intent-to-Treat |
78.1% (N = 196) | 73.3% (N = 206) | 4.8 [-3.6, 13.2] |
| 3-day RAC | 10-day OAC | ||
Per Protocol |
29.9% (N = 167) | 81.6% (N = 179) | -51.6 [-60.6, -42.6] |
Intent-to-Treat |
27.3% (N = 187) | 73.3% (N = 206) | -46.0 [-54.8, -37.2] |
14.6 Pathological Hypersecretory Conditions, Including Zollinger-Ellison Syndrome in Adults
Twelve patients with idiopathic gastric hypersecretion or Zollinger-Ellison syndrome have been treated successfully with rabeprazole at doses from 20 to 120 mg for up to 12 months. Rabeprazole produced satisfactory inhibition of gastric acid secretion in all patients and complete resolution of signs and symptoms of acid-peptic disease where present. Rabeprazole also prevented recurrence of gastric hypersecretion and manifestations of acid-peptic disease in all patients. The high doses of rabeprazole used to treat this small cohort of patients with gastric hypersecretion were well tolerated.
14.7 Pediatric GERD
Symptomatic GERD in Adolescents 12 to 16 Years of Age
In a multicenter, randomized, open-label, parallel-group study, 111 adolescent patients 12 to 16 years of age with a clinical diagnosis of symptomatic GERD or suspected or endoscopically proven GERD were randomized and treated with either rabeprazole 10 mg or rabeprazole 20 mg once daily for up to 8 weeks for the evaluation of safety and efficacy.
15 REFERENCES
1. National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically—Fifth Edition. Approved Standard NCCLS Document M7-A5, Vol. 20, No. 2, NCCLS, Wayne, PA, January 2000.
16 HOW SUPPLIED/STORAGE AND HANDLING
Rabeprazole sodium delayed-release tablets, 20 mg are supplied as enteric-coated, delayed-release, yellow, round tablets, imprinted on one side of the tablet with black ink "93" "64". They are available in bottles of 30 and 90.
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Protect from moisture.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide).
How to Take Rabeprazole Sodium Delayed-Release Tablets
Patients should be cautioned that rabeprazole sodium delayed-release tablets should be swallowed whole. The tablets should not be chewed, crushed, or split. Rabeprazole sodium delayed-release tablets can be taken with or without food.
Advise patient to immediately report and seek care for diarrhea that does not improve. This may be a sign of Clostridium difficile associated diarrhea [see Warnings and Precautions (5.3)].
Manufactured In Israel By:
TEVA PHARMACEUTICAL IND. LTD.
Jerusalem, 91010, Israel
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. D 10/2013
MEDICATION GUIDE
Rabeprazole Sodium Delayed-Release Tablets
Read the Medication Guide that comes with rabeprazole sodium delayed-release tablets before you start taking them and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or treatment.
What is the most important information I should know about rabeprazole sodium delayed-release tablets?
Rabeprazole sodium delayed-release tablets may help your acid-related symptoms, but you could still have serious stomach problems. Talk with your doctor.
Rabeprazole sodium delayed-release tablets can cause serious side effects, including:
-
Diarrhea. Rabeprazole sodium delayed-release tablets may increase your risk of getting severe diarrhea. This diarrhea may be caused by an infection (Clostridium difficile) in your intestines.
Call your doctor right away if you have watery stool, stomach pain, and fever that does not go away.
- Bone fractures. People who take multiple daily doses of Proton Pump Inhibitor (PPI) medicines for a long period of time (1 year or longer) may have an increased risk of fractures of the hip, wrist, or spine. You should take rabeprazole sodium delayed-release tablets exactly as prescribed, at the lowest dose possible for your treatment and for the shortest time needed. Talk to your doctor about your risk of bone fracture if you take rabeprazole sodium delayed-release tablets.
Rabeprazole sodium delayed-release tablets can have other serious side effects. See “What are the possible side effects of rabeprazole sodium delayed-release tablets?”
What are rabeprazole sodium delayed-release tablets?
Rabeprazole sodium delayed-release tablets are a prescription medicine called a Proton Pump Inhibitor (PPI). Rabeprazole sodium delayed-release tablets reduce the amount of acid in your stomach.
Rabeprazole sodium delayed-release tablets are used in adults:
- for up to 8 weeks to heal acid-related damage to the lining of the esophagus (called erosive esophagitis or EE) and to relieve symptoms, such as heartburn pain. If needed, your doctor may decide to prescribe another 8 weeks of rabeprazole sodium delayed-release tablets.
- to maintain the healing of the esophagus and relief of symptoms related to EE. It is not known if rabeprazole sodium delayed-release tablets are safe and effective if used longer than 12 months (1 year).
- for 4 weeks to treat daytime and nighttime heartburn and other symptoms that happen with Gastroesophageal Reflux Disease (GERD).
GERD happens when acid in your stomach backs up into the tube (esophagus) that connects your mouth to your stomach. This may cause a burning feeling in your chest or throat, sour taste, or burping.
- for up to 4 weeks for the healing and relief of duodenal ulcers. The duodenal area is the area where food passes when it leaves the stomach.
- for 7 days with certain antibiotic medicines to treat an infection caused by bacteria called H. pylori. Sometimes H. pylori bacteria can cause duodenal ulcers. The infection needs to be treated to prevent the ulcers from coming back.
- for the long-term treatment of conditions where your stomach makes too much acid. This includes a rare condition called Zollinger-Ellison syndrome.
Rabeprazole sodium delayed-release tablets are used in adolescents 12 years of age and older to treat symptoms of Gastroesophageal Reflux Disease (GERD) for up to 8 weeks.
Who should not take rabeprazole sodium delayed-release tablets?
Do not take rabeprazole sodium delayed-release tablets if you:
- are allergic to rabeprazole or any of the other ingredients in rabeprazole sodium delayed-release tablets. See the end of this Medication Guide for a complete list of ingredients in rabeprazole sodium delayed-release tablets.
- are allergic to any other Proton Pump Inhibitor (PPI) medicine.
What should I tell my doctor before taking rabeprazole sodium delayed-release tablets?
Before you take rabeprazole sodium delayed-release tablets tell your doctor if you:
- have been told that you have low magnesium levels in your blood
- have liver problems
- have any allergies
- have any other medical conditions
- are pregnant or planning to become pregnant. It is not known if rabeprazole sodium delayed-release tablets can harm your unborn baby.
- are breastfeeding. It is not known if rabeprazole passes into your breast milk. Talk to your doctor about the best way to feed your baby if you take rabeprazole sodium delayed-release tablets.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Rabeprazole sodium delayed-release tablets may affect how other medicines work, and other medicines may affect how rabeprazole sodium delayed-release tablets work.
Especially tell your doctor if you take:
- atazanavir (Reyataz®)
- cyclosporine (Sandimmune®, Neoral®)
- digoxin (Lanoxin®)
- ketoconazole (Nizoral®)
- warfarin (Coumadin®)
- theophylline (THEO-24® Thelair)
- diazepam (Valium®)
- phenytoin (Dilantin®)
- an antibiotic that contains amoxicillin or clarithromycin
- a "water pill" (diuretic)
- methotrexate
Ask your doctor or pharmacist for a list of these medicines, if you are not sure.
Know the medicines that you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take rabeprazole sodium delayed-release tablets?
- Take rabeprazole sodium delayed-release tablets exactly as prescribed. Your doctor will prescribe the dose that is right for you and your medical condition. Do not change your dose or stop taking rabeprazole sodium delayed-release tablets unless you talk to your doctor. Take rabeprazole sodium delayed-release tablets for as long as it is prescribed even if you feel better.
- Rabeprazole sodium delayed-release tablets are usually taken one time each day. Your doctor will tell you the time of day to take rabeprazole sodium delayed-release tablets, based on your medical condition.
- Rabeprazole sodium delayed-release tablets can be taken with or without food. Your doctor will tell you whether to take this medicine with or without food based on your medical condition.
- Swallow each rabeprazole sodium delayed-release tablet whole with water. Do not chew, crush, or split rabeprazole sodium delayed-release tablets. Tell your doctor if you cannot swallow tablets whole.
- If you miss a dose of rabeprazole sodium delayed-release tablets, take it as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your normal schedule. Do not take 2 doses at the same time.
- If you take too many rabeprazole sodium delayed-release tablets, call your doctor or Poison Control Center right away, or go to the nearest hospital emergency room.
- Your doctor may prescribe antibiotic medicines with rabeprazole sodium delayed-release tablets to help treat a stomach infection and heal stomach (duodenal) ulcers that are caused by bacteria called H. pylori. Make sure you read the patient information that comes with an antibiotic before you start taking it.
What are the possible side effects of rabeprazole sodium delayed-release tablets?
Rabeprazole sodium delayed-release tablets can cause serious side effects, including:
- See “What is the most important information I should know about rabeprazole sodium delayed-release tablets?”
-
Low magnesium levels in your body. This problem can be serious. Low magnesium can happen in some people who take a Proton Pump Inhibitor (PPI) medicine for at least 3 months. If low magnesium levels happen, it is usually after a year of treatment. You may or may not have symptoms of low magnesium.
Tell your doctor right away if you have any of these symptoms:
- seizures
- dizziness
- abnormal or fast heart beat
- jitteriness
- jerking movements or shaking (tremors)
- muscle weakness
- spasms of the hands and feet
- cramps or muscle aches
- spasm of the voice box
Your doctor may check the level of magnesium in your body before you start taking rabeprazole sodium delayed-release tablets, during treatment, or if you will be taking rabeprazole sodium delayed-release tablets for a long period of time.
The most common side effects with rabeprazole sodium delayed-release tablets include:
- headache
- pain
- sore throat
- gas
- infection
- constipation
Other side effects:
Serious allergic reactions. Tell your doctor if you get any of the following symptoms with rabeprazole sodium delayed-release tablets.
- rash
- face swelling
- throat tightness
- difficulty breathing
Your doctor may stop rabeprazole sodium delayed-release tablets if these symptoms happen.
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the side effects of rabeprazole sodium delayed-release tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store rabeprazole sodium delayed-release tablets?
- Store rabeprazole sodium delayed-release tablets in a dry place at room temperature between 20° to 25°C (68° to 77°F).
Keep rabeprazole sodium delayed-release tablets and all medicines out of the reach of children.
General Information about rabeprazole sodium delayed-release tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use rabeprazole sodium delayed-release tablets for a condition for which they were not prescribed. Do not give rabeprazole sodium delayed-release tablets to other people, even if they have the same symptoms that you have. They may harm them.
This Medication Guide summarizes the most important information about rabeprazole sodium delayed-release tablets. If you would like more information, talk to your doctor. You can also ask your doctor or pharmacist for information about rabeprazole sodium delayed-release tablets that is written for healthcare professionals. For more information, call 1-888-838-2872.
What are the ingredients in rabeprazole sodium delayed-release tablets?
Active ingredient: rabeprazole sodium
Inactive ingredients: D&C Yellow #10 Lake, FD&C Yellow #6 Lake, hydroxypropyl cellulose, hypromellose, hypromellose phthalate, iron oxide black, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium oxide, magnesium stearate, mannitol, microcrystalline cellulose, polyethylene glycol, propylene glycol, shellac glaze, stearic acid, titanium dioxide, and triethyl citrate.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
All brand names listed are the registered trademarks of their respective owners and are not trademarks of Teva Pharmaceuticals USA.
Manufactured In Israel By:
TEVA PHARMACEUTICAL IND. LTD.
Jerusalem, 91010, Israel
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. B 10/2013
PRINCIPAL DISPLAY PANEL
Rabeprazole Sodium Delayed-Release Tablets, 20 mg 30s Label Text
NDC 0093-0064-56
RABEPRAZOLE SODIUM
Delayed-Release Tablets
20 mg
PHARMACIST: Dispense the accompanying
Medication Guide to each patient.
Rx only
30 TABLETS
TEVA
Rabeprazole SodiumRabeprazole Sodium TABLET, DELAYED RELEASE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||