Protriptyline Hydrochloride
Roxane Laboratories, Inc
Roxane Laboratories, Inc
Protriptyline Hydrochloride Tablets, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- Rx only
- PROTRIPTYLINE HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- PROTRIPTYLINE HYDROCHLORIDE INDICATIONS AND USAGE
- PROTRIPTYLINE HYDROCHLORIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- PROTRIPTYLINE HYDROCHLORIDE ADVERSE REACTIONS
- OVERDOSAGE
- PROTRIPTYLINE HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- METABOLISM
- REFERENCES
- MEDICATION GUIDE
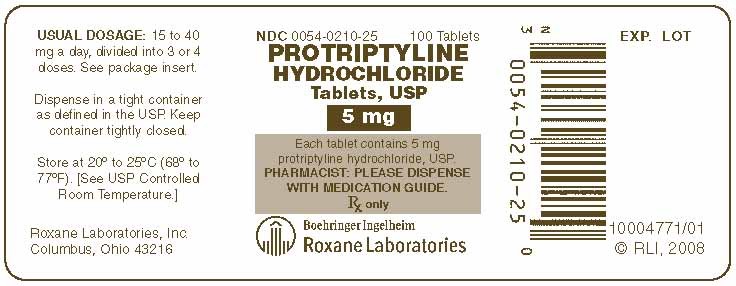
- 0054-0211-25 - 100 Tablets
- 0054-0210-25 - 100 Tablets
FULL PRESCRIBING INFORMATION
Rx only
| Suicidality and Antidepressant Drugs | |
|
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of protriptyline hydrochloride or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Protriptyline hydrochloride is not approved for use in pediatric patients. (See WARNINGS and PRECAUTIONS: Pediatric Use.) |
PROTRIPTYLINE HYDROCHLORIDE DESCRIPTION
Protriptyline HCl is N-methyl-5H dibenzo[a,d]-cycloheptene-5-propanamine hydrochloride. Its molecular formula is C19H21N•HCl and its structural formula is:

Protriptyline HCl, a dibenzocycloheptene derivative, has a molecular weight of 299.84. It is a white to yellowish powder that is freely soluble in water and soluble in dilute HCl. Protriptyline HCl is supplied as 5 mg or 10 mg tablets. Inactive ingredients are anhydrous lactose, colloidal silicon dioxide, magnesium stearate, and microcrystalline cellulose.
CLINICAL PHARMACOLOGY
Protriptyline hydrochloride is an antidepressant agent. The mechanism of its antidepressant action in man is not known. It is not a monoamine oxidase inhibitor, and it does not act primarily by stimulation of the central nervous system
Protriptyline has been found is some studies to have a more rapid onset of action than imipramine or amitriptyline. The initial clinical effect may occur within one week. Sedative and tranquilizing properties are lacking. The rate of excretion is slow.
PROTRIPTYLINE HYDROCHLORIDE INDICATIONS AND USAGE
Protriptyline Hydrochloride Tablets, USP are indicated for the treatment of symptoms of mental depression in patients who are under close medical supervision. Its activating properties make it particularly suitable for withdrawn and anergic patients.
PROTRIPTYLINE HYDROCHLORIDE CONTRAINDICATIONS
Protriptyline Hydrochloride Tablets, USP are contraindicated in patients who have shown prior hypersensitivity to it.
It should not be given concomitantly with a monoamine oxidase inhibiting compound. Hyperpyretic crises, severe convulsions, and deaths have occurred in patients receiving tricyclic antidepressant and monoamine oxidase inhibiting drugs simultaneously. When it is desired to substitute protriptyline for monoamine oxidase inhibitor, a minimum of 14 days should be allowed to elapse after the latter is discontinued. Protriptyline should then be initiated cautiously with gradual increase in dosage until optimum response is achieved.
Protriptyline Hydrochloride Tablets, USP are contraindicated in patients taking cisapride because of the possibility of adverse cardiac interactions including prolongation of the QT interval, cardiac arrhythmias and conduction system disturbances.
This drug should not be used during the acute recovery phase following myocardial infarction.
WARNINGS
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18 to 24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25 to 64 | 1 fewer case |
| >65 | 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms (see ADVERSE REACTIONS Withdrawal Symptoms for a description of the risks of discontinuation of protriptyline).
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for protriptyline should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that protriptyline hydrochloride is not approved for use in treating bipolar depression.
Protriptyline may block the antihypertensive effect of guanethidine or similarly acting compounds.
Protriptyline should be used with caution in patients with a history of seizures, and, because of its autonomic activity, in patients with a tendency to urinary retention, or increased intraocular tension.
Tachycardia and postural hypotension may occur more frequently with protriptyline than with other antidepressant drugs. Protriptyline should be used with caution in elderly patients and patients with cardiovascular disorders; such patients should be observed closely because of the tendency of the drug to produce tachycardia, hypotension, arrhythmias, and prolongation of the conduction time. Myocardial infarction and stroke have occurred with drugs of this class.
On rare occasions, hyperthyroid patients or those receiving thyroid medication may develop arrhythmias when this drug is given.
In patients who may use alcohol excessively, it should be borne in mind that the potentiation may increase the danger inherent in any suicide attempt or overdosage.
Usage in Pregnancy
Safe use in pregnancy and lactation has not been established; therefore, use in pregnant women, nursing mothers or women who may become pregnant requires that possible benefits be weighed against possible hazards to mother and child.
In mice, rats, and rabbits, doses about ten times greater than the recommended human doses had no apparent adverse effects on reproduction.
PRECAUTIONS
General
When protriptyline is used to treat the depressive component of schizophrenia, psychotic symptoms may be aggravated. Likewise, in manic-depressive psychosis, depressed patients may experience a shift toward the manic phase if they are treated with an antidepressant drug. Paranoid delusions, with or without associated hostility, may be exaggerated. In any of these circumstances, it may be advisable to reduce the dose of protriptyline or to use a major tranquilizing drug concurrently.
Symptoms, such as anxiety or agitation, maybe aggravated in overactive or agitated patients.
The possibility of suicide in depressed patients remains during treatment and until significant remission occurs. This type of patient should not have access to large quantities of the drug.
Concurrent administration of protriptyline and electroshock therapy may increase the hazards of therapy. Such treatment should be limited to patients for whom it is essential.
Discontinue the drug several days before elective surgery, if possible.
Both elevation and lowering of blood sugar levels have been reported.
Information for Patients
Prescribers or other health professionals should inform patients, their families and their caregivers about the benefits and risks associated with treatment with protriptyline hydrochloride and should counsel them in its appropriate use. A patient Medication Guide About "Antidepressant Medicines, Depression and Other Serious Mental Illness, and Suicidal Thoughts or Actions" is available for protriptyline hydrochloride. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking protriptyline hydrochloride.
Clinical Worsening and Suicide Risk
Patients, their families and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Drug Interactions
When protriptyline is given with anticholinergic agents or sympathomimetic drugs, including epinephrine combined with local anesthetics, close supervision and careful adjustment of dosages are required.
Hyperpyrexia has been reported when tricyclic antidepressants are administered with anticholinergic agents or with neuroleptic drugs, particularly during hot weather.
Cimetidine is reported to reduce hepatic metabolism of certain tricyclic antidepressants, thereby delaying elimination and increasing steady-state concentrations of these drugs. Clinically significant effects have been reported with the tricyclic antidepressants when used concomitantly with cimetidine. Increases in plasma levels of tricyclic antidepressants, and in the frequency and severity of side effects, particularly anticholinergic, have been reported when cimetidine was added to the drug regimen. Discontinuation of cimetidine in well-controlled patients receiving tricyclic antidepressants and cimetidine may decrease the plasma levels and efficacy of the antidepressants.
Tricyclic antidepressants may enhance the seizure risk in patients taking ULTRAM (tramadol hydrochloride).
Protriptyline may enhance the response to alcohol and the effects of barbiturates and other CNS depressants.
Drugs Metabolized by Cytochrome P450 2D6
The biochemical activity of the drug metabolizing isozyme cytochrome P450 2D6 (debrisoquine hydroxylase) is reduced in a subset of the Caucasian population (about 7% to 10% of Caucasians are so called "poor metabolizers"); reliable estimates of the prevalence of reduced P450 2D6 isozyme activity among Asian, African, and other populations are not yet available. Poor metabolizers have higher than expected plasma concentrations of tricyclic antidepressants (TCAs) when given usual doses. Depending on the fraction of drug metabolized be P450 2D6, the increase in plasma concentration may be small or quite large (8 fold increase in plasma AUC of the TCA).
In addition, certain drugs inhibit the activity of this isozyme and make normal metabolizers resemble poor metabolizers. An individual who is stable on a given dose of TCA may become abruptly toxic when given one of these inhibiting drugs as concomitant therapy. The drugs that inhibit cytochrome P450 2D6 include some that are not metabolized by the enzyme (quinidine; cimetidine) and many that are substrates for P450 2D6 (many other antidepressants, phenothiazines, and the Type 1C antiarrhythmics, propafenone and flecainide). While all the selective seratonin reuptake inhibitors (SSRIs), e.g., fluoxetine, sertraline, and paroxetine, inhibit P450 2D6, they may vary in the extent of inhibition. The extent to which SSRI-TCA interactions may pose clinical problems will depend on the degree of inhibition and the pharmacokinetics of the SSRI involved. Nevertheless, caution is indicated in the coadministration of TCAs with any of the SSRIs and also in switching from one class to the other. Of particular importance, sufficient time must elapse before initiating TCA treatment in a patient being withdrawn from fluoxetine, given the long half-life of the parent and active metabolite (at least 5 weeks may be necessary).
Concomitant use of tricyclic antidepressants with drugs that can inhibit cytochrome P450 2D6 may require lower doses than usually prescribed for either the tricyclic antidepressant or the other drug. Furthermore, whenever one of these other drugs is withdrawn from co-therapy, an increased dose of tricyclic antidepressant may be required. It is desirable to monitor TCA plasma levels whenever a TCA is going to be coadministered with another drug known to be an inhibitor of P450 2D6.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (see BOX WARNING and WARNINGS: Clinical Worsening and Suicide Risk). Anyone considering the use of protriptyline hydrochloride in a child or adolescent must balance the potential risks with the clinical need.
Geriatric Use
Clinical studies of protriptyline did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. (See DOSAGE AND ADMINISTRATION and ADVERSE REACTIONS.)
PROTRIPTYLINE HYDROCHLORIDE ADVERSE REACTIONS
Within each category the following adverse reactions are listed in order of decreasing severity. Included in the listing are a few adverse reactions which have not been reported with this specific drug. However, the pharmacological similarities among the tricyclic antidepressant drugs require that each of the reactions be considered when protriptyline is administered. Protriptyline is more likely to aggravate agitation and anxiety and produce cardiovascular reactions such as tachycardia and hypotension.
Cardiovascular: Myocardial infarction; stroke; heart block; arrhythmias; hypotension, particularly orthostatic hypotension; hypertension; tachycardia; palpitation.
Psychiatric: Confusional states (especially in the elderly) with hallucinations, disorientation, delusions, anxiety, restlessness, agitation; hypomania; exacerbation of psychosis; insomnia, panic, and nightmares.
Neurological: Seizures; incoordination; ataxia; tremors; peripheral neuropathy; numbness, tingling, and paresthesias of extremities; extrapyramidal symptoms; drowsiness; dizziness; weakness and fatigue; headache; syndrome of inappropriate ADH (antidiuretic hormone) secretion; tinnitus; alteration in EEG patterns.
Anticholinergic: Paralytic ileus; hyperpyrexia; urinary retention, delayed micturition, dilatation of the urinary tract; constipation; blurred vision, disturbance of accommodation, increased intraocular pressure, mydriasis; dry mouth and rarely associated sublingual adentitis.
Allergic: Drug fever; petechiae, skin rash, urticaria, itching, photosensitization (avoid excessive exposure to sunlight); edema (general, or of face and tongue).
Hematologic: Agranulocytosis; bone marrow depression; leukopenia; thrombocytopenia; purpura; eosinophilia.
Gastrointestinal: Nausea and vomiting; anorexia; epigastric distress; diarrhea; peculiar taste; stomatitis; abdominal cramps; black tongue.
Endocrine: Impotence, increased or decreased libido: gynecomastia in the male; breast enlargement and galactorrhea in the female; testicular swelling; elevation or depression of blood sugar levels.
Other: Jaundice (simulating obstructive); altered liver function; parotid swelling; alopecia; flushing; weight gain or loss; urinary frequency, nocturia; perspiration.
Withdrawal Symptoms
Though not indicative of addiction, abrupt cessation of treatment after prolonged therapy may produce nausea, headache, and malaise.
OVERDOSAGE
Deaths may occur from overdosage with this class of drugs. Multiple drug ingestion (including alcohol) is common in deliberate tricyclic antidepressant overdose. As management of overdose is complex and changing, it is recommended that the physician contact a poison control center for current information on treatment. Signs and symptoms of toxicity develop rapidly after tricyclic antidepressant overdose, therefore, hospital monitoring is required as soon as possible.
Manifestations
Critical manifestations of overdosage include: cardiac dysrhythmias, severe hypotension, convulsions, and CNS depression, including coma. Changes in the electrocardiogram, particularly in QRS axis or width, are clinically significant indicators of tricyclic antidepressant toxicity.
Other signs of overdose may include: confusion, disturbed concentration, transient visual hallucinations, dilated pupils, agitation, hyperactive reflexes, stupor, drowsiness, muscle rigidity, vomiting, hypothermia, hyperpyrexia, or any of the symptoms listed under ADVERSE REACTIONS.
Management
General
Obtain an ECG and immediately initiate cardiac monitoring. Protect the patient's airway, establish an intravenous line and initiate gastric decontamination. A minimum of six hours of observation with cardiac monitoring and observation for signs of CNS or respiratory depression, hypotension, cardiac dysrhythmias and/or conduction blocks, and seizures is necessary. If signs of toxicity occur at any time during this period, extended monitoring is required. There are case reports of patients succumbing to fatal dysrhythmias late after overdose. These patients had clinical evidence of significant poisoning prior to death and most received inadequate gastrointestinal decontamination. Monitoring of plasma drug levels should not guide management of the patient.
Gastrointestinal Decontamination
All patients suspected of a trycyclic antidepressant overdose should receive gastrointestinal decontamination. This should include large volume gastric lavage followed by activated charcoal. If consciousness is impaired, the airway should be secured prior to lavage. Emesis is contraindicated.
Cardiovascular
A maximal limb-lead QRS duration of ≥0.1 seconds may be the best indication of the severity of the overdose. Intravenous sodium bicarbonate should be used to maintain the serum pH in the range of 7.45 to 7.55. If the pH response is inadequate, hyperventilation may also be used. Concomitant use of hyperventilation and sodium bicarbonate should be done with extreme caution, with frequent pH monitoring. A pH >7.6 or a pCO2 <20 mmHg is undesirable. Dysrhythmias unresponsive to sodium bicarbonate therapy/hyperventilation may respond to lidocaine, bretylium or phenytoin. Type 1A and 1C antiarrhythmics are generally contraindicated (e.g., quinidine, disopyramide and procainamide).
In rare instances, hemoperfusion may be beneficial in acute refractory cardiovascular instability in patients with acute toxicity. However, hemodialysis, peritoneal dialysis, exchange transfusions, and forced diuresis generally have been reported as ineffective in tricyclic antidepressant poisoning.
CNS
In patients with CNS depression, early intubation is advised because of the potential for abrupt deterioration. Seizures should be controlled with benzodiazepines or, if these are ineffective, other anticonvulsants (e.g., phenobarbital, phenytoin). Physostigmine is not recommended except to treat life-threatening symptoms that have been unresponsive to other therapies, and then only in close consultation with a poison control center.
Psychiatric Follow-up
Since overdosage is often deliberate, patients may attempt suicide by other means during the recovery phase. Psychiatric referral may be appropriate.
Pediatric Management
The principles of management of child and adult overdosages are similar. It is strongly recommended that the physician contact the local poison control center for specific pediatric treatment.
PROTRIPTYLINE HYDROCHLORIDE DOSAGE AND ADMINISTRATION
Dosage should be initiated at a low level and increased gradually, noting carefully the clinical response and any evidence of intolerance.
Usual Adult Dosage
Fifteen to 40 mg a day divided into 3 or 4 doses. If necessary, dosage may be increased to 60 mg a day. Dosages above this amount are not recommended. Increases should be made in the morning dose.
Adolescent and Elderly Patients
In general, lower dosages are recommended for these patients. Five mg 3 times a day may be given initially, and increased gradually if necessary. In elderly patients, the cardiovascular system must be monitored closely if the daily dose exceeds 20 mg.
When satisfactory improvement has been reached, dosage should be reduced to the smallest amount that will maintain relief of symptoms.
Minor adverse reactions require reduction in dosage. Major adverse reactions or evidence of hypersensitivity require prompt discontinuation of the drug.
The safety and effectiveness of protriptyline in pediatric patients have not been established.
HOW SUPPLIED
Protriptyline Hydrochloride Tablets, USP are supplied as white, round, biconvex tablets. The 5 mg tablet is debossed with "54 306" on one side and plain on the other. The 10 mg tablet is debossed with "54 694" on one side and plain on the other.
| 0054-0210-25 | 5 mg, white tablet, bottle of 100 |
| 0054-0211-25 | 10 mg, white tablet, bottle of 100 |
Storage
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.] Dispense in a tight container as defined in the USP.
METABOLISM
Metabolic studies indicate that protriptyline is well absorbed from the gastrointestinal tract and is rapidly sequestered in tissues. Relatively low plasma levels are found after administration, and only a small amount of unchanged drug is excreted in the urine of dogs and rabbits. Preliminary studies indicate that demethylation of the secondary amine moiety occurs to a significant extent, and that metabolic transformation probably takes place in the liver. It penetrates the brain rapidly in mice and rats, and moreover that which is present in the brain is almost all unchanged drug.
Studies on the disposition of radioactive protriptyline in human test subjects showed significant plasma levels within 2 hours, peaking at 8 to 12 hours, then declining gradually.
Urinary excretion studies in the same subjects showed significant amounts of radioactivity in 2 hours. The rate of excretion was slow. Cumulative urinary excretion during 16 days accounted for approximately 50% of the drug. The fecal route of excretion did not seem to be important.
REFERENCES
ULTRAM is a registered trademark of Ortho-McNeil Pharmaceutical Inc.
10004773/03 Revised March 2010
© RLI, 2010
MEDICATION GUIDE
Antidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or Actions
Read the Medication Guide that comes with you or your family member’s antidepressant medicine. This Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines. Talk to your, or your family member’s, healthcare provider about:
• all risks and benefits of treatment with antidepressant medicines
• all treatment choices for depression or other serious mental illness
What is the most important information I should know about antidepressant medicines, depression, and other serious mental illnesses, and suicidal thoughts or actions?
1. Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults when the medicine is first started within the first few months of treatment.
2. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic-depressive illness) or suicidal thoughts or actions.
3. How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
• Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is first started or when the dose is changed.
• Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
• Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
• thoughts about suicide or dying
• attempts to commit suicide
• new or worse depression
• new or worse anxiety
• feeling very agitated or restless
• panic attacks
• trouble sleeping (insomnia)
• new or worse irritability
• acting aggressive, being angry, or violent
• acting on dangerous impulses
• an extreme increase in activity and talking (mania)
• other unusual changes in behavior or mood
What else do I need to know about antidepressant medicines?
• Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
• Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
• Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
• Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
• Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child’s healthcare provider for more information.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
This Medication Guide has been approved by the U.S. Food and Drug Administration for all antidepressants.
10004773/03 Revised March 2010
© RLI, 2010
Protriptyline HCl Tablets, USP
0054-0211-25 - 100 Tablets
Rx Only
Roxane Laboratories, Inc.

0054-0210-25 - 100 Tablets
Rx Only
Roxane Laboratories, Inc.
Protriptyline HydrochlorideProtriptyline Hydrochloride TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Protriptyline HydrochlorideProtriptyline Hydrochloride TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||