Plavix
Plavix
FULL PRESCRIBING INFORMATION: CONTENTS*
- PLAVIX DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL STUDIES
- PLAVIX INDICATIONS AND USAGE
- PLAVIX CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- PLAVIX ADVERSE REACTIONS
- OVERDOSAGE
- PLAVIX DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PACKAGE LABEL - PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
PLAVIX DESCRIPTION
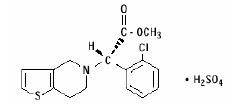
PLAVIX (clopidogrel bisulfate) is an inhibitor of ADP-induced platelet aggregation acting by direct inhibition of adenosine diphosphate (ADP) binding to its receptor and of the subsequent ADP-mediated activation of the glycoprotein GPIIb/IIIa complex. Chemically it is methyl (+)-(S)-α-(2-chlorophenyl)-6,7-dihydrothieno[3,2-c]pyridine-5(4H)-acetate sulfate (1:1). The empirical formula of clopidogrel bisulfate is C16H16ClNO2S•H2SO4 and its molecular weight is 419.9.
The structural formula is as follows:
Clopidogrel bisulfate is a white to off-white powder. It is practically insoluble in water at neutral pH but freely soluble at pH 1. It also dissolves freely in methanol, dissolves sparingly in methylene chloride, and is practically insoluble in ethyl ether. It has a specific optical rotation of about +56°.
PLAVIX for oral administration is provided as either pink, round, biconvex, debossed, film-coated tablets containing 97.875 mg of clopidogrel bisulfate which is the molar equivalent of 75 mg of clopidogrel base or pink, oblong, debossed film-coated tablets containing 391.5 mg of clopidogrel bisulfate which is the molar equivalent of 300 mg of clopidogrel base.
Each tablet contains hydrogenated castor oil, hydroxypropylcellulose, mannitol, microcrystalline cellulose and polyethylene glycol 6000 as inactive ingredients. The pink film coating contains ferric oxide, hypromellose 2910, lactose monohydrate, titanium dioxide and triacetin. The tablets are polished with Carnauba wax.
CLINICAL PHARMACOLOGY
Mechanism of Action and Pharmacodynamic Properties
Clopidogrel is a prodrug, one of whose metabolites is an inhibitor of platelet aggregation. A variety of drugs that inhibit platelet function have been shown to decrease morbid events in people with established cardiovascular atherosclerotic disease as evidenced by stroke or transient ischemic attacks, myocardial infarction, unstable angina or the need for vascular bypass or angioplasty. This indicates that platelets participate in the initiation and/or evolution of these events and that inhibiting platelet function can reduce the event rate.
Clopidogrel must be metabolized by CYP450 enzymes to produce the active metabolite that inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible. Consequently, platelets exposed to clopidogrel's active metabolite are affected for the remainder of their lifespan (about 7 to 10 days). Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP.
Because the active metabolite is formed by CYP450 enzymes, some of which are polymorphic or subject to inhibition by other drugs, not all patients will have adequate platelet inhibition.
Dose dependent inhibition of platelet aggregation can be seen 2 hours after single oral doses of PLAVIX. Repeated doses of 75 mg PLAVIX per day inhibit ADP-induced platelet aggregation on the first day, and inhibition reaches steady state between Day 3 and Day 7. At steady state, the average inhibition level observed with a dose of 75 mg PLAVIX per day was between 40% and 60%. Platelet aggregation and bleeding time gradually return to baseline values after treatment is discontinued, generally in about 5 days.
Pharmacokinetics
Absorption
After single and repeated oral doses of 75 mg per day, clopidogrel is rapidly absorbed. Mean peak plasma levels of unchanged clopidogrel (approximately 2.2-2.5 ng/mL after a single 75-mg oral dose) occurred approximately 45 minutes after dosing. Absorption is at least 50%, based on urinary excretion of clopidogrel metabolites.
Effect of Food
The effect of food on the bioavailability of the parent compound or active metabolite is currently not known.
Distribution
Clopidogrel and the main circulating inactive metabolite bind reversibly in vitro to human plasma proteins (98% and 94%, respectively). The binding is nonsaturable in vitro up to a concentration of 100 mcg/mL.
Metabolism
Clopidogrel is extensively metabolized by the liver. In vitro and in vivo, clopidogrel is metabolized according to two main metabolic pathways: one mediated by esterases and leading to hydrolysis into its inactive carboxylic acid derivative (85% of circulating metabolites), and one mediated by multiple cytochromes P450. Cytochromes first oxidize clopidogrel to a 2-oxo-clopidogrel intermediate metabolite. Subsequent metabolism of the 2-oxo-clopidogrel intermediate metabolite results in formation of the active metabolite, a thiol derivative of clopidogrel. In vitro, this metabolic pathway is mediated by CYP3A4, CYP2C19, CYP1A2 and CYP2B6. The active thiol metabolite which has been isolated in vitro, binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation.
Elimination
Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% of total radioactivity was excreted in urine and approximately 46% in feces over the 5 days post-dosing. After a single, oral dose of 75 mg, clopidogrel has a half-life of approximately 6 hours. The elimination half-life of the inactive acid metabolite was 8 hours after single and repeated administration. Covalent binding to platelets accounted for 2% of radiolabel with a half-life of 11 days. In plasma and urine, the glucuronide of the carboxylic acid derivative is also observed.
Pharmacogenetics
Several polymorphic CYP450 enzymes activate clopidogrel. CYP2C19 is involved in the formation of both the active metabolite and the 2-oxo-clopidogrel intermediate metabolite. Clopidogrel active metabolite pharmacokinetics and antiplatelet effects, as measured by ex vivo platelet aggregation assays, differ according to CYP2C19 genotype. The CYP2C19*1 allele corresponds to fully functional metabolism while the CYP2C19*2 and CYP2C19*3 alleles correspond to reduced metabolism. The CYP2C19*2 and CYP2C19*3 alleles account for 85% of reduced function alleles in whites and 99% in Asians. Other alleles associated with reduced metabolism include CYP2C19*4, *5, *6, *7, and *8, but these are less frequent in the general population. Published frequencies for the common CYP2C19 phenotypes and genotypes are listed in the table below.
Frequency (%) |
|||
|---|---|---|---|
| White (n=1356) | Black (n=966) | Chinese (n=573) | |
| Extensive metabolism: CYP2C19*1/*1 | 74 | 66 | 38 |
| Intermediate metabolism: CYP2C19*1/*2 or *1/*3 | 26 | 29 | 50 |
| Poor metabolism: CYP2C19*2/*2, *2/*3 or *3/*3 | 2 | 4 | 14 |
To date, the impact of CYP2C19 genotype on the pharmacokinetics of clopidogrel's active metabolite has been evaluated in 227 subjects from 7 reported studies. Reduced CYP2C19 metabolism in intermediate and poor metabolizers decreased the Cmax and AUC of the active metabolite by 30-50% following 300- or 600 mg loading doses and 75 mg maintenance doses. Lower active metabolite exposure results in less platelet inhibition or higher residual platelet reactivity. To date, diminished antiplatelet responses to clopidogrel have been described for intermediate and poor metabolizers in 21 reported studies involving 4,520 subjects. The relative difference in antiplatelet response between genotype groups varies across studies depending on the method used to evaluate response, but is typically greater than 30%.
The association between CYP2C19 genotype and clopidogrel treatment outcome was evaluated in 2 post-hoc clinical trial analyses (substudies of CLARITY-TIMI 28






Pharmacogenetic testing can identify genotypes associated with variability in CYP2C19 activity.
There may be genetic variants of other CYP450 enzymes with effects on the ability to form clopidogrel's active metabolite.
Special Populations
The pharmacokinetics of clopidogrel's active metabolite is not known in these special populations.
Geriatric Patients
In elderly (≥75 years) volunteers compared to young healthy volunteers, there were no differences in platelet aggregation and bleeding time. No dosage adjustment is needed for the elderly.
Renally-Impaired Patients
After repeated doses of 75 mg PLAVIX per day in patients with severe renal impairment (creatinine clearance from 5 to 15 mL/min), inhibition of ADP-induced platelet aggregation was lower (25%) than that observed in healthy volunteers, however, the prolongation of bleeding time was similar to healthy volunteers receiving 75 mg of PLAVIX per day.
Hepatically-Impaired Patients
After repeated doses of 75 mg PLAVIX per day for 10 days in patients with severe hepatic impairment, inhibition of ADP-induced platelet aggregation was similar to that observed in healthy subjects. The mean bleeding time prolongation was also similar in the two groups.
Gender
In a small study comparing men and women, less inhibition of ADP-induced platelet aggregation was observed in women, but there was no difference in prolongation of bleeding time. In the large, controlled clinical study (Clopidogrel vs. Aspirin in Patients at Risk of Ischemic Events; CAPRIE), the incidence of clinical outcome events, other adverse clinical events, and abnormal clinical laboratory parameters was similar in men and women.
Race
The prevalence of CYP2C19 alleles that result in intermediate and poor CYP2C19 metabolism differs according to race/ethnicity (see CLINICAL PHARMACOLOGY: Pharmacogenetics ).
CLINICAL STUDIES
The clinical evidence for the efficacy of PLAVIX is derived from four double-blind trials involving 81,090 patients: the CAPRIE study (Clopidogrel vs. Aspirin in Patients at Risk of Ischemic Events), a comparison of PLAVIX to aspirin, and the CURE (Clopidogrel in Unstable Angina to Prevent Recurrent Ischemic Events), the COMMIT/CCS-2 (Clopidogrel and Metoprolol in Myocardial Infarction Trial / Second Chinese Cardiac Study) studies comparing PLAVIX to placebo, both given in combination with aspirin and other standard therapy and CLARITY-TIMI 28 (Clopidogrel as Adjunctive Reperfusion Therapy – Thrombolysis in Myocardial Infarction).
Recent Myocardial Infarction (MI), Recent Stroke or Established Peripheral Arterial Disease
The CAPRIE trial was a 19,185-patient, 304-center, international, randomized, double-blind, parallel-group study comparing PLAVIX (75 mg daily) to aspirin (325 mg daily). The patients randomized had: 1) recent histories of myocardial infarction (within 35 days); 2) recent histories of ischemic stroke (within 6 months) with at least a week of residual neurological signs; or 3) objectively established peripheral arterial disease. Patients received randomized treatment for an average of 1.6 years (maximum of 3 years).
The trial's primary outcome was the time to first occurrence of new ischemic stroke (fatal or not), new myocardial infarction (fatal or not), or other vascular death. Deaths not easily attributable to nonvascular causes were all classified as vascular.
| Patients |
PLAVIX
9599 |
aspirin
9586 |
|---|---|---|
| IS (fatal or not) | 438 (4.6%) | 461 (4.8%) |
| MI (fatal or not) | 275 (2.9%) | 333 (3.5%) |
| Other vascular death | 226 (2.4%) | 226 (2.4%) |
| Total | 939 (9.8%) | 1020 (10.6%) |
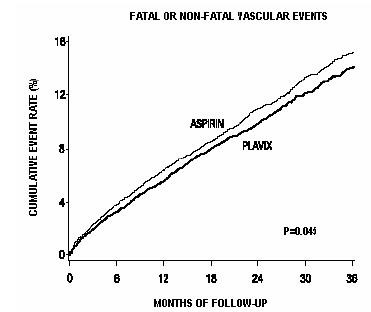
As shown in the table, PLAVIX (clopidogrel bisulfate) was associated with a lower incidence of outcome events of every kind. The overall risk reduction (9.8% vs. 10.6%) was 8.7%, P=0.045. Similar results were obtained when all-cause mortality and all-cause strokes were counted instead of vascular mortality and ischemic strokes (risk reduction 6.9%). In patients who survived an on-study stroke or myocardial infarction, the incidence of subsequent events was again lower in the PLAVIX group.
The curves showing the overall event rate are shown in Figure 1. The event curves separated early and continued to diverge over the 3-year follow-up period.
| Figure 1: Fatal or Non-Fatal Vascular Events in the CAPRIE Study |
|
Although the statistical significance favoring PLAVIX over aspirin was marginal (P=0.045), and represents the result of a single trial that has not been replicated, the comparator drug, aspirin, is itself effective (vs. placebo) in reducing cardiovascular events in patients with recent myocardial infarction or stroke. Thus, the difference between PLAVIX and placebo, although not measured directly, is substantial.
The CAPRIE trial included a population that was randomized on the basis of 3 entry criteria. The efficacy of PLAVIX relative to aspirin was heterogeneous across these randomized subgroups (P=0.043). It is not clear whether this difference is real or a chance occurrence. Although the CAPRIE trial was not designed to evaluate the relative benefit of PLAVIX over aspirin in the individual patient subgroups, the benefit appeared to be strongest in patients who were enrolled because of peripheral vascular disease (especially those who also had a history of myocardial infarction) and weaker in stroke patients. In patients who were enrolled in the trial on the sole basis of a recent myocardial infarction, PLAVIX was not numerically superior to aspirin.
In the meta-analyses of studies of aspirin vs. placebo in patients similar to those in CAPRIE, aspirin was associated with a reduced incidence of thrombotic events. There was a suggestion of heterogeneity in these studies too, with the effect strongest in patients with a history of myocardial infarction, weaker in patients with a history of stroke, and not discernible in patients with a history of peripheral vascular disease. With respect to the inferred comparison of PLAVIX to placebo, there is no indication of heterogeneity.
Acute Coronary Syndrome
The CURE study included 12,562 patients with acute coronary syndrome without ST segment elevation (unstable angina or non-Q-wave myocardial infarction) and presenting within 24 hours of onset of the most recent episode of chest pain or symptoms consistent with ischemia. Patients were required to have either ECG changes compatible with new ischemia (without ST segment elevation) or elevated cardiac enzymes or troponin I or T to at least twice the upper limit of normal. The patient population was largely Caucasian (82%) and included 38% women, and 52% patients ≥65 years of age.
Patients were randomized to receive PLAVIX (300 mg loading dose followed by 75 mg/day) or placebo, and were treated for up to one year. Patients also received aspirin (75–325 mg once daily) and other standard therapies such as heparin. The use of GPIIb/IIIa inhibitors was not permitted for three days prior to randomization.
The number of patients experiencing the primary outcome (CV death, MI, or stroke) was 582 (9.30%) in the PLAVIX-treated group and 719 (11.41%) in the placebo-treated group, a 20% relative risk reduction (95% CI of 10%–28%; p=0.00009) for the PLAVIX-treated group (see Table 3).
At the end of 12 months, the number of patients experiencing the co-primary outcome (CV death, MI, stroke or refractory ischemia) was 1035 (16.54%) in the PLAVIX-treated group and 1187 (18.83%) in the placebo-treated group, a 14% relative risk reduction (95% CI of 6%–21%, p=0.0005) for the PLAVIX-treated group (see Table 3).
In the PLAVIX-treated group, each component of the two primary endpoints (CV death, MI, stroke, refractory ischemia) occurred less frequently than in the placebo-treated group.
| Outcome | PLAVIX (+ aspirin)  |
Placebo (+ aspirin)  |
Relative Risk Reduction (%) (95% CI) |
|
|---|---|---|---|---|
| (n=6259) | (n=6303) | |||
| Primary outcome | 582 | (9.3%) | 719 (11.4%) | 20% |
| (Cardiovascular death, MI, Stroke) | (10.3, 27.9) | |||
| P=0.00009 | ||||
| Co-primary outcome | 1035 | (16.5%) | 1187 (18.8%) | 14% |
| (Cardiovascular death, MI, Stroke, Refractory Ischemia) | (6.2, 20.6) | |||
| P=0.00052 | ||||
All Individual Outcome Events: |
||||
| CV death | 318 | (5.1%) | 345 (5.5%) | 7% (-7.7, 20.6) |
| MI | 324 | (5.2%) | 419 (6.6%) | 23% (11.0, 33.4) |
| Stroke | 75 | (1.2%) | 87 (1.4%) | 14% (-17.7, 36.6) |
| Refractory ischemia | 544 | (8.7%) | 587 (9.3%) | 7% (-4.0, 18.0) |
The benefits of PLAVIX (clopidogrel bisulfate) were maintained throughout the course of the trial (up to 12 months).
| Figure 2: Cardiovascular Death, Myocardial Infarction, and Stroke in the CURE Study |
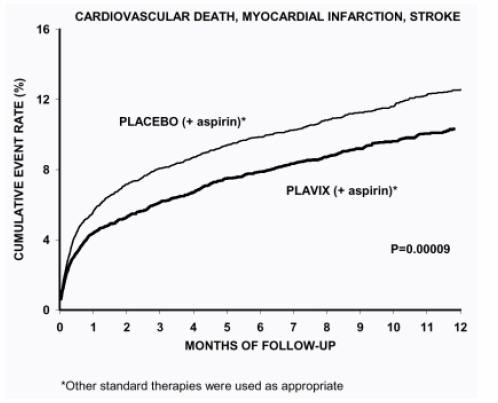
|
In CURE, the use of PLAVIX was associated with a lower incidence of CV death, MI or stroke in patient populations with different characteristics, as shown in Figure 3. The benefits associated with PLAVIX were independent of the use of other acute and long-term cardiovascular therapies, including heparin/LMWH (low molecular weight heparin), IV glycoprotein IIb/IIIa (GPIIb/IIIa) inhibitors, lipid-lowering drugs, beta-blockers, and ACE-inhibitors. The efficacy of PLAVIX was observed independently of the dose of aspirin (75–325 mg once daily). The use of oral anticoagulants, non-study anti-platelet drugs and chronic NSAIDs was not allowed in CURE.
| Figure 3: Hazard Ratio for Patient Baseline Characteristics and On-Study Concomitant Medications/Interventions for the CURE Study |
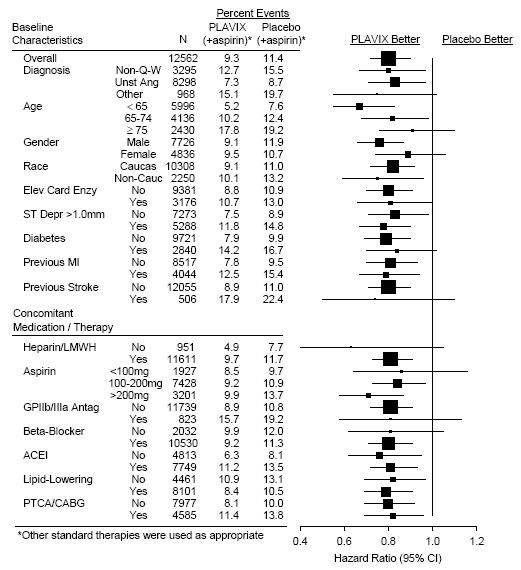
|
The use of PLAVIX in CURE was associated with a decrease in the use of thrombolytic therapy (71 patients [1.1%] in the PLAVIX group, 126 patients [2.0%] in the placebo group; relative risk reduction of 43%, P=0.0001), and GPIIb/IIIa inhibitors (369 patients [5.9%] in the PLAVIX group, 454 patients [7.2%] in the placebo group, relative risk reduction of 18%, P=0.003). The use of PLAVIX in CURE did not impact the number of patients treated with CABG or PCI (with or without stenting), (2253 patients [36.0%] in the PLAVIX group, 2324 patients [36.9%] in the placebo group; relative risk reduction of 4.0%, P=0.1658).
In patients with ST-segment elevation acute myocardial infarction, safety and efficacy of clopidogrel have been evaluated in two randomized, placebo-controlled, double-blind studies, COMMIT- a large outcome study conducted in China - and CLARITY- a supportive study of a surrogate endpoint conducted internationally.
The randomized, double-blind, placebo-controlled, 2×2 factorial design COMMIT trial included 45,852 patients presenting within 24 hours of the onset of the symptoms of suspected myocardial infarction with supporting ECG abnormalities (i.e., ST elevation, ST depression or left bundle-branch block). Patients were randomized to receive PLAVIX (75 mg/day) or placebo, in combination with aspirin (162 mg/day), for 28 days or until hospital discharge whichever came first.
The co-primary endpoints were death from any cause and the first occurrence of re-infarction, stroke or death.
The patient population included 28% women, 58% patients ≥60 years (26% patients ≥70 years) and 55% patients who received thrombolytics, 68% received ace-inhibitors, and only 3% had percutaneous coronary intervention (PCI).
As shown in Table 4 and Figures 4 and 5 below, PLAVIX significantly reduced the relative risk of death from any cause by 7% (p = 0.029), and the relative risk of the combination of re-infarction, stroke or death by 9% (p = 0.002).
| Event | PLAVIX (+ aspirin) (N=22961) |
Placebo (+ aspirin) (N=22891) |
Odds ratio (95% CI) |
p-value |
|---|---|---|---|---|
Composite endpoint: Death, MI, or Stroke |
2121 (9.2%) | 2310 (10.1%) | 0.91 (0.86, 0.97) | 0.002 |
| Death | 1726 (7.5%) | 1845 (8.1%) | 0.93 (0.87, 0.99) | 0.029 |
Non-fatal MI |
270 (1.2%) | 330 (1.4%) | 0.81 (0.69, 0.95) | 0.011 |
Non-fatal Stroke |
127 (0.6%) | 142 (0.6%) | 0.89 (0.70, 1.13) | 0.33 |
Figure 4: Cumulative Event Rates for Death in the COMMIT Study |
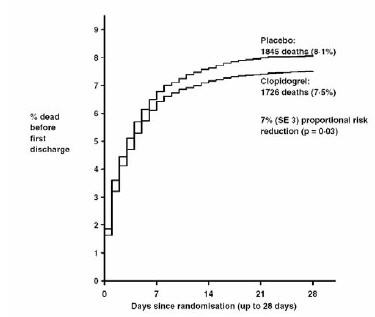
|
Figure 5: Cumulative Event Rates for the Combined Endpoint Re-Infarction, Stroke or Death in the COMMIT Study |
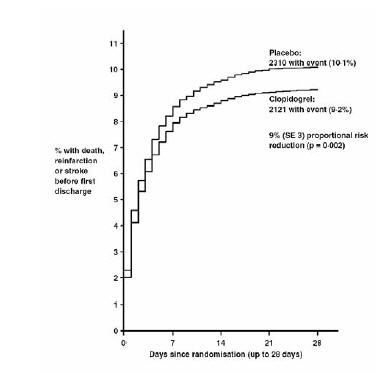
|
The effect of PLAVIX did not differ significantly in various pre-specified subgroups as shown in Figure 6. Additionally, the effect was similar in non-prespecified subgroups including those based on infarct location, Killip class or prior MI history (see Figure 7). Such subgroup analyses should be interpreted very cautiously.
| Figure 6: Effects of Adding PLAVIX to Aspirin on the Combined Primary Endpoint across Baseline and Concomitant Medication Subgroups for the COMMIT Study |
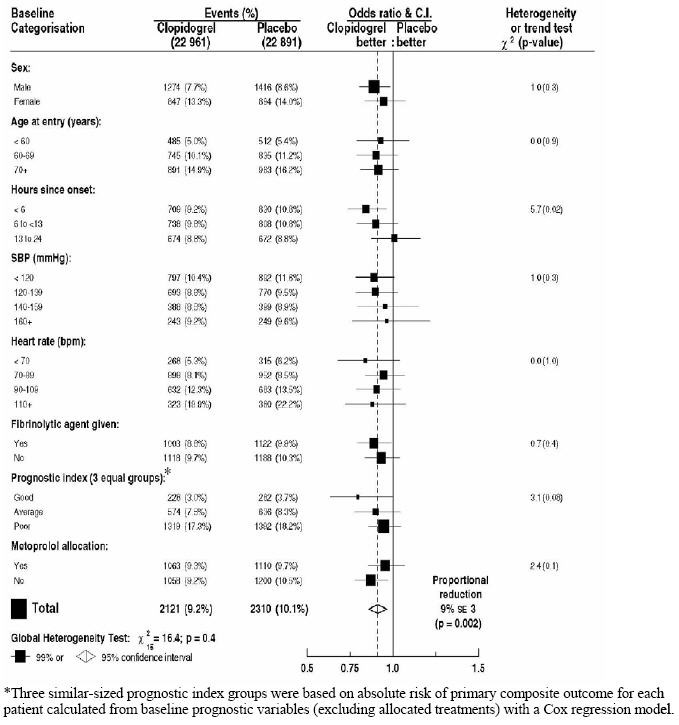
|
| Figure 7: Effects of Adding PLAVIX to Aspirin in the Non-Prespecified Subgroups in the COMMIT Study |
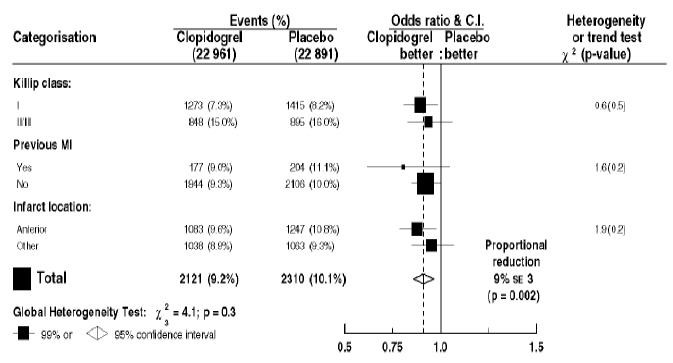
|
The randomized, double-blind, placebo-controlled CLARITY trial included 3,491 patients, 5% U.S., presenting within 12 hours of the onset of a ST elevation myocardial infarction and planned for thrombolytic therapy. Patients were randomized to receive PLAVIX (300-mg loading dose, followed by 75 mg/day) or placebo until angiography, discharge, or Day 8. Patients also received aspirin (150 to 325 mg as a loading dose, followed by 75 to 162 mg/day), a fibrinolytic agent and, when appropriate, heparin for 48 hours. The patients were followed for 30 days.
The primary endpoint was the occurrence of the composite of an occluded infarct-related artery (defined as TIMI Flow Grade 0 or 1) on the predischarge angiogram, or death or recurrent myocardial infarction by the time of the start of coronary angiography.
The patient population was mostly Caucasian (89.5%) and included 19.7% women and 29.2% patients ≥65 years. A total of 99.7% of patients received fibrinolytics (fibrin specific: 68.7%, non-fibrin specific: 31.1%), 89.5% heparin, 78.7% beta-blockers, 54.7% ACE inhibitors and 63% statins.
The number of patients who reached the primary endpoint was 262 (15.0%) in the PLAVIX-treated group and 377 (21.7%) in the placebo group, but most of the events related to the surrogate endpoint of vessel patency.
| Clopidogrel 1752 |
Placebo 1739 |
OR | 95% CI | |
|---|---|---|---|---|
| *The total number of patients with a component event (occluded IRA, death, or recurrent MI) is greater than the number of patients with a composite event because some patients had more than a single type of component event. | ||||
| Number (%) of patients reporting the composite endpoint | 262 (15.0%) | 377 (21.7%) | 0.64 | 0.53, 0.76 |
| Occluded IRA | ||||
| N (subjects undergoing angiography) | 1640 | 1634 | ||
| n (%) patients reporting endpoint | 192 (11.7%) | 301 (18.4%) | 0.59 | 0.48, 0.72 |
| Death | ||||
| n (%) patients reporting endpoint | 45 (2.6%) | 38 (2.2%) | 1.18 | 0.76, 1.83 |
| Recurrent MI | ||||
| n (%) patients reporting endpoint | 44 (2.5%) | 62 (3.6%) | 0.69 | 0.47, 1.02 |
PLAVIX INDICATIONS AND USAGE
PLAVIX (clopidogrel bisulfate) is indicated for the reduction of atherothrombotic events as follows:
-
Recent MI, Recent Stroke or Established Peripheral Arterial Disease
For patients with a history of recent myocardial infarction (MI), recent stroke, or established peripheral arterial disease, PLAVIX has been shown to reduce the rate of a combined endpoint of new ischemic stroke (fatal or not), new MI (fatal or not), and other vascular death. -
Acute Coronary Syndrome
- -For patients with non-ST-segment elevation acute coronary syndrome (unstable angina/non-Q-wave MI) including patients who are to be managed medically and those who are to be managed with percutaneous coronary intervention (with or without stent) or CABG, PLAVIX has been shown to decrease the rate of a combined endpoint of cardiovascular death, MI, or stroke as well as the rate of a combined endpoint of cardiovascular death, MI, stroke, or refractory ischemia.
- -For patients with ST-segment elevation acute myocardial infarction, PLAVIX has been shown to reduce the rate of death from any cause and the rate of a combined endpoint of death, re-infarction or stroke. This benefit is not known to pertain to patients who receive primary angioplasty.
PLAVIX CONTRAINDICATIONS
The use of PLAVIX is contraindicated in the following conditions:
- Hypersensitivity to the drug substance or any component of the product.
- Active pathological bleeding such as peptic ulcer or intracranial hemorrhage.
WARNINGS
Thrombotic thrombocytopenic purpura (TTP)
TTP has been reported rarely following use of PLAVIX, sometimes after a short exposure (<2 weeks). TTP is a serious condition that can be fatal and requires urgent treatment including plasmapheresis (plasma exchange). It is characterized by thrombocytopenia, microangiopathic hemolytic anemia (schistocytes [fragmented RBCs] seen on peripheral smear), neurological findings, renal dysfunction, and fever. (See ADVERSE REACTIONS .)
PRECAUTIONS
General: PLAVIX prolongs the bleeding time and therefore should be used with caution in patients who may be at risk of increased bleeding from trauma, surgery, or other pathological conditions (particularly gastrointestinal and intraocular). If a patient is to undergo elective surgery and an antiplatelet effect is not desired, PLAVIX should be discontinued 5 days prior to surgery.
Due to the risk of bleeding and undesirable hematological effects, blood cell count determination and/or other appropriate testing should be promptly considered, whenever such suspected clinical symptoms arise during the course of treatment (see ADVERSE REACTIONS ).
In patients with recent TIA or stroke who are at high risk of recurrent ischemic events, the combination of aspirin and PLAVIX has not been shown to be more effective than PLAVIX alone, but the combination has been shown to increase major bleeding.
Pharmacogenetics: Based on literature data, patients with genetically reduced CYP2C19 function have lower systemic exposure to the active metabolite of clopidogrel and diminished antiplatelet responses, and generally exhibit higher cardiovascular event rates following myocardial infarction than do patients with normal CYP2C19 function (see CLINICAL PHARMACOLOGY: Pharmacogenetics ).
GI Bleeding: In CAPRIE, PLAVIX was associated with a rate of gastrointestinal bleeding of 2.0%, vs. 2.7% on aspirin. In CURE, the incidence of major gastrointestinal bleeding was 1.3% vs. 0.7% (PLAVIX + aspirin vs. placebo + aspirin, respectively). PLAVIX should be used with caution in patients who have lesions with a propensity to bleed (such as ulcers). Drugs that might induce such lesions should be used with caution in patients taking PLAVIX.
Use in Hepatically-Impaired Patients: Experience is limited in patients with severe hepatic disease, who may have bleeding diatheses. PLAVIX should be used with caution in this population.
Use in Renally-Impaired Patients: Experience is limited in patients with severe renal impairment. PLAVIX should be used with caution in this population.
Information for Patients
Patients should be told that it may take them longer than usual to stop bleeding, that they may bruise and/or bleed more easily when they take PLAVIX or PLAVIX combined with aspirin, and that they should report any unusual bleeding to their physician. Patients should inform physicians and dentists that they are taking PLAVIX and/or any other product known to affect bleeding before any surgery is scheduled and before any new drug is taken.
Drug Interactions
Since clopidogrel is metabolized to its active metabolite by CYP2C19, use of drugs that inhibit the activity of this enzyme would be expected to result in reduced drug levels of the active metabolite of clopidogrel and a reduction in clinical efficacy. Concomitant use of drugs that inhibit CYP2C19 (e.g., omeprazole) should be discouraged.
Study of specific drug interactions yielded the following results:
Aspirin
Aspirin did not modify the clopidogrel-mediated inhibition of ADP-induced platelet aggregation. Concomitant administration of 500 mg of aspirin twice a day for 1 day did not significantly increase the prolongation of bleeding time induced by PLAVIX. PLAVIX potentiated the effect of aspirin on collagen-induced platelet aggregation. PLAVIX and aspirin have been administered together for up to one year.
Heparin
In a study in healthy volunteers, PLAVIX did not necessitate modification of the heparin dose or alter the effect of heparin on coagulation. Coadministration of heparin had no effect on inhibition of platelet aggregation induced by PLAVIX.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
In healthy volunteers receiving naproxen, concomitant administration of PLAVIX was associated with increased occult gastrointestinal blood loss. NSAIDs and PLAVIX should be coadministered with caution.
Warfarin
Because of the increased risk of bleeding, the concomitant administration of warfarin with PLAVIX should be undertaken with caution. (See PRECAUTIONS: General .)
Other Concomitant Therapy
No clinically significant pharmacodynamic interactions were observed when PLAVIX was coadministered with atenolol, nifedipine, or both atenolol and nifedipine. The pharmacodynamic activity of PLAVIX was also not significantly influenced by the coadministration of phenobarbital, cimetidine or estrogen.
The pharmacokinetics of digoxin or theophylline were not modified by the coadministration of PLAVIX (clopidogrel bisulfate).
At high concentrations in vitro, clopidogrel inhibits P450 (2C9). Accordingly, PLAVIX may interfere with the metabolism of phenytoin, tamoxifen, tolbutamide, warfarin, torsemide, fluvastatin, and many non-steroidal anti-inflammatory agents, but there are no data with which to predict the magnitude of these interactions. Caution should be used when any of these drugs is coadministered with PLAVIX.
In addition to the above specific interaction studies, patients entered into clinical trials with PLAVIX received a variety of concomitant medications including diuretics, beta-blocking agents, angiotensin converting enzyme inhibitors, calcium antagonists, cholesterol lowering agents, coronary vasodilators, antidiabetic agents (including insulin), thrombolytics, heparins (unfractionated and LMWH), GPIIb/IIIa antagonists, antiepileptic agents and hormone replacement therapy without evidence of clinically significant adverse interactions.
There are no data on the concomitant use of oral anticoagulants, non study oral anti-platelet drugs and chronic NSAIDs with clopidogrel.
Drug/Laboratory Test Interactions
None known.
Carcinogenesis, Mutagenesis, Impairment of Fertility
There was no evidence of tumorigenicity when clopidogrel was administered for 78 weeks to mice and 104 weeks to rats at dosages up to 77 mg/kg per day, which afforded plasma exposures >25 times that in humans at the recommended daily dose of 75 mg.
Clopidogrel was not genotoxic in four in vitro tests (Ames test, DNA-repair test in rat hepatocytes, gene mutation assay in Chinese hamster fibroblasts, and metaphase chromosome analysis of human lymphocytes) and in one in vivo test (micronucleus test by oral route in mice).
Clopidogrel was found to have no effect on fertility of male and female rats at oral doses up to 400 mg/kg per day (52 times the recommended human dose on a mg/m2 basis).
Pregnancy
Pregnancy Category B
Reproduction studies performed in rats and rabbits at doses up to 500 and 300 mg/kg/day (respectively, 65 and 78 times the recommended daily human dose on a mg/m2 basis), revealed no evidence of impaired fertility or fetotoxicity due to clopidogrel. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of a human response, PLAVIX should be used during pregnancy only if clearly needed.
Nursing Mothers
Studies in rats have shown that clopidogrel and/or its metabolites are excreted in the milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the nursing woman.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established.
Geriatric Use
Of the total number of subjects in the CAPRIE, CURE and CLARITY controlled clinical studies, approximately 50% of patients treated with PLAVIX were 65 years of age and older, and 15% were 75 years and older. In COMMIT, approximately 58% of the patients treated with PLAVIX were 60 years and older, 26% of whom were 70 years and older.
The observed risk of thrombotic events with clopidogrel plus aspirin versus placebo plus aspirin by age category is provided in Figures 3 and 6 for the CURE and COMMIT trials, respectively (see CLINICAL STUDIES ). The observed risk of bleeding events with clopidogrel plus aspirin versus placebo plus aspirin by age category is provided in Tables 6 and 7 for the CURE and COMMIT trials, respectively (see ADVERSE REACTIONS ).
PLAVIX ADVERSE REACTIONS
PLAVIX has been evaluated for safety in more than 42,000 patients, including over 9,000 patients treated for 1 year or more. The clinically important adverse events observed in CAPRIE, CURE, CLARITY and COMMIT are discussed below.
The overall tolerability of PLAVIX in CAPRIE was similar to that of aspirin regardless of age, gender and race, with an approximately equal incidence (13%) of patients withdrawing from treatment because of adverse reactions.
Hemorrhagic
In CAPRIE patients receiving PLAVIX, gastrointestinal hemorrhage occurred at a rate of 2.0%, and required hospitalization in 0.7%. In patients receiving aspirin, the corresponding rates were 2.7% and 1.1%, respectively. The incidence of intracranial hemorrhage was 0.4% for PLAVIX compared to 0.5% for aspirin.
In CURE, PLAVIX use with aspirin was associated with an increase in bleeding compared to placebo with aspirin (see Table 6). There was an excess in major bleeding in patients receiving PLAVIX plus aspirin compared with placebo plus aspirin, primarily gastrointestinal and at puncture sites. The incidence of intracranial hemorrhage (0.1%), and fatal bleeding (0.2%), were the same in both groups.
The overall incidence of bleeding is described in Table 6 for patients receiving both PLAVIX and aspirin in CURE.
| Event | PLAVIX (+ aspirin)  (n=6259) |
Placebo (+ aspirin)  (n=6303) |
P-value |
|---|---|---|---|
Major bleeding  |
3.7  Major bleeding event rates for PLAVIX + aspirin by age were: <65 years = 2.5%, ≥65 to <75 years = 4.1%, ≥75 years 5.9% |
2.7  Major bleeding event rates for placebo + aspirin by age were: <65 years = 2.1%, ≥65 to <75 years = 3.1%, ≥75 years 3.6% |
0.001 |
| Life-threatening bleeding | 2.2 | 1.8 | 0.13 |
| Fatal | 0.2 | 0.2 | |
| 5 g/dL hemoglobin drop | 0.9 | 0.9 | |
| Requiring surgical intervention | 0.7 | 0.7 | |
| Hemorrhagic strokes | 0.1 | 0.1 | |
| Requiring inotropes | 0.5 | 0.5 | |
| Requiring transfusion (≥4 units) | 1.2 | 1.0 | |
| Other major bleeding | 1.6 | 1.0 | 0.005 |
| Significantly disabling | 0.4 | 0.3 | |
| Intraocular bleeding with significant loss of vision | 0.05 | 0.03 | |
| Requiring 2–3 units of blood | 1.3 | 0.9 | |
Minor bleeding  |
5.1 | 2.4 | <0.001 |
Ninety-two percent (92%) of the patients in the CURE study received heparin/LMWH, and the rate of bleeding in these patients was similar to the overall results.
There was no excess in major bleeds within seven days after coronary bypass graft surgery in patients who stopped therapy more than five days prior to surgery (event rate 4.4% PLAVIX + aspirin; 5.3% placebo + aspirin). In patients who remained on therapy within five days of bypass graft surgery, the event rate was 9.6% for PLAVIX + aspirin, and 6.3% for placebo + aspirin.
In CLARITY, the incidence of major bleeding (defined as intracranial bleeding or bleeding associated with a fall in hemoglobin > 5 g/dL) was similar between groups (1.3% versus 1.1% in the PLAVIX + aspirin and in the placebo + aspirin groups, respectively). This was consistent across subgroups of patients defined by baseline characteristics, and type of fibrinolytics or heparin therapy. The incidence of fatal bleeding (0.8% versus 0.6% in the PLAVIX + aspirin and in the placebo + aspirin groups, respectively) and intracranial hemorrhage (0.5% versus 0.7%, respectively) was low and similar in both groups.
The overall rate of noncerebral major bleeding or cerebral bleeding in COMMIT was low and similar in both groups as shown in Table 7 below.
| Type of bleeding | PLAVIX (+ aspirin) (N=22961) |
Placebo (+ aspirin) (N=22891) |
P-value |
|---|---|---|---|
Major  |
134 (0.6%) | 125 (0.5%) | 0.59 |
| Major noncerebral | 82 (0.4%) | 73 (0.3%) | 0.48 |
| Fatal | 36 (0.2%) | 37 (0.2%) | 0.90 |
| Hemorrhagic stroke | 55 (0.2%) | 56 (0.2%) | 0.91 |
| Fatal | 39 (0.2%) | 41 (0.2%) | 0.81 |
| Other noncerebral bleeding (non-major) | 831 (3.6%) | 721 (3.1%) | 0.005 |
| Any noncerebral bleeding | 896 (3.9%) | 777 (3.4%) | 0.004 |
Adverse events occurring in ≥2.5% of patients on PLAVIX in the CAPRIE controlled clinical trial are shown below regardless of relationship to PLAVIX. The median duration of therapy was 20 months, with a maximum of 3 years.
| % Incidence (% Discontinuation) | ||
|---|---|---|
|
Body System
Event |
PLAVIX [n=9599] |
Aspirin [n=9586] |
| Body as a Whole – general disorders | ||
| Chest Pain | 8.3 (0.2) | 8.3 (0.3) |
| Accidental/Inflicted Injury | 7.9 (0.1) | 7.3 (0.1) |
| Influenza-like symptoms | 7.5 (<0.1) | 7.0 (<0.1) |
| Pain | 6.4 (0.1) | 6.3 (0.1) |
| Fatigue | 3.3 (0.1) | 3.4 (0.1) |
| Cardiovascular disorders, general | ||
| Edema | 4.1 (<0.1) | 4.5 (<0.1) |
| Hypertension | 4.3 (<0.1) | 5.1 (<0.1) |
| Central & peripheral nervous system disorders | ||
| Headache | 7.6 (0.3) | 7.2 (0.2) |
| Dizziness | 6.2 (0.2) | 6.7 (0.3) |
| Gastrointestinal system disorders | ||
| Any event | 27.1(3.2) | 29.8 (4.0) |
| Abdominal pain | 5.6 (0.7) | 7.1 (1.0) |
| Dyspepsia | 5.2 (0.6) | 6.1 (0.7) |
| Diarrhea | 4.5 (0.4) | 3.4 (0.3) |
| Nausea | 3.4 (0.5) | 3.8 (0.4) |
| Metabolic & nutritional disorders | ||
| Hypercholesterolemia | 4.0 (0) | 4.4 (<0.1) |
| Musculo-skeletal system disorders | ||
| Arthralgia | 6.3 (0.1) | 6.2 (0.1) |
| Back Pain | 5.8 (0.1) | 5.3 (<0.1) |
| Platelet, bleeding, & clotting disorders | ||
| Purpura/Bruise | 5.3 (0.3) | 3.7 (0.1) |
| Epistaxis | 2.9 (0.2) | 2.5 (0.1) |
| Psychiatric disorders | ||
| Depression | 3.6 (0.1) | 3.9 (0.2) |
| Respiratory system disorders | ||
| Upper resp tract infection | 8.7 (<0.1) | 8.3 (<0.1) |
| Dyspnea | 4.5 (0.1) | 4.7 (0.1) |
| Rhinitis | 4.2 (0.1) | 4.2 (<0.1) |
| Bronchitis | 3.7 (0.1) | 3.7 (0) |
| Coughing | 3.1 (<0.1) | 2.7(<0.1) |
| Skin & appendage disorders | ||
| Any event | 15.8 (1.5) | 13.1 (0.8) |
| Rash | 4.2 (0.5) | 3.5 (0.2) |
| Pruritus | 3.3 (0.3) | 1.6 (0.1) |
| Urinary system disorders | ||
| Urinary tract infection | 3.1 (0) | 3.5 (0.1) |
No additional clinically relevant events to those observed in CAPRIE with a frequency ≥2.5%, have been reported during the CURE and CLARITY controlled studies. COMMIT collected only limited safety data.
Other adverse experiences of potential importance occurring in 1% to 2.5% of patients receiving PLAVIX (clopidogrel bisulfate) in the controlled clinical trials are listed below regardless of relationship to PLAVIX. In general, the incidence of these events was similar to that in patients receiving aspirin (in CAPRIE) or placebo + aspirin (in the other clinical trials).
Autonomic Nervous System Disorders: Syncope, Palpitation. Body as a Whole-general disorders: Asthenia, Fever, Hernia. Cardiovascular disorders: Cardiac failure. Central and peripheral nervous system disorders: Cramps legs, Hypoaesthesia, Neuralgia, Paraesthesia, Vertigo. Gastrointestinal system disorders: Constipation, Vomiting. Heart rate and rhythm disorders: Fibrillation atrial. Liver and biliary system disorders: Hepatic enzymes increased. Metabolic and nutritional disorders: Gout, hyperuricemia, non-protein nitrogen (NPN) increased. Musculo-skeletal system disorders: Arthritis, Arthrosis. Platelet, bleeding & clotting disorders: GI hemorrhage, hematoma, platelets decreased. Psychiatric disorders: Anxiety, Insomnia. Red blood cell disorders: Anemia. Respiratory system disorders: Pneumonia, Sinusitis. Skin and appendage disorders: Eczema, Skin ulceration. Urinary system disorders: Cystitis. Vision disorders: Cataract, Conjunctivitis.
Other potentially serious adverse events which may be of clinical interest but were rarely reported (<1%) in patients who received PLAVIX in the controlled clinical trials are listed below regardless of relationship to PLAVIX. In general, the incidence of these events was similar to that in patients receiving aspirin (in CAPRIE) or placebo + aspirin (in the other clinical trials).
Body as a whole: Allergic reaction, necrosis ischemic. Cardiovascular disorders: Edema generalized. Gastrointestinal system disorders: Peptic, gastric or duodenal ulcer, gastritis, gastric ulcer perforated, gastritis hemorrhagic, upper GI ulcer hemorrhagic. Liver and Biliary system disorders: Bilirubinemia, hepatitis infectious, liver fatty. Platelet, bleeding and clotting disorders: hemarthrosis, hematuria, hemoptysis, hemorrhage intracranial, hemorrhage retroperitoneal, hemorrhage of operative wound, ocular hemorrhage, pulmonary hemorrhage, purpura allergic, thrombocytopenia. Red blood cell disorders: Anemia aplastic, anemia hypochromic. Reproductive disorders, female: Menorrhagia. Respiratory system disorders: Hemothorax. Skin and appendage disorders: Bullous eruption, rash erythematous, rash maculopapular, urticaria. Urinary system disorders: Abnormal renal function, acute renal failure. White cell and reticuloendothelial system disorders: Agranulocytosis, granulocytopenia, leukemia, leukopenia, neutropenia.
Postmarketing Experience
The following events have been reported spontaneously from worldwide postmarketing experience:
-
Body as a whole:
- -hypersensitivity reactions, anaphylactoid reactions, serum sickness
-
Central and Peripheral Nervous System disorders:
- -confusion, hallucinations, taste disorders
-
Hepato-biliary disorders:
- -abnormal liver function test, hepatitis (non-infectious), acute liver failure
-
Platelet, Bleeding and Clotting disorders:
- -cases of bleeding with fatal outcome (especially intracranial, gastrointestinal and retroperitoneal hemorrhage)
- -thrombotic thrombocytopenic purpura (TTP) – some cases with fatal outcome – (see WARNINGS )
- -agranulocytosis, aplastic anemia/pancytopenia
- -conjunctival, ocular and retinal bleeding
-
Respiratory, thoracic and mediastinal disorders:
- -bronchospasm, interstitial pneumonitis
-
Skin and subcutaneous tissue disorders:
- -angioedema, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, lichen planus
-
Renal and urinary disorders:
- -glomerulopathy, increased creatinine levels
-
Vascular disorders:
- -vasculitis, hypotension
-
Gastrointestinal disorders:
- -colitis (including ulcerative or lymphocytic colitis), pancreatitis, stomatitis
-
Musculoskeletal, connective tissue and bone disorders:
- -myalgia
OVERDOSAGE
Overdose following clopidogrel administration may lead to prolonged bleeding time and subsequent bleeding complications. A single oral dose of clopidogrel at 1500 or 2000 mg/kg was lethal to mice and to rats and at 3000 mg/kg to baboons. Symptoms of acute toxicity were vomiting (in baboons), prostration, difficult breathing, and gastrointestinal hemorrhage in all species.
Recommendations About Specific Treatment
Based on biological plausibility, platelet transfusion may be appropriate to reverse the pharmacological effects of PLAVIX if quick reversal is required.
PLAVIX DOSAGE AND ADMINISTRATION
Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
The recommended daily dose of PLAVIX is 75 mg once daily.
Acute Coronary Syndrome
For patients with non-ST-segment elevation acute coronary syndrome (unstable angina/non-Q-wave MI), PLAVIX should be initiated with a single 300-mg loading dose and then continued at 75 mg once daily. Aspirin (75 mg–325 mg once daily) should be initiated and continued in combination with PLAVIX. In CURE, most patients with Acute Coronary Syndrome also received heparin acutely (see CLINICAL STUDIES ).
For patients with ST-segment elevation acute myocardial infarction, the recommended dose of PLAVIX is 75 mg once daily, administered in combination with aspirin, with or without thrombolytics. PLAVIX may be initiated with or without a loading dose (300 mg was used in CLARITY; see CLINICAL STUDIES ).
Pharmacogenetics
CYP2C19 poor metabolizer status is associated with diminished response to clopidogrel. The optimal dose regimen for poor metabolizers has yet to be determined. (See CLINICAL PHARMACOLOGY: Pharmacogenetics .)
No dosage adjustment is necessary for elderly patients or patients with renal disease. (See CLINICAL PHARMACOLOGY: Special Populations.)
HOW SUPPLIED
PLAVIX (clopidogrel bisulfate) 75-mg tablets are available as pink, round, biconvex, film-coated tablets debossed with "75" on one side and "1171" on the other. Tablets are provided as follows:
- NDC 63653-1171-6 bottles of 30
- NDC 63653-1171-1 bottles of 90
- NDC 63653-1171-5 bottles of 500
- NDC 63653-1171-3 blisters of 100
PLAVIX (clopidogrel bisulfate) 300-mg tablets are available as pink, oblong, film-coated tablets debossed with "300" on one side and "1332" on the other. Tablets are provided as follows:
NDC 63653-1332-2 unit-dose packages of 30
NDC 63653-1332-3 unit-dose packages of 100
Storage
Store at 25° C (77° F); excursions permitted to 15°–30° C (59°–86° F) [See USP Controlled Room Temperature].
Distributed by:
Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership
Bridgewater, NJ 08807
PLAVIX® is a registered trademark.
Revised May 2009
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL
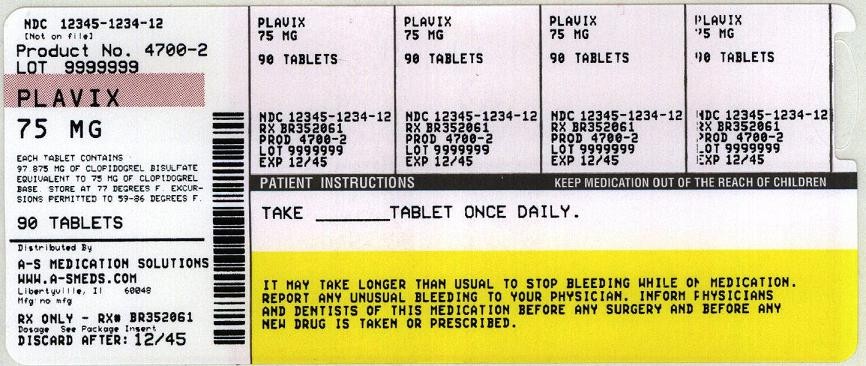
Plavixclopidogrel bisulfate TABLET, FILM COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||