Omnaris
FULL PRESCRIBING INFORMATION: CONTENTS*
- OMNARIS DESCRIPTION
- CLINICAL PHARMACOLOGY
- CLINICAL TRIALS
- OMNARIS INDICATIONS AND USAGE
- OMNARIS CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- OMNARIS ADVERSE REACTIONS
- OVERDOSAGE
- OMNARIS DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
OMNARIS DESCRIPTION
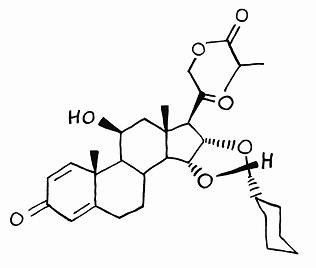
The active component of OMNARIS Nasal Spray is ciclesonide, a non-halogenated glucocorticoid having the chemical name pregna -1,4-diene-3,20-dione, 16,17-[[R-cyclohexylmethylene]bis(oxy)]-11-hydroxy-21-(2-methyl-1-oxopropoxy)-,(11β,16α)-. Ciclesonide is delivered as the R-epimer. The empirical formula is C32H44O7 and its molecular weight is 540.7. Its structural formula is as follows:
Ciclesonide is a white to yellow-white powder, practically insoluble in water and freely soluble in ethanol and acetone. OMNARIS Nasal Spray is a metered-dose, manual-pump spray formulation containing a hypotonic aqueous suspension of ciclesonide. OMNARIS Nasal Spray also contains microcrystalline cellulose, carboxymethylcellulose sodium, hypromellose, potassium sorbate and edetate sodium; and hydrochloric acid to adjust the pH to 4.5. The contents of one 12.5 gram bottle provide 120 actuations, after initial priming. Prior to initial use, OMNARIS Nasal Spray must be gently shaken and then the pump must be primed by actuating eight times. Once primed, each actuation of the pump delivers 50 mcg ciclesonide in a volume of 70 microliters from the nasal actuator. If the product is not used for four consecutive days, it should be gently shaken and reprimed with one spray or until a fine mist appears.
CLINICAL PHARMACOLOGY
Ciclesonide is a pro-drug that is enzymatically hydrolyzed to a pharmacologically active metabolite, C21-desisobutyryl-ciclesonide (des-ciclesonide or RM1) following intranasal application. Des-ciclesonide has anti-inflammatory activity with affinity for the glucocorticoid receptor that is 120 times higher than the parent compound.
The precise mechanism through which ciclesonide affects allergic rhinitis symptoms is not known. Corticosteroids have been shown to have a wide range of effects on multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, and lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, and cytokines) involved in allergic inflammation.
Absorption
Ciclesonide and des-ciclesonide have negligible oral bioavailability (both less than 1%) due to low gastrointestinal absorption and high first-pass metabolism. The intranasal administration of ciclesonide at recommended doses results in negligible serum concentrations of ciclesonide. However, the known active metabolite (des-ciclesonide) is detected in the serum of some patients after nasal inhalation of ciclesonide. The bioanalytical assay used has a lower limit of quantification of 25 pg/mL and 10 pg/mL, for ciclesonide and des-ciclesonide, respectively
In healthy adults treated for two weeks with 50 to 800 mcg of ciclesonide nasal spray daily (n=6 in each treatment group), the peak serum concentrations of des-ciclesonide in all subjects were found to be below 30 pg/mL. Of those treated with 800 mcg and 400 mcg daily, 100% and 67% had detectable levels of des-ciclesonide, respectively. With daily doses of 200 mcg or less, detectable serum levels of des-ciclesonide were not observed.
In pediatric subjects treated with 25 to 200 mcg of ciclesonide nasal spray daily, serum concentrations of des-ciclesonide were below 45 pg/mL, with the exception of one value of 64.5 pg/mL. In a 12-week study in children 6 to 11 years of age with perennial allergic rhinitis, des-ciclesonide was detected in 50% of the subjects treated with 200 mcg and in 5% of those treated with 100 mcg ciclesonide nasal spray daily. In a 6-week study in children 2 to 5 years of age with perennial allergic rhinitis, des-ciclesonide was detected in 41%, 22%, and 13% of the subjects treated with 200 mcg, 100 mcg, and 25 mcg ciclesonide nasal spray daily, respectively.
Distribution
Following intravenous administration of 800 mcg of ciclesonide, the volumes of distribution of ciclesonide and des-ciclesonide were approximately 2.9 L/kg and 12.1 L/kg, respectively. The percentage of ciclesonide and des-ciclesonide bound to human plasma proteins averaged ≥ 99% each, with ≤ 1% of unbound drug detected in the systemic circulation. Des-ciclesonide is not significantly bound to human transcortin.
Metabolism
Intranasal ciclesonide is hydrolyzed to a biologically active metabolite, des-ciclesonide, by esterases in the nasal mucosa. Des-ciclesonide undergoes further metabolism in the liver to additional metabolites mainly by the cytochrome P450 (CYP) 3A4 isozyme and to a lesser extent by CYP 2D6. The full range of potentially active metabolites of ciclesonide has not been characterized. After intravenous administration of 14C-ciclesonide, 19.3% of the resulting radioactivity in the plasma is accounted for by ciclesonide or des-ciclesonide; the remainder may be a result of other, as yet, unidentified multiple metabolites.
Elimination
Following intravenous administration of 800 mcg of ciclesonide, the clearance values of ciclesonide and des-ciclesonide were high (approximately 152 L/h and 228 L/h, respectively). 14C-labeled ciclesonide was predominantly excreted via the feces after intravenous administration (66%) indicating that excretion through bile is the major route of elimination. Approximately 20% or less of drug related radioactivity was excreted in the urine.
Special Populations
The pharmacokinetics of intranasally administered ciclesonide have not been assessed in patient subpopulations because the resulting blood levels of ciclesonide and des-ciclesonide are insufficient for pharmacokinetic calculations. However, population pharmacokinetic analysis showed that characteristics of des-ciclesonide after oral inhalation of ciclesonide were not appreciably influenced by a variety of subject characteristics such as body weight, age, race, and gender. Compared to healthy subjects, the systemic exposure (Cmax and AUC) in patients with liver impairment increased in the range of 1.4 to 2.7 fold after 1280 mcg ex-actuator ciclesonide by oral inhalation and dose adjustment in liver impairment is not necessary. Studies in renal impaired patients were not conducted.
In a 12-week study in children 6-11 years of age with perennial allergic rhinitis, daily doses of 200 mcg, 100 mcg, and 25 mcg of OMNARIS Nasal Spray were compared to placebo nasal spray. Adrenal function was assessed by measurement of 24-hour urinary free cortisol (in 32 to 44 patients per group) and morning plasma cortisol levels (in 45 to 61 patients per group) before and after 12 consecutive weeks of treatment. The ciclesonide-treated groups had a numerically greater decline in 24-hour urinary free cortisol compared to the placebo treated group. The differences (and 95% confidence intervals) from placebo in the mean change from baseline to 12 weeks were -0.81 (-4.0, 2.4), -0.08 (-3.1, 2.9), and -2.11 (-5.3, 1.1) mcg/day for 200 mcg, 100 mcg, and 25 mcg dose groups, respectively. The mean AM plasma cortisol value did not show any consistent treatment effect with differences (and 95% confidence intervals) from placebo in the mean change from baseline to 12 weeks of 0.35 (-1.4, 2.1), 0.12 (-1.5, 1.7), and -0.38 (-2.1, 1.3) mcg/dL for 200 mcg, 100 mcg, and 25 mcg dose groups respectively. In this study, serum was assayed for ciclesonide and des-ciclesonide (see CLINICAL PHARMACOLOGY: Pharmacokinetics: Absorption).
In a 6-week study in children 2 to 5 years of age with perennial allergic rhinitis, daily doses of 200 mcg, 100 mcg, and 25 mcg of OMNARIS Nasal Spray were compared to placebo nasal spray. Adrenal function was assessed by measurement of 24-hour urinary free cortisol (in 15 to 22 patients per group) and morning plasma cortisol levels (in 28 to 30 patients per group) before and after 6 consecutive weeks of treatment. The ciclesonide-treated groups had a numerically greater decline in 24-hour urinary free cortisol compared to the placebo treated group. The differences (and 95% confidence intervals) from placebo in the mean change from baseline to 6 weeks were -2.04 (-4.4, 0.3), -1.96 (-4.5, 0.6), and -1.76 (-4.3, 0.8) mcg/day for the 200 mcg, 100 mcg, and 25 mcg dose groups, respectively. The plasma cortisol also decreased numerically after treatment with ciclesonide. The differences (and 95% confidence intervals) from placebo in the mean change in plasma cortisol from baseline to 6 weeks were -1.04 (-2.7, 0.7), -0.36 (-2.1, 1.4), and -0.12 (-1.8, 1.6) mcg/dL for the 200 mcg, 100 mcg, and 25 mcg dose groups, respectively. In this study, serum was assayed for ciclesonide and des-ciclesonide (see CLINICAL PHARMACOLOGY: Pharmacokinetics: Absorption).
There are no adequately conducted studies in adults and adolescents that assess the effect of OMNARIS Nasal Spray on adrenal function.
CLINICAL TRIALS
Adult and Adolescent Patients Aged 12 Years and Older:
The efficacy and safety of OMNARIS Nasal Spray were evaluated in 4 randomized, double-blind, parallel-group, multicenter, placebo-controlled clinical trials of 2 weeks to 1 year in duration conducted in the United States and Canada in adolescents and adults with allergic rhinitis. Three of these trials were 2 to 6 weeks in duration and primarily designed to assess efficacy. One of these trials was 1 year in duration and primarily designed to assess safety. The three trials of 2 to 6 weeks duration included a total of 1524 patients (495 males and 1029 females) of whom 79 were adolescents, ages 12 to 17 years. Of the 1524 patients, 546 patients received OMNARIS Nasal Spray 200 mcg once daily administered as 2 sprays in each nostril. Patients enrolled in the studies were 12 to 86 years of age with a history of seasonal or perennial allergic rhinitis, a positive skin test to at least one relevant allergen, and active symptoms of allergic rhinitis at study entry. Assessment of efficacy in these trials was based on patient recording of four nasal symptoms (runny nose, nasal itching, sneezing, and nasal congestion) on a 0-3 categorical severity scale (0=absent, 1=mild, 2=moderate, and 3=severe) as reflective or instantaneous scores. Reflective scoring required the patients to record symptom severity over the previous 12 hours; the instantaneous scoring required patients to record symptom severity at the time of recording. The results of these trials showed that patients treated with OMNARIS Nasal Spray 200 mcg once daily exhibited statistically significantly greater decreases in total nasal symptom scores than placebo treated patients. Secondary measures of efficacy were also generally supportive.
Of the three trials primarily designed to assess efficacy, one was a 2-week dose-ranging trial that evaluated efficacy of four doses of OMNARIS Nasal Spray in patients with seasonal allergic rhinitis. The primary efficacy endpoint was the difference from placebo in the change from baseline of the sum of morning and evening reflective total nasal symptom score averaged over the 2-week treatment period. Results of the primary efficacy endpoint are shown in Table 1. In this trial OMNARIS Nasal Spray 200 mcg once daily was statistically significantly different from placebo, but the lower doses were not statistically significantly different from placebo.
|
Treatment
|
N
|
Baseline*
|
Change from Baseline |
Difference
Estimate |
from Placebo 95% CI |
p-value |
|
Seasonal Allergic Rhinits Trial - Reflective total nasal symptoms score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
144 |
18.8 |
-5.73 |
-1.35 |
(-2.43, -0.28) |
0.014 |
| Ciclesonide 100 mcg |
145 |
18.7 |
-5.26 |
-0.88 |
(-1.96, 0.19) |
0.11 |
| Ciclesonide 50 mcg |
143 |
18.4 |
-4.82 |
-0.44 |
(-1.52, 0.63) |
0.42 |
| Ciclesonide 25 mcg |
146 |
18.7 |
-4.74 |
-0.35 |
(-1.42, 0.71) |
0.51 |
| Placebo |
148 |
17.8 |
-4.38 |
|
|
|
|
Treatment
|
n
|
Baseline*
|
Change from Baseline |
Estimate |
Difference
95% CI |
from Placebo p-value |
|
Seasonal Allergic Rhinitis Trial - Reflective total nasal symptom score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
162 |
8.96 |
-2.40 |
-0.90 |
(-1.36, -0.45) |
less than 0.001 |
| Placebo |
162 |
8.83 |
-1.50 |
|
|
|
|
Seasonal Allergic Rhinitis Trial - Instantaneous total nasal symptom score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
162 |
8.45 |
-1.87 |
-0.84 |
(-1.30, -0.39) |
less than 0.001 |
| Placebo |
162 |
8.33 |
-1.03 |
|
|
|
|
Perennial Allergic Rhinitis Trial - Reflective total nasal symptom score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
232 |
7.59 |
-2.51 |
-0.62 |
(-0.97, -0.28) |
less than 0.001 |
| Placebo |
229 |
7.72 |
-1.89 |
|
|
|
|
Perennial Allergic Rhinitis Trial - Instantaneous total nasal symptom score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
232 |
7.05 |
-1.99 |
-0.53 |
(-0.90, -0.17) |
0.004 |
| Placebo |
229 |
7.05 |
-1.46 |
|
|
|
Onset of action was evaluated in two environmental exposure unit studies with a single dose of OMNARIS Nasal Spray 200 mcg. Results from these two studies did not demonstrate a replicate onset of action within the assessment period. Onset of action was also evaluated in the 4-week seasonal allergic rhinitis and in the 6-week perennial allergic rhinitis trial by frequent recording of instantaneous symptom score after the first dose. In these trials, onset of effect was seen within 24 to 48 hours with further symptomatic improvement observed over 1 to 2 weeks in seasonal allergic rhinitis and 5 weeks in perennial allergic rhinitis.
Pediatric Patients Aged 6 to 11 Years:
The efficacy of OMNARIS Nasal Spray was evaluated in two randomized, double-blind, parallel-group, multicenter, placebo-controlled clinical trials of 2 and 12 weeks in duration in 1282 patients 6 to 11 years of age with allergic rhinitis. Of the two trials, one was 2 weeks in duration conducted in patients with seasonal allergic rhinitis that evaluated efficacy of 200 mcg and 100 mcg of OMNARIS nasal spray once daily. The other trial was 12 weeks in duration conducted in patients with perennial allergic rhinitis that evaluated efficacy of 200 mcg, 100 mcg, and 25 mcg of OMNARIS nasal spray once daily. Of the total number of patients enrolled in the 2 studies, 380 were treated with 200 mcg of OMNARIS nasal spray once daily. The primary efficacy endpoint was the difference from placebo in the change from baseline of the average of morning and evening reflective total nasal symptom score averaged over 2 weeks of treatment in the seasonal allergic rhinitis trial and over the first 6 weeks of treatment in the perennial allergic rhinitis trial. In the 2-week trial in patients with seasonal allergic rhinitis, the OMNARIS Nasal Spray 200 mcg once daily dose was statistically significantly different from placebo, but the 100 mcg once daily dose was not statistically significantly different from placebo. The efficacy results for the seasonal allergic rhinitis trial are shown in Table 3.
|
Treatment
|
n
|
Baseline*
|
Change from Baseline |
Estimate |
Difference
95% CI |
from Placebo p-value |
| Reflective total nasal symptom score |
|
|
|
|
|
|
| Ciclesonide 200 mcg |
215 |
8.25 |
-2.46 |
-0.39 |
(-0.76, -0.02) |
0.040 |
| Ciclesonide 100 mcg |
199 |
8.41 |
-2.38 |
-0.32 |
(-0.69, 0.06) |
0.103 |
| Placebo |
204 |
8.41 |
-2.07 |
|
|
|
In the 12-week trial in patients with perennial allergic rhinitis, none of the ciclesonide doses were statistically significantly different from placebo. The means and 95% confidence intervals for the differences (OMNARIS Nasal Spray minus placebo) between OMNARIS Nasal Spray 200 mcg, 100 mcg, and 25 mcg treatment groups and placebo were -0.31 (-0.75, 0.13), 0.02 (-0.41, 0.46), and 0.09 (-0.35, 0.53), respectively.
Pediatric Patients Aged 2 to 5 Years:
Efficacy of OMNARIS Nasal Spray in patients 2 to 5 years of age has not been established (See PRECAUTIONS: Pediatric Use).
OMNARIS INDICATIONS AND USAGE
OMNARIS Nasal Spray is indicated for the treatment of nasal symptoms associated with seasonal allergic rhinitis in adults and children 6 years of age and older.
OMNARIS Nasal Spray is indicated for the treatment of nasal symptoms associated with perennial allergic rhinitis in adults and adolescents 12 years of age and older.
OMNARIS CONTRAINDICATIONS
OMNARIS Nasal Spray is contraindicated in patients with a hypersensitivity to any of its ingredients.
WARNINGS
The replacement of a systemic corticosteroid with a topical corticosteroid can be accompanied by signs of adrenal insufficiency. In addition, some patients may experience symptoms of corticosteroid withdrawal, e.g., joint and/or muscular pain, lassitude, and depression. Patients previously treated for prolonged periods with systemic corticosteroids and transferred to topical corticosteroids should be carefully monitored for acute adrenal insufficiency in response to stress. In those patients who have asthma or other clinical conditions requiring long-term systemic corticosteroid treatment, rapid decreases in systemic corticosteroid dosages may cause a severe exacerbation of their symptoms.
Patients who are using drugs that suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in children or adults using corticosteroids. In children or adults who have not had these diseases or been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information). If chickenpox develops, treatment with antiviral agents may be considered.
PRECAUTIONS
Intranasal corticosteroids may cause a reduction in growth velocity when administered to pediatric patients (see PRECAUTIONS: Pediatric Use). Rarely, immediate hypersensitivity reactions or contact dermatitis may occur after the administration of intranasal corticosteroids. Patients with a known hypersensitivity reaction to other corticosteroid preparations should use caution when using ciclesonide nasal spray since cross reactivity to other corticosteroids including ciclesonide may also occur.
Because of the inhibitory effect of corticosteroids on wound healing, patients who have experienced recent nasal septal ulcers, nasal surgery, or nasal trauma should not use a nasal corticosteroid until healing has occurred. In clinical studies with OMNARIS Nasal Spray, the development of localized infections of the nose and pharynx with Candida albicans has rarely occurred. When such an infection develops, it may require treatment with appropriate local therapy and discontinuation of OMNARIS Nasal Spray. Therefore, patients using OMNARIS Nasal Spray over several months or longer should be examined periodically for evidence of Candida infection or other signs of adverse effects on the nasal mucosa. Intranasal corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculosis infections of the respiratory tract; or in patients with untreated local or systemic fungal or bacterial infections; systemic viral or parasitic infections; or ocular herpes simplex.
If recommended doses of intranasal corticosteroids are exceeded or if individuals are particularly sensitive or predisposed by virtue of recent systemic steroid therapy, symptoms of hypercorticism may occur, including very rare cases of menstrual irregularities, acneiform lesions, and cushingoid features. If such changes occur, topical corticosteroids should be discontinued slowly, consistent with accepted procedures for discontinuing oral steroid therapy.
The risk of glaucoma was evaluated by assessments of intraocular pressure in 3 studies including 943 patients. Of these, 390 adolescents or adults were treated for up to 52 weeks and 186 children ages 2 to 11 received treatment with OMNARIS Nasal Spray 200 mcg daily for up to 12 weeks. In these trials, no significant differences in intraocular pressure changes were observed between OMNARIS Nasal Spray 200 mcg and placebo-treated patients. Additionally, no significant differences between OMNARIS Nasal Spray 200 mcg and placebo-treated patients were noted during the 52-week study of adults and adolescent patients in whom thorough ophthalmologic assessments were performed including evaluation of cataract formation using slit lamp examinations. Rare instances of wheezing, nasal septum perforation, cataracts, glaucoma, and increased intraocular pressure have been reported following the intranasal application of corticosteroids. Close follow-up is warranted in patients with a change in vision and with a history of glaucoma and/or cataracts.
Patients being treated with OMNARIS Nasal Spray should receive the following information and instructions. This information is intended to aid them in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
Patients who are on immunosuppressive doses of corticosteroids should be warned to avoid exposure to chickenpox or measles, and if exposed, to obtain medical advice. Patients should use OMNARIS Nasal Spray at regular intervals since its effectiveness depends on its regular use (See DOSAGE AND ADMINISTRATION).
In clinical trials, the onset of effect was seen within 24 to 48 hours with further symptomatic improvement observed over 1 to 2 weeks in seasonal allergic rhinitis and 5 weeks in perennial allergic rhinitis. Initial assessment of response should be made during this timeframe and periodically until the patients symptoms are stabilized.
The patient should take the medication as directed and should not exceed the prescribed dosage. The patient should contact the physician if symptoms do not improve by a reasonable time or if the condition worsens. For the proper use of this unit and to attain maximum improvement, the patients should read and follow the accompanying patient instructions carefully. Spraying OMNARIS Nasal Spray directly into the eyes or onto the nasal septum should be avoided. It is important that the bottle is gently shaken prior to use to ensure that a consistent amount is dispensed per actuation. The bottle should be discarded after 120 actuations following initial priming or after 4 months after the bottle is removed from the foil pouch, whichever occurs first.
Based on in vitro studies in human liver microsomes, des-ciclesonide appears to have no inhibitory or induction potential on the metabolism of other drugs metabolized by CYP 450 enzymes. The inhibitory potential of ciclesonide on CYP450 isoenzymes has not been studied. In vitro studies demonstrated that the plasma protein binding of des-ciclesonide was not affected by warfarin or salicylic acid, indicating no potential for protein binding-based drug interactions.
In a drug interaction study, co-administration of orally inhaled ciclesonide and oral erythromycin, an inhibitor of cytochrome P450 3A4, had no effect on the pharmacokinetics of either des-ciclesonide or erythromycin. In another drug interaction study, co-administration of orally inhaled ciclesonide and oral ketoconazole, a potent inhibitor of cytochrome P450 3A4, increased the exposure (AUC) of des-ciclesonide by approximately 3.6-fold at steady state, while levels of ciclesonide remained unchanged. Therefore, ketoconazole should be administered with caution with intranasal ciclesonide.
Ciclesonide demonstrated no carcinogenic potential in a study of oral doses up to 900 mcg/kg (approximately 20 and 10 times the maximum human daily intranasal dose in adults and children, respectively, based on mcg/m2) in mice for 104 weeks and in a study of inhalation doses up to 193 mcg/kg (approximately 8 and 5 times the maximum human daily intranasal dose in adults and children, respectively, based on mcg/m2) in rats for 104 weeks. Ciclesonide was not mutagenic in an Ames test or in a forward mutation assay and was not clastogenic in a human lymphocyte assay or in an in vitro micronucleus test. However, ciclesonide was clastogenic in the in vivo mouse micronucleus test. The concurrent reference corticosteroid (dexamethasone) in this study showed similar findings. No evidence of impairment of fertility was observed in a reproductive study conducted in male and female rats both dosed orally up to 900 mcg/kg/day (approximately 35 times the maximum human daily intranasal dose in adults based on mcg/m2).
Pregnancy Category C
Oral administration of ciclesonide in rats up to 900 mcg/kg (approximately 35 times the maximum human daily intranasal dose in adults based on mcg/m2) produced no teratogenicity or other fetal effects. However, subcutaneous administration of ciclesonide in rabbits at 5 mcg/kg (less than the maximum human daily intranasal dose in adults based on mcg/m2) or greater produced fetal toxicity. This included fetal loss, reduced fetal weight, cleft palate, skeletal abnormalities including incomplete ossifications, and skin effects. No toxicity was observed at 1 mcg/kg (less than the maximum human daily intranasal dose based on mcg/m2).
There are no adequate and well-controlled studies in pregnant women. OMNARIS Nasal Spray, like other corticosteroids, should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Experience with oral corticosteroids since their introduction in pharmacologic, as opposed to physiologic, doses suggests that rodents are more prone to teratogenic effects from corticosteroids than humans. In addition, because there is a natural increase in corticosteroid production during pregnancy, most women will require a lower exogenous corticosteroid dose and many will not need corticosteroid treatment during pregnancy.
Hypoadrenalism may occur in infants born of mothers receiving corticosteroids during pregnancy. Such infants should be carefully monitored.
It is not known if ciclesonide is excreted in human milk. However, other corticosteroids are excreted in human milk. In a study with lactating rats, minimal but detectable levels of ciclesonide were recovered in milk. Caution should be used when OMNARIS Nasal Spray is administered to nursing women.
The safety and effectiveness for seasonal and perennial allergic rhinitis in children 12 years of age and older have been established. The efficacy of OMNARIS Nasal Spray in patients 6 to 11 years of age for treatment of the symptoms of seasonal allergic rhinitis is supported by evidence from four adequate and well-controlled studies in adults and adolescents 12 years of age and older with seasonal and perennial allergic rhinitis, and one study in patients 6 to 11 years of age with seasonal allergic rhinitis. The efficacy of OMNARIS Nasal Spray for the treatment of the symptoms of perennial allergic rhinitis in patient 6 to 11 years of age has not been established (see CLINICAL TRIALS: Pediatric Patients Aged 6 to 11 Years). The efficacy of OMNARIS Nasal Spray in children 2 to 5 years of age has not been established. The safety of OMNARIS Nasal Spray in children 2 to 11 years of age was evaluated in 4 controlled clinical studies of 2 to 12 weeks duration (See CLINICAL PHARMACOLOGY: Pharmacodynamics, CLINICAL TRIALS, ADVERSE REACTIONS: Pediatric Patients).
Clinical studies in children less than two years of age have not been conducted. Studies in children under 2 years of age are waived because of local and systemic safety concerns.
Controlled clinical studies have shown that intranasal corticosteroids may cause a reduction in growth velocity in pediatric patients. This effect has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA)-axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA-axis function. The long-term effects of this reduction in growth velocity associated with intranasal corticosteroids, including the impact on final adult height, are unknown. The potential for "catch-up" growth following discontinuation of treatment with intranasal corticosteroids has not been adequately studied. The growth of pediatric patients receiving intranasal corticosteroids, including OMNARIS Nasal Spray, should be monitored routinely (e.g., via stadiometry). The potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of safe and effective noncorticosteroid treatment alternatives. To minimize the systemic effects of intranasal corticosteroids, each patient should be titrated to the lowest dose that effectively controls his/her symptoms.
Clinical studies of OMNARIS Nasal Spray did not include sufficient numbers of subjects age 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
OMNARIS ADVERSE REACTIONS
Adult and Adolescent Patients Aged 12 Years and Older:
In controlled clinical studies conducted in the US and Canada, a total of 1524 patients ages 12 years and older received treatment with ciclesonide administered intranasally. In studies of 2 to 6 weeks duration in patients 12 years and older, 546 patients were treated with OMNARIS Nasal Spray 200 mcg daily, and in a study of up to one year in duration, 441 patients were treated with OMNARIS Nasal Spray 200 mcg daily. The overall incidence of adverse events for patients treated with OMNARIS Nasal Spray was comparable to that in patients treated with placebo. Adverse events did not differ appreciably based on age, gender, or race. Approximately 2% of patients treated with OMNARIS Nasal Spray 200 mcg in clinical trials discontinued because of adverse events; this rate was similar for patients treated with placebo. Table 4 displays adverse events, irrespective of drug relationship, that occurred with an incidence of 2% or greater and more frequently with OMNARIS Nasal Spray 200 mcg than with placebo in clinical trials of 2 to 6 weeks in duration.
| Adverse Event | OMNARIS Nasal Spray 200 mcg Once Daily (N =546) % |
Placebo (N = 544) % |
|---|---|---|
| Headache | 6.0 | 4.6 |
| Epistaxis | 4.9 | 2.9 |
| Nasopharyngitis | 3.7 | 3.3 |
| Ear Pain | 2.2 | 0.6 |
In a 52-week long-term safety trial that included 663 adults and adolescent patients (441 treated with ciclesonide: 227 males and 436 females) with perennial allergic rhinitis, the adverse event profile over the treatment period was similar to the adverse event profile in trials of shorter duration. Adverse events considered likely or definitely related to OMNARIS Nasal Spray that were reported at an incidence of 1% or greater of patients and more commonly in OMNARIS Nasal Spray versus placebo were epistaxis, nasal discomfort, and headache. No patient experienced a nasal septal perforation or nasal ulcer during long-term use of OMNARIS Nasal Spray. While primarily designed to assess the long-term safety of OMNARIS Nasal Spray 200 mcg once daily, this 52-week trial demonstrated greater decreases in total nasal symptom scores with OMNARIS Nasal Spray versus placebo treated patients over the entire treatment period.
Pediatric Patients Aged 6 to 11 Years:
Two controlled clinical studies 2 and 12 weeks in duration were conducted in the US and Canada and included a total of 1282 patients with allergic rhinitis ages 6 to 11 years, of which 913 were treated with OMNARIS (ciclesonide) Nasal Spray 200 mcg, 100 mcg or 25 mcg daily. The overall incidence of adverse events for patients treated with OMNARIS Nasal Spray was comparable to that in patients treated with placebo. Adverse events did not differ appreciably based on age, gender, or race. In clinical trials, 1.6% and 2.7% of patients treated with OMNARIS Nasal Spray 200 mcg or 100 mcg, respectively, discontinued because of adverse events; these rates were lower than the rate in patients treated with placebo (2.8%). Table 5 displays adverse events, irrespective of drug relationship, that occurred with an incidence of 3% or greater and more frequently with OMNARIS Nasal Spray 200 mcg than with placebo.
| Adverse Event | OMNARIS Nasal Spray 200 mcg Once Daily (N =380) % |
Placebo (N = 369) % |
|---|---|---|
| Headache | 6.6 | 5.7 |
| Nasopharyngitis | 6.6 | 5.4 |
| Pharyngolaryngeal pain | 3.4 | 3.3 |
Pediatric Patients Aged 2 to 5 Years:
Two controlled clinical studies 6 and 12 weeks in duration were conducted in the US and included a total of 258 patients 2 to 5 years of age with perennial allergic rhinitis, of which 183 were treated with OMNARIS Nasal Spray 200 mcg, 100 mcg or 25 mcg daily. The distribution of adverse events was similar to that seen in the 6 to 11 year old children.
OVERDOSAGE
There are no data available on the effects of acute or chronic overdosage with OMNARIS Nasal Spray. Because of low systemic bioavailability, acute overdosage is unlikely to require any therapy other than observation. A single oral dose of up to 10 mg of ciclesonide in healthy volunteers was well tolerated and serum cortisol levels were virtually unchanged in comparison with placebo treatment. Chronic overdosage with any corticosteroid may result in signs or symptoms of hypercorticism (See PRECAUTIONS).
OMNARIS DOSAGE AND ADMINISTRATION
Seasonal Allergic Rhinitis
Adults and Children (6 Years of Age and Older): The recommended dose of OMNARIS Nasal Spray is 200 mcg per day administered as 2 sprays (50 mcg/spray) in each nostril once daily.
Perennial Allergic Rhinitis
Adults and Adolescents (12 Years of Age and Older): The recommended dose of OMNARIS Nasal Spray is 200 mcg per day administered as 2 sprays (50 mcg/spray) in each nostril once daily.
The maximum total daily dosage should not exceed 2 sprays in each nostril (200 mcg/day).
Prior to initial use, OMNARIS Nasal Spray must be gently shaken and then the pump must be primed by actuating eight times. If the product is not used for four consecutive days, it should be gently shaken and reprimed with one spray or until a fine mist appears.
Directions for Use
Illustrated patient's instructions for proper use accompany each package of OMNARIS Nasal Spray.
HOW SUPPLIED
OMNARIS is supplied in an amber glass bottle and provides for nasal delivery with a manual metered pump. OMNARIS Nasal Spray is supplied with an oxygen absorber sachet and enclosed in a foil pouch. OMNARIS Nasal Spray provides 120 metered sprays after initial priming. Each spray delivers 50 mcg of ciclesonide from the nasal actuator. The OMNARIS Nasal Spray bottle has been filled with an excess to accommodate the priming activity. The bottle should be discarded after removal from the foil pouch either after 120 sprays following initial priming (since the amount of ciclesonide delivered per spray thereafter may be substantially less than the labeled dose) or after 4 months. Patient instructions are also provided.
OMNARIS Nasal Spray 50 mcg, 120 metered sprays; net fill weight 12.5 g. (NDC 54868-6020-0)
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [See USP Controlled Room Temp]. Do not freeze. Shake gently before use. Do not spray in eyes. Keep out of reach of children.
Manufactured for:
Sepracor Inc.
Marlborough, MA 01752 USA
Made in Germany
For customer service, call 1-888-394-7377
To report adverse events, call
1-877-737-7226
For medical information, call 1-800-739-0565
November 2007
USA F.1/1207/3.5472.73
Relabeling of "Additional Barcode" by:
Physicians Total Care, Inc.
Tulsa, OK 74146
OMNARIS (ciclesonide) Nasal Spray, 50 mcg
FOR INTRANASAL ADMINISTRATION ONLY
Please read this leaflet carefully before taking OMNARIS Nasal Spray. This leaflet does not contain the complete information about this medication. If you have any questions about OMNARIS Nasal Spray, ask your health care provider or pharmacist.
What you should know about OMNARIS Nasal Spray.
Your healthcare provider has prescribed OMNARIS Nasal Spray. It contains a medicine called ciclesonide, which helps relieve inflammation. This medication is used for the treatment of nasal symptoms associated with seasonal nasal allergy in adults and children 6 years of age and older and year-round nasal allergy in adults and adolescents 12 years of age and older.
The nasal spray delivers your medication as an aqueous spray. Once you begin treatment, use your nasal spray once a day, every day, as prescribed by your health care provider. OMNARIS Nasal Spray may begin to work within 24 hours after the first dose. Further symptom improvements may occur over 1 to 2 weeks for seasonal allergy symptoms and 5 weeks for year-round allergy symptoms. If your symptoms do not improve in that time frame or if your condition worsens, contact your health care provider.
Dosage
For Adults and Children (6 Years of Age and Older) with seasonal allergy symptoms: The recommended dose is 2 sprays in each nostril once daily.
For Adults and Adolescents (12 Years of Age and Older) with year-round allergy symptoms: The recommended dose is 2 sprays in each nostril once daily.
You should not use more than a total of 2 sprays in each nostril daily.
Preparing For Use
- Remove OMNARIS Nasal Spray from its foil pouch. Count 4 months from this date and write this date (that is 4 months from removing the bottle from the foil pouch) on the sticker provided on the carton. Peel off this sticker and place it in the space provided on your nasal spray bottle. It's important to throw away the nasal spray bottle after this date.
- Before the first use, shake the bottle gently and prime the pump by pressing downward on the shoulders of the applicator eight times. Read the complete instructions carefully and use only as directed. If you have not used the nasal spray for 4 days, shake the bottle gently and prime the pump again by spraying one time or until a fine mist appears.
Using the Spray
1. Blow your nose to clear your nostrils if needed.
2. Shake the bottle gently and remove the dust cap.
3. Hold the bottle firmly with your index and middle finger on either side of the spray tip while supporting the base of the bottle with your thumb (Figure 1).

Figure 1.
4. Insert spray tip into one nostril, and close the other nostril with your finger (Figure 2).
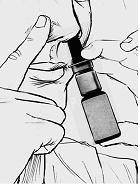
Figure 2.
5. Tilt your head forward slightly and keeping the bottle upright, press the pump quickly and firmly and inhale through your nose as you spray (Figure 3). Avoid spraying in eyes or directly onto the nasal septum (the wall between the two nostrils).

Figure 3.
6. Repeat steps 3-5 for the second spray in the same nostril and for each spray in the other nostril.
Storage Instructions
Keep your nasal spray clean and dry at all times. Store medication between 59° and 86° F. Do not freeze. Keep out of the reach of young children.
How To Know When Your Nasal Spray Bottle Is Empty
The amount of nasal spray left can be seen through a window on the bottle. Do not use this bottle for more than the labeled number of sprays or after the "discard by date" you wrote on the sticker when you opened the foil pouch. You may want to obtain a refill before your supply runs out if recommended by your health care provider.
Applicator Cleaning Instructions
After daily use of your nasal spray, wipe the applicator tip with a clean tissue and replace the dust cap.
If the nasal applicator is clogged or requires more thorough cleaning, use the following cleaning instructions (Do not try to unblock the tiny spray hole on the nasal applicator with a pin or other sharp object):
- Remove the dust cap and then gently pull upwards to free the nasal applicator.
- Wash the dust cap and applicator with warm water.
- Dry and replace the nasal applicator.
- Prime the unit with one spray or until a fine mist appears.
- Replace the dust cap.
Further Information
Avoid spraying in eyes or directly onto the nasal septum (the wall between the two nostrils).
This leaflet does not contain the complete information about your medicine. If you have any questions or are not sure about something, then you should ask your doctor or pharmacist.
You may want to read this leaflet again. Please DO NOT THROW IT AWAY until you have finished your medicine.
Manufactured for:
Sepracor Inc.
Marlborough, MA 01752 USA
Made in Germany
For customer service, call 1-888-394-7377
To report adverse events, call
1-877-737-7226
For medical information, call 1-800-739-0565
November 2007
USA F.1/1207/3.5472.82
PRINCIPAL DISPLAY PANEL
OMNARIS (ciclesonide) Nasal Spray, 50 mcg
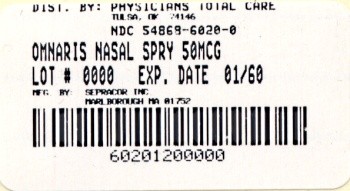
Omnarisciclesonide SPRAY
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||