Metronidazole
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Metronidazole safely and effectively. See full prescribing information for Metronidazole. Metronidazole (Metronidazole) GEL for TOPICAL use.Initial U.S. Approval: 1963INDICATIONS AND USAGE Metronidazole gel USP, 1% is a nitroimidazole indicated for the topical treatment of inflammatory lesions of rosacea (1).DOSAGE AND ADMINISTRATION ● Not for oral, ophthalmic or intravaginal use. ● Apply and rub in a thin film of metronidazole gel USP, 1% once daily to affected area(s). ● Treated areas should be cleansed before the application of metronidazole gel USP, 1%. ● Cosmetics may be applied after the application of metronidazole gel USP, 1%.DOSAGE FORMS AND STRENGTHS Gel, 1%.CONTRAINDICATIONS Metronidazole gel USP, 1% is contraindicated in those patients with a history of hypersensitivity to metronidazole or to any other ingredient in this formulation.WARNINGS AND PRECAUTIONS ● Peripheral neuropathy, characterized by numbness or paresthesia of an extremity has been reported in patients treated with systemic metronidazole. Although not evident in clinical trials for topical metronidazole, peripheral neuropathy has been reported with the post approval use. The appearance of abnormal neurologic signs should prompt immediate reevaluation of metronidazole gel USP, 1% therapy. (5.1) ● Metronidazole is a nitroimidazole and should be used with care in patients with evidence of, or history of, blood dyscrasia. (5.2) ● If dermatitis occurs, patients may need to discontinue use. (5.3) ● Topical metronidazole has been reported to cause tearing of the eyes. Therefore, contact with the eyes should be avoided. (5.4)Side Effects Most common adverse reactions (incidence > 2%) are nasopharyngitis, upper respiratory tract infection, and headache. To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Oral metronidazole has been reported to potentiate the anticoagulant effect of coumarin and warfarin, resulting in a prolongation of prothrombin time. Drug interactions should be kept in mind when metronidazole gel USP, 1% is prescribed for patients who are receiving anticoagulant treatment, although they are less likely to occur with topical metronidazole administration because of low absorption.
FULL PRESCRIBING INFORMATION
Metronidazole gel USP, 1% is indicated for the topical treatment of inflammatory lesions of rosacea.
Apply and rub in a thin film of metronidazole gel USP, 1% once daily to affected area(s).
A gentle cleanser should be used before the application of metronidazole gel USP, 1%.
Cosmetics may be applied after the application of metronidazole gel USP, 1%.
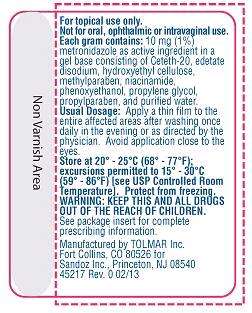
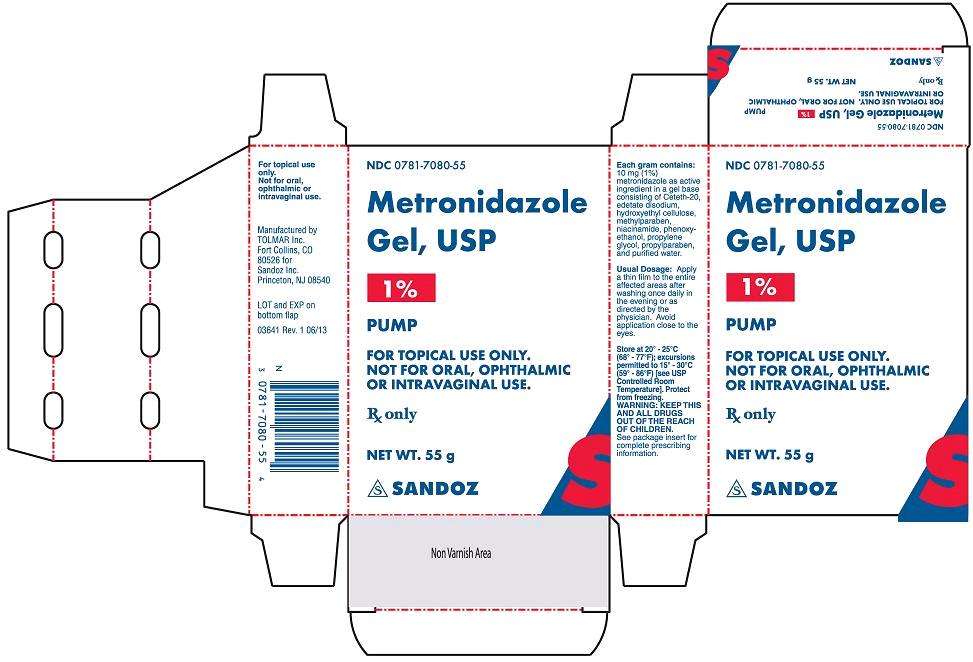
Not for oral, ophthalmic or intravaginal use.
Gel, 1%. Metronidazole gel USP, 1% is a clear, colorless to pale yellow gel. Each gram of metronidazole gel USP, 1% contains 10 mg (1%) of metronidazole.
Metronidazole gel USP, 1% is contraindicated in patients with a history of hypersensitivity to metronidazole or to any other ingredient in the formulation.
Peripheral neuropathy, characterized by numbness or paresthesia of an extremity has been reported in patients treated with systemic metronidazole. Although not evident in clinical trials for topical metronidazole, peripheral neuropathy has been reported with the post approval use. The appearance of abnormal neurologic signs should prompt immediate reevaluation of metronidazole gel USP, 1% therapy. Metronidazole should be administered with caution to patients with central nervous system diseases.
Metronidazole is a nitroimidazole; use with care in patients with evidence of, or history of, blood dyscrasia.
Irritant and allergic contact dermatitis have been reported. If dermatitis occurs, patients may need to discontinue use.
Topical metronidazole has been reported to cause tearing of the eyes. Avoid contact with the eyes.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a controlled clinical trial, 557 patients used metronidazole gel USP, 1% and 189 patients used the gel vehicle once daily for up to 10 weeks. The following table summarizes selected adverse reactions that occurred at a rate of ≥1%:
Table 1: Adverse Reactions That Occurred at a Rate of ≥1 %
| System Organ Class/Preferred Term | Metronidazole Gel USP, 1% | Gel Vehicle |
| N= 557 | N= 189 | |
| Patients with at least one AE Number (%) of Patients | 186 (33.4) | 51 (27.0) |
| Infections and infestations | 76 (13.6) | 28 (14.8) |
| Bronchitis | 6 (1.1) | 3 (1.6) |
| Influenza | 8 (1.4) | 1 (0.5) |
| Nasopharyngitis | 17 (3.1) | 8 (4.2) |
| Sinusitis | 8 (1.4) | 3 (1.6) |
| Upper respiratory tract infection | 14 (2.5) | 4 (2.1) |
| Urinary tract infection | 6 (1.1) | 1 (0.5) |
| Vaginal mycosis | 1 (0.2) | 2 (1.1) |
| Musculoskeletal and connective tissue disorders | 19 (3.4) | 5 (2.6) |
| Back pain | 3 (0.5) | 2 (1.1) |
| Neoplasms | 4 (0.7) | 2 (1.1) |
| Basal cell carcinoma | 1 (0.2) | 2 (1.1) |
| Nervous system disorders | 18 (3.2) | 3 (1.6) |
| Headache | 12 (2.2) | 1 (0.5) |
| Respiratory, thoracic and mediastinal disorders | 22 (3.9) | 5 (2.6) |
| Nasal congestion | 6 (1.1) | 3 (1.6) |
| Skin and subcutaneous tissue disorders | 36 (6.5) | 12 (6.3) |
| Contact dermatitis | 7 (1.3) | 1 (0.5) |
| Dry skin | 6 (1.1) | 3 (1.6) |
| Vascular disorders | 8 (1.4) | 1 (0.5) |
| Hypertension | 6 (1.1) | 1 (0.5) |
Table 2: Local Cutaneous Signs and Symptoms of Irritation That Were Worse Than Baseline
| Metronidazole Gel USP, 1% | Gel Vehicle | |
| Sign/Symptom | N= 544 | N= 184 |
| Dryness | 138 (25.4) | 63 (34.2) |
| Mild | 93 (17.1) | 41 (22.3) |
| Moderate | 42 (7.7) | 20 (10.9) |
| Severe | 3 (0.6) | 2 (1.1) |
| Scaling | 134 (24.6) | 60 (32.6) |
| Mild | 88 (16.2) | 32 (17.4) |
| Moderate | 43 (7.9) | 27 (14.7) |
| Severe | 3 (0.6) | 1 (0.5) |
| Pruritus | 86 (15.8) | 35 (19.0) |
| Mild | 53 (9.7) | 21 (11.4) |
| Moderate | 27 (5.0) | 13 (7.1) |
| Severe | 6 (1.1) | 1 (0.5) |
| Stinging/burning | 56 (10.3) | 28 (15.2) |
| Mild | 39 (7.2) | 18 (9.8) |
| Moderate | 7 (1.3) | 9 (4.9) |
| Severe | 10 (1.8) | 1 (0.5) |
The following additional adverse experiences have been reported with the topical use of metronidazole: skin irritation, transient redness, metallic taste, tingling or numbness of extremities, and nausea.
The following adverse reaction has been identified during post approval use of topical metronidazole: peripheral neuropathy. Because this reaction is reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure.
Oral metronidazole has been reported to potentiate the anticoagulant effect of coumarin and warfarin, resulting in a prolongation of prothrombin time. Drug interactions should be kept in mind when metronidazole gel USP, 1% is prescribed for patients who are receiving anticoagulant treatment, although they are less likely to occur with topical metronidazole administration because of low absorption.
Teratogenic Effects: Pregnancy Category B. There are no adequate and well-controlled studies with the use of metronidazole gel USP, 1% in pregnant women. Metronidazole crosses the placental barrier and enters the fetal circulation rapidly. No fetotoxicity was observed after oral administration of metronidazole in rats or mice at 200 and 20 times, respectively, the expected clinical dose. However, oral metronidazole has shown carcinogenic activity in rodents. Because animal reproduction studies are not always predictive of human response, metronidazole gel USP, 1% should be used during pregnancy only if clearly needed.
After oral administration, metronidazole is secreted in breast milk in concentrations similar to those found in the plasma. Even though blood levels taken after topical metronidazole application are significantly lower than those achieved after oral metronidazole a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother and the risk to the infant.
Safety and effectiveness in pediatric patients have not been established.
Sixty-six subjects aged 65 years and older were treated with metronidazole gel USP, 1% in the clinical study. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
There are no reported human experiences with overdosage of metronidazole gel USP, 1%. Topically applied metronidazole can be absorbed in sufficient amount to produce systemic effects.
Metronidazole gel USP, 1% contains metronidazole, USP. Chemically, metronidazole is 2-methyl-5-nitro-1 H-imidazole-1-ethanol. The molecular formula for metronidazole is C6H9N3O3. It has the following structural formula:
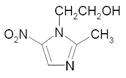
Metronidazole has a molecular weight of 171.16. It is a white to pale yellow crystalline powder. It is slightly soluble in alcohol and has solubility in water of 10 mg/mL at 20°C. Metronidazole belongs to the nitroimidazole class of compounds.
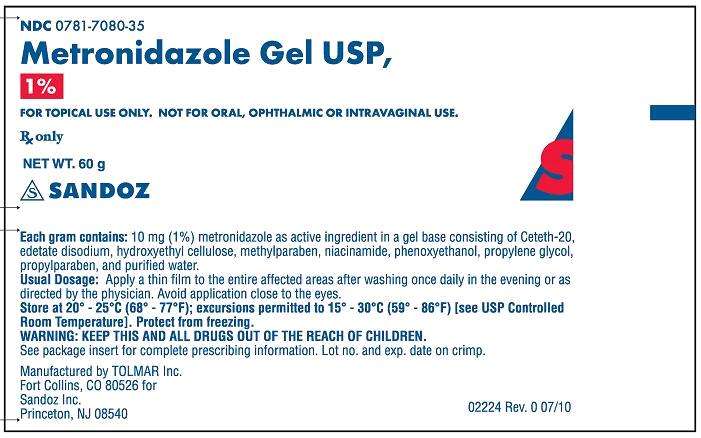
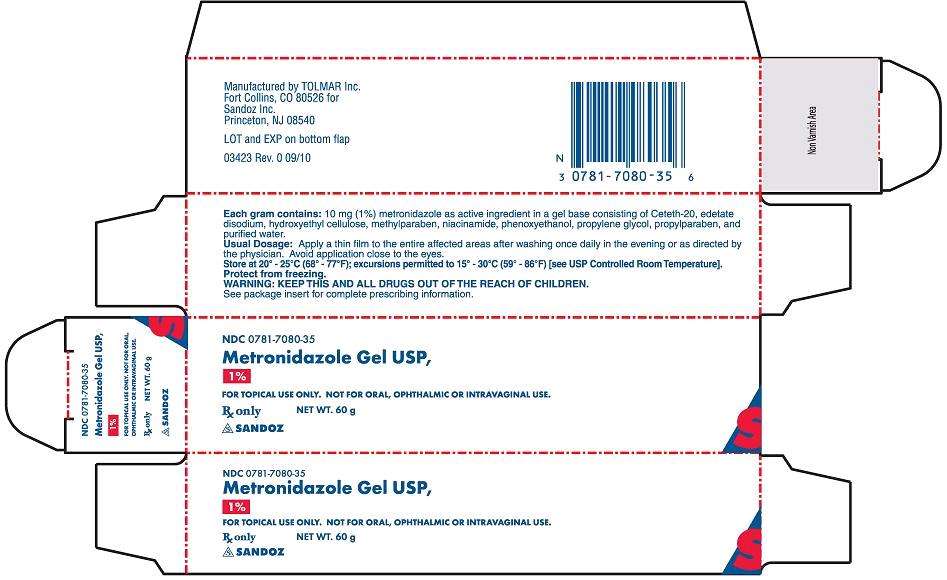
Metronidazole gel USP, 1% is a clear, colorless to pale yellow, aqueous gel; each gram contains 10 mg of metronidazole in a base of ceteth-20, edetate disodium, hydroxyethyl cellulose, methylparaben, niacinamide, phenoxyethanol, propylene glycol, propylparaben and purified water.
The mechanism of action of metronidazole in the treatment of rosacea is unknown.
The pharmacodynamics of metronidazole in association with the treatment of rosacea are unknown.
Topical administration of a one gram dose of metronidazole gel USP, 1% to the face of 13 patients with moderate to severe rosacea once daily for 7 days resulted in a mean ± SD Cmax of metronidazole of 32 ± 9 ng/mL. The mean ± SD AUC(0-24) was 595 ± 154 ng*hr/mL. The mean Cmax and AUC(0-24) are less than 1% of the value reported for a single 250 mg oral dose of metronidazole. The time to maximum plasma concentration (Tmax) was 6-10 hours after topical application.
Metronidazole has shown evidence of carcinogenic activity in a number of studies involving chronic, oral administration in mice and rats, but not in studies involving hamsters.
In several long-term studies in mice, oral doses of approximately 225 mg/m2/day or greater (approximately 37 times the human topical dose on a mg/m2 basis) were associated with an increase in pulmonary tumors and lymphomas. Several long-term oral studies in the rat have shown statistically significant increases in mammary and hepatic tumors at doses >885 mg/m2/day (144 times the human dose).
Metronidazole has shown evidence of mutagenic activity in several in vitro bacterial assay systems. In addition, a dose-related increase in the frequency of micronuclei was observed in mice after intraperitoneal injections. An increase in chromosomal aberrations in peripheral blood lymphocytes was reported in patients with Crohn's disease who were treated with 200 to 1200 mg/day of metronidazole for 1 to 24 months. However, in another study, no increase in chromosomal aberrations in circulating lymphocytes was observed in patients with Crohn’s disease treated with the drug for 8 months.
In one published study, using albino hairless mice, intraperitoneal administration of metronidazole at a dose of 45 mg/m2/day (approximately 7 times the human topical dose on a mg/m2 basis) was associated with an increase in ultraviolet radiation-induced skin carcinogenesis. Neither dermal carcinogenicity nor photocarcinogenicity studies have been performed with metronidazole gel USP, 1% or any marketed metronidazole formulations.
In a randomized, vehicle-controlled trial, 746 subjects with rosacea were treated with metronidazole gel USP, 1% or gel vehicle once daily for 10 weeks. Most subjects had “moderate” rosacea at baseline. Efficacy was determined by recording reduction in inflammatory lesion counts and success rate in the Investigator Global Assessment (percentage of subjects “clear” and “almost clear” of rosacea at the end of the study). The scale is based on the following definitions:
Table 3: Investigator Global Assessment Scale
| Score | Grade | Definition |
| 0 | Clear | No signs or symptoms present; at most, mild erythema |
| 1 | Almost Clear | Very mild erythema present. Very few small papules/pustules |
| 2 | Mild | Mild erythema. Several small papules/pustules |
| 3 | Moderate | Moderate erythema. Several small or large papules/pustules, and up to 2 nodules |
| 4 | Severe | Severe erythema. Numerous small and/or large papules/pustules, up to several nodules |
The results are shown in the following table:
Table 4: Inflammatory Lesion Counts and Global Scores in a Clinical Trial of Rosacea
| Metronidazole Gel USP, 1% |
Vehicle | |||
| N | Results N (%) | N | Results N (%) | |
| Inflammatory lesions | 557 | 189 | ||
| Baseline, mean count | 18.3 | 18.4 | ||
| Week-10, mean count | 8.9 | 12.8 | ||
| Reduction | 9.4 (50.7) | 5.6 (32.6) | ||
| Investigator Global Assessment | 557 | 189 | ||
| Subject clear or almost clear | 214 (38.42) | 52 (27.51) | ||
| Subject with no change | 159 (28.5) | 77 (40.7) | ||
Subjects treated with metronidazole gel USP, 1% experienced a mean reduction of 9.4 inflammatory lesions in the Week-10 LOCF group, compared to a reduction of 5.6 for those treated with vehicle, or a difference in means of 3.8 lesions.
The contribution to efficacy of individual components of the vehicle has not been established.
Metronidazole Gel USP, 1% is clear, colorless to pale yellow in color, and supplied as follows:
60 gram tube – NDC 0781-7080-35
55 gram pump – NDC 0781-7080-55
Storage Conditions: Store at 20° - 25°C (68° - 77°F); excursions permitted to 15° - 30°C (59° - 86°F) [see USP Controlled Room Temperature]. Protect from freezing.
Patients using metronidazole gel USP, 1% should receive the following information and instructions:
- This medication is to be used as directed.
- It is for external use only.
- Avoid contact with the eyes.
- Cleanse affected area(s) before applying metronidazole gel USP, 1%.
- This medication should not be used for any condition other than that for which it is prescribed.
- Keep out of reach of children.
- Patients should report any adverse reaction to their physicians.
Rx only
Manufactured by
TOLMAR Inc.
Fort Collins, CO 80526 for
Sandoz Inc.
Princeton, NJ 08540
44445 Rev. 1 02/13
MetronidazoleMetronidazole GEL
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||