LANOXIN
These highlights do not include all the information needed to use LANOXIN safely and effectively. See full prescribing information for LANOXIN. LANOXIN® (digoxin) tablets, for oral useInitial U.S. Approval: 1954
FULL PRESCRIBING INFORMATION: CONTENTS*
- INDICATIONS & USAGE
- DOSAGE & ADMINISTRATION
- DOSAGE FORMS & STRENGTHS
- LANOXIN CONTRAINDICATIONS
- WARNINGS AND PRECAUTIONS
- LANOXIN ADVERSE REACTIONS
- DRUG INTERACTIONS
- USE IN SPECIFIC POPULATIONS
- OVERDOSAGE
- LANOXIN DESCRIPTION
- CLINICAL PHARMACOLOGY
- NONCLINICAL TOXICOLOGY
- CLINICAL STUDIES
- HOW SUPPLIED
- INFORMATION FOR PATIENTS
- SPL UNCLASSIFIED
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
FULL PRESCRIBING INFORMATION
INDICATIONS & USAGE
LANOXIN is indicated for the treatment of mild to moderate heart failure in adults. LANOXIN increases left ventricular ejection fraction and improves heart failure symptoms as evidenced by improved exercise capacity and decreased heart failure-related hospitalizations and emergency care, while having no effect on mortality. Where possible, LANOXIN should be used in combination with a diuretic and an angiotensin-converting enzyme (ACE) inhibitor.
Digoxin increases myocardial contractility in pediatric patients with heart failure.
LANOXIN is indicated for the control of ventricular response rate in adult patients with chronic atrial fibrillation.
DOSAGE & ADMINISTRATION
In selecting a LANOXIN dosing regimen, it is important to consider factors that affect digoxin blood levels (e.g., body weight, age, renal function, concomitant drugs) since toxic levels of digoxin are only slightly higher than therapeutic levels. Dosing can be either initiated with a loading dose followed by maintenance dosing if rapid titration is desired or initiated with maintenance dosing without a loading dose.
Consider interruption or reduction in digoxin dose prior to electrical cardioversion [see Warnings and Precautions (5.6)].
Use digoxin solution to obtain the appropriate dose in infants, young pediatric patients, or patients with very low body weight.
For adults and pediatric patients if a loading dosage is to be given, administer half the total loading dose initially, then ¼ the loading dose every 4 to 8 hours twice, with careful assessment of clinical response and toxicity before each dose. The recommended loading dose is displayed in Table 1.
| Age | Oral Loading Dose, mcg/kg |
| 5 to 10 years | 20 - 45 |
| Adults and pediatric patients over 10 years | 10 - 15 |
| mcg = micrograms |
The maintenance dose is based on the lean body weight, renal function, age, and concomitant products [see Drug Interactions (7.1, 7.2, 7.3)].
The recommended starting maintenance dosage in adults and pediatric patients over 10 years old is displayed in Table 2. Doses may be increased every 2 weeks according to clinical response, serum drug levels, and toxicity.
| Age |
Oral Maintenance Dose, mcg/kg/day (given once daily) |
| Adults and pediatric patients over 10 years | 3.4 – 5.1 |
| mcg = micrograms |
Table 3 displays the recommended (once daily) maintenance dose of LANOXIN in pediatric patients over 10 years old and adult patients according to lean body weight and renal function. The doses are based on studies in adult patients with heart failure. Alternatively, the maintenance dose may be estimated by the following formula (peak body stores lost each day through elimination):
Total Maintenance Dose = Loading Dose (i.e., Peak Body Stores) x % Daily Loss/100
(% Daily Loss = 14 + Creatinine clearance/5)
Reduce the dose of LANOXIN in patients whose lean weight is an abnormally small fraction of their total body mass because of obesity or edema.
|
Corrected Creatinine Clearanceb |
Number of Days Before Steady State Achievedc |
||||||||
| Lean Body Weightd | |||||||||
| kg | 40 | 50 | 60 | 70 | 80 | 90 | 100 | ||
| lb | 88 | 110 | 132 | 154 | 176 | 198 | 220 | ||
| 10 mL/min | 62.5* | 125 | 125 | 187.5 | 187.5 | 187.5 | 250 | 19 | |
| 20 mL/min | 125 | 125 | 125 | 187.5 | 187.5 | 250 | 250 | 16 | |
| 30 mL/min | 125 | 125 | 187.5 | 187.5 | 250 | 250 | 312.5 | 14 | |
| 40 mL/min | 125 | 187.5 | 187.5 | 250 | 250 | 312.5 | 312.5 | 13 | |
| 50 mL/min | 125 | 187.5 | 187.5 | 250 | 250 | 312.5 | 312.5 | 12 | |
| 60 mL/min | 125 | 187.5 | 250 | 250 | 312.5 | 312.5 | 375 | 11 | |
| 70 mL/min | 187.5 | 187.5 | 250 | 250 | 312.5 | 375 | 375 | 10 | |
| 80 mL/min | 187.5 | 187.5 | 250 | 312.5 | 312.5 | 375 | 437.5 | 9 | |
| 90 mL/min | 187.5 | 250 | 250 | 312.5 | 375 | 437.5 | 437.5 | 8 | |
| 100 mL/min | 187.5 | 250 | 312.5 | 312.5 | 375 | 437.5 | 500 | 7 | |
|
a Doses are rounded to the nearest dose possible using whole and/or half LANOXIN tablets. Recommended doses approximately 30 percent lower than the calculated dose are designated with an *. Monitor digoxin levels in patients receiving these initial doses and increase dose if needed. b For adults, creatinine clearance was corrected to 70-kg body weight or 1.73 m2 body surface area. If only serum creatinine concentrations (Scr) are available, a corrected Ccr may be estimated in men as (140 – Age)/Scr. For women, this result should be multiplied by 0.85. For pediatric patients, the modified Schwartz equation may be used. The formula is based on height in cm and Scr in mg/dL where k is a constant. Ccr is corrected to 1.73 m2 body surface area. During the first year of life, the value of k is 0.33 for pre-term babies and 0.45 for term infants. The k is 0.55 for pediatric patients and adolescent girls and 0.7 for adolescent boys. GFR (mL/min/1.73 m2) = (k x Height)/Scr c If no loading dose administered. d The doses listed assume average body composition. |
The starting maintenance dose for heart failure in pediatric patients less than 10 years old is based on the lean body weight, renal function, age, and concomitant products [see Drug Interactions (7.1, 7.2, 7.3)]. The recommended starting maintenance dose for pediatric patients between 5 and 10 years old with normal renal function is displayed in Table 4.
| Age |
Daily Oral Maintenance Dose, mcg/kg/day |
Dose Regimen, mcg/kg/dose |
| 5 to 10 years | 6.4 – 12.9 | 3.2 – 6.4 Twice daily |
The recommended maintenance dose (to be given twice daily) is presented in Table 5.
|
Corrected Creatinine Clearancec |
Number of Days Before Steady State Achievedd |
||||||
| Lean Body Weight | |||||||
| kg | 20 | 30 | 40 | 50 | 60 | ||
| lb | 44 | 66 | 88 | 110 | 132 | ||
| 10 mL/min | - | 62.5 | 62.5* | 125 | 125 | 19 | |
| 20 mL/min | 62.5 | 62.5 | 125 | 125 | 125 | 16 | |
| 30 mL/min | 62.5 | 62.5* | 125 | 125 | 187.5 | 14 | |
| 40 mL/min | 62.5 | 62.5* | 125 | 187.5 | 187.5 | 13 | |
| 50 mL/min | 62.5 | 125 | 125 | 187.5 | 187.5 | 12 | |
| 60 mL/min | 62.5 | 125 | 125 | 187.5 | 250 | 11 | |
| 70 mL/min | 62.5 | 125 | 187.5 | 187.5 | 250 | 10 | |
| 80 mL/min | 62.5* | 125 | 187.5 | 187.5 | 250 | 9 | |
| 90 mL/min | 62.5* | 125 | 187.5 | 250 | 250 | 8 | |
| 100 mL/min | 62.5* | 125 | 187.5 | 250 | 312.5 | 7 | |
|
a Recommended are doses to be given twice daily. b The doses are rounded to the nearest dose possible using whole and/or half LANOXIN tablets. Recommended doses approximately 30 percent lower than the calculated dose are designated with an *. Monitor digoxin levels in patients receiving these initial doses and increase dose if needed. c The modified Schwartz equation may be used to estimate creatinine clearance. See footnote b under Table 2. d If no loading dose administered. |
Monitor for signs and symptoms of digoxin toxicity and clinical response. Adjust dose based on toxicity, efficacy, and blood levels.
Serum digoxin levels < 0.5 ng/mL have been associated with diminished efficacy, while levels above 2 ng/mL have been associated with increased toxicity without increased benefit.
Interpret the serum digoxin concentration in the overall clinical context, and do not use an isolated measurement of serum digoxin concentration as the basis for increasing or decreasing the LANOXIN dose. Serum digoxin concentrations may be falsely elevated by endogenous digoxin-like substances [see Drug Interactions (7.4)]. If the assay is sensitive to these substances, consider obtaining a baseline digoxin level before starting LANOXIN and correct post-treatment values by the reported baseline level.
Obtain serum digoxin concentrations just before the next scheduled LANOXIN dose or at least 6 hours after the last dose. The digoxin concentration is likely to be 10% to 25% lower when sampled right before the next dose (24 hours after dosing) compared to sampling 8 hours after dosing (using once-daily dosing). However, there will be only minor differences in digoxin concentrations using twice daily dosing whether sampling is done at 8 or 12 hours after a dose.
When switching from intravenous to oral digoxin formulations, make allowances for differences in bioavailability when calculating maintenance dosages (see Table 6).
| Absolute Bioavailability |
Equivalent Doses (in micrograms) | ||||
| LANOXIN Tablets | 60 - 80% | 62.5 | 125 | 250 | 500 |
| LANOXIN Intravenous Injection | 100% | 50 | 100 | 200 | 400 |
DOSAGE FORMS & STRENGTHS
Tablets: 125 micrograms are yellow, round, scored tablets with “Y3B” imprinted on one side.
Tablets: 250 micrograms are white, round, scored tablets with “X3A” imprinted on one side.
LANOXIN CONTRAINDICATIONS
LANOXIN is contraindicated in patients with:
- Ventricular fibrillation [see Warnings and Precautions (5.1)]
- Known hypersensitivity reaction to digitalis (reactions seen include unexplained rash, swelling of the mouth, lips or throat or a difficulty in breathing)
WARNINGS AND PRECAUTIONS
Patients with Wolff-Parkinson-White syndrome who develop atrial fibrillation are at high risk of ventricular fibrillation. Treatment of these patients with digoxin leads to greater slowing of conduction in the atrioventricular node than in accessory pathways, and the risks of rapid ventricular response leading to ventricular fibrillation are thereby increased.
LANOXIN may cause severe sinus bradycardia or sinoatrial block particularly in patients with pre-existing sinus node disease and may cause advanced or complete heart block in patients with pre-existing incomplete AV block. Consider insertion of a pacemaker before treatment with digoxin.
Signs and symptoms of digoxin toxicity include anorexia, nausea, vomiting, visual changes and cardiac arrhythmias [first-degree, second-degree (Wenckebach), or third-degree heart block (including asystole); atrial tachycardia with block; AV dissociation; accelerated junctional (nodal) rhythm; unifocal or multiform ventricular premature contractions (especially bigeminy or trigeminy); ventricular tachycardia; and ventricular fibrillation]. Toxicity is usually associated with digoxin levels >2ng/ml although symptoms may also occur at lower levels. Low body weight, advanced age or impaired renal function, hypokalemia, hypercalcemia, or hypomagnesemia may predispose to digoxin toxicity. Obtain serum digoxin levels in patients with signs or symptoms of digoxin therapy and interrupt or adjust dose if necessary [see Adverse Reactions (6) and Overdosage (10)]. Assess serum electrolytes and renal function periodically.
The earliest and most frequent manifestation of digoxin toxicity in infants and children is the appearance of cardiac arrhythmias, including sinus bradycardia. In children, the use of digoxin may produce any arrhythmia. The most common are conduction disturbances or supraventricular tachyarrhythmias, such as atrial tachycardia (with or without block) and junctional (nodal) tachycardia. Ventricular arrhythmias are less common. Sinus bradycardia may be a sign of impending digoxin intoxication, especially in infants, even in the absence of first-degree heart block. Any arrhythmias or alteration in cardiac conduction that develops in a child taking digoxin should initially be assumed to be a consequence of digoxin intoxication.
Given that adult patients with heart failure have some symptoms in common with digoxin toxicity, it may be difficult to distinguish digoxin toxicity from heart failure. Misidentification of their etiology might lead the clinician to continue or increase LANOXIN dosing, when dosing should actually be suspended. When the etiology of these signs and symptoms is not clear, measure serum digoxin levels.
Patients with heart failure associated with preserved left ventricular ejection fraction may experience decreased cardiac output with use of Lanoxin. . Such disorders include restrictive cardiomyopathy, constrictive pericarditis, amyloid heart disease, and acute cor pulmonale. Patients with idiopathic hypertrophic subaortic stenosis may have worsening of the outflow obstruction due to the inotropic effects of digoxin. Patients with amyloid heart disease may be more susceptible to digoxin toxicity at therapeutic levels because of an increased binding of digoxin to extracellular amyloid fibrils.
LANOXIN should generally be avoided in these patients, although it has been used for ventricular rate control in the subgroup of patients with atrial fibrillation.
Hypocalcemia can nullify the effects of digoxin in humans; thus, digoxin may be ineffective until serum calcium is restored to normal. These interactions are related to the fact that digoxin affects contractility and excitability of the heart in a manner similar to that of calcium.
It may be desirable to reduce the dose of or discontinue digoxin for 1 to 2 days prior to electrical cardioversion of atrial fibrillation to avoid the induction of ventricular arrhythmias, but physicians must consider the consequences of increasing the ventricular response if digoxin is decreased or withdrawn. If digitalis toxicity is suspected, elective cardioversion should be delayed. If it is not prudent to delay cardioversion, the lowest possible energy level should be selected to avoid provoking ventricular arrhythmias.
Hypothyroidism may reduce the requirements for digoxin.
Heart failure and/or atrial arrhythmias resulting from hypermetabolic or hyperdynamic states (e.g., hyperthyroidism, hypoxia, or arteriovenous shunt) are best treated by addressing the underlying condition. Atrial arrhythmias associated with hypermetabolic states are particularly resistant to digoxin treatment. Patients with beri beri heart disease may fail to respond adequately to digoxin if the underlying thiamine deficiency is not treated concomitantly.
Digoxin is not recommended in patients with acute myocardial infarction because undesirable increases in myocardial oxygen demand and ischemia may result.
Digoxin can precipitate vasoconstriction and may promote production of pro-inflammatory cytokines, therefore should be avoided in patients with myocarditis.
LANOXIN ADVERSE REACTIONS
The following adverse reactions are included in more detail in the Warnings and Precautions section of the label:
- Cardiac arrhythmias [see Warnings and Precautions (5.1, 5.2)]
- Digoxin Toxicity [see Warnings and Precautions (5.3)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In general, the adverse reactions of LANOXIN are dose-dependent and occur at doses higher than those needed to achieve a therapeutic effect. Hence, adverse reactions are less common when LANOXIN is used within the recommended dose range, is maintained within the therapeutic serum concentration range, and when there is careful attention to concurrent medications and conditions.
In the DIG trial (a trial investigating the effect of digoxin on mortality and morbidity in patients with heart failure), the incidence of hospitalization for suspected digoxin toxicity was 2% in patients taking LANOXIN compared to 0.9% in patients taking placebo [see Clinical Studies (14.1)].
The overall incidence of adverse reactions with digoxin has been reported as 5 to 20%, with 15 to 20% of adverse events considered serious. Cardiac toxicity accounts for about one-half, gastrointestinal disturbances for about one-fourth, and CNS and other toxicity for about one-fourth of these adverse events.
Gastrointestinal: In addition to nausea and vomiting, the use of digoxin has been associated with abdominal pain, intestinal ischemia, and hemorrhagic necrosis of the intestines.
CNS: Digoxin can cause headache, weakness, dizziness, apathy, confusion, and mental disturbances (such as anxiety, depression, delirium, and hallucination).
Other: Gynecomastia has been occasionally observed following the prolonged use of digoxin. Thrombocytopenia and maculopapular rash and other skin reactions have been rarely observed.
DRUG INTERACTIONS
Digoxin has a narrow therapeutic index, increased monitoring of serum digoxin concentrations and for potential signs and symptoms of clinical toxicity is necessary when initiating, adjusting, or discontinuing drugs that may interact with digoxin. Prescribers should consult the prescribing information of any drug which is co-prescribed with digoxin for potential drug interaction information.
Digoxin is a substrate of P-glycoprotein. Drugs that induce or inhibit P-glycoprotein in intestine or kidney have the potential to alter digoxin pharmacokinetics.
| Digoxin concentrations increased > 50% | |||
| Digoxin Serum Concentration Increase |
Digoxin AUC Increase |
Recommendations | |
| Amiodarone | 70% | NA | Measure serum digoxin concentrations before initiating concomitant drugs. Reduce digoxin concentrations by decreasing dose by approximately 30% to 50% or by modifying the dosing frequency and continue monitoring. |
| Captopril | 58% | 39% | |
| Clarithromycin | NA | 70% | |
| Dronedarone | NA | 150% | |
| Gentamicin | 129-212% | NA | |
| Erythromycin | 100% | NA | |
| Itraconazole | 80% | NA | |
| Nitrendipine | 57% | 15% | |
| Propafenone | NA | 60-270% | |
| Quinidine | 100% | NA | |
| Ranolazine | 50% | NA | |
| Ritonavir | NA | 86% | |
| Tetracycline | 100% | NA | |
| Verapamil | 50-75% | NA | |
| Digoxin concentrations increased < 50% | |||
| Atorvastatin | 22% | 15% | Measure serum digoxin concentrations before initiating concomitant drugs. Reduce digoxin concentrations by decreasing the dose by approximately 15% to 30% or by modifying the dosing frequency and continue monitoring. |
| Carvedilol | 16% | 14% | |
| Diltiazem | 20% | NA | |
| Indomethacin | 40% | NA | |
| Nefazodone | 27% | 15% | |
| Nifedipine | 45% | NA | |
| Propantheline | 24% | 24% | |
| Quinine | NA | 33% | |
| Saquinavir | 27% | 49% | |
| Spironolactone | 25% | NA | |
| Telmisartan | 20-49% | NA | |
| Tolvaptan | 30% | NA | |
| Trimethoprim | 22-28% | NA | |
| Digoxin concentrations increased, but magnitude is unclear | |||
| Alprazolam, azithromycin, cyclosporine, diclofenac, diphenoxylate, epoprostenol, esomeprazole, ibuprofen, ketoconazole, lansoprazole, metformin, omeprazole, quinine, rabeprazole, |
Measure serum digoxin concentrations before initiating concomitant drugs. Continue monitoring and reduce digoxin dose as necessary. | ||
| Digoxin concentrations decreased | |||
| Acarbose, activated charcoal, albuterol, antacids, certain cancer chemotherapy or radiation therapy, cholestyramine, colestipol, extenatide, kaolin-pectin, meals high in bran, metoclopramide, miglitol, neomycin, penicillamine, phenytoin, rifampin, St. John’s Wort, sucralfate, sulfasalazine |
Measure serum digoxin concentrations before initiating concomitant drugs. Continue monitoring and increase digoxin dose by approximately 20 % to 40 % as necessary. | ||
| No significant Digoxin exposure changes | |||
| Please refer to section 12 for a complete list of drugs which were studies but reported no significant changes on digoxin exposure. |
No additional actions are required. | ||
| NA – Not available/reported |
Due to considerable variability of pharmacodynamic interactions, the dosage of digoxin should be individualized when patients receive these medications concurrently.
| Drugs that Affect Renal Function | Caution should be exercised when combining digoxin with any drug that may cause significant deterioration in renal function (e.g., ACE inhibitors, angiotensin receptor blockers, nonsteroidal anti-inflammatory drugs [NSAIDs], COX-2 inhibitors) since a decline in glomerular filtration or tubular secretion may impair the excretion of digoxin. | |
| Antiarrthymics | Dofetilide | Concomitant administration with digoxin was associated with a higher rate of torsades de pointes |
| Sotalol | Proarrhythmic events were more common in patients receiving sotalol and digoxin than on either alone; it is not clear whether this represents an interaction or is related to the presence of CHF, a known risk factor for proarrhythmia, in patients receiving digoxin. | |
| Dronedarone | Sudden death was more common in patients receiving digoxin with dronedarone than on either alone; it is not clear whether this represents an interaction or is related to the presence of advanced heart disease, a known risk factor for sudden death in patients receiving digoxin. | |
| Parathyroid Hormone Analog | Teriparatide | Sporadic case reports have suggested that hypercalcemia may predispose patients to digitalis toxicity. Teriparatide transiently increases serum calcium. |
| Thyroid supplement | Thyroid | Treatment of hypothyroidism in patients taking digoxin may increase the dose requirements of digoxin. |
| Sympathomimetics | Epinephrine Norepinephrine Dopamine |
Can increase the risk of cardiac arrhythmias |
| Neuromuscular Blocking Agents | Succinylcholine | May cause sudden extrusion of potassium from muscle cells causing arrhythmias in patients taking digoxin. |
| Supplements | Calcium | If administered rapidly by intravenous route, can produce serious arrhythmias in digitalized patients. |
| Beta-adrenergic blockers and calcium channel blockers | Additive effects on AV node conduction can result in bradycardia and advanced or complete heart block. |
Endogenous substances of unknown composition (digoxin-like immunoreactive substances, DLIS) can interfere with standard radioimmunoassays for digoxin. The interference most often causes results to be falsely positive or falsely elevated, but sometimes it causes results to be falsely reduced. Some assays are more subject to these failings than others. Several LC/MS/MS methods are available that may provide less susceptibility to DLIS interference. DLIS are present in up to half of all neonates and in varying percentages of pregnant women, patients with hypertrophic cardiomyopathy, patients with renal or hepatic dysfunction, and other patients who are volume-expanded for any reason. The measured levels of DLIS (as digoxin equivalents) are usually low (0.2 to 0.4 ng/mL), but sometimes they reach levels that would be considered therapeutic or even toxic.
In some assays, spironolactone, canrenone and potassium canrenoate may be falsely detected as digoxin, at levels up to 0.5 ng/mL. Some traditional Chinese and Ayurvedic medicine substances like Chan Su, Siberian Ginseng, Asian Ginseng, Ashwagandha or Dashen, can cause similar interference.
Spironolactone and DLIS are much more extensively protein-bound than digoxin. As a result, assays of free digoxin levels in protein-free ultrafiltrate (which tend to be about 25% less than total levels, consistent with the usual extent of protein binding) are less affected by spironolactone or DLIS. It should be noted that ultrafiltration does not solve all interference problems with alternative medicines. The use of an LC/MS/MS method may be the better option according to the good results it provides, especially in term of specificity and limit of quantization.
USE IN SPECIFIC POPULATIONS
Digoxin should be given to a pregnant woman only if clearly needed. It is also not known whether digoxin can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Animal reproduction studies have not been conducted with digoxin.
There is not enough data from clinical trials to determine the safety and efficacy of digoxin during labor and delivery.
Studies have shown that digoxin distributes into breast milk, and that the milk-to-serum concentration ratio is approximately 0.6 to 0.9. However, the estimated exposure of a nursing infant to digoxin via breastfeeding is far below the usual infant maintenance dose. Therefore, this amount should have no pharmacologic effect upon the infant. Nevertheless, caution should be exercised when digoxin is administered to a nursing woman.
The safety and effectiveness of LANOXIN in the control of ventricular rate in children with atrial fibrillation in children have not been established.
The safety and effectiveness of LANOXIN in the treatment of heart failure in children have not been established in adequate and well-controlled studies. However, in published literature of children with heart failure due to various etiologies (e.g., ventricular septal defects, anthracycline toxicity, patent ductus arteriosus), treatment with digoxin has been associated with improvements in hemodynamic parameters, and in clinical signs and symptoms.
Newborn infants display considerable variability in their tolerance to digoxin. Premature and immature infants are particularly sensitive to the effects of digoxin, and the dosage of the drug must not only be reduced but must be individualized according to their degree of maturity.
The majority of clinical experience gained with digoxin has been in the elderly population. This experience has not identified differences in response or adverse effects between the elderly and younger patients. However, this drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, which should be based on renal function, and it may be useful to monitor renal function [see Dosage and Administration (2.1)].
The clearance of digoxin can be primarily correlated with the renal function as indicated by creatinine clearance. Tables 2 and 4 provides the usual daily maintenance dose requirements for digoxin based on creatinine clearance (per 70 kg or per 1.73 m2) [see Dosage and Administration (2.3)].
Digoxin is primarily excreted by the kidneys; therefore, patients with impaired renal function require smaller than usual maintenance doses of digoxin [see Dosage and Administration (2.3)]. Because of the prolonged elimination half-life, a longer period of time is required to achieve an initial or new steady-state serum concentration in patients with renal impairment than in patients with normal renal function. If appropriate care is not taken to reduce the dose of digoxin, such patients are at high risk for toxicity, and toxic effects will last longer in such patients than in patients with normal renal function.
Plasma digoxin concentrations in patients with acute hepatitis generally fall within the range of profiles in a group of healthy subjects.
The absorption of digoxin is reduced in some malabsorption conditions such as chronic diarrhea.
OVERDOSAGE
The signs and symptoms of toxicity are generally similar to those described in the Adverse Reactions (6.1) but may be more frequent and can be more severe. Signs and symptoms of digoxin toxicity become more frequent with levels above 2 ng/mL. However, in deciding whether a patient’s symptoms are due to digoxin, the clinical state together with serum electrolyte levels and thyroid function are important factors [see Dosage and Administration (2)].
Adults: In adults, the signs and symptoms of toxicity are similar to those described in Adverse Reactions (6) but may be more frequent and severe. The most common signs and symptoms of digoxin toxicity are nausea, vomiting, anorexia, and fatigue that occur in 30 to 70% of patients who are overdosed. Extremely high serum concentrations produce hyperkalemia especially in patients with impaired renal function. Almost every type of cardiac arrhythmia has been associated with digoxin overdose and multiple rhythm disturbances in the same patient are common. Peak cardiac effects occur 3 to 6 hours following ingestion and may persist for 24 hours or longer. Arrhythmias that are considered more characteristic of digoxin toxicity are new-onset Mobitz type 1 A-V block, accelerated junctional rhythms, non-paroxysmal atrial tachycardia with A-V block, and bi-directional ventricular tachycardia. Cardiac arrest from asystole or ventricular fibrillation is usually fatal.
Digoxin toxicity is related to serum concentration. As digoxin serum levels increase above 1.2 ng/mL, there is a potential for increase in adverse reactions. Futhermore, lower potassium levels increases the risk for adverse reactions. In adults with heart disease, clinical observations suggest that an overdose of digoxin of 10 to 15 mg results in death of half of patients. A dose above 25 mg ingested by an adult without heart disease appeared to be uniformly fatal if no Digoxin Immune Fab (DIGIBIND®, DIGIFAB®) was administered.
Among the extra-cardiac manifestations, gastrointestinal symptoms (e.g. nausea, vomiting, anorexia) are very common (up to 80% incidence) and precede cardiac manifestations in approximately half of the patients in most literature reports. Neurologic manifestations (e.g. dizziness, various CNS disturbances), fatigue, and malaise are very common. Visual manifestations may also occur with aberration in color vision (predominance of yellow green) the most frequent. Neurological and visual symptoms may persist after other signs of toxicity have resolved. In chronic toxicity, non-specific extra-cardiac symptoms, such as malaise and weakness, may predominate.
Children: In pediatric patients, signs and symptoms of toxicity can occur during or shortly after the dose of digoxin. Frequent non-cardiac effects are similar to those observed in adults although nausea and vomiting are not seen frequently in infants and small pediatric patients. Other reported manifestations of overdose are weight loss in older age groups, failure to thrive in infants, abdominal pain caused by mesenteric artery ischemia, drowsiness, and behavioral disturbances including psychotic episodes. Arrhythmias and combinations of arrhythmias that occur in adult patients can also occur in pediatric patients although sinus tachycardia, supraventricular tachycardia, and rapid atrial fibrillation are seen less frequently in pediatric patients. Pediatric patients are more likely to develop A-V conduction disturbances, or sinus bradycardia. Any arrhythmia in a child treated with digoxin should be considered related to digoxin until otherwise ruled out. In pediatric patients aged 1 to 3 years without heart disease, clinical observations suggest that an overdose of digoxin of 6 to 10 mg would result in death of half of the patients. In the same population, a dose above 10 mg resulted in death if no Digoxin Immune Fab was administered.
Chronic Overdose
If there is suspicion of toxicity, digoxin should be discontinued and the patient placed on a cardiac monitor. Contributing factors such as electrolyte abnormalities, thyroid dysfunction, and concomitant medications should be corrected [see Dosage and Administration (2.5)]. Hypokalemia should be corrected by administering potassium so that serum potassium is maintained between 4.0 and 5.5 mmol/L. Potassium is usually administered orally, but when correction of the arrhythmia is urgent and serum potassium concentration is low, potassium may be administered cautiously by the intravenous route. The electrocardiogram should be monitored for any evidence of potassium toxicity (e.g. peaking of T waves) and to observe the effect on the arrhythmia. Potassium salts should be avoided in patients with bradycardia or heart block. Symptomatic arrhythmias may be treated with Digoxin Immune Fab.
Acute Overdose
Patients who have intentionally or accidently ingested massive doses of digoxin should receive activated charcoal orally or by nasogastric tube regardless of the time since ingestion since digoxin recirculates to the intestine by enterohepatic circulation. In addition to cardiac monitoring, digoxin should be temporarily discontinued until the adverse reaction resolves. Factors that may be contributing to the adverse reactions should also be corrected [see Warnings and Precautions (5)]. In particular, hypokalemia and hypomagnesemia should be corrected. Digoxin is not effectively removed from the body by dialysis because of its large extravascular volume of distribution. Life threatening arrhythmias (ventricular tachycardia, ventricular fibrillation, high degree A-V block, bradyarrhythma, sinus arrest) or hyperkalemia requires administration of Digoxin Immune Fab. Digoxin Immune Fab has been shown to be 80-90% effective in reversing signs and symptoms of digoxin toxicity. Bradycardia and heart block caused by digoxin are parasympathetically mediated and respond to atropine. A temporary cardiac pacemaker may also be used. Ventricular arrhythmias may respond to lidocaine or phenytoin. When a large amount of digoxin has been ingested, especially in patients with impaired renal function, hyperkalemia may be present due to release of potassium from skeletal muscle. In this case, treatment with Digoxin Immune Fab is indicated; an initial treatment with glucose and insulin may be needed if the hyperkalemia is life-threatening. Once the adverse reaction has resolved, therapy with digoxin may be reinstituted following a careful reassessment of dose.
LANOXIN DESCRIPTION
LANOXIN (digoxin) is a cardiac glycoside, aclosely related group of drugs having in common specific effects on the myocardium. These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitalis lanata. The term “digitalis” is used to designate the whole group of glycosides. The glycosides are composed of 2 portions: a sugar and a cardenolide (hence “glycosides”).
Digoxin is described chemically as (3β,5β,12β)-3-[(O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-2,6-dideoxy-β-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy-card-20(22)-enolide. Its molecular formula is C41H64O14, its molecular weight is 780.95, and its structural formula is:
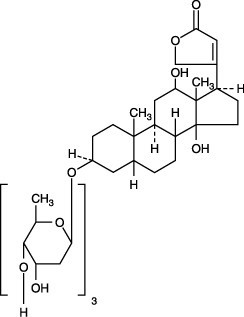
Digoxin exists as odorless white crystals that melt with decomposition above 230°C. The drug is practically insoluble in water and in ether; slightly soluble in diluted (50%) alcohol and in chloroform; and freely soluble in pyridine.
LANOXIN is supplied as 125 mcg (0.125-mg) or 250 mcg (0.25-mg) tablets for oral administration. Each tablet contains the labeled amount of digoxin USP and the following inactive ingredients: corn and potato starches, lactose, and magnesium stearate. In addition, the dyes used in the 125 mcg (0.125 mg) tablets are D&C Yellow No. 10 and FD&C Yellow No. 6.
CLINICAL PHARMACOLOGY
All of digoxin’s actions are mediated through its effects on Na-K ATPase. This enzyme, the “sodium pump,” is responsible for maintaining the intracellular milieu throughout the body by moving sodium ions out of and potassium ions into cells. By inhibiting Na-K ATPase, digoxin
- causes increased availability of intracellular calcium in the myocardium and conduction system, with consequent increased inotropy, increased automaticity, and reduced conduction velocity
- indirectly causes parasympathetic stimulation of the autonomic nervous system, with consequent effects on the sino-atrial (SA) and atrioventricular (AV) nodes
- reduces catecholamine reuptake at nerve terminals, rendering blood vessels more sensitive to endogenous or exogenous catecholamines
- increases baroreceptor sensitization, with consequent increased carotid sinus nerve activity and enhanced sympathetic withdrawal for any given increment in mean arterial pressure
- increases (at higher concentrations) sympathetic outflow from the central nervous system (CNS) to both cardiac and peripheral sympathetic nerves
- allows (at higher concentrations) progressive efflux of intracellular potassium, with consequent increase in serum potassium levels.
The cardiologic consequences of these direct and indirect effects are an increase in the force and velocity of myocardial systolic contraction (positive inotropic action), a slowing of the heart rate (negative chronotropic effect), decreased conduction velocity through the AV node, and a decrease in the degree of activation of the sympathetic nervous system and renin-angiotensin system (neurohormonal deactivating effect).
The times to onset of pharmacologic effect and to peak effect of preparations of LANOXIN are shown in Table 7.
| Product | Time to Onset of Effecta | Time to Peak Effecta |
| LANOXIN Tablets | 0.5 - 2 hours | 2 - 6 hours |
| LANOXIN Injection/IV | 5 - 30 minutesb | 1 - 4 hours |
|
a Documented for ventricular response rate in atrial fibrillation, inotropic effects and electrocardiographic changes. b Depending upon rate of infusion. |
Hemodynamic Effects: Short- and long-term therapy with the drug increase cardiac output and lowers pulmonary artery pressure, pulmonary capillary wedge pressure, and systemic vascular resistance in patients with heart failure. These hemodynamic effects are accompanied by an increase in the left ventricular ejection fraction and a decrease in end-systolic and end-diastolic dimensions.
ECG Changes: The use of therapeutic doses of LANOXIN may cause prolongation of the PR interval and depression of the ST segment on the electrocardiogram. LANOXIN may produce false positive ST-T changes on the electrocardiogram during exercise testing. These electrophysiologic effects are not indicative of toxicity. LANOXIN does not significantly reduce heart rate during exercise.
Absorption: Following oral administration, peak serum concentrations of digoxin occur at 1 to 3 hours. Absorption of digoxin from LANOXIN Tablets has been demonstrated to be 60% to 80% complete compared to an identical intravenous dose of digoxin (absolute bioavailability). When LANOXIN Tablets are taken after meals, the rate of absorption is slowed, but the total amount of digoxin absorbed is usually unchanged. When taken with meals high in bran fiber, however, the amount absorbed from an oral dose may be reduced. Comparisons of the systemic availability and equivalent doses for oral preparations of LANOXIN are shown in Dosage and Administration (2.6).
Digoxin is a substrate for P-glycoprotein. As an efflux protein on the apical membrane of enterocytes, P-glycoprotein may limit the absorption of digoxin.
In some patients, orally administered digoxin is converted to inactive reduction products (e.g., dihydrodigoxin) by colonic bacteria in the gut. Data suggest that 1 in 10 patients treated with digoxin tablets, colonic bacteria will degrade 40% or more of the ingested dose. As a result, certain antibiotics may increase the absorption of digoxin in such patients. Although inactivation of these bacteria by antibiotics is rapid, the serum digoxin concentration will rise at a rate consistent with the elimination half-life of digoxin. Serum digoxin concentration relates to the extent of bacterial inactivation, and may be as much as doubled in some cases [see Drug Interactions (7.2)].
Patients with malabsorption syndromes (e.g., short bowel syndrome, celiac sprue, jejunoileal bypass) may have a reduced ability to absorb orally administered digoxin.
Distribution: Following drug administration, a 6- to 8-hour tissue distribution phase is observed. This is followed by a much more gradual decline in the serum concentration of the drug, which is dependent on the elimination of digoxin from the body. The peak height and slope of the early portion (absorption/distribution phases) of the serum concentration-time curve are dependent upon the route of administration and the absorption characteristics of the formulation. Clinical evidence indicates that the early high serum concentrations do not reflect the concentration of digoxin at its site of action, but that with chronic use, the steady-state post-distribution serum concentrations are in equilibrium with tissue concentrations and correlate with pharmacologic effects. In individual patients, these post-distribution serum concentrations may be useful in evaluating therapeutic and toxic effects [see Dosage and Administration (2.1)].
Digoxin is concentrated in tissues and therefore has a large apparent volume of distribution (approximately 475 to 500L). Digoxin crosses both the blood-brain barrier and the placenta. At delivery, the serum digoxin concentration in the newborn is similar to the serum concentration in the mother. Approximately 25% of digoxin in the plasma is bound to protein. Serum digoxin concentrations are not significantly altered by large changes in fat tissue weight, so that its distribution space correlates best with lean (i.e., ideal) body weight, not total body weight.
Metabolism: Only a small percentage (13%) of a dose of digoxin is metabolized in healthy volunteers. The urinary metabolites, which include dihydrodigoxin, digoxigenin bisdigitoxoside, and their glucuronide and sulfate conjugates, are polar in nature and are postulated to be formed via hydrolysis, oxidation, and conjugation. The metabolism of digoxin is not dependent upon the cytochrome P-450 system, and digoxin is not known to induce or inhibit the cytochrome P-450 system.
Excretion: Elimination of digoxin follows first-order kinetics (that is, the quantity of digoxin eliminated at any time is proportional to the total body content). Following intravenous administration to healthy volunteers, 50% to 70% of a digoxin dose is excreted unchanged in the urine. Renal excretion of digoxin is proportional to creatinine clearance and is largely independent of urine flow. In healthy volunteers with normal renal function, digoxin has a half-life of 1.5 to 2 days. The half-life in anuric patients is prolonged to 3.5 to 5 days. Digoxin is not effectively removed from the body by dialysis, exchange transfusion, or during cardiopulmonary bypass because most of the drug is bound to extravascular tissues.
Special Populations: Geriatrics: Because of age-related declines in renal function, elderly patients would be expected to eliminate digoxin more slowly than younger subjects. Elderly patients may also exhibit a lower volume of distribution of digoxin due to age-related loss of lean muscle mass. Thus, the dosage of digoxin should be carefully selected and monitored in elderly patients [see Use in Specific Populations (8.5)].
Gender: In a study of 184 patients, the clearance of digoxin was 12% lower in females than in male patients. This difference is not likely to be clinically important.
Hepatic Impairment: Because only a small percentage (approximately 13%) of a dose of digoxin undergoes metabolism, hepatic impairment would not be expected to significantly alter the pharmacokinetics of digoxin. In a small study, plasma digoxin concentration profiles in patients with acute hepatitis generally fell within the range of profiles in a group of healthy subjects. No dosage adjustments are recommended for patients with hepatic impairment; however, serum digoxin concentrations should be used as appropriate to help guide dosing in these patients.
Renal Impairment: Since the clearance of digoxin correlates with creatinine clearance, patients with renal impairment generally demonstrate prolonged digoxin elimination half-lives and greater exposures to digoxin. Therefore, digoxin must be carefully titrated in these patients based on clinical response, and based on monitoring of serum digoxin concentrations, as appropriate.
Race: The impact of race differences on digoxin pharmacokinetics have not been formally studied. Because digoxin is primarily eliminated as unchanged drug via the kidney and because there are no important differences in creatinine clearance among races, pharmacokinetic differences due to race are not expected.
Drug-drug Interactions
Based on literature reports no significant changes in digoxin exposure were reported when digoxin was co-administered with the following drugs:
alfuzosin, aliskiren, amlodipine, aprepitant, argatroban, aspirin, atorvastatin, benazepril, bisoprolol, black cohosh, bosentan, candesartan, citalopram, clopidogrel, colesevelam, dipyridamole, disopyramide, donepezil, doxazosin, dutasteride, echinacea, enalapril, eprosartan, ertapenem, escitalopram, esmolol, ezetimibe, famciclovir, felodipine, finasteride, flecainide, fluvastatin, fondaparinux, galantamine, gemifloxacin, grapefruit juice, irbesartan, isradipine, ketorlac, levetiracetam, levofloxacin, lisinopril, losartan, lovastatin, meloxicam, mexilitine, midazolam, milk thistle, moexipril, montelukast, moxifloxacin, mycophenolate, nateglinide, nesiritide, nicardipine, nisoldipine, olmesartan, orlistat, pantoprazole, paroxetine,perindopril, pioglitazone, pravastatin, prazosin, procainamide, quinapril, raloxifene, ramipril, repaglinide, rivastigmine, rofecoxib, ropinirole, rosiglitazone, rosuvastatin, sertraline, sevelamer, simvastatin, sirolimus, solifenacin, tamsulosin, tegaserod, terbinafine, tiagabine, ticlopidine, tigecycline, topiramate, torsemide, tramadol, trandolapril, triamterene, trospium, trovafloxacin, valacyclovir, valsartan, varenicline, voriconazole, zaleplon, zolpidem
NONCLINICAL TOXICOLOGY
Digoxin showed no genotoxic potential in in vitro studies (Ames test and mouse lymphoma). No data are available on the carcinogenic potential of digoxin, nor have studies been conducted to assess its potential to affect fertility.
CLINICAL STUDIES
Two 12-week, double-blind, placebo-controlled studies enrolled 178 (RADIANCE trial) and 88 (PROVED trial) patients with NYHA class II or III heart failure previously treated with digoxin, a diuretic, and an ACE inhibitor (RADIANCE only) and randomized them to placebo or treatment with LANOXIN. Both trials demonstrated better preservation of exercise capacity in patients randomized to LANOXIN. Continued treatment with LANOXIN reduced the risk of developing worsening heart failure, as evidenced by heart failure-related hospitalizations and emergency care and the need for concomitant heart failure therapy.
Dig Trial of LANOXIN in Patients with Heart Failure
The Digitalis Investigation Group (DIG) main trial was a 37-week, multicenter, randomized, double-blind mortality study comparing digoxin to placebo in 6800 adult patients with heart failure and left ventricular ejection fraction ≤0.45. At randomization, 67% were NYHA class I or II, 71% had heart failure of ischemic etiology, 44% had been receiving digoxin, and most were receiving a concomitant ACE inhibitor (94%) and diuretics (82%). As in the smaller trials described above, patients who had been receiving open-label digoxin were withdrawn from this treatment before randomization. Randomization to digoxin was again associated with a significant reduction in the incidence of hospitalization, whether scored as number of hospitalizations for heart failure (relative risk 75%), risk of having at least one such hospitalization during the trial (RR 72%), or number of hospitalizations for any cause (RR 94%). On the other hand, randomization to digoxin had no apparent effect on mortality (RR 99%, with confidence limits of 91 to 107%).
Digoxin has also been studied as a means of controlling the ventricular response to chronic atrial fibrillation in adults. Digoxin reduced the resting heart rate, but not the heart rate during exercise.
In 3 different randomized, double-blind trials that included a total of 315 adult patients, digoxin was compared to placebo for the conversion of recent-onset atrial fibrillation to sinus rhythm. Conversion was equally likely, and equally rapid, in the digoxin and placebo groups. In a randomized 120-patient trial comparing digoxin, sotalol, and amiodarone, patients randomized to digoxin had the lowest incidence of conversion to sinus rhythm, and the least satisfactory rate control when conversion did not occur.
In at least one study, digoxin was studied as a means of delaying reversion to atrial fibrillation in adult patients with frequent recurrence of this arrhythmia. This was a randomized, double-blind, 43-patient crossover study. Digoxin increased the mean time between symptomatic recurrent episodes by 54%, but had no effect on the frequency of fibrillatory episodes seen during continuous electrocardiographic monitoring.
HOW SUPPLIED
LANOXIN (digoxin) Tablets, Scored 125 mcg (0.125 mg): Bottles of 100 with child-resistant cap (NDC 0173-0242-55) and 1,000 (NDC 0173-0242-75); unit dose pack of 100 (NDC 0173-0242-56). Imprinted with LANOXIN and Y3B (yellow).
LANOXIN (digoxin) Tablets, Scored 250 mcg (0.25 mg): Bottles of 100 with child-resistant cap (NDC 0173-0249-55), 1,000 (NDC 0173-0249-75), and 5,000 (NDC 0173-0249-80); unit dose pack of 100 (NDC 0173-0249-56). Imprinted with LANOXIN and X3A (white).
Store at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F) in a dry place. Keep out of reach of children.
INFORMATION FOR PATIENTS
- Advise patients that digoxin is a cardiac glycoside used to treat heart failure and heart arrhythmias. Digoxin helps the heart beat more efficiently in adults and pediatric patients and decreases the heart rate at rest during abnormal rhythms in adults.
- Instruct patients to take this medication as directed by their physician. The dose of digoxin should not be adjusted without consulting with a physician or other healthcare professional.
- Advise patients that many drugs can interact with digoxin. Patients should be instructed to inform their doctor and pharmacist if they are taking any over the counter medications, including herbal medication, or are started on a new prescription.
- The patient should be made aware that blood tests will be necessary to ensure that their digoxin dose is appropriate for them.
- Advise patients to contact their doctor or a health care professional if they experience nausea, vomiting, persistent diarrhea, confusion, weakness, or visual disturbances (including blurred vision, green-yellow color disturbances, halo effect) as these could be signs that the dose of digoxin may be too high.
- Advise parents or caregivers that the symptoms of having too high digoxin doses may be difficult to recognize in infants and pediatric patients. Symptoms such as weight loss, failure to thrive in infants, abdominal pain, and behavioral disturbances may be indications of digoxin toxicity.
- Suggest to the patient to monitor and record their heart rate and blood pressure daily.
- Instruct women of childbearing potential who become or are planning to become pregnant to consult a physician prior to initiation or continuing therapy with digoxin.
SPL UNCLASSIFIED
LANOXIN is a registered trademark of GlaxoSmithKline
Manufactured for
GlaxoSmithKline
Research Triangle Park, NC 27709
by DSM Pharmaceuticals, Inc.
Greenville, NC 27834 or
GlaxoSmithKline
Research Triangle Park, NC 27709
©2012, GlaxoSmithKline. All rights reserved.
06/2012
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION

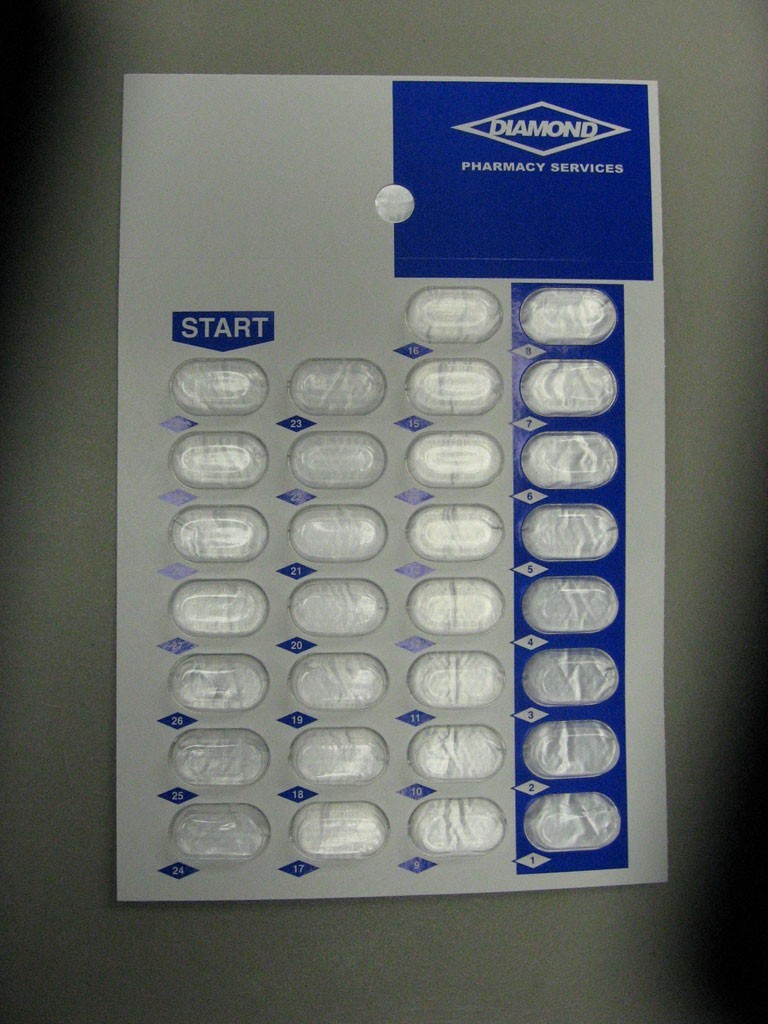
LANOXINdigoxin TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||