ISOVUE-M 200
General Injectables & Vaccines, Inc.
ISOVUE-M 200
FULL PRESCRIBING INFORMATION: CONTENTS*
- Description
- Clinical Pharmacology
- ISOVUE-M 200 Indications and Usage
- Contraindications
- Warnings
- Precautions
- Adverse Reaction
- Overdosage
- Dosage and Administration
- How Supplied
- Sample Outer Label
FULL PRESCRIBING INFORMATION
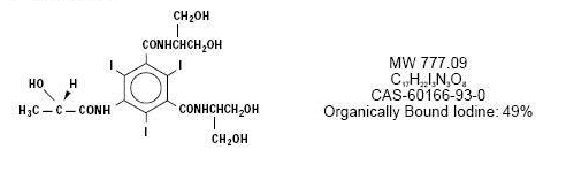
Description
Diagnostic
NONIONIC RADIOPAQUE CONTRAST MEDIA
For Intrathecal Administration in Neuroradiology
Including Myelography (Lumbar, Thoracic, Cervical, Total Columnar) Pediatric Myelography (Lumbar, Thoracic), and for Contrast Enhancement of Computed Tomographic (CECT) Cisternography and Ventriculography
ISOVUE-M (Iopamidol Injection) formulations are stable, aqueous, sterile, and nonprrogenic solutions for intrathecal administration. Each mL of ISOVUE-M 200 (lopamidol Injection 41%) provides 408 mg iopamidol with 1mg tromethamine and 0.26 mg edetate calcium disodium. The solution contains approximately 0.029 mg (0.001mEq) sodium and 200 mg organically bound iodine per mL. Each mL of ISOVUE-M 300 (lopamidol Injection 61%) provides 612 mg iopamidol with 1 mg tromethamine and 0.39 mg edetate calcium disodium. The solution contains approximately 0.043 mg (0.002 mEq) sodium and 300 mg organically bound iodine per mL. The pH of ISOVUE-M contrast media has been adjusted to 6.5-7.5 with hydrochloric acid and/or sodium hydroxide. Pertinent physicochemical data are noted below. ISOVUE-M (lopamidol Injection) is hypertonic as compared to plasma and cerbrospinal fluid (approximately 285 and 301 mOsm/kg water, respectively).
|
|
Iopamidol |
|
| Parameter | 41% | 61% |
| Concentration | 200 | 300 |
| (mgl/mL) |
|
|
| Osmolality @ 37 degrees C | 413 | 616 |
| (mOsm/kg water) |
|
|
| Visosity (cP) @ 37 degrees C | 2.0 | 4.7 |
| @ 20 degrees C | 3.3 | 8.8 |
| Specific Gravity @37 degrees C | 1.216 | 1.328 |
Clinical Pharmacology
The pharmacokinetics of intravenously administered iopamidol in normal subjects conform to an open two-compartment model with first order elimination (a rapid alpha phase for drug distribution and a slow beta phase for drug elimination). The elimination serum or plasma half-life is approximately two hours; the half-life is not dose dependent. No significant metabolism, deiodination, or biotransformation occurs. Iopamidol is rapidly absorbed into the bloodstream from cerebrospinal fluid (CSF); following intrathecal administration, iopamidol apperrs in plasma within one hour and virtually all of the drug reaches the systemic circulation within 24 hours, Iopamidol is excreted mainly through the kidneys following intrthecal administration, and the drug is essentially undetectable in the plasma 48 hours later. In patients with impaired renal function, the elimination half-life is prolonged dependent upon the degree of impairment. In the absence of renal dysfunction, the cumulative urinary excretion for iopamidol, expressed as a percentage of administered intravenous dose is approximately 35 to 40 percent at 60 minutes, 80 to 90 percent at 8 hours, and 90 percent or more in the 72- to 96-hour period after admininstration. In normal subjects approximately 1 percent or less of the administered dose appears in cumulative 72- to 96-hour fecal specimens. Iopamidol displays little tendency to bind to serum or plasma proteins. No evidence of in vivo complement activation has been found in normal subjects. Animal studies indicate that iopamidol does not cross the blood-brain barrier to any significant extent following intravascular administration.
ISOVUE-M 200 Indications and Usage
ISOVUE-M (Iopamidol Injection) is indicated for intrathecal administration in adult neuroradiology inculding myelography(lumbar, thoracic, cervical, total columnar), and for contrast enhancement of computed tomographic (CECT) cisternography and ventriculography. ISOVUE-M 200 (lopamidol Injection) is indicated for thoraco-lumbar myelography in children over the age of two years.
Contraindications
Intrathecal administration of corticosteroids with iopamidol is contraindicated. Because of overdosage considerations, immediate repeat myelography in the event of technical failure is contraindicated (see interval recommendation under DOSAGE AND ADMINISTRATION). Myelography should not be performed in the presence of significant local or systemic infection where bacteremia is likely.
Warnings
The need for myelographic examination should be
carefully evaluated. Iopamidol should be administered with caution in
patients with increased intrcranial pressure or suspicion of
intracranial tumor, abscess or hematoma, those with a history of
convulsive disorder, severe cardiovascular disease, chronic alcoholism,
or multiple sclerosis, and elderly patients. Particular attention must
be given to state of hydration, concentration of medium, dose, and
technique used in these patients. Contrast media may promote sickling
in individuals who are homozygous for sickle cell disease when injected
intravenously or intra-arterially. Although ISOVUE-M is not injected
intravascularly, measurable plasma levels are attained after
intrathecal administration of iopamidol. If frankly bloody
cerebrospinal fluid is observed, the possible benefits of a
myelographic examination should be considered in terms of risk to the
patient.
Patients on anticonvulsant medication should be maintained on this therapy.
Direct intracisternal or ventricular administration for standard radiography (without computerized tomographic enhancement) is not recommended. Inadvertent intracranial entry of a large or concentrated bolus of the contrast medium, which increase the risk of neurotoxicity, can be prevented by careful patient management. Also, effort should be directed to avoid rapid dispersion of the medium causing inadvertent rise to intracranial levels (e.g., by active patient movement). If such intracranial entry of the medium occurs, prophylactic anticonvulsant treatment with diazepam or barbiturates orally for 24 to 48 hours should be considered.
Use of medications that may lower the seizure thresnold (phenothiazine derivatives, including those used for their antihistaminic properties; tricyclic antidepressants; MAO inhibitors; CNS stimulants; analeptics; antipsychotic agents) should be carefully evaluated While the contributory role of such medications has not been established, some physicians have discontinued these agents at least 48 hours before and for at least 24 hours following intrathecal use.
Focal and generalized motor seizures have been reported after intrathecal use of water-soluble contrast agents including iopamidol. In several of those cases reported with iopamidol, higher than recommended doses were employed. Therfore avoid:
- Deviations from recommended neuroradiologic procedure or patient management.
- Use in patients with a history of epilepsy unless medically justified.
- Overdosage.
- Intracranial entry of a bolus or premature diffusion of a high concentration of the medium.
- Failure to maintain elvation of the head during the procedure, on the stretcher, and in bed.
- Excessive and particularly active patient movement or straining.
Precautions
General
Diagnostic procedures which involve the use of any radiopaque agent should be carried out under the direction of personnel with the prerequisite training and with a thorough knowledge of the particular procedure to be performed. Appropriate facilities should be available for coping with any complication of the procedure, as well as for emergency treatment of severe reaction to the contrast agent itself. After parenteral administration of a radiopaque agent, competent personnel and emergency facilities should be available for at least 30 to 60 minutes since sever delayed reactions may occur.
Preparatory dehydration is dangerous and may contribute to acute renal failure in patients with advanced vascular disease, diabetic patients, and in susceptible nondiabetic patients (often elderly with preexisting renal disease). Patients should be well hydrated prior to and following iopamidol administration.
Preparatory dehydration is dangerous and may contribute to acute renal failure in patients with advanced vascular disease, diabetic patients, and in susceptible nondiabetic patients (often elderly with preexisting renal disease). Patients should be well hydrated prior to following iopamidol administration.
The possibility of a reaction, including serious, life-threatening, fatal, anaphylactoid or cardiovascular reactions, should always be considered (see ADVERSE REACTIONS). Patients at increased risk include those with a history of a previous reaction to a contrast medium, patients with a know sensitivity to iodine per se, and patients with a know clinical hypersensitivity (bronchial asthma, hay fever, and food allergies). The occurrence of sever idiosyncratic reactions has prompted the use of several pretesting methods. However, pretesting cannot be relied upon to predict severe reactions and may itself be hazardous for the patient. It is suggested that a thorough medical history with emphasis on allergy and hypersensitivity, prior to the injection of any contrast medium, may be more accurate than pretesting in predicting potential adverse reactions. A positive history of allergies or hypersensitivity does not arbitrarily contraindicate the use of a contrast agent where a diagnostic procedure is thought essential, but caution should be exercised. Premedication with antihistamines or corticosteroids to avoid or minimize possible allergic reactions in such patients should be considered (see CONTRAINDICATIONS).
Reports indicate that such pretreatment does not prevent serious life-threatening reactions, but may reduce both their incidence and severity.
The possibility of inducing bacterial meningitis in patients during intrathecal procedures should always be considered. To avoid bacterial contamination during spinal puncture, a sterile field should be maintained at all times.
If nondisposable equipment is used, scrupulous care should be taken to prevent residual contamination with traces of cleansing agents.
Information for Patients
Patients receiving injectable radiopaque diagnostic agents should be instructed to:
1. Inform your physician if you are pregnant.
2. Inform your physician if you are diabetic or if you have multiple myeloma, pheochromocytoma, homozygous sickle cell disease, or known thyroid disorder.
3. Inform your physician if you are allergic to any drugs, food, or if you had any reactions to previous injections of substance used for x-ray procedures (see PRECAUTIONS-General).
4. Inform your physician about any other medications you are currently taking, including nonprescription drug, before you have this procedure.
Drug Interactions
Other drugs should not be admixed with iopamidol (see CONTRAINDICATIONS, and DOSAGE AND ADMINISTRATION, Drug Incompatibilities).
Drug/Laboratory Test Interactions
The results of PBI and radioactive iodine uptake studies, which depend on iodine estimations, will not accurately reflect thyroid function for up to 16 days following administration of iodinated contrast media. However, thyroid function tests not depending on iodine estimations, e.g., T3 resin uptake and total or free thyroxine (T4) assays are not affected. Any test which might be affected by contrast media should be performed prior to administration of the contrast medium.
Laboratory Test Findings
Carcinogenesis, Mutagenesis, Impairment of Fertility
Pregnancy: Teratogenic Effects
Pregnancy Category B
Nursing Mothers
Pediatric Use
Adverse Reaction
The most frequently reported adverse reactions
following intrathecal administration of iopamidol are headache, nausea,
vomiting, and musculoskeletal pain. These reactions usually occur 1 to
10 hours after injection, almost all occurring within 24 hours. They
are usually mild to moderate in degree, lasting for a few hours and
usually disappearing within 24 hours. Rarely, headaches may be severe
or persist for days. Headache is often accompanied by nausea and
vomiting, and tends to be more frequent and persistent in patients not
optimally hydrated. Backache, neck stiffness, numbness and
paresthesias, leg or sciatic-type pain occurred less frequently, often
in the form of a transient exacerbation of preexisting symptomatology.
Transient alterations in vital signs may occur and their significance
must be assessed on an individual basis.
The following table of incidence of reactions is based on clinical studies with ISOVUE-M (lopamidol Injection) in about 686 patients.
|
|
Estimated Overall Incidence |
|
| System |
Greater than 1% |
less than or Equal to 1% |
| Body as a Whole |
headache (16.4%) |
pyrexia |
|
|
|
muscle weakness |
|
|
|
hot flashes |
|
|
|
malaise |
|
|
|
fatigue |
|
|
|
weakness |
| Digestive |
nausea (7.3%) |
diarrhea |
|
|
vomiting (3.6%) |
heartburn |
| Musculoskeletal |
back pain (2.2%) |
leg cramps |
|
|
leg pain (1.4%) |
sciatica |
|
|
neck pain (1.1%) |
cervicobrachial irritation |
|
|
|
meningeal irritation |
|
|
|
radicular irritation |
|
|
|
lumbosacral |
|
|
|
other musculoskeletal |
|
|
|
pain |
|
|
|
involuntary movement |
|
|
|
burning sensation |
| Cardiovascular |
hypotension (1.1%) |
tachycardia |
|
|
|
hypertension |
|
|
|
chest pain |
| Nervous |
none |
emotional stress |
|
|
|
dizziness |
|
|
|
paresthesia |
|
|
|
confusion |
|
|
|
hallucinations |
|
|
|
lightheadedness |
|
|
|
syncope |
|
|
|
numbness |
|
|
|
cold extremities |
|
|
|
ataxia |
|
|
|
irritability |
| Urogenital |
none |
urinary retention |
| Respiratory |
none |
dyspnea |
| Skin and Appendages |
none |
rash |
| Miscellaneous |
none |
injection site pain |
|
|
|
|
General Adverse Reactions To Contrast Media
PRECAUTIONS-GENERAL
Cardiovascular:
Digestive:
Nervous:
Respiratory:
Skin and Appendages:
Urogenital:
Special Senses:
Overdosage
A dose of 3000 mgl in adults and 2400 mgl in children is sufficient for
most myelographic procedures. Doses above these levels may result in
an increased frequency and severity of adverse reactions including
seizures. However, in myelography, even use of a recommended dose can
produce mental aberrations tantamount to overdosage, if incorrect
management of the patient during or immediately following the procedure
permits inadvertent early intracranial entry of a large portion of the
medium.
Treatment of an overdose of an injectiable radiopaque
contrast medium is directed toward the support of all vital functions,
and prompt institution of symptomatic therapy.
Dosage and Administration
In adults a solution that is approximately isotonic (ISOVUE-M 200) is recommended for examination of the lumbar region. For movement of the contrast medium to distant target areas the more concentrated ISOVUE-M 300 preparation should be used to compensate for dilution of ISOVUE-M (lopamidol Injection) with cerebrospinal fluid.
The usual recommended adult dose range for iopamidol is 2000-3000 mg iodine. Iopamidol formulated to contain more than 300 mgl/ml should not be used intrathecally in adults. The minimum dose needed to perform a procedure should always be used.
In pediatric patients, a solution that is approximately isotonic (ISOVUE-M 200) is recommended for all intrathecal procedures. In children, loss of contrast due to mixing on movement of the medium is less apt to occur because of their shorter spinal cord.
The usual recommended pediatric dose range for iopamidol is 1400-2400 mg iodine. Iopamidol formulated to contain more than 200 mgl/ml should not be used. See pediatric dosage table for recommended dosage.
Anesthesia is not necessary. However, young children may require general anesthesia for technical reasons. Premedication with sedatives or tranquillizers is usually not needed. In patients with a history of seizure activity who are on anticonvulsant therapy, premedication with barbiturates or phenytoin should be considered.
Lumbar puncture is usually made between L3 and L4; if pathology is suspected at this level, the interspace immediately above or below may be selected. A lateral cervical puncture may also be used.
Rate of Injection: To avoid excessive mixing with cerebrospinal fluid and consequent loss of contrast as well as premature cephalad dispersion, injection must be made slowly over one to two minutes; the needle may
then be removed.
An interval of at least 48 hours should be allowed before repeat examination; however, whenever possible five to seven days is
recommended.
As with all radiopaque contrast agents, only the lowest dose of ISOVUE-M necessary to obtain adequate visualization should be used. A lower dose reduces the possibility of an adverse reaction. Most procedures do not require use of either a maximum dose or the highest available concentration of ISOVUE-M; the combination of dose and ISOVUE-M concentration to be used should be carefully individualized, and factors such as age, body size, anticipated pathology and degree and extent of opacification required, structure(s) or area to be examined, disease processes affecting the patient, and equipment and technique to be employed should be considered. Following are the usual recommended pediatric and adult doses of ISOVUE-M.
The pediatric doses listed below, intended as a guideline, are based on age rather than weight because the brain and CSF capacity is independent of weight. Variations will depend on such factors as height, suspected pathology, the patient's condition, technique used, etc. (e.g. CT or standard radiology or movement of the contrast media directed distal to the sit of injection).
|
|
|
Usual |
|
|
Age |
Recommended |
| Procedure |
Years |
Dose (mL) |
| Lumbar, thoracic myelogram |
2-7 |
7-9 |
|
|
8-12 |
8-11 |
|
|
13-18 |
10-12 |
|
|
|
|
|
|
|
|
|
|
|
Usual |
|
|
Concentration |
Recommended |
|
|
of Solution |
Dose |
|
|
(mgl/mL) |
(mL) |
| Lumbar myelogram |
200 |
10 to 15 |
| Thoracic myelogram |
200 |
10 to 15 |
| Cervical myelogram |
200 |
10 to 15 |
| (via lumbar injection) |
300 |
10 |
| Cervical myelogram |
200 |
10 |
| (via lateral cervical injection) |
|
|
| Total columnar myelography |
300 |
10 |
| CT cisternography |
200 |
4 to 6 |
| (via lumbar injection) |
|
|
Suggestions for Usual Patient Management
Preprocedure
WARNINGS
During Procedure
Post procedure
WARNINGS
Drug Incompatibilities
How Supplied
ISOVUE-M 200 (Iopamidol Injection 41%)
Ten 10mL single dose vials (NDC 0270-1411-11)
Ten 20mL single dose vials (NDC 0270-1411-25)
ISOVUE-M 300 (Iopamidol Injection 61%)
Ten 15mL single dose vials (NDC 270-1412-15)
Storage
Sample Outer Label
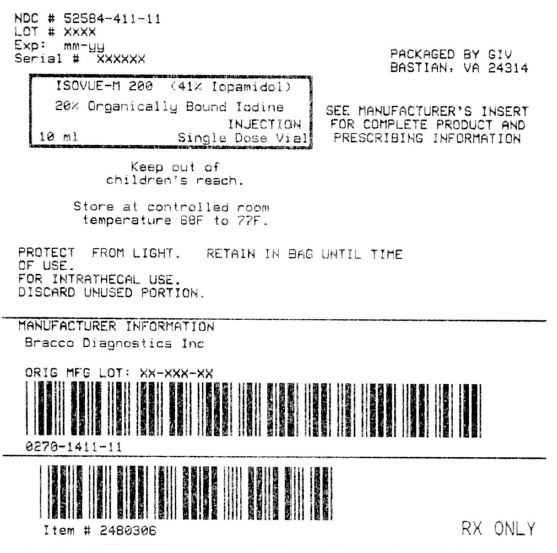
ISOVUE-M 200Iopamidol INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||