Geodon
Lake Erie Medical DBA Quality Care Products LLC
Geodon 20 mg
FULL PRESCRIBING INFORMATION
GEODON is available as capsules (ziprasidone hydrochloride) for oral administration and as an injection (ziprasidone mesylate) for intramuscular use only. Ziprasidone is a psychotropic agent that is chemically unrelated to phenothiazine or butyrophenone antipsychotic agents. It has a molecular weight of 412.94 (free base), with the following chemical name: 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-2H-indol-2-one. The empirical formula of C21H21ClN4OS (free base of ziprasidone) represents the following structural formula:
GEODON Capsules contain a monohydrochloride, monohydrate salt of ziprasidone. Chemically, ziprasidone hydrochloride monohydrate is 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-2H-indol-2-one, monohydrochloride, monohydrate. The empirical formula is C21H21ClN4OS • HCl • H2O and its molecular weight is 467.42. Ziprasidone hydrochloride monohydrate is a white to slightly pink powder.
GEODON Capsules are supplied for oral administration in 20 mg (blue/white), 40 mg (blue/blue), 60 mg (white/white), and 80 mg (blue/white) capsules. GEODON Capsules contain ziprasidone hydrochloride monohydrate, lactose, pregelatinized starch, and magnesium stearate.
GEODON for Injection contains a lyophilized form of ziprasidone mesylate trihydrate. Chemically, ziprasidone mesylate trihydrate is 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-2H-indol-2-one, methanesulfonate, trihydrate. The empirical formula is C21H21ClN4OS • CH3SO3H • 3H2O and its molecular weight is 563.09.
[See Dosage and Administration (2.3)].The mechanism of action of ziprasidone, as with other drugs having efficacy in schizophrenia, is unknown. However, it has been proposed that this drug's efficacy in schizophrenia is mediated through a combination of dopamine type 2 (D2) and serotonin type 2 (5HT2) antagonism. As with other drugs having efficacy in bipolar disorder, the mechanism of action of ziprasidone in bipolar disorder is unknown.
Ziprasidone exhibited high in vitro binding affinity for the dopamine D2 and D3, the serotonin 5HT2A, 5HT2C, 5HT1A, 5HT1D, and α1-adrenergic receptors (Ki s of 4.8, 7.2, 0.4, 1.3, 3.4, 2, and 10 nM, respectively), and moderate affinity for the histamine H1 receptor (Ki=47 nM). Ziprasidone functioned as an antagonist at the D2, 5HT2A, and 5HT1D receptors, and as an agonist at the 5HT1A receptor. Ziprasidone inhibited synaptic reuptake of serotonin and norepinephrine. No appreciable affinity was exhibited for other receptor/binding sites tested, including the cholinergic muscarinic receptor (IC50 greather than 1 µM). Antagonism at receptors other than dopamine and 5HT2 with similar receptor affinities may explain some of the other therapeutic and side effects of ziprasidone. Ziprasidone's antagonism of histamine H1 receptors may explain the somnolence observed with this drug. Ziprasidone's antagonism of α1-adrenergic receptors may explain the orthostatic hypotension observed with this drug.
Oral Pharmacokinetics
Ziprasidone's activity is primarily due to the parent drug. The multiple-dose pharmacokinetics of ziprasidone are dose-proportional within the proposed clinical dose range, and ziprasidone accumulation is predictable with multiple dosing. Elimination of ziprasidone is mainly via hepatic metabolism with a mean terminal half-life of about 7 hours within the proposed clinical dose range. Steady-state concentrations are achieved within one to three days of dosing. The mean apparent systemic clearance is 7.5 mL/min/kg. Ziprasidone is unlikely to interfere with the metabolism of drugs metabolized by cytochrome P450 enzymes.
Absorption: Ziprasidone is well absorbed after oral administration, reaching peak plasma concentrations in 6 to 8 hours. The absolute bioavailability of a 20 mg dose under fed conditions is approximately 60%. The absorption of ziprasidone is increased up to two-fold in the presence of food.
Distribution: Ziprasidone has a mean apparent volume of distribution of 1.5 L/kg. It is greater than 99% bound to plasma proteins, binding primarily to albumin and α1-acid glycoprotein. The in vitro plasma protein binding of ziprasidone was not altered by warfarin or propranolol, two highly protein-bound drugs, nor did ziprasidone alter the binding of these drugs in human plasma. Thus, the potential for drug interactions with ziprasidone due to displacement is minimal.
an drug. Ziprasidone is primarily cleared via three metabolic routes to yield four major circulating metabolites, benzisothiazole (BITP) sulphoxide, BITP-sulphone, ziprasidone sulphoxide, and S-methyl-dihydroziprasidone. Approximately 20% of the dose is excreted in the urine, with approximately 66% being eliminated in the feces. Unchanged anziprasidone represents about 44% of total drug-related material in serum. In vitro studies using human liver subcellular fractions indicate that S-methyl-dihydroziprasidone is generated in two steps. The data indicate that the reduction reaction is mediated by aldehyde oxidase and the subsequent methylation is mediated by thiol methyltransferase. In vitro studies using human liver microsomes and recombinant enzymes indicate that CYP3A4 is the major CYP contributing to the oxidative metabolism of ziprasidone. CYP1A2 may contribute to a much lesser extent. Based on in vivo abundance of excretory metabolites, less than one-third of ziprasidone metabolic clearance is mediated by cytochrome P450 catalyzed oxidation and approximately two-thirds via reduction by aldehyde oxidase. There are no known clinically relevant inhibitors or inducers of aldehyde oxidase.
Intramuscular Pharmacokinetics
Systemic Bioavailability: The bioavailability of ziprasidone administered intramuscularly is 100%. After intramuscular administration of single doses, peak serum concentrations typically occur at approximately 60 minutes post-dose or earlier and the mean half-life (T½) ranges from two to five hours. Exposure increases in a dose-related manner and following three days of intramuscular dosing, little accumulation is observed.
Metabolism and Elimination: Although the metabolism and elimination of IM ziprasidone have not been systematically evaluated, the intramuscular route of administration would not be expected to alter the metabolic pathways.
Uses
see Warnings and Precautions (5.2) [see Warnings and Precautions (5.2)]
Geodon is indicated for the treatment of schizophrenia. The
efficacy of oral ziprasidone was established in four short-term (4- and 6-week)
controlled trials of adult schizophrenic inpatients and in one maintenance trial
of stable adult schizophrenic inpatients [see Clinical Studies (14.1)].
Geodon is indicated as monotherapy for the acute treatment of manic or mixed episodes associated with bipolar I disorder. Efficacy was established in two 3-week monotherapy studies in adult patients. [see Clinical Studies (14.2)].
Geodon is indicated as an adjunct to lithium or valproate for the maintenance
treatment of bipolar I disorder. Efficacy was established in a maintenance trial
in adult patients. The efficacy of Geodon as monotherapy for the maintenance
treatment of bipolar I disorder has not been systematically evaluated in
controlled clinical trials. [see Clinical Studies (14.2)].
GEODON intramuscular is indicated for the treatment of acute agitation in schizophrenic patients for whom treatment with ziprasidone is appropriate and who need intramuscular antipsychotic medication for rapid control of agitation. The efficacy of intramuscular ziprasidone for acute agitation in schizophrenia was established in single day controlled trials of agitated schizophrenic inpatients. [see Clinical Trials (14.1)]
"Psychomotor agitation" is defined in DSM-IV as "excessive motor activity associated with a feeling of inner tension." Schizophrenic patients experiencing agitation often manifest behaviors that interfere with their diagnosis and care, e.g., threatening behaviors, escalating or urgently distressing behavior, or self-exhausting behavior, leading clinicians to the use of intramuscular antipsychotic medications to achieve immediate control of the agitation.
Since there is no experience regarding the safety of administering ziprasidone intramuscular to schizophrenic patients already taking oral ziprasidone, the practice of co-administration is not recommended.
Ziprasidone intramuscular is intended for intramuscular use only and should not be administered intravenously.
Because of ziprasidone's dose-related prolongation of the QT interval and the known association of fatal arrhythmias with QT prolongation by some other drugs, ziprasidone is contraindicated:
- in patients with a known history of QT prolongation (including congenital long QT syndrome)
- in patients with recent acute myocardial infarction
- in patients with uncompensated heart failure
Pharmacokinetic/pharmacodynamic studies between ziprasidone and other drugs that prolong the QT interval have not been performed. An additive effect of ziprasidone and other drugs that prolong the QT interval cannot be excluded. Therefore, ziprasidone should not be given with:
- dofetilide, sotalol, quinidine, other Class Ia and III anti-arrhythmics, mesoridazine, thioridazine, chlorpromazine, droperidol, pimozide, sparfloxacin, gatifloxacin, moxifloxacin, halofantrine, mefloquine, pentamidine, arsenic trioxide, levomethadyl acetate, dolasetron mesylate, probucol or tacrolimus.
- other drugs that have demonstrated QT prolongation as one of their pharmacodynamic effects and have this effect described in the full prescribing information as a contraindication or a boxed or bolded warning [see Warnings and Precautions (5.2)].
Ziprasidone is contraindicated in individuals with a known hypersensitivity to the product.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical trials for oral ziprasidone included approximately 5700 patients and/or normal subjects exposed to one or more doses of ziprasidone. Of these 5700, over 4800 were patients who participated in multiple-dose effectiveness trials, and their experience corresponded to approximately 1831 patient-years. These patients include: (1) 4331 patients who participated in multiple-dose trials, predominantly in schizophrenia, representing approximately 1698 patient-years of exposure as of February 5, 2000; and (2) 472 patients who participated in bipolar mania trials representing approximately 133 patient-years of exposure. An additional 127 patients with bipolar disorder participated in a long-term maintenance treatment study representing approximately 74.7 patient-years of exposure to ziprasidone. The conditions and duration of treatment with ziprasidone included open-label and double-blind studies, inpatient and outpatient studies, and short-term and longer-term exposure.
Clinical trials for intramuscular ziprasidone included 570 patients and/or normal subjects who received one or more injections of ziprasidone. Over 325 of these subjects participated in trials involving the administration of multiple doses.
Adverse reactions during exposure were obtained by collecting voluntarily reported adverse experiences, as well as results of physical examinations, vital signs, weights, laboratory analyses, ECGs, and results of ophthalmologic examinations.
The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation.
Adverse Findings Observed in Short-Term, Placebo-Controlled Trials with Oral Ziprasidone
The following findings are based on the short-term placebo-controlled premarketing trials for schizophrenia (a pool of two 6-week, and two 4-week fixed-dose trials) and bipolar mania (a pool of two 3-week flexible-dose trials) in which ziprasidone was administered in doses ranging from 10 to 200 mg/day.
Commonly Observed Adverse Reactions in Short Term-Placebo-Controlled Trials
The following adverse reactions were the most commonly observed adverse reactions associated with the use of ziprasidone (incidence of 5% or greater) and not observed at an equivalent incidence among placebo-treated patients (ziprasidone incidence at least twice that for placebo):
Schizophrenia trials (see Table 1 )
- Somnolence
- Respiratory Tract Infection
Bipolar trials (see Table 2)
- Somnolence
- Extrapyramidal Symptoms which includes the following adverse reaction terms: extrapyramidal syndrome, hypertonia, dystonia, dyskinesia, hypokinesia, tremor, paralysis and twitching. None of these adverse reactions occurred individually at an incidence greater than 10% in bipolar mania trials.
- Dizziness which includes the adverse reaction terms dizziness and lightheadedness.
- Akathisia
- Abnormal Vision
- Asthenia
- Vomiting
SCHIZOPHRENIA
Adverse Reactions Associated with Discontinuation of Treatment in Short-Term, Placebo-Controlled Trials of Oral Ziprasidone
Approximately 4.1% (29/702) of ziprasidone-treated patients in short-term, placebo-controlled studies discontinued treatment due to an adverse reaction, compared with about 2.2% (6/273) on placebo. The most common reaction associated with dropout was rash, including 7 dropouts for rash among ziprasidone patients (1%) compared to no placebo patients [See Warnings and Precautions (5.6)].
Adverse Reactions Occurring at an Incidence of 2% or More Among Ziprasidone-Treated Patients in Short-Term, Oral, Placebo-Controlled Trials
Table 1 enumerates the incidence, rounded to the nearest percent, of treatment-emergent adverse reactions that occurred during acute therapy (up to 6 weeks) in predominantly patients with schizophrenia, including only those reactions that occurred in 2% or more of patients treated with ziprasidone and for which the incidence in patients treated with ziprasidone was greater than the incidence in placebo-treated patients
In premarketing trials involving more than 5400 patients and/or normal subjects, accidental or intentional overdosage of oral ziprasidone was documented in 10 patients. All of these patients survived without sequelae. In the patient taking the largest confirmed amount, 3,240 mg, the only symptoms reported were minimal sedation, slurring of speech, and transitory hypertension (200/95).
Adverse reactions reported with ziprasidone overdose included extrapyramidal symptoms, somnolence, tremor, and anxiety. [see Adverse Reactions (6.2)]
Cardiovascular monitoring should commence immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of additive QT-prolonging effects that might be additive to those of ziprasidone.
Hypotension and circulatory collapse should be treated with appropriate measures such as intravenous fluids. If sympathomimetic agents are used for vascular support, epinephrine and dopamine should not be used, since beta stimulation combined with α1 antagonism associated with ziprasidone may worsen hypotension. Similarly, it is reasonable to expect that the alpha-adrenergic-blocking properties of bretylium might be additive to those of ziprasidone, resulting in problematic hypotension.
In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered. There is no specific antidote to ziprasidone, and it is not dialyzable. The possibility of multiple drug involvement should be considered. Close medical supervision and monitoring should continue until the patient recovers.
Dose Selection
Efficacy in schizophrenia was demonstrated in a dose range of 20 mg to 100 mg twice daily in short-term, placebo-controlled clinical trials. There were trends toward dose response within the range of 20 mg to 80 mg twice daily, but results were not consistent. An increase to a dose greater than 80 mg twice daily is not generally recommended. The safety of doses above 100 mg twice daily has not been systematically evaluated in clinical trials [see Clinical Studies (14.1)].
Maintenance Treatment
While there is no body of evidence available to answer the question of how long a patient treated with ziprasidone should remain on it, a maintenance study in patients who had been symptomatically stable and then randomized to continue ziprasidone or switch to placebo demonstrated a delay in time to relapse for patients receiving Geodon. [see Clinical Studies (14.1)]. No additional benefit was demonstrated for doses above 20 mg twice daily. Patients should be periodically reassessed to determine the need for maintenance treatment.
Acute Treatment of Manic or Mixed Episodes
Dose Selection--Oral ziprasidone should be administered at an initial daily dose of 40 mg twice daily with food. The dose may then be increased to 60 mg or 80 mg twice daily on the second day of treatment and subsequently adjusted on the basis of tolerance and efficacy within the range 40 mg–80 mg twice daily. In the flexible-dose clinical trials, the mean daily dose administered was approximately 120 mg [see Clinical Studies (14.2)].
Maintenance Treatment (as an adjunct to lithium or valproate)Continue treatment at the same dose on which the patient was initially stabilized, within the range of 40 mg–80 mg twice daily with food. Patients should be periodically reassessed to determine the need for maintenance treatment. [see Clinical Studies (14.2)]
Intramuscular Dosing
The recommended dose is 10 mg to 20 mg administered as required up to a maximum dose of 40 mg per day. Doses of 10 mg may be administered every two hours; doses of 20 mg may be administered every four hours up to a maximum of 40 mg/day. Intramuscular administration of ziprasidone for more than three consecutive days has not been studied.
If long-term therapy is indicated, oral ziprasidone hydrochloride capsules should replace the intramuscular administration as soon as possible.
Since there is no experience regarding the safety of administering ziprasidone intramuscular to schizophrenic patients already taking oral ziprasidone, the practice of co-administration is not recommended.
Ziprasidone intramuscular is intended for intramuscular use only and should not be administered intravenously
Intramuscular Preparation for Administration
GEODON for Injection (ziprasidone mesylate) should only be administered by intramuscular injection and should not be administered intravenously. Single-dose vials require reconstitution prior to administration.
Add 1.2 mL of Sterile Water for Injection to the vial and shake vigorously until all the drug is dissolved. Each mL of reconstituted solution contains 20 mg ziprasidone. To administer a 10 mg dose, draw up 0.5 mL of the reconstituted solution. To administer a 20 mg dose, draw up 1.0 mL of the reconstituted solution. Any unused portion should be discarded. Since no preservative or bacteriostatic agent is present in this product, aseptic technique must be used in preparation of the final solution. This medicinal product must not be mixed with other medicinal products or solvents other than Sterile Water for Injection. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Oral: Dosage adjustments are generally not required on the basis of age, gender, race, or renal or hepatic impairment. Geodon is not approved for use in children or adolescents.
Intramuscular: Ziprasidone intramuscular has not been systematically evaluated in elderly patients or in patients with hepatic or renal impairment. As the cyclodextrin excipient is cleared by renal filtration, ziprasidone intramuscular should be administered with caution to patients with impaired renal function. Dosing adjustments are not required on the basis of gender or race [see Use in Specific Populations (8)].
GEODON Capsules are differentiated by capsule color/size and are imprinted in black ink with "Pfizer" and a unique number. GEODON Capsules are supplied for oral administration in 20 mg (blue/white), 40 mg (blue/blue), 60 mg (white/white), and 80 mg (blue/white) capsules. They are supplied in the following strengths and package configurations:
GEODON for Injection is available in a single-dose vial as
ziprasidone mesylate (20 mg ziprasidone/mL when reconstituted according to label
instructions) [see Dosage and Administration
(2.3)]. Each mL of ziprasidone mesylate for injection (when
reconstituted) affords a colorless to pale pink solution that contains 20 mg of
ziprasidone and 4.7 mg of methanesulfonic acid solubilized by 294 mg of
sulfobutylether β-cyclodextrin sodium (SBECD).
See FDA-Approved Patient Labeling (17.3) .
Please refer to the patient package insert. To assure safe and effective use of GEODON, the information and instructions provided in the patient information should be discussed with patients.
Patients should be instructed to take GEODON Capsules with food for optimal absorption. The absorption of ziprasidone is increased up to two-fold in the presence of food [see Drug Interactions (7.8) and Clinical Pharmacology (12.3)].
Patients should be advised to inform their health care providers of the following: History of QT prolongation; recent acute myocardial infarction; uncompensated heart failure; prescription of other drugs that have demonstrated QT prolongation; risk for significant electrolyte abnormalities; and history of cardiac arrhythmia [see Contraindications (4.1) and Warnings and Precautions (5.2)].
Patients should be instructed to report the onset of any conditions that put them at risk for significant electrolyte disturbances, hypokalemia in particular, including but not limited to the initiation of diuretic therapy or prolonged diarrhea. In addition, patients should be instructed to report symptoms such as dizziness, palpitations, or syncope to the prescriber [see Warnings and Precautions (5.2)].
PATIENT SUMMARY OF INFORMATION ABOUT
GEODON® Capsules
(ziprasidone
HCl)
Information for patients taking GEODON or their caregivers
This summary contains important information about GEODON. It is not meant to take the place of your doctor's instructions. Read this information carefully before you take GEODON. Ask your doctor or pharmacist if you do not understand any of this information or if you want to know more about GEODON.
What Is GEODON?
GEODON is a type of prescription medicine called a psychotropic, also known as an atypical antipsychotic. GEODON can be used to treat symptoms of schizophrenia and acute manic or mixed episodes associated with bipolar disorder. GEODON can also be used as maintenance treatment of bipolar disorder when added to lithium or valproate.
Who Should Take GEODON?
Only your doctor can know if GEODON is right for you. GEODON may be prescribed for you if you have schizophrenia or bipolar disorder.
Symptoms of schizophrenia may include:
- hearing voices, seeing things, or sensing things that are not there (hallucinations)
- beliefs that are not true (delusions)
- unusual suspiciousness (paranoia)
- becoming withdrawn from family and friends
Symptoms of manic or mixed episodes of bipolar disorder may include:
- extremely high or irritable mood
- increased energy, activity, and restlessness
- racing thoughts or talking very fast
- easily distracted
- little need for sleep
If you show a response to GEODON, your symptoms may improve. If you continue to take GEODON there is less chance of your symptoms returning. Do not stop taking the capsules even when you feel better without first discussing it with your doctor.
It is also important to remember that GEODON capsules should be taken with food.
What is the most important safety information I should know about GEODON?
GEODON is not approved for the treatment of patients with dementia-related psychosis. Elderly patients with a diagnosis of psychosis related to dementia treated with antipsychotics are at an increased risk of death when compared to patients who are treated with placebo (a sugar pill).
GEODON is an effective drug to treat the symptoms of schizophrenia and the manic or mixed episodes of bipolar disorder. However, one potential side effect is that it may change the way the electrical current in your heart works more than some other drugs. The change is small and it is not known whether this will be harmful, but some other drugs that cause this kind of change have in rare cases caused dangerous heart rhythm abnormalities. Because of this, GEODON should be used only after your doctor has considered this risk for GEODON against the risks and benefits of other medications available for treating schizophrenia or bipolar manic and mixed episodes.
Your risk of dangerous changes in heart rhythm can be increased if you are taking certain other medicines and if you already have certain abnormal heart conditions. Therefore, it is important to tell your doctor about any other medicines that you take, including non-prescription medicines, supplements, and herbal medicines. You must also tell your doctor about any heart problems you have or have had.
Who should NOT take GEODON?
Elderly patients with a diagnosis of psychosis related to dementia. GEODON is not approved for the treatment of these patients.
Anything that can increase the chance of a heart rhythm abnormality should be avoided. Therefore, do not take GEODON if:
- You have certain heart diseases, for example, long QT syndrome, a recent heart attack, severe heart failure, or certain irregularities of heart rhythm (discuss the specifics with your doctor)
- You are currently taking medications that should not be taken in combination with ziprasidone, for example, dofetilide, sotalol, quinidine, other Class Ia and III anti-arrhythmics, mesoridazine, thioridazine, chlorpromazine, droperidol, pimozide, sparfloxacin, gatifloxacin, moxifloxacin, halofantrine, mefloquine, pentamidine, arsenic trioxide, levomethadyl acetate, dolasetron mesylate, probucol or tacrolimus.
What To Tell Your Doctor Before You Start GEODON
Only your doctor can decide if GEODON is right for you. Before you start GEODON, be sure to tell your doctor if you:
- have had any problem with the way your heart beats or any heart related illness or disease
- any family history of heart disease, including recent heart attack
- have had any problem with fainting or dizziness
- are taking or have recently taken any prescription medicines
- are taking any over-the-counter medicines you can buy without a prescription, including natural/herbal remedies
- have had any problems with your liver
- are pregnant, might be pregnant, or plan to get pregnant
- are breast feeding
- are allergic to any medicines
- have ever had an allergic reaction to ziprasidone or any of the other ingredients of GEODON capsules. Ask your doctor or pharmacist for a list of these ingredients
- have low levels of potassium or magnesium in your blood
Your doctor may want you to get additional laboratory tests to see if GEODON is an appropriate treatment for you.
GEODON And Other Medicines
There are some medications that may be unsafe to use when taking GEODON, and there are some medicines that can affect how well GEODON works. While you are on GEODON, check with your doctor before starting any new prescription or over-the-counter medications, including natural/herbal remedies.
How To Take GEODON
- Take GEODON only as directed by your doctor.
- Swallow the capsules whole.
- Take GEODON capsules with food.
- It is best to take GEODON at the same time each day.
- GEODON may take a few weeks to work. It is important to be patient.
- Do not change your dose or stop taking your medicine without your doctor's approval.
- Remember to keep taking your capsules, even when you feel better.
Possible Side Effects
Because these problems could mean you're having a heart rhythm abnormality, contact your doctor IMMEDIATELY if you:
- Faint or lose consciousness
- Feel a change in the way that your heart beats (palpitations)
Common side effects of GEODON include the following and should also be discussed with your doctor if they occur:
- Feeling unusually tired or sleepy
- Nausea or upset stomach
- Constipation
- Dizziness
- Restlessness
- Abnormal muscle movements, including tremor, shuffling, and uncontrolled involuntary movements
- Diarrhea
- Rash
- Increased cough / runny nose
If you develop any side effects that concern you, talk with your doctor. It is particularly important to tell your doctor if you have diarrhea, vomiting, or another illness that can cause you to lose fluids. Your doctor may want to check your blood to make sure that you have the right amount of important salts after such illnesses.
For a list of all side effects that have been reported, ask your doctor or pharmacist for the GEODON Professional Package Insert.
What To Do For An Overdose
In case of an overdose, call your doctor or poison control center right away or go to the nearest emergency room.
Other Important Safety Information
A serious condition called neuroleptic malignant syndrome (NMS) can occur with all antipsychotic medications including GEODON. Signs of NMS include very high fever, rigid muscles, shaking, confusion, sweating, or increased heart rate and blood pressure. NMS is a rare but serious side effect that could be fatal. Therefore, tell your doctor if you experience any of these signs.
Adverse reactions related to high blood sugar (hyperglycemia), sometimes serious, have been reported in patients treated with atypical antipsychotics. There have been few reports of hyperglycemia or diabetes in patients treated with GEODON, and it is not known if GEODON is associated with these reactions. Patients treated with an atypical antipsychotic should be monitored for symptoms of hyperglycemia.
Dizziness caused by a drop in your blood pressure may occur with GEODON, especially when you first start taking this medication or when the dose is increased. If this happens, be careful not to stand up too quickly, and talk to your doctor about the problem.
Before taking GEODON, tell your doctor if you are pregnant or plan on becoming pregnant. It is advised that you don't breast feed an infant if you are taking GEODON.
Because GEODON can cause sleepiness, be careful when operating machinery or driving a motor vehicle.
Since medications of the same drug class as GEODON may interfere with the ability of the body to adjust to heat, it is best to avoid situations involving high temperature or humidity.
It is best to avoid consuming alcoholic beverages while taking GEODON.
Call your doctor immediately if you take more than the amount of GEODON prescribed by your doctor.
GEODON has not been shown to be safe or effective in the treatment of children and teenagers under the age of 18 years old.
Keep GEODON and all medicines out of the reach of children.
How To Store GEODON
Store GEODON capsules at room temperature (59°–86°F or 15°–30°C).
For More Information About GEODON
This sheet is only a summary. GEODON is a prescription medicine and only your doctor can decide if it is right for you. If you have any questions or want more information about GEODON, talk with your doctor or pharmacist. You can also visit www.geodon.com
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. GEODON (ziprasidone) is not approved for the treatment of patients with Dementia-Related Psychosis [see Warnings and Precautions (5.1)]).
Image of label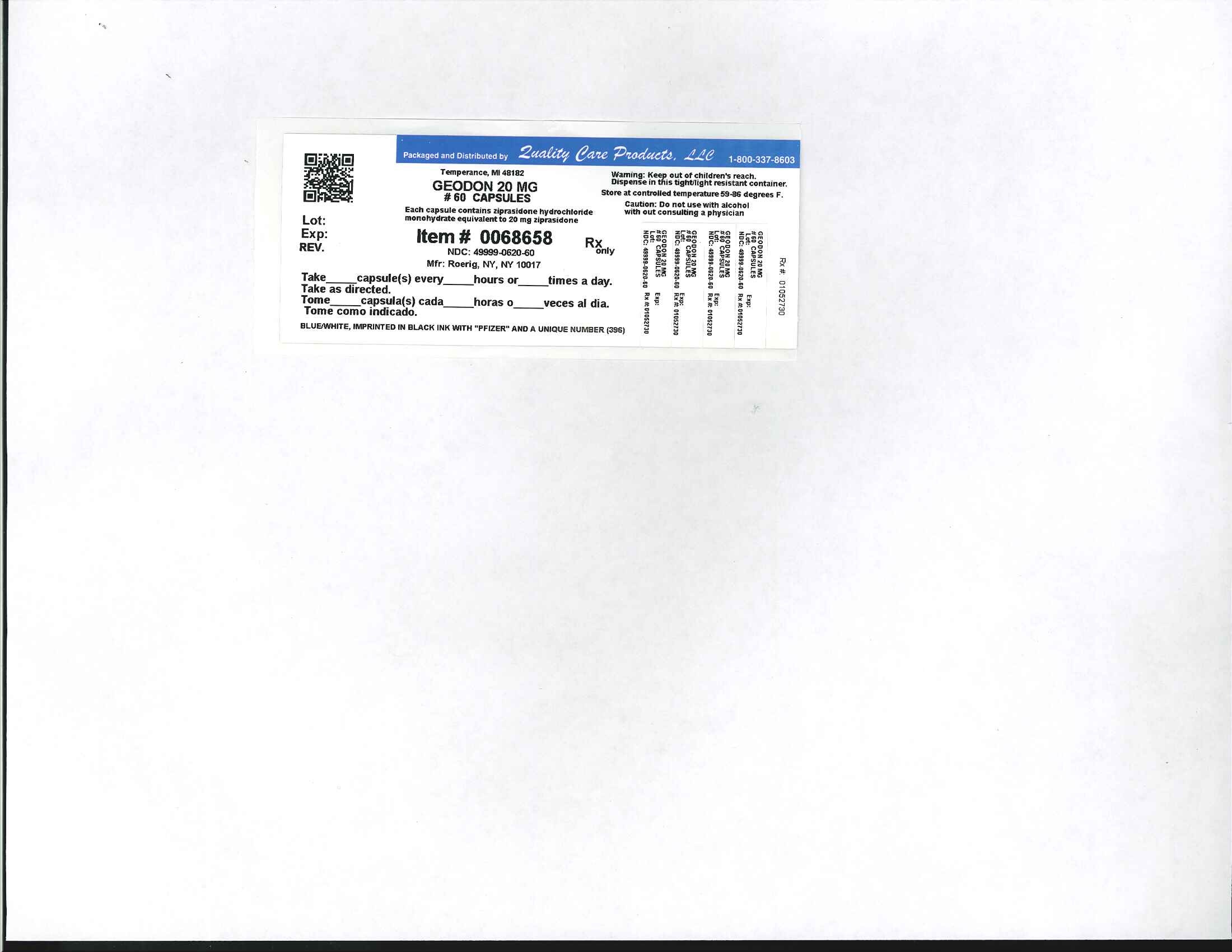
GeodonZiprasidone Hydrochloride Monohydrate CAPSULE
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||