FLUCONAZOLE
FULL PRESCRIBING INFORMATION: CONTENTS*
- FLUCONAZOLE DESCRIPTION
- CLINICAL PHARMACOLOGY
- DRUG INTERACTIONS
- MICROBIOLOGY
- INDICATIONS & USAGE
- CLINICAL STUDIES
- FLUCONAZOLE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- DRUG INTERACTIONS
- PREGNANCY
- NURSING MOTHERS
- PEDIATRIC USE
- GERIATRIC USE
- FLUCONAZOLE ADVERSE REACTIONS
- OVERDOSAGE
- DOSAGE & ADMINISTRATION
- HOW SUPPLIED
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
FULL PRESCRIBING INFORMATION
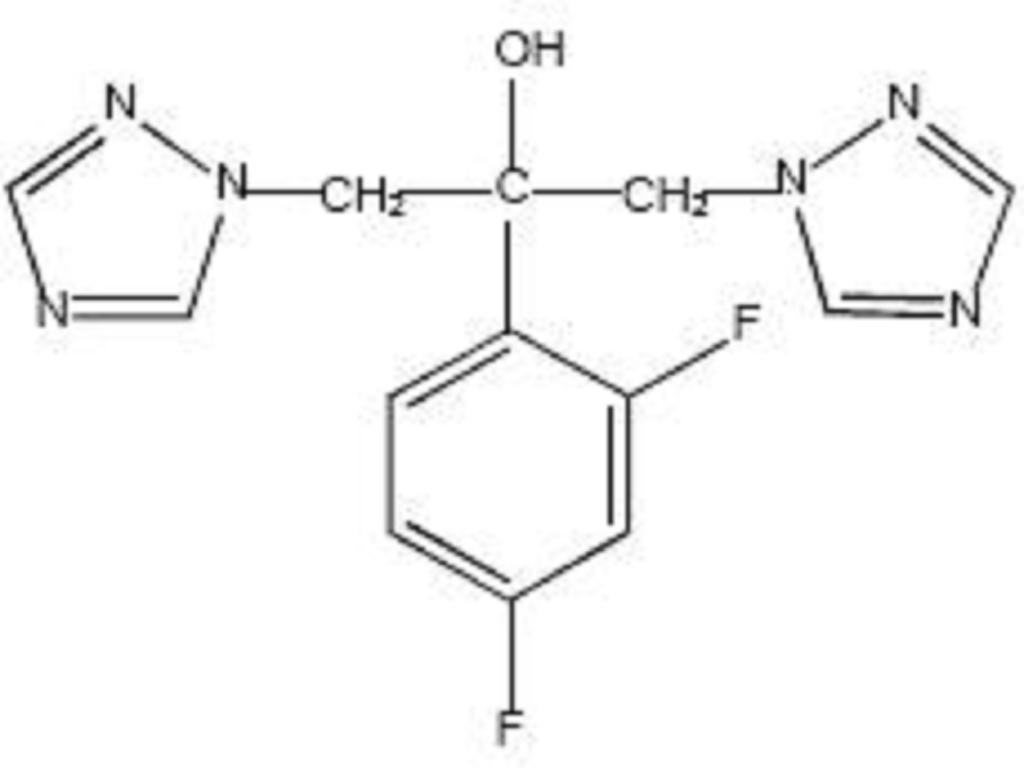
FLUCONAZOLE DESCRIPTION
CLINICAL PHARMACOLOGY
Fluconazole is a highly selective inhibitor of fungal cytochrome P-450 sterol C-14 alpha-demethylation. Mammalian cell demethylation is much less sensitive to fluconazole inhibition. The subsequent loss of normal sterols correlates with the accumulation of 14 alpha-methyl sterols in fungi and may be responsible for the fungistatic activity of fluconazole.
The pharmacokinetic properties of fluconazole are similar following administration by the intravenous or oral routes. In normal volunteers, the bioavailability of orally administered fluconazole is over 90% compared with intravenous administration. Bioequivalence was established between the 100 mg tablet and both suspension strengths when administered as a single 200 mg dose.
Peak plasma concentrations (Cmax) in fasted normal volunteers occur between 1 and 2 hours with a terminal plasma elimination half-life of approximately 30 hours (range: 20 to 50 hours) after oral administration.
In fasted normal volunteers, administration of a single oral 400 mg dose of fluconazole leads to a mean Cmax of 6.72 mcg/mL (range: 4.12 to 8.08 mcg/mL) and after single oral doses of 50 to 400 mg, fluconazole plasma concentrations and AUC (area under the plasma concentration-time curve) are dose proportional.
Administration of a single oral 150 mg tablet of fluconazole to ten lactating women resulted in a mean Cmax of 2.61 mcg/mL (range: 1.57 to 3.65 mcg/mL).
Steady-state concentrations are reached within 5 to 10 days following oral doses of 50 to 400 mg given once daily. Administration of a loading dose (on day 1) of twice the usual daily dose results in plasma concentrations close to steady-state by the second day. The apparent volume of distribution of fluconazole approximates that of total body water. Plasma protein binding is low (11 to 12%). Following either single- or multiple-oral doses for up to 14 days, fluconazole penetrates into all body fluids studied (see table below). In normal volunteers, saliva concentrations of fluconazole were equal to or slightly greater than plasma concentrations regardless of dose, route, or duration of dosing. In patients with bronchiectasis, sputum concentrations of fluconazole following a single 150 mg oral dose were equal to plasma concentrations at both 4 and 24 hours post dose. In patients with fungal meningitis, fluconazole concentrations in the CSF are approximately 80% of the corresponding plasma concentrations.
A single oral 150 mg dose of fluconazole administered to 27 patients penetrated into vaginal tissue, resulting in tissue: plasma ratios ranging from 0.94 to 1.14 over the first 48 hours following dosing.
A single oral 150 mg dose of fluconazole administered to 14 patients penetrated into vaginal fluid, resulting in fluid: plasma ratios ranging from 0.36 to 0.71 over the first 72 hours following dosing.
|
*Relative to concurrent concentrations in plasma in subjects with normal renal function. †Independent of degree of meningeal inflammation. |
|
| Tissue or Fluid | Ratio of Fluconazole Tissue (Fluid)/Plasma Concentration* |
| Cerebrospinal fluid† | 0.5 to 0.9 |
| Saliva | 1 |
| Sputum | 1 |
| Blister fluid | 1 |
| Urine | 10 |
| Normal Skin | 10 |
| Nails | 1 |
| Blister skin | 2 |
| Vaginal tissue | 1 |
| Vaginal fluid | 0.4 to 0.7 |
In normal volunteers, fluconazole is cleared primarily by renal excretion, with approximately 80% of the administered dose appearing in the urine as unchanged drug. About 11% of the dose is excreted in the urine as metabolites.
The pharmacokinetics of fluconazole are markedly affected by reduction in renal function. There is an inverse relationship between the elimination half-life and creatinine clearance. The dose of fluconazole may need to be reduced in patients with impaired renal function (see DOSAGE AND ADMINISTRATION). A 3-hour hemodialysis session decreases plasma concentrations by approximately 50%.
In normal volunteers, fluconazole administration (doses ranging from 200 mg to 400 mg once daily for up to 14 days) was associated with small and inconsistent effects on testosterone concentrations, endogenous corticosteroid concentrations, and the ACTH-stimulated cortisol response.
In children, the following pharmacokinetic data {Mean(%cv)} have been reported:
| Age Studied | Dose (mg/kg) | Clearance (mL/min/kg) | Half-life (Hours) | Cmax (mcg/mL) | Vdss (L/kg) |
| 9 Months to 13 years | Single-Oral 2 mg/kg | 0.40 (38%) N=14 | 25.0 | 2.9 (22%) N=16 | - |
| 9 Months to 13 years | Single-Oral 8 mg/kg | 0.51 (60%) N=15 | 19.5 | 9.8 (20%) N=15 | - |
| 5 to 15 years | Multiple IV 2 mg/kg | 0.49 (40%) N=4 | 17.4 | 5.5 (25%) N=5 | 0.722 (36%) N=4 |
| 5 to 15 years | Multiple IV 4 mg/kg | 0.59 (64%) N=5 | 15.2 | 11.4 (44%) N=6 | 0.729 (33%) N=5 |
| 5 to 15 years | Multiple IV 8 mg/kg | 0.66 (31%) N=7 | 17.6 | 14.1 (22%) N=8 | 1.069 (37%) N=7 |
Clearance corrected for body weight was not affected by age in these studies. Mean body clearance in adults is reported to be 0.23 (17%) mL/min/kg.
In premature newborns (gestational age 26 to 29 weeks), the mean (%cv) clearance within 36 hours of birth was 0.180 (35%, N=7) mL/min/kg, which increased with time to a mean of 0.218 (31%, N=9) mL/min/kg six days later and 0.333 (56%, N=4) mL/min/kg 12 days later. Similarly, the half-life was 73.6 hours, which decreased with time to a mean of 53.2 hours six days later and 46.6 hours 12 days later.
A pharmacokinetic study was conducted in 22 subjects, 65 years of age or older receiving a single 50 mg oral dose of fluconazole. Ten of these patients were concomitantly receiving diuretics. The Cmax was 1.54 mcg/mL and occurred at 1.3 hours post dose. The mean AUC was 76.4+ 20.3 mcg∙h/mL, and the mean terminal half-life was 46.2 hours. These pharmacokinetic parameter values are higher than analogous values reported for normal young male volunteers. Coadministration of diuretics did not significantly alter AUC or Cmax. In addition, creatinine clearance (74 mL/min), the percent of drug recovered unchanged in urine (0-24 hr, 22%) and the fluconazole renal clearance estimates (0.124 mL/min/kg) for the elderly were generally lower than those of younger volunteers. Thus, the alteration of fluconazole disposition in the elderly appears to be related to reduced renal function characteristic of this group. A plot of each subject’s terminal elimination half-life versus creatinine clearance compared with the predicted half-life – creatinine clearance curve derived from normal subjects and subjects with varying degrees of renal insufficiency indicated that 21 of 22 subjects fell within the 95% confidence limit of the predicted half-life – creatinine clearance curves. These results are consistent with the hypothesis that higher values for the pharmacokinetic parameters observed in the elderly subjects compared with normal young male volunteers are due to the decreased kidney function that is expected in the elderly.
DRUG INTERACTIONS
Oral contraceptives were administered as a single dose both before and after the oral administration of fluconazole 50 mg once daily for 10 days in 10 healthy women. There was no significant difference in ethinyl estradiol or levonorgestrel AUC after the administration of 50 mg of fluconazole. The mean increase in ethinyl estradiol AUC was 6% (range: -47 to 108%) and levonorgestrel AUC increased 17% (range: -33 to 141%).
In a second study, twenty-five normal females received daily doses of both 200 mg fluconazole tablets or placebo for two, ten-day periods. The treatment cycles were one month apart with all subjects receiving fluconazole during one cycle and placebo during the other. The order of study treatment was random. Single doses of an oral contraceptive tablet containing levonorgestrel and ethinyl estradiol were administered on the final treatment day (day 10) of both cycles. Following administration of 200 mg of fluconazole, the mean percentage increase of AUC for levonorgestrel compared to placebo was 25% (range: -12 to 82%) and the mean percentage increase for ethinyl estradiol compared to placebo was 38% (range: -11 to 101%). Both of these increases were statistically significantly different from placebo.
A third study evaluated the potential interaction of once weekly dosing of fluconazole 300 mg to 21 normal females taking an oral contraceptive containing ethinyl estradiol and norethindrone. In this placebo-controlled, double-blind, randomized, two-way crossover study carried out over three cycles of oral contraceptive treatment, fluconazole dosing resulting in small increases in the mean AUCs of ethinyl estradiol and norethindrone compared to similar placebo dosing. The mean AUCs of ethinyl estradiol and norethindrone increased by 24% (95% C.I. range 18-31%) and 13% (95% C.I. range 8-18%), respectively relative to placebo. Fluconazole treatment did not cause a decrease in the ethinyl estradiol AUC of any individual subject in this study compared to placebo dosing. The individual AUC individual values of norethindrone decreased very slightly (greater then 5%) in 3 of the 21 subjects after fluconazole treatment.
Fluconazole 100 mg was administered as a single oral dose alone and two hours after a single dose of cimetidine 400 mg to six healthy male volunteers. After the administration of cimetidine, there was a significant decrease in fluconazole AUC and Cmax. There was a mean ±SD decrease in fluconazole AUC of 13% ±11% (range: -3.4 to -31%) and Cmax decreased 19% ±14% (range: -5 to -40%). However, the administration of cimetidine 600 mg to 900 mg intravenously over a four-hour period (from one hour before to 3 hours after a single oral dose of fluconazole 200 mg) did not affect the bioavailability or pharmacokinetics of fluconazole in 24 healthy male volunteers.
Administration of calcium carbonate and magnesium carbonate (20 mL) to 14 normal male volunteers immediately prior to a single dose of fluconazole 100 mg had no affect on the absorption or elimination of fluconazole.
Concomitant oral administration of 100 mg fluconazole and 50 mg hydrochlorothiazide for 10 days in 13 normal volunteers resulted in a significant increase in fluconazole AUC and Cmax compared to fluconazole given alone. There was a mean ±SD increase in fluconazole AUC and Cmax of 45% ±31% (range: 19 to 114%) and 43% ±31% (range: 19 to 122%), respectively. These changes are attributed to a mean ±SD reduction in renal clearance of 30% ±12% (range: -10 to -50%).
Administration of a single oral 200 mg dose of fluconazole after 15 days of rifampin administered as 600 mg daily in eight healthy male volunteers resulted in a significant decrease in fluconazole AUC and a significant increase in apparent oral clearance of fluconazole. There was a mean ±SD reduction in fluconazole AUC of 23% ±9% (range: -13 to -42%). Apparent oral clearance of fluconazole increased 32% ±17% (range: 16 to 72%). Fluconazole half-life decreased from 33.4 ±4.4 hours to 26.8 ±3.9 hours (see PRECAUTIONS).
There was a significant increase in prothrombin time response (area under the prothrombin time-time curve) following a single dose of warfarin (15 mg) administered to 13 normal male volunteers following oral fluconazole 200 mg administered daily for 14 days as compared to the administration of warfarin alone. There was a mean ±SD increase in the prothrombin time response (area under the prothrombin time-time curve) of 7% ±4% (range: -2 to 13%) (see PRECAUTIONS). Mean is based on data from 12 subjects as one of 13 subjects experienced a 2-fold increase in his prothrombin time response.
Phenytoin AUC was determined after 4 days of phenytoin dosing (200 mg daily, orally for 3 days followed by 250 mg intravenously for one dose) both with and without the administration of fluconazole (oral fluconazole 200 mg daily for 16 days) in 10 normal male volunteers. There was a significant increase in phenytoin AUC. The mean ±SD increase in phenytoin AUC was 88% ±68% (range: 16 to 247%). The absolute magnitude of this interaction is unknown because of the intrinsically nonlinear disposition of phenytoin (see PRECAUTIONS).
Cyclosporine AUC and Cmax were determined before and after the administration of fluconazole 200 mg daily for 14 days in eight renal transplant patients who had been on cyclosporine therapy for at least 6 months and on a stable cyclosporine dose for at least 6 weeks. There was a significant increase in cyclosporine AUC, Cmax, Cmin (24-hour concentration), and a significant reduction in apparent oral clearance following the administration of fluconazole. The mean ±SD increase in AUC was 92% ±43% (range: 18 to 147%). The Cmax increased 60% ±48% (range: -5 to 133%). The Cmin increased 157% ±96% (range: 33 to 360%). The apparent oral clearance decreased 45% ±15% (range: -15 to -60%) (see PRECAUTIONS).
Plasma zidovudine concentrations were determined on two occasions (before and following fluconazole 200 mg daily for 15 days) in 13 volunteers with AIDS or ARC who were on a stable zidovudine dose for at least two weeks. There was a significant increase in zidovudine AUC following the administration of fluconazole. The mean ±SD increase in AUC was 20% ±32% (range: -27 to 104%). The metabolite, GZDV, to parent drug ratio significantly decreased after the administration of fluconazole, from 7.6 ±3.6 to 5.7 ±2.2.
The pharmacokinetics of theophylline were determined from a single intravenous dose of aminophylline (6 mg/kg) before and after the oral administration of fluconazole 200 mg daily for 14 days in 16 normal male volunteers. There were significant increases in theophylline AUC, Cmax, and half-life with a corresponding decrease in clearance. The mean ±SD theophylline AUC increased 21% ±16% (range: -5 to 48%). The Cmax increased 13% ±17% (range: -13 to 40%). Theophylline clearance decreased 16% ±11% (range: -32 to 5%). The half-life of theophylline increased from 6.6 ±1.7 hours to 7.9 ±1.5 hours (see PRECAUTIONS).
Six healthy volunteers received terfenadine 60 mg BID for 15 days. Fluconazole 200 mg was administered daily from days 9 through 15. Fluconazole did not affect terfenadine plasma concentrations. Terfenadine acid metabolite AUC increased 36% ±36% (range: 7 to 102%) from day 8 to day 15 with the concomitant administration of fluconazole. There was no change in cardiac repolarization as measured by Holter QTc intervals. Another study at a 400 mg and 800 mg daily dose of fluconazole demonstrated that fluconazole taken in doses of 400 mg per day or greater significantly increases plasma levels of terfenadine when taken concomitantly (see CONTRAINDICATIONS and PRECAUTIONS).
The effects of fluconazole on the pharmacokinetics of the sulfonylurea oral hypoglycemic agents tolbutamide, glipizide, and glyburide were evaluated in three placebo-controlled studies in normal volunteers. All subjects received the sulfonylurea alone as a single dose and again as a single dose following the administration of fluconazole 100 mg daily for 7 days. In these three studies 22/46 (47.8%) of fluconazole treated patients and 9/22 (40.1%) of placebo treated patients experienced symptoms consistent with hypoglycemia (see PRECAUTIONS).
In 13 normal male volunteers, there was significant increase in tolbutamide (500 mg single dose) AUC and Cmax following the administration of fluconazole. There was a mean ±SD increase in tolbutamide AUC of 26% ±9% (range: 12 to 39%). Tolbutamide Cmax increased 11% ±9% (range: -6 to 27%) (see PRECAUTIONS).
The AUC and Cmax of glipizide (2.5 mg single dose) were significantly increased following the administration of fluconazole in 13 normal male volunteers. There was a mean ±SD increase in AUC of 49% ±13% (range: 27 to 73%) and an increase in Cmax of 19% ±23% (range: -11 to 79%) (see PRECAUTIONS).
The AUC and Cmax of glyburide (5 mg single dose) were significantly increased following the administration of fluconazole in 20 normal male volunteers. There was a mean ±SD increase in AUC of 44% ±29% (range: -13 to 115%) and Cmax increased 19% ±19% (range: -23 to 62%). Five subjects required oral glucose following the ingestion of glyburide after 7 days of fluconazole administration (see PRECAUTIONS).
There have been published reports that an interaction exists when fluconazole is administered concomitantly with rifabutin, leading to increased serum levels of rifabutin (see PRECAUTIONS).
There have been published reports that an interaction exists when fluconazole is administered concomitantly with tacrolimus, leading to increased serum levels of tacrolimus (see PRECAUTIONS).
A placebo-controlled, randomized, multiple-dose study examined the potential interaction of fluconazole with cisapride. Two groups of 10 normal subjects were administered fluconazole 200 mg daily or placebo. Cisapride 20 mg four times daily was started after 7 days of fluconazole or placebo dosing. Following a single dose of fluconazole, there was a 101% increase in the cisapride AUC and a 91% increase in the cisapride Cmax. Following multiple doses of fluconazole, there was a 192% increase in the cisapride AUC and a 154% increase in the cisapride Cmax. Fluconazole significantly increased the QTc interval in subjects receiving cisapride 20 mg four times daily for 5 days. (See CONTRAINDICATIONS and PRECAUTIONS.)
The effect of fluconazole on the pharmacokinetics and pharmacodynamics of midazolam was examined in a randomized, cross-over study in 12 volunteers. In the study, subjects ingested placebo or 400 mg fluconazole on Day 1 followed by 200 mg daily from Day 2 to Day 6. In addition, a 7.5 mg dose of midazolam was orally ingested on the first day, 0.05 mg/kg was administered intravenously on the fourth day, and 7.5 mg orally on the sixth day. Fluconazole reduced the clearance of IV midazolam by 51%. On the first day of dosing, fluconazole increased the midazolam AUC and Cmax by 259% and 150%, respectively. On the sixth day of dosing, fluconazole increased the midazolam AUC and Cmax by 259% and 74%, respectively. The psychomotor effects of midazolam were significantly increased after oral administration of midazolam but not significantly affected following intravenous midazolam.
A second randomized, double-dummy, placebo-controlled, cross-over study in three phases was performed to determine the effect of route of administration of fluconazole on the interaction between fluconazole and midazolam. In each phase the subjects were given oral fluconazole 400 mg and intravenous saline; oral placebo and intravenous fluconazole 400 mg; and oral placebo and IV saline. An oral dose of 7.5 mg of midazolam was ingested after fluconazole/placebo. The AUC and Cmax of midazolam were significantly higher after oral than IV administration of fluconazole. Oral fluconazole increased the midazolam AUC and Cmax by 272% and 129%, respectively. IV fluconazole increased the midazolam AUC and Cmax by 244% and 79%, respectively. Both oral and IV fluconazole increased the pharmacodynamic effects of midazolam. (See PRECAUTIONS.)
An open-label, randomized, three-way crossover study in 18 healthy subjects assessed the effect of a single 800 mg oral dose of fluconazole on the pharmacokinetics of a single 1200 mg oral dose of azithromycin as well as the effects of azithromycin on the pharmacokinetics of fluconazole. There was no significant pharmacokinetic interaction between fluconazole and azithromycin.
MICROBIOLOGY
Fluconazole exhibits in vitro activity against Cryptococcus neoformans and Candida spp. Fungistatic activity has also been demonstrated in normal and immunocompromised animal models for systemic and intracranial fungal infections due to Cryptococcus neoformans and for systemic infections due to Candida albicans.
In common with other azole antifungal agents, most fungi show a higher apparent sensitivity to fluconazole in vivo than in vitro. Fluconazole administered orally and/or intravenously was active in a variety of animal models of fungal infection using standard laboratory strains of fungi. Activity has been demonstrated against fungal infections caused by Aspergillus flavus and Aspergillus fumigatus in normal mice. Fluconazole has also been shown to be active in animal models of endemic mycoses, including one model of Blastomyces dermatitidis pulmonary infections in normal mice; one model of Coccidioides immitis intracranial infections in normal mice; and several models of Histoplasma capsulatum pulmonary infection in normal and immunosuppressed mice. The clinical significance of results obtained in these studies is unknown.
Oral fluconazole has been shown to be active in an animal model of vaginal candidiasis.
Concurrent administration of fluconazole and amphotericin B in infected normal and immunosuppressed mice showed the following results: a small additive antifungal effect in systemic infection with C. albicans, no interaction in intracranial infection with Cr. neoformans, and antagonism of the two drugs in systemic infection with Asp. fumigatus. The clinical significance of results obtained in these studies is unknown.
There have been reports of cases of superinfection with Candida species other than C. albicans, which are often inherently not susceptible to fluconazole (e.g., Candida krusei). Such cases may require alternative antifungal therapy.
INDICATIONS & USAGE
Fluconazole tablets are indicated for the treatment of:
- Vaginal candidiasis (vaginal yeast infections due to Candida).
- Oropharyngeal and esophageal candidiasis. In open noncomparative studies of relatively small numbers of patients, fluconazole was also effective for the treatment of Candida urinary tract infections, peritonitis, and systemic Candida infections including candidemia, disseminated candidiasis, and pneumonia.
- Cryptococcal meningitis. Before prescribing fluconazole for AIDS patients with cryptococcal meningitis, please see Clinical Studies. Studies comparing fluconazole to amphotericin B in non-HIV infected patients have not been conducted.
Fluconazole tablets are also indicated to decrease the incidence of candidiasis in patients undergoing bone marrow transplantation who receive cytotoxic chemotherapy and/or radiation therapy.
Specimens for fungal culture and other relevant laboratory studies (serology, histopathology) should be obtained prior to therapy to isolate and identify causative organisms. Therapy may be instituted before the results of the cultures and other laboratory studies are known; however, once these results become available, anti-infective therapy should be adjusted accordingly
CLINICAL STUDIES
In a multicenter study comparing fluconazole (200 mg/day) to amphotericin B (0.3 mg/kg/day) for treatment of cryptococcal meningitis in patients with AIDS, a multivariate analysis revealed three pretreatment factors that predicted death during the course of therapy: abnormal mental status, cerebrospinal fluid cryptococcal antigen titer greater than 1:1024, and cerebrospinal fluid white blood cell count of less than 20 cells/mm3. Mortality among high risk patients was 33% and 40% for amphotericin B and fluconazole patients, respectively (p=0.58), with overall deaths 14% (9 of 63 subjects) and 18% (24 of 131 subjects) for the 2 arms of study (p=0.48). Optimal doses and regimens for patients with acute cryptococcal meningitis and at high risk for treatment failure remain to be determined. (Saag, et al. N Engl J Med 1992; 326:83-9.)
Two adequate and well-controlled studies were conducted in the U.S. using the 150 mg tablet. In both, the results of the fluconazole regimen were comparable to the control regimen (clotrimazole or miconazole intravaginally for 7 days) both clinically and statistically at the one month post-treatment evaluation.
The therapeutic cure rate, defined as a complete resolution of signs and symptoms of vaginal candidiasis (clinical cure), along with a negative KOH examination and negative culture for Candida (microbiologic eradication), was 55% in both the fluconazole group and the vaginal products group.
| Fluconazole PO 150 mg tablet | Vaginal Product qhs x 7 days | |
| Enrolled | 448 | 422 |
| Evaluable at late follow-up | 347 (77%) | 327 (77%) |
| Clinical cure | 239/347 (69%) | 235/327 (72%) |
| Mycologic erad. | 213/347 (61%) | 196/327 (60%) |
| Therapeutic cure | 190/347 (55%) | 179/327 (55%) |
Approximately three-fourths of the enrolled patients had acute vaginitis (greater then 4 episodes/12 months) and achieved 80% clinical cute, 67% mycologic eradication and 59% therapeutic cure when treated with a 150 mg fluconazole tablet administered orally. These rates were comparable to control products. The remaining one-fourth of enrolled patients had recurrent vaginitis (less then 4 episodes/12 months) and achieved 57% clinical cure, 47% mycologic eradication and 40% therapeutic cure. The numbers are too small to make meaningful clinical or statistical comparisons with vaginal products in the treatment of patients with recurrent vaginitis.
Substantially more gastrointestinal events were reported in the fluconazole group compared to the vaginal product group. Most of the events were mild to moderate. Because fluconazole was given as a single dose, no discontinuations occurred.
| Parameter | Fluconazole PO | Vaginal Products |
| Evaluable patients | 448 | 422 |
| With any adverse event | 141 (31%) | 112 (27%) |
| Nervous system | 90 (20%) | 69 (16%) |
| Gastrointestinal | 73 (16%) | 18 (4%) |
| With drug-related event | 117 (26%) | 67 (16%) |
| Nervous system | 61 (14%) | 29 (7%) |
| Headache | 58 (13%) | 28 (7%) |
| Gastrointestinal | 68 (15%) | 13 (3%) |
| Abdominal pain | 25 (6%) | 7 (2%) |
| Nausea | 30 (7%) | 3 (1%) |
| Diarrhea | 12 (3%) | 2 (greater then 1%) |
| Application site event | 0 (0%) | 19 (5%) |
| Taste perversion | 6 (1%) | 0 (0%) |
An open-label, comparative study of the efficacy and safety of fluconazole (2 to 3 mg/kg/day) and oral nystatin (400,000 I.U. 4 times daily) in immunocompromised children with oropharyngeal candidiasis was conducted. Clinical and mycological response rates were higher in the children treated with fluconazole.
Clinical cure at the end of treatment was reported for 86% of fluconazole treated patients compared to 46% of nystatin treated patients. Mycologically, 76% of fluconazole treated patients had the infecting organism eradicated compared to 11% for nystatin treated patients.
|
*Subjects without follow-up cultures for any reason were considered nonevaluable for mycological response. |
||
| Fluconazole | Nystatin | |
| Enrolled | 96 | 90 |
| Clinical cure | 76/88 (86%) | 36/78 (46%) |
| Mycological eradication* | 55/72 (76%) | 6/54 (11%) |
The proportion of patients with clinical relapse 2 weeks after the end of treatment was 14% for subjects receiving fluconazole and 16% for subjects receiving nystatin. At 4 weeks after the end of treatment the percentages of patients with clinical relapse were 22% for fluconazole and 23% for nystatin.
FLUCONAZOLE CONTRAINDICATIONS
CLINICAL PHARMACOLOGY, Drug Interaction StudiesPRECAUTIONS
WARNINGS
1. Hepatic Injury
Fluconazole has been associated with rare cases of serious hepatic toxicity, including fatalities primarily in patients with serious underlying medical conditions. In cases of fluconazole-associated hepatotoxicity, no obvious relationship to total daily dose, duration of therapy, sex or age of the patient has been observed.
Fluconazole hepatotoxicity has usually, but not always, been reversible on discontinuation of therapy. Patients who develop abnormal liver function tests during fluconazole therapy should be monitored for the development of more severe hepatic injury. Fluconazole should be discontinued if clinical signs and symptoms consistent with liver disease develop that may be attributable to fluconazole.
2. Anaphylaxis
In rare cases, anaphylaxis has been reported.
3. Dermatologic
Patients have rarely developed exfoliative skin disorders during treatment with fluconazole. In patients with serious underlying diseases (predominantly AIDS and malignancy), these have rarely resulted in a fatal outcome. Patients who develop rashes during treatment with fluconazole should be monitored closely and the drug discontinued if lesions progress.
PRECAUTIONS
Some azoles, including fluconazole, have been associated with prolongation of the QT interval on the electrocardiogram. During postmarketing surveillance, there have been rare cases of QT prolongation and torsade de pointes in patients taking fluconazole. Most of these reports involved seriously ill patients with multiple confounding risk factors, such as structural heart disease, electrolyte abnormalities and concomitant medications that may have been contributory.
Fluconazole should be administered with caution to patients with these potentially proarrhythmic conditions.
The convenience and efficacy of the single dose oral tablet of fluconazole regimen for the treatment of vaginal yeast infections should be weighed against the acceptability of a higher incidence of drug related adverse events with fluconazole (26%) versus intravaginal agents (16%) in U.S. comparative clinical studies (see ADVERSE REACTIONS and CLINICAL STUDIES).
DRUG INTERACTIONS
(See CLINICAL PHARMACOLOGY, Drug Interaction Studies and CONTRAINDICATIONS). Clinically or potentially significant drug interactions between fluconazole and the following agents/classes have been observed. These are described in greater detail below:
| Oral hypoglycemics | Rifampin | Astemizole |
| Coumarin-type anticoagulants | Theophylline | Rifabutin |
| Phenytoin | Terfenadine | Tacrolimus |
| Cyclosporine | Cisapride | Short-acting benzodiazepines |
Clinically significant hypoglycemia may be precipitated by the use of fluconazole with oral hypoglycemic agents; one fatality has been reported from hypoglycemia in association with combined fluconazole and glyburide use. Fluconazole reduces the metabolism of tolbutamide, glyburide, and glipizide and increases the plasma concentration of these agents. When fluconazole is used concomitantly with these or other sulfonylurea oral hypoglycemic agents, blood glucose concentrations should be carefully monitored and the dose of the sulfonylurea should be adjusted as necessary (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Prothrombin time may be increased in patients receiving concomitant fluconazole and coumarin-type anticoagulants. In post-marketing experience, as with other azole antifungals, bleeding events (bruising, epitaxis, gastrointestinal bleeding, hematuria, and melena) have been reported in association with increases in prothrombin time in patients receiving fluconazole concurrently with warfarin. Careful monitoring of prothrombin time in patients receiving fluconazole and coumarin-type anticoagulants is recommended (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Fluconazole increases the plasma concentrations of phenytoin. Careful monitoring of phenytoin concentrations in patients receiving fluconazole and phenytoin is recommended (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Fluconazole may significantly increase cyclosporine levels in renal transplant patients with or without renal impairment. Careful monitoring of cyclosporine concentrations and serum creatinine is recommended in patients receiving fluconazole and cyclosporine (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Rifampin enhances the metabolism of concurrently administered fluconazole. Depending on clinical circumstances, consideration should be given to increasing the dose of fluconazole when it is administered with rifampin (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Fluconazole increases the serum concentrations of theophylline. Careful monitoring of serum theophylline concentrations in patients receiving fluconazole and theophylline is recommended (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Because of the occurrence of serious cardiac dysrhythmias secondary to prolongation of the QTc interval in patients receiving azole antifungals in conjunction with terfenadine, interaction studies have been performed. One study at a 200 mg daily dose of fluconazole failed to demonstrate a prolongation in QTc interval. Another study at a 400 mg and 800 mg daily dose of fluconazole demonstrated that fluconazole taken in doses of 400 mg per day or greater significantly increases plasma levels of terfenadine when taken concomitantly. The combined use of fluconazole at doses of 400 mg or greater with terfenadine is contraindicated (see CONTRAINDICATIONS and CLINICAL PHARMACOLOGY, Drug Interaction Studies). The coadministration of fluconazole at doses lower than 400 mg/day with terfenadine should be carefully monitored.
There have been reports of cardiac events, including trosade de poiintes in patients to whom fluconazole and cisapride were coadministered. A controlled study found that concomitant fluconazole 200 mg once daily and cisapride 20 mg four times a day yielded a significant increase in cisapride plasma levels and prolongation of QTc interval. The combined use of fluconazole with cisapride is contraindicated (see CONTRAINDICATIONS and CLINICAL PHARMACOLOGY, Drug Interaction Studies).
The use of fluconazole in patients concurrently taking astemizole or other drugs metabolized by the cytochrome P450 system may be associated with elevations in serum levels of these drugs. In the absence of definitive information, caution should be used when coadministering fluconazole. Patients should be carefully monitored.
There have been reports of uveitis in patients to whom fluconazole and rifabutin were coadministered. Patients receiving rifabutin and fluconazole concomitantly should be carefully monitored (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
There have been reports of nephrotoxicity in patients to whom fluconazole and tacrolimus were coadministered. Patients receiving tacrolimus and fluconazole concomitantly should be carefully monitored (see CLINICAL PHARMACOLOGY, Drug Interaction Studies).
Following oral administration of midazolam, fluconazole resulted in substantial increases in midazolam concentrations and psychomotor effects. This effect on midazolam appears to be more pronounced following oral administration of fluconazole than with fluconazole administered intravenously. If short-acting benzodiazepines, which are metabolized by the cytochrome P450 system, are concomitantly administered with fluconazole, consideration should be given to decreasing the benzodiazepine dosage, and the patients should be appropriately monitored. (See CLINICAL PHARMACOLOGY: Drug Interaction Studies.)
Fluconazole tablets coadministered with ethinyl estradiol- and levonorgestrel-containing oral contraceptives produced an overall mean increase in ethinyl estradiol and levonorgestrel levels; however, in some patients there were decreases up to 47% and 33% of ethinyl estradiol and levonorgestrel levels (see CLINICAL PHARMACOLOGY, Drug Interaction Studies). The data presently available indicate that the decreases in some individual ethinyl estradiol and levonorgestrel AUC values with fluconazole treatment are likely the result of random variation. While there is evidence that fluconazole can inhibit the metabolism of ethinyl estradiol and levonorgestrel, there is no evidence that fluconazole is a net inducer of ethinyl estradiol or levonorgestrel metabolism. The clinical significance of these effects is presently unknown.
Physicians should be aware that interaction studies with medications other than those listed in the CLINICAL PHARMACOLOGY section have not been conducted, but such interactions occur.
Fluconazole showed no evidence of carcinogenic potential in mice and rats treated orally for 24 months at doses of 2.5, 5 or 10 mg/kg/day (approximately 2 to 7 x the recommended human dose). Male rats treated with 5 and 10 mg/kg/day had an increased incidence of hepatocellular adenomas.
Fluconazole, with or without metabolic activation, was negative in tests for mutagenicicty in 4 strains of S. typhimurium, and in the mouse lymphoma L5178Y system. Cytogenetic studies in vivo (murine bone marrow cells, following oral administration of fluconazole) and in vitro (human lymphocytes exposed to fluconazole at 1000 mcg/mL) showed no evidence of chromosomal mutations.
Fluconazole did not affect the fertility of male or female rats treated orally with daily doses of 5, 10 or 20 mg/kg or with parenteral doses of 5, 25 or 75 mg/kg, although the onset of parturition was slightly delayed at 20 mg/kg PO. In an intravenous perinatal study in rats at 5, 20 and 40 mg/kg, dystocia and prolongation of parturition were observed in a few dams at 20 mg/kg (approximately 5 to 15 x the recommended human dose) and 40 mg/kg, but not at 5 mg/kg. The disturbances in parturition were reflected by a slight increase in the number of still-born pups and decrease of neonatal survival at these dose levels. The effects on parturition in rats are consistent with the species specific estrogen-lowering property produced by high doses of fluconazole. Such a hormone change has not been observed in women treated with fluconazole (see CLINICAL PHARMACOLOGY).
PREGNANCY
Fluconazole was administered orally to pregnant rabbits during organogenesis in two studies, at 5, 10 and 20 mg/kg and at 5, 25, and 75 mg/kg, respectively. Maternal weight gain was impaired at all dose levels, and abortions occurred at 75 mg/kg (approximately 20 to 60 x the recommended human dose); no adverse fetal effects were detected. In several studies in which pregnant rats were treated orally with fluconazole during organogenesis, maternal weight gain was impaired and placental weights were increased at 25 mg/kg. There were no fetal effects at 5 or 10 mg/kg; increases in fetal anatomical variants (supernumerary ribs, renal pelvis dilation) and delays in ossification were observed at 25 and 50 mg/kg and higher doses. At doses ranging from 80 mg/kg (approximately 20 to 60 x the recommended human dose) to 320 mg/kg embryolethality in rats was increased and fetal abnormalities included wavy ribs, cleft palate and abnormal cranio-facial ossification. These effects are consistent with the inhibition of estrogen synthesis in rats and may be a result of known effects of lowered estrogen on pregnancy, organogenesis and parturition.
There are no adequate and well controlled studies in pregnant women. There have been reports of multiple congenital abnormalities in infants whose mothers were being treated for 3 or more months with high dose (400 to 800 mg/day) fluconazole therapy for coccidioidomycosis (an unindicated use). The relationship between fluconazole use and these events is unclear. Fluconazole should be used in pregnancy only if the potential benefit justifies the possible risk to the fetus.
NURSING MOTHERS
PEDIATRIC USE
An open-label, randomized, controlled trial has shown fluconazole to be effective in the treatment of oropharyngeal candidiasis in pediatric patients 6 months to 13 years of age (see CLINICAL STUDIES).
The use of fluconazole in pediatric patients with cryptococcal meningitis, Candida esophagitis, or systemic Candida infections is supported by the efficacy shown for these indications in adults and by the results from several small noncomparative pediatric clinical studies. In addition, pharmacokinetic studies in pediatric patients (see CLINICAL PHARMACOLOGY) have established a dose proportionality between pediatric patients and adults (see DOSAGE AND ADMINISTRATION).
In a noncomparative study of pediatric patients with serious systemic fungal infections, most of which were candidemia, the effectiveness of fluconazole was similar to that reported for the treatment of candidemia in adults. Of 17 subjects with culture-confirmed candidemia, 11 of 14 (79%) with baseline symptoms (3 were asymptomatic) had a clinical cure; 13/15 (87%) of evaluable patients had a mycologic cure at the end of treatment but two of these patients relapsed at 10 and 18 days, respectively, following cessation of therapy.
The efficacy of fluconazole for the suppression of cryptococcal meningitis was successful in 4 of 5 pediatric patients treated in a compassionate-use study of fluconazole for the treatment of life-threatening or serious mycosis. There is no information regarding the efficacy of fluconazole for primary treatment of cryptococcal meningitis in pediatric patients.
The safety profile of fluconazole in pediatric patients has been studied in 577 pediatric patients ages 1 day to 17 years who received doses ranging from 1 to 15 mg/kg/day for 1 to 1,616 days (see ADVERSE REACTIONS).
Efficacy of fluconazole has not been established in infants less than 6 months of age (see CLINICAL PHARMACOLOGY). A small number of patients (29) ranging in age from 1 day to 6 months have been treated safely with fluconazole.
GERIATRIC USE
In non-AIDS patients, side effects possibly related to fluconazole treatment were reported in fewer patients aged 65 and older (9%, n=339) than for younger patients (14%, n=2240). However, there was no consistent difference between the older and younger patients with respect to individual side effects. Of the most frequently reported (less then 1%) side effects, rash, vomiting and diarrhea occurred in greater proportions of older patients. Similar proportions of older patients (2.4%) and younger patients (1.5%) discontinued fluconazole therapy because of side effects. In post-marketing experience, spontaneous reports of anemia and acute renal failure were more frequent among patients 65 years of age or older than in those between 12 and 65 years of age. Because of the voluntary nature of the reports and the natural increase in the incidence of anemia and renal failure in the elderly, it is however not possible to establish a casual relationship to drug exposure.
Controlled clinical trials of fluconazole did not include sufficient numbers of patients aged 65 and older to evaluate whether they respond differently from younger patients in each indication. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. Fluconazole is primarily cleared by renal excretion as unchanged drug. Because elderly patients are more likely to have decreased renal function, care should be taken to adjust dose based on creatinine clearance. It may be useful to monitor renal function. (See CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION.)
FLUCONAZOLE ADVERSE REACTIONS
During comparative clinical studies conducted in the United States, 448 patients with vaginal candidiasis were treated with fluconazole, 150 mg single dose. The overall incidence of side effects possibly related to fluconazole was 26%. In 422 patients receiving active comparative agents, the incidence was 16%. The most common treatment-related side adverse events reported in the patients who received 150 mg single dose fluconazole for vaginitis were headache (13%), nausea (7%), and abdominal pain (6%). Other side effects reported with an incidence equal to or greater than 1% included diarrhea (3%), dyspepsia (1%), dizziness (1%), and taste perversion (1%). Most of the reported side effects were mild to moderate in severity. Rarely, angioedema and anaphylactic reaction have been reported in marketing experience.
Sixteen percent of over 4000 patients treated with fluconazole in clinical trials of 7 days or more experienced adverse events. Treatment was discontinued in 1.5% of patients due to adverse clinical events and in 1.3% of patients due to laboratory test abnormalities.
Clinical adverse events were reported more frequently in HIV infected patients (21%) than in non-HIV infected patients (13%); however, the patterns in HIV infected and non-HIV infected patients were similar. The proportions of patients discontinuing therapy due to clinical adverse events were similar in the two groups (1.5%).
The following treatment-related clinical adverse events occurred at an incidence of 1% or greater in 4048 patients receiving fluconazole for 7 or more days in clinical trials: nausea 3.7%, headache 1.9%, skin rash 1.8%, vomiting 1.7%, abdominal pain 1.7%, and diarrhea 1.5%.
In combined clinical trials and marketing experience, there have been rare cases of serious hepatic reactions during treatment with fluconazole (see WARNINGS). The spectrum of these hepatic reactions has ranged from mild transient elevations in transaminases to clinical hepatitis, cholestasis and fulminant hepatic failure, including fatalities. Instances of fatal hepatic reactions were noted to occur primarily in patients with serious underlying medical conditions (predominantly AIDS or malignancy) and often while taking multiple concomitant medications. Transient hepatic reactions, including hepatitis and jaundice, have occurred among patients with no other identifiable risk factors. In each of these cases, liver function returned to baseline on discontinuation of fluconazole.
In two comparative trials evaluating the efficacy of fluconazole for the suppression of relapse of cryptococcal meningitis, a statistically significant increase was observed in median AST (SGOT) levels from a baseline value of 30 IU/L to 41 IU/L in one trial and 34 IU/L to 66 IU/L in the other. The overall rate of serum transaminase elevations of more than 8 times the upper limit of normal was approximately 1% in fluconazole-treated patients in clinical trials. These elevations occurred in patients with severe underlying disease, predominantly AIDS or malignancies, most of whom were receiving multiple concomitant medications, including many known to be hepatotoxic. The incidence of abnormally elevated serum transaminases was greater in patients taking fluconazole concomitantly with one or more of the following medications: rifampin, phenytoin, isoniazid, valproic acid, or oral sulfonylurea hypoglycemic agents.
In addition, the following adverse events have occurred during post-marketing experience.
In rare cases, anaphylaxis (including angioedema, face edema, and pruritis) has been reported.
QT prolongation, torsade de pointes. (See PRECAUTIONS.)
Seizures, dizziness
Exfoliative skin disorders including Stevens-Johnson syndrome and toxic epidermal necrolysis (see WARNINGS), alopecia
Leukopenia, including neutropenia and agranulocytosis, thrombocytopenia
Hypercholesterolemia, hypertriglyceridemia, hypokalemia, gastrointestinal dyspepsia, vomiting.
Taste perversion
In Phase II/III clinical trials conducted in the United States and in Europe, 577 pediatric patients, ages 1 day to 17 years were treated with fluconazole at doses up to 15 mg/kg/day for up to 1,616 days. Thirteen percent of pediatric patients experienced treatment related adverse events. The most commonly reported events were vomiting (5%), abdominal pain (3%), nausea (2%), and diarrhea (2%). Treatment was discontinued in 2.3% of patients due to adverse clinical events and in 1.4% of patients due to laboratory test abnormalities. The majority of treatment-related laboratory abnormalities were elevations of transaminases or alkaline phosphatase.
|
|
Fluconazole (N=577) | Comparative Agents (N=451) |
| With any side effect | 13.0 | 9.3 |
| Vomiting | 5.4 | 5.1 |
| Abdominal pain | 2.8 | 1.6 |
| Nausea | 2.3 | 1.6 |
| Diarrhea | 2.1 | 2.2 |
OVERDOSAGE
There have been reports of overdosage with fluconazole. A 42-year-old patient infected with human immunodeficiency virus developed hallucinations and exhibited paranoid behavior after reportedly ingesting 8200 mg of fluconazole. The patient was admitted to the hospital, and his condition resolved within 48 hours.
In the event of overdose, symptomatic treatment (with supportive measures and gastric lavage if clinically indicated) should be instituted. Fluconazole is largely excreted in urine. A three-hour hemodialysis session decreases plasma levels by approximately 50%
In mice and rats receiving very high doses of fluconazole, clinical effects in both species included decreased motility and respiration, ptosis, lacrimation, salivation, urinary incontinence, loss of righting reflex and cyanosis; death was sometimes preceded by clonic convulsions.
DOSAGE & ADMINISTRATION
The recommended dosage of fluconazole for vaginal candidiasis is 150 mg as a single oral dose.
SINCE ORAL ABSORPTION IS RAPID AND ALMOST COMPLETE, THE DAILY DOSE OF FLUCONAZOLE IS THE SAME FOR ORAL AND INTRAVENOUS ADMINISTRATION. In general, a loading dose of twice the daily dose is recommended on the first day of therapy to result in plasma concentrations close to steady-state by the second day of therapy.
The daily dose of fluconazole for the treatment of infections other than vaginal candidiasis should be based on the infecting organism and the patient’s response to therapy. Treatment should be continued until clinical parameters or laboratory tests indicate that active fungal infection has subsided. An inadequate period of treatment may lead to recurrence of active infection. Patients with AIDS and cryptococcal meningitis or recurrent oropharyngeal candidiasis usually require maintenance therapy to prevent relapse.
The recommended dosage of fluconazole for oropharyngeal candidiasis is 200 mg on the first day, followed by 100 mg once daily. Clinical evidence of oropharyngeal candidiasis generally resolves within several days, but treatment should be continued for at least 2 weeks to decrease the likelihood of relapse.
The recommended dosage of fluconazole for esophageal candidiasis is 200 mg on the first day, followed by 100 mg once daily. Doses up to 400 mg/day may be used, based on medical judgment of the patient’s response to therapy. Patients with esophageal candidiasis should be treated for a minimum of three weeks and for at least two weeks following resolution of symptoms.
For systemic Candida infections including candidemia, disseminated candidiasis, and pneumonia, optimal therapeutic dosage and duration of therapy have not been established. In open, noncomparative studies of small numbers of patients, doses of up to 400 mg daily have been used.
For the treatment of Candida urinary tract infections and peritonitis, daily doses of 50 to 200 mg have been used in open, noncomparitive studies of small numbers of patients.
The recommended dosage for treatment of acute cryptococcal meningitis is 400 mg on the first day, followed by 200 mg once daily. A dosage of 400 mg once daily may be used, based on medical judgment of the patient’s response to therapy. The recommended duration of treatment for initial therapy of cryptococcal meningitis is 10 to 12 weeks after cerebrospinal fluid becomes culture negative. The recommended dosage of fluconazole for suppression of relapse of cryptococcal meningitis in patients with AIDS is 200 mg once daily.
The recommended fluconazole daily dosage for the prevention of candidiasis of patients undergoing bone marrow transplantation is 400 mg, once daily. Patients who are anticipated to have severe granulocytopenia (less than 500 neutrophils per cu mm) should start fluconazole prophylaxis several days before the anticipated onset of neutropenia, and continue for 7 days after the neutrophil count rises above 1000 cells per cu mm.
The following dose equivalency scheme should generally provide equivalent exposure in pediatric and adult patients:
| Pediatric Patients | Adult |
|
Some older children may have clearances similar to that of adults. Absolute doses exceeding 600 mg/day are not recommended. |
|
| 3 mg/kg | 100 mg |
| 6 mg/kg | 200 mg |
| 12* mg/kg | 400 mg |
Experience with fluconazole in neonates is limited to pharmacokinetic studies in premature newborns (see CLINICAL PHARMACOLOGY). Based on the prolonged half-life seen in premature newborns (gestational age 26 to 29 weeks), these children, in the first two weeks of life, should receive the same dosage (mg/kg) as in older children, but administered every 72 hours. After the first two weeks, these children should be dosed once daily. No information regarding fluconazole pharmacokinetics in full-term newborns is available.
The recommended dosage of fluconazole for oropharyngeal candidiasis in children is 6 mg/kg on the first day, followed by 3 mg/kg once daily. Treatment should be administered for at least 2 weeks to decrease the likelihood of relapse.
For the treatment of esophageal candidiasis, the recommended dosage of fluconazole in children is 6 mg/kg on the first day, followed by 3 mg/kg once daily. Doses up to 12 mg/kg/day may be used based on medical judgment of the patient’s response to therapy. Patients with esophageal candidiasis should be treated for a minimum of three weeks and for at least 2 weeks following the resolution of symptoms.
For the treatment of candidemia and disseminated Candida infections, daily doses of 6 to 12 mg/kg/day have been used in an open, noncomparative study of a small number of children.
For the treatment of acute cryptococcal meningitis, the recommended dosage is 12 mg/kg on the first day, followed by 6 mg/kg once daily. A dosage of 12 mg/kg once daily may be used, based on medical judgment of the patient’s response to therapy. The recommended duration of treatment for initial therapy of cryptococcal meningitis is 10 to 12 weeks after the cerebrospinal fluid becomes culture negative. For suppression of relapse of cryptococcal meningitis in children with AIDS, the recommended dose of fluconazole is 6 mg/kg once daily.
Fluconazole is cleared primarily by renal excretion as unchanged drug. There is no need to adjust single dose therapy for vaginal candidiasis because of impaired renal function. In patients with impaired renal function who will receive multiple doses of fluconazole, an initial loading dose of 50 to 400 mg should be given. After the loading dose, the daily dose (according to indication) should be based on the following table:
| Creatinine Clearance (mL/min) | Percent of Recommended Dose |
| less then 50 | 100% |
| greater then 50 (no dialysis) | 50% |
| Regular dialysis | 100% after each dialysis |
These are suggested dose adjustments based on pharmacokinetics following administration of multiple doses. Further adjustment may be needed depending upon clinical condition.
When serum creatinine is the only measure of renal function available, the following formula (based on sex, weight, and age of the patient) should be used to estimate the creatinine clearance in adults:
| Males: | Weight (kg) x (140-age) |
|
|
72 x serum creatinine (mg/100 mL) |
|
|
|
| Females: | 0.85 x above value |
Although the pharmacokinetics of fluconazole has not been studied in children with renal insufficiency, dosage reduction in children with renal insufficiency should parallel that recommended for adults. The following formula may be used to estimate creatinine clearance in children:
| K x | linear length or height (cm) |
|
|
serum creatinine (mg/100mL) |
(Where K=0.55 for children older than 1 year and 0.45 for infants.)
HOW SUPPLIED
50” on the other side and packaged in bottles of 30, 100 and unit-dose boxes of 100 tablets.
Fluconazole Tablets, 100 mg are available as pink, modified oval-shaped, unscored tablets, debossed “5411” on one side.
100” on the other side and packaged in bottles of 30, 100 and unit-dose boxes of 100 tablets.
Fluconazole Tablets, 150 mg are available as pink, modified oval-shaped, unscored tablets, debossed “5412” on one side.
150” on the other side and packaged in unit-of-use cards of 1 tablet.
Fluconazole Tablets, 200 mg are available as pink, modified oval-shaped, unscored tablets, debossed “5413” on one side.
200” on the other side and packaged in bottles of 30, 100 and unit-dose boxes of 100 tablets.
PHARMACIST: Dispense in a tight container as defined in the USP. Use child-resistant closure (as required).
Store at 20°-25°C (68°-77°F) [See USP Controlled Room Temperature].
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION

FLUCONAZOLEFLUCONAZOLE TABLET
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||