Epinephrine
Amphastar Pharmaceuticals, Inc.
EPINEPHRINE INJECTION, USP, 1:1000
FULL PRESCRIBING INFORMATION: CONTENTS*
- EPINEPHRINE DESCRIPTION
- CLINICAL PHARMACOLOGY
- EPINEPHRINE INDICATIONS AND USAGE
- EPINEPHRINE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- EPINEPHRINE ADVERSE REACTIONS
- OVERDOSAGE
- EPINEPHRINE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PRINCIPAL DISPLAY PANEL - 30 mL Vial
FULL PRESCRIBING INFORMATION
EPINEPHRINE DESCRIPTION
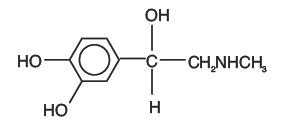
Epinephrine Injection, USP, is a sterile, nonpyrogenic solution intended for subcutaneous or intramuscular injection. When diluted, it may also be administered intracardially or intravenously. Each mL contains: 1 mg Epinephrine as the hydrochloride, in Water for Injection, USP, q.s. Sodium Chloride added for isotonicity, 0.5% Chlorobutanol (chloroform derivative) as a preservative and not more than 0.15% Sodium Metabisulfite as an antioxidant. The pH may be adjusted with Sodium Hydroxide and/ or Hydrochloric Acid. Epinephrine is the active principle of the adrenal medulla, chemically described as (-)-3,4-Dihydroxy-α-[(methylamino)methyl]benzyl alcohol, and has the following structural formula:
CLINICAL PHARMACOLOGY
Epinephrine is a sympathomimetic drug. It activates an adrenergic receptive mechanism on effector cells and imitates all actions of the sympathetic nervous system except those on the arteries of the face and sweat glands. Epinephrine acts on both alpha and beta receptors and is the most potent alpha receptor activator.
Epinephrine relaxes the smooth muscle of the bronchi and iris and is a physiologic antagonist of histamine. The drug also produces an increase in blood sugar and glycogenolysis in the liver.
Pharmacokinetics
Intravenous injection produces an immediate and intensified response. Following I.V. injection, epinephrine disappears rapidly from the blood stream. Subcutaneously or I.M. administered epinephrine has a rapid onset and short duration of action. Subcutaneous administration during asthmatic attacks may produce bronchodilation within 5 to 10 minutes, and maximal effects may occur within 20 minutes.
The drug becomes fixed in the tissues and is rapidly inactivated chiefly by enzymic transformation to metanephrine or normetanephrine, either of which is subsequently conjugated and excreted in the urine in the form of sulfates and glucuronides. Either sequence results in the formation of 3-methoxy-4-hydroxy-mandelic acid(vanillylmandelic acid, VMA) which is also detectable in the urine.
EPINEPHRINE INDICATIONS AND USAGE
In general, the most common uses of epinephrine are to relieve respiratory distress due to bronchospasm, to provide rapid relief of hypersensitivity reactions to drugs and other allergens, and to prolong the action of infiltration anesthetics. Its cardiac effects may be of use in restoring cardiac rhythm in cardiac arrest due to various causes, but is not used in cardiac failure or in hemorrhagic, traumatic, or cardiogenic shock.
Epinephrine is used as a hemostatic agent. It is also used in treating mucosal congestion of hay fever, rhinitis, and acute sinusitis; to relieve bronchial asthmatic paroxysms; in syncope due to complete heart block or carotid sinus hypersensitivity; for symptomatic relief of serum sickness, urticaria, angioneurotic edema; for resuscitation in cardiac arrest following anesthetic accidents; in simple (open angle) glaucoma; for relaxation of uterine musculature and to inhibit uterine contractions. Epinephrine injection can be utilized to prolong the action of local anesthetics (see CONTRAINDICATIONS).
EPINEPHRINE CONTRAINDICATIONS
Epinephrine is contraindicated in narrow angle (congestive) glaucoma, shock, during general anesthesia with halogenated hydrocarbons or cyclopropane and in individuals with organic brain damage. Epinephrine is also contraindicated with local anesthesia of certain areas, e.g., fingers, toes, because of the danger of vasoconstriction producing sloughing of tissue; in labor because it may delay the second stage; in cardiac dilatation and coronary insufficiency.
Epinephrine should not be used in those cases where vasopressor drugs may be contraindicated, e.g., in thyrotoxicosis, diabetes, in obstetrics when maternal blood pressure is in excess of 130/80, and in hypertension and other cardiovascular disorders.
WARNINGS
Administer with caution to elderly people; to those with cardiovascular disease, hypertension, diabetes, or hyperthyroidism; in psychoneurotic individuals; and in pregnancy.
Patients with long-standing bronchial asthma and emphysema who have developed degenerative heart disease should be administered the drug with extreme caution.
Overdosage or inadvertent intravenous injection of epinephrine may cause cerebrovascular hemorrhage resulting from the sharp rise in blood pressure. (See OVERDOSAGE )
Fatalities may also result from pulmonary edema because of the peripheral constriction and cardiac stimulation produced. Rapidly acting vasodilators, such as nitrites, or alpha blocking agents may counteract the marked pressor effects of epinephrine.
Epinephrine contains sodium bisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic rather than in non-asthmatic people.
Epinephrine is the preferred treatment of serious allergic or other emergency situations even though this product contains sodium metabisulfite, a sulfite that may in other products cause allergic-type reactions including anaphylactic symptoms or life-threatening or less severe asthmatic episodes in certain susceptible persons. The alternative to using epinephrine in a life-threatening situation may not be satisfactory. The presence of a sulfite in this product should not deter administration of the drug for treatment of serious allergic or other emergency situations.
Cardiovascular effects
Inadvertently induced high arterial blood pressure may result in angina pectoris (especially when coronary insufficiency is present), or aortic rupture.
Epinephrine may induce potentially serious cardiac arrhythmias in patients not suffering from heart disease and patients with organic heart disease or who are receiving drugs that sensitize the myocardium. With Epinephrine 1:1,000, a paradoxical but transient lowering of blood pressure, bradycardia and apnea may occur immediately after injection.
Cerebrovascular hemorrhage
Overdosage or inadvertent I.V. injection of epinephrine may cause cerebrovascular hemorrhage resulting from the sharp rise in blood pressure.
Pulmonary edema
Fatalities may also result from pulmonary edema because of the peripheral constriction and cardiac stimulation produced.
PRECAUTIONS
General
Epinephrine injection should be protected from exposure to light. Do not remove vial from carton until ready to use. The solution should not be used if it is pinkish or darker than slightly yellow or if it contains a precipitate.
Epinephrine is readily destroyed by alkalies and oxidizing agents. In the latter category are oxygen, chlorine, bromine, iodine, permanganates, chromates, nitrites, and salts of easily reducible metals, especially iron.
Drug Interactions
Use of epinephrine with excessive doses of digitalis, mercurial diuretics, or other drugs that sensitize the heart to arrhythmias is not recommended. Anginal pain may be induced when coronary insufficiency is present.
The effects of epinephrine may be potentiated by tricyclic antidepressants; certain antihistamines, e.g., diphenhydramine, tripelennamine, d-chlorpheniramine; and sodium I-thyroxine.
In obstetrics, if vasopressor drugs are used either to correct hypotension or added to the local anesthetic solution, some oxytocic drugs may cause severe persistent hypertension; even rupture of a cerebral blood vessel may occur during the postpartum period.
All vasopressors should be used cautiously in patients taking monoamine oxidase (MAO) inhibitors.
Cyclopropane or halogenated hydrocarbon anesthetics such as halothane which sensitize the myocardium administration of a beta-adrenergic blocking drug.
Diuretic agents may decrease vascular response to pressor drugs such as epinephrine.
Epinephrine may antagonize the neuron blockade produced by guanethidine resulting in decreased antihypertensive effect and requiring increased dosage of the latter.
Use of epinephrine with excessive doses of digitalis, mercurial diuretics or other drugs that sensitize the heart to arrhythmias is not recommended. Rapidly acting vasodilators such as nitrites or alpha-blocking agents may counteract the marked pressor effects of epinephrine.
Propranolol administered concomitantly with epinephrine may block the beta-adrenergic effects of epinephrine, causing hypertension.
PREGNANCY
Teratogenic effects
Pregnancy Category C
Epinephrine has been shown to be teratogenic in rats when given in doses about 25 times the human dose. There are not adequate and well-controlled studies in pregnant women. Epinephrine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Usage in Labor and Delivery
Parenteral administration of epinephrine, if used to support blood pressure during low or other spinal anesthesia for delivery, can cause acceleration of fetal heart rate and should not be used in obstetrics when maternal blood pressure exceeds 130/80.
Usage in Children
Epinephrine should be administered with caution to infants and children. Syncope has occurred following the administration of epinephrine to asthmatic children.
EPINEPHRINE ADVERSE REACTIONS
Transient and minor side effects of anxiety, headache, fear, and palpitations often occur with therapeutic doses, especially in hyperthyroid individuals. Repeated local injections can result in necrosis at sites of injection from vascular constriction. "Epinephrine-fastness" can occur with prolonged use.
Local
Repeated local injections can result in necrosis at sites of injection from vascular constriction.
Systemic
Cerebral hemorrhage; hemiplegia; subarachnoid hemorrhage; anginal pain in patients with angina pectoris; anxiety; restlessness; throbbing headache; tremor; weakness; dizziness; pallor; respiratory difficulty; palpitation; apprehensiveness; sweating; nausea; vomiting.
OVERDOSAGE
Symptoms
Erroneous administration of large doses of epinephrine may lead to precordial distress, vomiting, headache, dyspnea, as well as unusually elevated blood pressure.
Treatment
Most toxic effects can be counteracted by injection of an alpha-adrenergic blocker and a beta-adrenergic blocker. In the event of a sharp rise in blood pressure, rapid acting vasodilators such as the nitrites, or alpha-adrenergic blocking agents can counteract the marked pressor effects. If prolonged hypotension follows, it may be necessary to administer another pressor drug, such as norepinephrine.
If an epinephrine overdose induces pulmonary edema that interferes with respiration, treatment consists of a rapidly acting alpha-adrenergic blocking drug such as phentolamine and/or intermittent positive pressure respiration. Treatment of cardiac consists of a beta-adrenergic blocking drug such as propranolol.
Epinephrine overdosage can also cause transient bradycardia followed by tachycardia; these may be accompanied by potentially fatal cardiac arrhythmias. Ventricular premature contractions may appear within one minute after injection and may be followed by multifocal ventricular tachycardia (prefibrillation rhythm). Subsidence of the ventricular effects may be followed by atrial tachycardia, and occasionally, by atrioventricular block.
Overdosage sometimes results in extreme pallor and coldness of the skin, metabolic acidosis and kidney failure. Take suitable corrective measures.
EPINEPHRINE DOSAGE AND ADMINISTRATION
Subcutaneously or intramuscularly — 0.2 to 1 mL (mg). Start with a small dose and increase if required.
Note: The subcutaneous is the preferred route of administration. If given intramuscularly, injection into the buttocks should be avoided.
For bronchial asthma and certain allergic manifestations, e.g., angioedema, urticaria, serum sickness, anaphylactic shock, use epinephrine subcutaneously. For bronchial asthma in pediatric patients, administer 0.01 mg/kg or 0.3 mg/m2 to a maximum of 0.5 mg subcutaneously, repeated every four hours if required.
For cardiac resuscitation - A dose of 0.5 mL (0.5 mg) diluted to 10 mL with sodium chloride injection, can be administered intravenously or intracardially to restore myocardial contractility. External cardiac massage should follow intracardial administration to permit the drug to enter coronary circulation. The drug should be used secondarily to unsuccessful attempts with physical or electromechanical methods.
Parenteral drug products should be inspected visually for particulate matter and discoloration whenever solution and container permit.
HOW SUPPLIED
Epinephrine Injection, USP 1:1000 (1 mg/mL) Packaged individually.
| NDC 0548-9061-00 | 30 mL Multiple Dose Vial | Stock No. 9061 |
Store at Controlled room temperature 15° to 25°C (59° to 77°F). Protect from light and freezing.
International Medication Systems, Limited
So. El Monte, CA 91733, U.S.A.
An Amphastar Pharmaceuticals Company
Rx Only
REV. 1-08
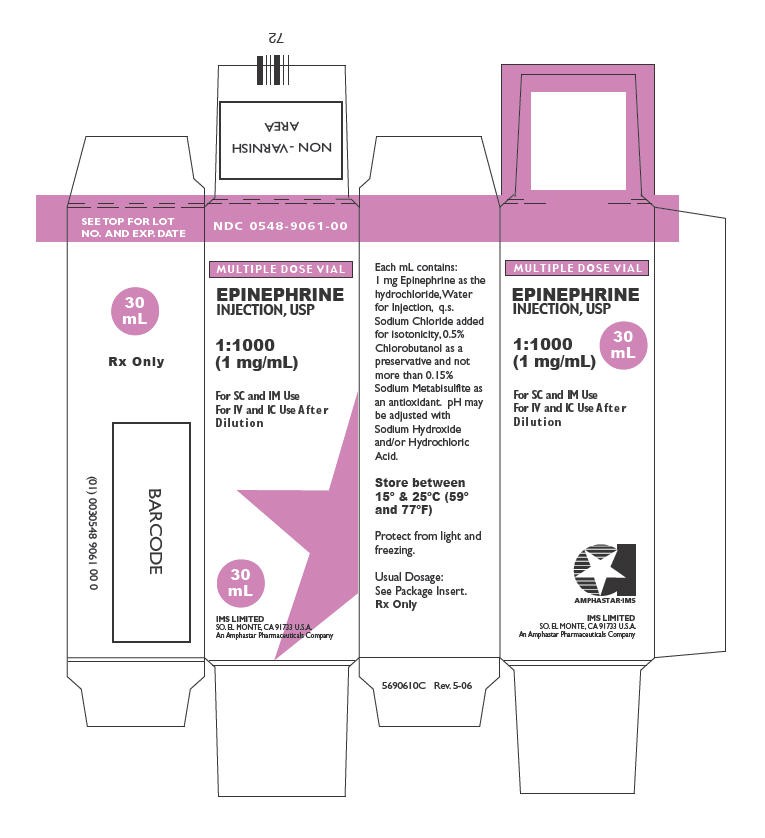
PRINCIPAL DISPLAY PANEL - 30 mL Vial
NDC 0548-9061-00
MULTIPLE DOSE VIAL
EPINEPHRINE
INJECTION, USP
1:1000
(1 mg/mL)
For SC and IM Use
For IV and IC Use After
Dilution
30
mL
IMS LIMITED
SO. EL MONTE, CA 91733 U.S.A.
An Amphastar Pharmaceuticals Company
EpinephrineEpinephrine INJECTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||