Dilaudid
Purdue Pharma LP
Purdue Pharma LP
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use DILAUDID INJECTION and DILAUDID-HP INJECTION safely and effectively. See full prescribing information for DILAUDID INJECTION and DILAUDID-HP INJECTION. DILAUDID INJECTION (hydromorphone hydrochloride) DILAUDID-HP INJECTION (hydromorphone hydrochloride) CII For intravenous, intramuscular and subcutaneous use Initial U.S. Approval: January 1984BOXED WARNING WARNING: RISK OF RESPIRATORY DEPRESSION, ABUSE, AND MEDICATION ERRORS DILAUDID-HP® INJECTION IS FOR USE IN OPIOID-TOLERANT PATIENTS ONLY See full prescribing information for complete boxed warning. Do not confuse DILAUDID-HP INJECTION with standard parenteral formulations of DILAUDID or other opioids, as overdose and death could result. (5) Hydromorphone is a potent Schedule II opioid agonist. Schedule II opioid agonists have the highest potential for abuse and risk of producing respiratory depression. Ethanol, other opioids, and other central nervous system depressants can potentiate the respiratory-depressant effects of hydromorphone and increase the risk of adverse outcomes, including death. (5.1, 7.1) INDICATIONS AND USAGE DILAUDID INJECTION is an opioid analgesic indicated for the management of pain where an opioid analgesic is appropriate. (1) DILAUDID-HP INJECTION is indicated for the management of moderate-to-severe pain in opioid-tolerant patients who require higher doses of opioids. (1) DOSAGE AND ADMINISTRATION DILAUDID INJECTION: The usual starting dose is 1 mg to 2 mg subcutaneously or intramuscularly every 2 to 3 hours as necessary. (2.3) DILAUDID-HP INJECTION should be used only if the amount of hydromorphone required can be delivered accurately with this formulation. (2.5) For patients already receiving opioids, use standard conversion ratio estimates. (2.4) The dose should be adjusted according to the severity of pain, as well as the patient's underlying disease state and age. (2.1, 2.2) Should intravenous administration be necessary, the injection should be given slowly, over at least 2 to 3 minutes and the usual starting dose is 0.2 to 1 mg. (2.3.2) DOSAGE FORMS AND STRENGTHS DILAUDID INJECTION: 1 mg/mL, 2 mg/mL, or 4 mg/mL. (3) DILAUDID-HP INJECTION: 10 mg/mL in 1 mL or 5 mL ampule or 50 mL single-dose vial. (3) DILAUDID-HP INJECTION Sterile Lyophilized Powder: 250 mg of sterile, lyophilized hydromorphone hydrochloride to be reconstituted to provide a solution containing 10 mg/mL. (3) CONTRAINDICATIONS Known hypersensitivity to hydromorphone, hydromorphone salts, any components of the product, or in any situation where opioids are contraindicated (4) Patients with respiratory depression in the absence of resuscitative equipment or in unmonitored settings; patients with status asthmaticus (4) Gastrointestinal obstruction, especially paralytic ileus (4) DILAUDID-HP INJECTION: Patients who are not opioid tolerant (4) WARNINGS AND PRECAUTIONS DILAUDID-HP INJECTION is a concentrated formulation of hydromorphone. Do NOT confuse DILAUDID-HP INJECTION with DILAUDID INJECTION. Overdose and death could result. (5.1) May cause respiratory depression, use with extreme caution in patients at risk of respiratory depression, elderly, and debilitated patients. (5.2) Abuse of DILAUDID INJECTION and DILAUDID-HP INJECTION poses a hazard of overdose and death. (5.3) Risk of medication errors: Morphine does not convert to hydromorphone on a milligram per milligram basis. Use Table 1 to convert. (5.1) Alcohol, other opioids and central nervous system depressants potentiate the respiratory depressant effects of hydromorphone. (5.4) Infants born to mothers physically dependent on DILAUDID INJECTION or DILAUDID-HP INJECTION will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms. (5.5) Respiratory depression may be markedly increased in patients with head injury, other intracranial lesions, or preexisting increase in intracranial pressure. (5.6) May cause hypotension, use with caution in patients at increased risk of hypotension and in patients in circulatory shock. (5.7) DILAUDID INJECTION and DILAUDID-HP INJECTION contain sodium metabisulfite. There is a risk of anaphylactic symptoms and life-threatening asthmatic episodes in susceptible people. (5.8) Use with caution in patients with biliary tract disease including pancreatitis. (5.9) Use with caution and in reduced initial doses in the elderly, debilitated, or other patient populations with increased risk of adverse reactions from opioids. (5.10) Use with caution in patients with alcoholism or other drug dependencies. (5.11) May impair the mental and physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. (5.12) Side EffectsMost common adverse reactions are lightheadedness, dizziness, sedation, nausea, vomiting, sweating, flushing, dysphoria, euphoria, dry mouth, and pruritus. (6) To report Suspected Adverse Reactions, contact Purdue Pharma L.P. at 1-888-726-7535 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .DRUG INTERACTIONS Concurrent use of other CNS depressants may cause respiratory depression, hypotension, and profound sedation or coma. (7.1) Mixed agonist/antagonist analgesics may reduce the analgesic effect of hydromorphone and may precipitate withdrawal symptoms in these patients. (7.2) USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm. (8.1) Labor and Delivery: Use with caution during labor. (8.2) Nursing Mothers: Nursing should not be undertaken while a patient is receiving DILAUDID INJECTION or DILAUDID-HP INJECTION. (8.3) Pediatrics: Safety and effectiveness in pediatric patients have not been established. (8.4) Geriatrics: Use with caution in elderly patients, initiate dose at low end of dosing range. (8.5) Hepatic and Renal Impairment: Patients with hepatic and renal impairment should be started on a lower starting dose. (8.6, 8.7, 12.2)
FULL PRESCRIBING INFORMATION: CONTENTS*
- BOX WARNING
- 1 DILAUDID INDICATIONS AND USAGE
- 2 DILAUDID DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 DILAUDID CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 5.1 Risk of Medication Errors
- 5.2 Respiratory Depression
- 5.3 Misuse, Abuse and Diversion of Opioids
- 5.4 Interactions with Alcohol and other CNS Depressants
- 5.5 Neonatal Withdrawal Syndrome
- 5.6 Use in Increased Intracranial Pressure or Head Injury
- 5.7 Hypotensive Effect
- 5.8 Sulfites
- 5.9 Use in Pancreatic/Biliary Tract Disease and Other Gastrointestinal Conditions
- 5.10 Special Risk Patients
- 5.11 Use in Drug and Alcohol Dependent Patients
- 5.12 Use in Ambulatory Patients
- 5.13 Parenteral Administration
- 6 DILAUDID ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 DILAUDID DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
FULL PRESCRIBING INFORMATION
DILAUDID® INJECTION (hydromorphone hydrochloride), CII
DILAUDID-HP® INJECTION (hydromorphone hydrochloride), CII
For intravenous, intramuscular, and subcutaneous use
BOX WARNING
WARNING: RISK OF RESPIRATORY DEPRESSION, ABUSE, AND MEDICATION ERRORS
DILAUDID-HP INJECTION IS FOR USE IN OPIOID-TOLERANT PATIENTS ONLY
Patients considered opioid tolerant are those who are taking at least 60 mg oral morphine/day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for one week or longer.
DILAUDID-HP INJECTION is a more concentrated solution of hydromorphone than DILAUDID INJECTION, and is for use in opioid-tolerant patients only. Do not confuse DILAUDID-HP INJECTION with standard parenteral formulations of DILAUDID INJECTION or other opioids, as overdose and death could result.
DILAUDID INJECTION and DILAUDID-HP INJECTION contain hydromorphone, an opioid agonist and a Schedule II controlled substance with an abuse liability similar to other opioid analgesics. DILAUDID INJECTION and DILAUDID-HP INJECTION can be abused in a manner similar to other opioid agonists, legal or illicit. These risks should be considered when administering, prescribing, or dispensing DILAUDID INJECTION and DILAUDID-HP INJECTION in situations where the healthcare professional is concerned about increased risk of misuse, abuse, or diversion.
Schedule II opioid agonists, including morphine, oxymorphone, hydromorphone, oxycodone, fentanyl and methadone, have the highest potential for abuse and risk of producing fatal overdose due to respiratory depression. Ethanol, other opioids, and other central nervous system depressants (e.g., sedative-hypnotics, skeletal muscle relaxants) can potentiate the respiratory-depressant effects of hydromorphone and increase the risk of adverse outcomes, including death.
1 INDICATIONS AND USAGE
DILAUDID INJECTION is indicated for the management of pain in patients where an opioid analgesic is appropriate.
DILAUDID-HP INJECTION is indicated for the management of moderate-to-severe pain in opioid-tolerant patients who require higher doses of opioids.
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Considerations
Take care when prescribing and administering Dilaudid and Dilaudid-HP Injection to avoid dosing errors due to confusion between the different concentrations and between mg and mL, which could result in accidental overdose and death. Take care to ensure the proper dose is communicated and dispensed. When writing prescriptions, include both the total dose in mg and the total volume of the dose.
Selection of patients and administration of Dilaudid and Dilaudid-HP injection should be governed by the same principles that apply to the use of similar opioid analgesics to treat patients with acute or chronic pain, and depends upon a comprehensive assessment of the patient. Individualize treatment in every case, using non-opioid analgesics, opioids on an as-needed basis and/or combination products, and chronic opioid therapy in a progressive plan of pain management such as outlined by the World Health Organization, the Agency for Healthcare Research and Quality, and the American Pain Society.
The nature of the pain (severity, frequency, etiology, and pathophysiology), as well as the medical status of the patient, will affect selection of the starting dosage. Opioid analgesics, including DILAUDID INJECTION and DILAUDID-HP INJECTION, have a narrow therapeutic index in certain patient populations, especially when combined with CNS depressant drugs, and should be reserved for cases where the benefits of opioid analgesia outweigh the known risks.
2.2 Individualization of Dosing
Initiate the dosing regimen for each patient individually, taking into account the patient’s prior analgesic treatment. Give attention to the following:
- the age, general condition, and medical status of the patient;
- the patient's degree of opioid tolerance;
- the daily dose, potency, and specific characteristics of the opioid the patient has been taking previously;
- concurrent medications
- the type and severity of the patient’s pain
- risk factors for abuse or addiction; including whether the patient has a previous or current substance abuse problem, a family history of substance abuse, or a history of mental illness or depression;
- the balance between pain control and adverse reactions.
Periodic reassessment after the initial dosing of DILAUDID INJECTION and DILAUDID-HP INJECTION is required. If pain management is not satisfactory, and opioid-induced adverse events are tolerable, the hydromorphone dose may be increased gradually. If excessive opioid side effects are observed early in the dosing interval, reduce the hydromorphone hydrochloride dose. If this results in breakthrough pain at the end of the dosing interval, the dosing interval may need to be shortened. Dose titration should be guided more by the need for analgesia and the severity of adverse events than the absolute dose of opioid employed.
2.3 Initiation of Therapy in Opioid-Naïve Patients
Always initiate dosing in opioid-naïve patients using Dilaudid Injection. Never administer Dilaudid-HP injection to opioid-naïve patients.
2.3.1 Subcutaneous or Intramuscular Administration
The usual starting dose of Dilaudid Injection is 1 mg to 2 mg every 2 to 3 hours as necessary. Depending on the clinical situation, the initial starting dose may be lowered in patients who are opioid naïve. Adjust the dose according to the severity of pain, the severity of adverse events, as well as the patient's underlying disease and age.
2.3.2 Intravenous Administration
The initial starting dose is 0.2 to 1 mg every 2 to 3 hours. Intravenous administration should be given slowly , over at least 2 to 3 minutes, depending on the dose. Titrate the dose to achieve acceptable analgesia and tolerable adverse events. The initial dose should be reduced in the elderly or debilitated and may be lowered to 0.2 mg.
2.3.3 Hepatic Impairment
Start patients with hepatic impairment on one-fourth to one-half the usual DILAUDID INJECTION starting dose depending on the extent of impairment [see CLINICAL PHARMACOLOGY, Pharmacokinetics (12.2)] .
2.3.4 Renal Impairment
Start patients with renal impairment on one-fourth to one-half the usual DILAUDID INJECTION starting dose depending on the degree of impairment [see CLINICAL PHARMACOLOGY, Pharmacokinetics (12.2)] .
2.4 Conversion From Prior Opioid
Use the equianalgesic dose table below (Table 1) as a guide to determine the appropriate dose of DILAUDID INJECTION. Convert the current total daily amount(s) of opioid(s) received to an equivalent total daily dose of DILAUDID INJECTION and reduce by one-half due to the possibility of incomplete cross tolerance. Divide the new total amount by the number of doses permitted based on dosing interval (e.g., 8 doses for every-three-hour dosing). Titrate the dose according to the patient's response. For opioids not in Table 1, first estimate the daily amount of morphine that is equivalent to the current total daily amount of other opioid(s) received, then use Table 1 to find the approximate equivalent total daily dose of DILAUDID INJECTION.
| DRUG SUBSTANCE | PARENTERAL DOSE | ORAL DOSE |
|---|---|---|
| * Dosages, and ranges of dosages represented, are a compilation of estimated equipotent dosages from published references comparing opioid analgesics in cancer and severe pain. | ||
| Morphine sulfate | 10 mg | 40 – 60 mg |
| Hydromorphone HCl | 1.3 – 2 mg | 6.5 – 7.5 mg |
| Oxymorphone HCl | 1 – 1.1 mg | 6.6 mg |
| Levorphanol tartrate | 2 – 2.3 mg | 4 mg |
| Meperidine HCl (Pethidine HCl) | 75 – 100 mg | 300 – 400 mg |
| Methadone HCl | 10 mg | 10 – 20 mg |
| Nalbuphine HCl | 10 – 12 mg | – |
| Butorphanol tartrate | 1.5 – 2.5 mg | – |
2.5 DILAUDID-HP Injection (for use in opioid-tolerant patients only)
Do not use DILAUDID-HP for patients who are not tolerant to the respiratory depressant or sedating effects of opioids. Patients considered opioid tolerant are those who are taking at least 60 mg oral morphine/day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for one week or longer.
Use DILAUDID-HP ONLY for patients who require the higher concentration and lower total volume of DILAUDID-HP.
Because of its high concentration, the delivery of precise doses of DILAUDID-HP INJECTION may be difficult if low doses of hydromorphone are required. Therefore, use DILAUDID-HP INJECTION only if the amount of hydromorphone required can be delivered accurately with this formulation.
Base the starting dose for DILAUDID-HP INJECTION on the prior dose of DILAUDID INJECTION or on the prior dose of an alternate opioid as described above in Section 2.4 Conversion From Prior Opioid and Table 1.
2.6 Administration and Reconstitution
Inspect parenteral drug products visually for particulate matter and discoloration prior to administration, whenever solution and container permit. A slight yellowish discoloration may develop in DILAUDID INJECTION and DILAUDID-HP INJECTION ampules. No loss of potency has been demonstrated. DILAUDID INJECTION and DILAUDID-HP INJECTION are physically compatible and chemically stable for at least 24 hours at 25°C, protected from light in most common large-volume parenteral solutions.
500 mg/50 mL Vial
To use this single dose presentation, do not penetrate the stopper with a syringe. Instead, remove both the aluminum flipseal and rubber stopper in a suitable work area such as under a laminar flow hood (or equivalent clean air compounding area). The contents may then be withdrawn for preparation of a single, large-volume parenteral solution. Discard any unused portion in an appropriate manner.
Reconstitution of Sterile Lyophilized DILAUDID-HP INJECTION 250 mg
Reconstitute immediately prior to use with 25 mL of Sterile Water for Injection USP to provide a sterile solution containing 10 mg/mL of hydromorphone hydrochloride.
3 DOSAGE FORMS AND STRENGTHS
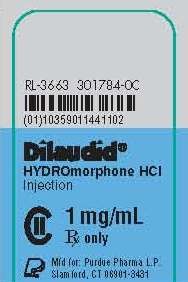
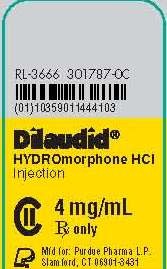
DILAUDID INJECTION:
Each 1 mL colorless ampule contains 1 mg/mL, 2 mg/mL, or 4 mg/mL of hydromorphone hydrochloride in a sterile, aqueous solution.
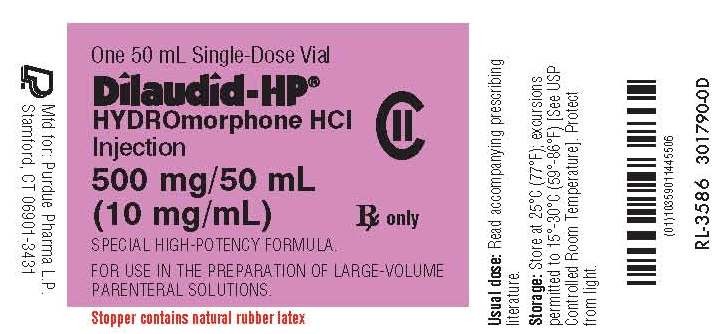
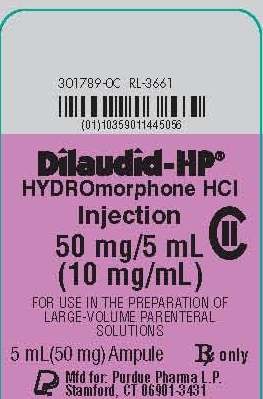
DILAUDID-HP INJECTION (for use in opioid-tolerant patients only):
Each amber ampule and amber single-dose vial contains 10 mg/mL of hydromorphone hydrochloride in a sterile, aqueous solution
and is available in 1 mL or 5 mL ampules
or in 50 mL single-dose vials†.
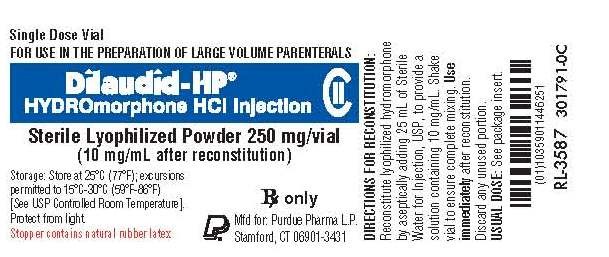
DILAUDID-HP INJECTION Sterile Lyophilized Powder:
Each amber, single-dose vial† contains 250 mg of sterile, lyophilized hydromorphone hydrochloride to be reconstituted with 25 mL of Sterile Water for Injection USP to provide a solution containing 10 mg/mL.
†The Stoppers Of These Products Contain Natural Rubber Latex.
4 CONTRAINDICATIONS
Both DILAUDID INJECTION and DILAUDID-HP INJECTION are contraindicated:
- In patients with known hypersensitivity to hydromorphone, hydromorphone salts, any other components of the product, or sulfite-containing medications [see WARNINGS AND PRECAUTIONS, Sulfites (5.8)].
- In any situation where opioids are contraindicated, e.g., in patients with respiratory depression in the absence of resuscitative equipment or in unmonitored settings; or patients with acute or severe bronchial asthma.
- In patients with, or at risk of developing, gastrointestinal obstruction, especially paralytic ileus because hydromorphone diminishes the propulsive peristaltic wave in the gastrointestinal tract and may prolong the obstruction.
DILAUDID-HP INJECTION is contraindicated in patients who are not opioid tolerant [see WARNINGS AND PRECAUTIONS (5.1)] .
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Medication Errors
DILAUDID-HP INJECTION is a 10 mg/mL concentrated solution of hydromorphone, and is intended for use in opioid-tolerant patients only. Patients considered opioid tolerant are those who are taking at least 60 mg oral morphine/day, 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for one week or longer.
Do not confuse DILAUDID-HP INJECTION with standard parenteral formulations of DILAUDID INJECTION (1 mg/mL, 2 mg/mL, 4 mg/mL) or other opioids, as overdose and death could result.
Morphine does not convert to hydromorphone on a mg per mg basis. Use Table 1 when converting a patient from morphine to hydromorphone to avoid errors that can lead to overdose or death.
5.2 Respiratory Depression
Respiratory depression is the chief hazard of DILAUDID INJECTION and DILAUDID-HP INJECTION. Respiratory depression occurs most frequently in the elderly, in the debilitated, and in those suffering from conditions accompanied by hypoxia or hypercapnia, or upper airway obstruction, in whom even moderate therapeutic doses may dangerously decrease pulmonary ventilation. Respiratory depression is also a particular problem following large initial doses in non opioid-tolerant patients or when opioids are given in conjunction with other agents that depress respiration.
Use DILAUDID INJECTION and DILAUDID-HP INJECTION with extreme caution in patients with chronic obstructive pulmonary disease or cor pulmonale, patients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression. In such patients, even usual therapeutic doses of opioid analgesics may decrease respiratory drive while simultaneously increasing airway resistance to the point of apnea. Consider using non-opioid analgesics, and administer DILAUDID only under careful medical supervision at the lowest effective dose in such patients.
5.3 Misuse, Abuse and Diversion of Opioids
DILAUDID INJECTION and DILAUDID-HP INJECTION contain hydromorphone, an opioid agonist with an abuse liability similar to morphine, and a Schedule II, controlled substance. Hydromorphone has the potential for being abused, is sought by drug abusers and people with addiction disorders, and is subject to criminal diversion. Diversion of Schedule II products is an act subject to criminal penalty.
Abuse of DILAUDID INJECTION and DILAUDID-HP INJECTION, poses a hazard of overdose and death. This risk is increased with concurrent abuse of alcohol or other substances. Schedule II opioid agonists have the highest potential for abuse and risk of fatal respiratory depression.
DILAUDID INJECTION and DILAUDID-HP INJECTION can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing DILAUDID INJECTION and DILAUDID-HP INJECTION in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse or diversion.
Concerns about abuse, addiction, and diversion should not prevent the proper management of pain. Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
5.4 Interactions with Alcohol and other CNS Depressants
The concurrent use of DILAUDID INJECTION or DILAUDID-HP INJECTION with other central nervous system (CNS) depressants, including, but not limited to, other opioids, illicit drugs, sedatives, hypnotics, general anesthetics, phenothiazines, muscle relaxants, other tranquilizers, and alcohol, increases the risk of respiratory depression, hypotension, and profound sedation, potentially resulting in coma or death. Use with caution and in reduced dosages in patients taking CNS depressants.
5.5 Neonatal Withdrawal Syndrome
Infants born to mothers physically dependent on DILAUDID INJECTION or DILAUDID-HP INJECTION will also be physically dependent and may exhibit signs of withdrawal. The withdrawal signs include irritability and excessive crying, tremors, hyperactive reflexes, increased respiratory rate, increased stools, sneezing, yawning, vomiting, and fever. The intensity of the syndrome does not always correlate with the duration of maternal opioid use or dose. Neonatal opioid withdrawal syndrome may be life-threatening and should be treated according to protocols developed by neonatology experts [see DRUG ABUSE AND DEPENDENCE (9.3)] .
5.6 Use in Increased Intracranial Pressure or Head Injury
The respiratory depressant effects of DILAUDID INJECTION and DILAUDID-HP INJECTION promote carbon dioxide retention which results in elevation of cerebrospinal fluid pressure. This increase in intracranial pressure may be markedly exaggerated in the presence of head injury, intracranial lesions, or other conditions that predispose patients to increased intracranial pressure.
DILAUDID INJECTION and DILAUDID-HP INJECTION may produce effects on pupillary response and consciousness which can obscure the clinical course and neurologic signs of further increase in pressure in patients with head injuries.
5.7 Hypotensive Effect
DILAUDID INJECTION and DILAUDID-HP INJECTION may cause severe hypotension in patients whose ability to maintain blood pressure is compromised by a depleted blood volume, or a concurrent administration of drugs such as phenothiazines, general anesthetics, or other agents which compromise vasomotor tone [see DRUG INTERACTIONS (7.1)] .
DILAUDID INJECTION and DILAUDID-HP INJECTION may produce orthostatic hypotension in ambulatory patients.
Administer DILAUDID INJECTION and DILAUDID-HP INJECTION with caution to patients in circulatory shock, since vasodilation produced by the drug may further reduce cardiac output and blood pressure.
5.8 Sulfites
DILAUDID INJECTION and DILAUDID-HP INJECTION contain sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
5.9 Use in Pancreatic/Biliary Tract Disease and Other Gastrointestinal Conditions
The administration of DILAUDID INJECTION or DILAUDID-HP INJECTION may obscure the diagnosis or clinical course in patients with acute abdominal conditions [see CONTRAINDICATIONS (4.0)] .
Use DILAUDID INJECTION and DILAUDID-HP with caution in patients who are at risk of developing ileus.
Use DILAUDID INJECTION and DILAUDID-HP INJECTION with caution in patients with biliary tract disease, including acute pancreatitis, as hydromorphone may cause spasm of the sphincter of Oddi and diminish biliary and pancreatic secretions.
5.10 Special Risk Patients
Give DILAUDID INJECTION and DILAUDID-HP INJECTION with caution and the initial dose should be reduced in the elderly or debilitated and those with severe impairment of hepatic, pulmonary, or renal function; myxedema or hypothyroidism; adrenocortical insufficiency (e.g., Addison's Disease); CNS depression or coma; toxic psychoses; prostatic hypertrophy or urethral stricture; acute alcoholism; delirium tremens; or kyphoscoliosis associated with respiratory depression.
The administration of opioid analgesics including DILAUDID INJECTION and DILAUDID-HP INJECTION may aggravate preexisting convulsions in patients with convulsive disorders.
DILAUDID INJECTION and DILAUDID-HP INJECTION, as with other opioids, may aggravate convulsions in patients with convulsive disorders, and may induce or aggravate seizures in some clinical settings.
Reports of mild to severe seizures and myoclonus have been reported in severely compromised patients administered high doses of parenteral hydromorphone.
5.11 Use in Drug and Alcohol Dependent Patients
Use DILAUDID INJECTION and DILAUDID-HP INJECTION with caution in patients with alcoholism and other drug dependencies due to the increased frequency of opioid tolerance, dependence, and the risk of addiction observed in these patient populations. Abuse of DILAUDID INJECTION or DILAUDID-HP INJECTION in combination with other CNS depressant drugs can result in serious risk to the patient.
DILAUDID INJECTION and DILAUDID-HP INJECTION contain hydromorphone, an opioid with no approved use in the management of addiction disorders. Its proper usage in individuals with drug or alcohol dependence, either active or in remission, is for the management of pain requiring opioid analgesia.
5.12 Use in Ambulatory Patients
DILAUDID INJECTION and DILAUDID-HP INJECTION may impair mental and/or physical ability required for the performance of potentially hazardous tasks (e.g., driving, operating machinery). Patients should be cautioned accordingly. DILAUDID INJECTION and DILAUDID-HP INJECTION may produce orthostatic hypotension in ambulatory patients.
5.13 Parenteral Administration
DILAUDID INJECTION may be given intravenously, but the injection should be given very slowly. Rapid intravenous injection of opioid analgesics increases the possibility of side effects such as hypotension and respiratory depression [see DOSAGE AND ADMINSTRATION (2.3)] .
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Serious adverse reactions associated with DILAUDID INJECTION and DILAUDID-HP INJECTION include respiratory depression and apnea and, to a lesser degree, circulatory depression, respiratory arrest, shock, and cardiac arrest.
The following serious adverse reactions described elsewhere in the labeling include:
-
- Respiratory depression and secondary effects on intracranial pressure [see WARNINGS AND PRECAUTIONS (5.2, 5.6)] -
- Hypotension [see WARNINGS AND PRECAUTIONS (5.7)] -
- Gastrointestinal effects and effects in sphincter of Oddi [see WARNINGS AND PRECAUTIONS (5.9)] -
- Drug abuse, addiction, and dependence [see DRUG ABUSE AND DEPENDENCE (9.2, 9.3)] -
- Effects on the ability to drive and operate machinery [see WARNINGS AND PRECAUTIONS (5.12)]
The most common adverse effects are lightheadedness, dizziness, sedation, nausea, vomiting, sweating, flushing, dysphoria, euphoria, dry mouth, and pruritus. These effects seem to be more prominent in ambulatory patients and in those not experiencing severe pain.
Less Frequently Observed Adverse Reactions
Cardiac disorders: tachycardia, bradycardia, palpitations
Eye disorders: vision blurred, diplopia, miosis, visual impairment
Gastrointestinal disorders: constipation, ileus, diarrhea, abdominal pain
General disorders and administration site conditions: weakness, feeling abnormal, chills, injection site urticaria
Hepatobiliary disorders: biliary colic
Metabolism and nutrition disorders: decreased appetite
Musculoskeletal and connective tissue disorders: muscle rigidity
Nervous system disorders: headache, tremor, paraesthesia, nystagmus, increased intracranial pressure, syncope, taste alteration, involuntary muscle contractions, presyncope
Psychiatric disorders: agitation, mood altered, nervousness, anxiety, depression, hallucination, disorientation, insomnia, abnormal dreams
Renal and urinary disorders: urinary retention, urinary hesitation, antidiuretic effects
Respiratory, thoracic, and mediastinal disorders: bronchospasm, laryngospasm
Skin and subcutaneous tissue disorders: injection site pain, urticaria, rash, hyperhidrosis
Vascular disorders: flushing, hypotension, hypertension
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of hydromorphone. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: anaphylactic reactions, confusional state, convulsions, drowsiness, dyskinesia, dyspnea, erectile dysfunction, fatigue, hepatic enzymes increased, hyperalgesia, hypersensitivity reaction, injection site reactions, lethargy, myoclonus, oropharyngeal swelling, peripheral edema, and somnolence.
7 DRUG INTERACTIONS
7.1 Drug Interactions with other CNS Depressants
DILAUDID INJECTION and DILAUDID-HP INJECTION should be used with caution and in reduced dosages when administered to patients concurrently receiving other central nervous system depressants including sedatives or hypnotics, general anesthetics, phenothiazines, centrally acting anti-emetics, tranquilizers, and alcohol because respiratory depression, hypotension, and profound sedation or coma may result.
When such combined therapy is contemplated, the dose of one or both agents should be reduced. Opioid analgesics, including DILAUDID INJECTION and DILAUDID-HP INJECTION, may enhance the action of neuromuscular blocking agents and produce an increased degree of respiratory depression.
7.2 Interactions with Mixed Agonist/Antagonist Opioid Analgesics
Agonist/antagonist analgesics (e.g., pentazocine, nalbuphine, and butorphanol) and partial agonist analgesics (buprenorphine) should be administered with caution to a patient who has received or is receiving a course of therapy with a pure opioid agonist analgesic such as DILAUDID INJECTION and DILAUDID-HP INJECTION. In this situation, mixed agonist/antagonist analgesics may reduce the analgesic effect of DILAUDID INJECTION and DILAUDID-HP INJECTION and/or may precipitate withdrawal symptoms in these patients.
7.3 Monoamine Oxidase Inhibitors (MAOIs)
MAOIs may potentiate the action of DILAUDID INJECTION and DILAUDID-HP INJECTION. Allow at least 14 days after stopping treatment with MAOIs before initiating treatment with DILAUDID INJECTION and DILAUDID-HP INJECTION.
7.4 Anticholinergics
Anticholinergics or other medications with anticholinergic activity when used concurrently with DILAUDID INJECTION and DILAUDID-HP INJECTION may result in increased risk of urinary retention and severe constipation, which may lead to paralytic ileus.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C: There are no adequate and well-controlled studies in pregnant women. Hydromorphone crosses the placenta. DILAUDID INJECTION or DILAUDID-HP INJECTION should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
No effects on teratogenicity or embryotoxicity were observed in pregnant rats given oral doses up to 7 mg/kg/day which is 3-fold higher than the human dose of 24 mg DILAUDID INJECTION (4 mg every 4 hours), on a body surface area basis. Hydromorphone administration to pregnant Syrian hamsters and CF-1 mice during major organ development revealed teratogenic effects likely the result of maternal toxicity associated with sedation and hypoxia. In Syrian hamsters given single subcutaneous doses from 14 to 258 mg/kg during organogenesis (gestation days 8-10), doses ≥ 19 mg/kg of hydromorphone produced skull malformations (exencephaly and cranioschisis). In CF-1 mice, continuous infusion of hydromorphone (≥ 15 mg/kg over 24 hours) via implanted osmotic pumps during organogenesis (gestation days 7-10) produced soft tissue malformations (cryptorchidism, cleft palate, malformed ventricles and retina), and skeletal variations (split supraoccipital, checkerboard and split sternebrae, delayed ossification of the paws and ectopic ossification sites). The malformations and variations observed in the hamsters and mice were observed at doses approximately 6-fold and 3-fold higher, respectively, than the human dose of 24 mg DILAUDID INJECTION (4 mg every 4 hours) on a body surface area basis.
8.2 Labor and Delivery
DILAUDID should be used with caution during labor. Opioids cross the placenta and may produce respiratory depression and physiologic effects in neonates. Sinusoidal fetal heart rate patterns may occur with the use of opioid analgesics.
Occasionally, opioid analgesics, including DILAUDID INJECTION and DILAUDID-HP INJECTION, may prolong labor through actions which temporarily reduce the strength, duration, and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilatation, which tends to shorten labor.
Opioid analgesics, including DILAUDID INJECTION and DILAUDID-HP INJECTION, may cause respiratory depression in the newborn. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression. Have a specific opioid antagonist, such as naloxone or nalmefene, available for reversal of opioid-induced respiratory depression in the neonate.
Neonates whose mothers have been taking opioids chronically may also exhibit withdrawal signs, either at birth or in the nursery, because they have developed physical dependence. This is not, however, synonymous with addiction
[see DRUG ABUSE AND DEPENDENCE (9.3)]
. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening and should be treated according to protocols developed by neonatology experts
[see WARNINGS AND PRECAUTIONS (5.3)]
.
The effect of DILAUDID, if any, on the later growth, development, and functional maturation of the child is unknown.
8.3 Nursing Mothers
Low levels of opioid analgesics have been detected in human milk. As a general rule, nursing should not be undertaken while a patient is receiving DILAUDID INJECTION or DILAUDID-HP INJECTION since it, and other drugs in this class, may be excreted in the milk.
8.4 Pediatric Use
The safety and effectiveness of DILAUDID INJECTION and DILAUDID-HP INJECTION in pediatric patients has not been established.
8.5 Geriatric Use
Clinical studies of DILAUDID INJECTION and DILAUDID-HP INJECTION did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Respiratory depression is the chief risk in elderly or debilitated patients, usually the result of large initial doses in non opioid-tolerant patients. Titration in these patients should proceed cautiously [see DOSAGE AND ADMINISTRATION (2.4) and WARNINGS AND PRECAUTIONS (5.10)] .
8.6 Renal Impairment
The pharmacokinetics of hydromorphone following an oral administration of hydromorphone at a single 4 mg dose (2 mg hydromorphone immediate-release tablets) are affected by renal impairment. Mean exposure to hydromorphone (Cmax and AUC0-∞) is increased by 2-fold in patients with moderate (CLcr = 40 - 60 mL/min) renal impairment and increased by 4-fold in patients with severe (CLcr < 30 mL/min) renal impairment compared with normal subjects (CLcr > 80 mL/min). In addition, in patients with severe renal impairment, hydromorphone appeared to be more slowly eliminated with a longer terminal elimination half-life (40 hr) compared to patients with normal renal function (15 hr). Start patients with renal impairment on one-fourth to one-half the usual starting dose depending on the degree of impairment. Patients with renal impairment should be closely monitored during dose titration [see CLINICAL PHARMACOLOGY (12.2)] .
8.7 Hepatic Impairment
The pharmacokinetics of hydromorphone following an oral administration of hydromorphone at a single 4 mg dose (2 mg hydromorphone immediate-release tablets) are affected by hepatic impairment. Mean exposure to hydromorphone (Cmax and AUC∞) is increased 4-fold in patients with moderate (Child-Pugh Group B) hepatic impairment compared with subjects with normal hepatic function. Due to increased exposure of hydromorphone, patients with moderate hepatic impairment should be started at one-fourth to one-half the recommended starting dose depending on the degree of hepatic dysfunction and closely monitored during dose titration. The pharmacokinetics of hydromorphone in patients with severe hepatic impairment has not been studied. A further increase in Cmax and AUC of hydromorphone in this group is expected and should be taken into consideration when selecting a starting dose [see CLINICAL PHARMACOLOGY (12.2)] .
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
DILAUDID INJECTION and DILAUDID-HP INJECTION contain hydromorphone, which is a Schedule II controlled substance with an abuse liability similar to morphine. DILAUDID can be abused and is subject to criminal diversion.
9.2 Abuse
DILAUDID INJECTION and DILAUDID-HP INJECTION are intended for parenteral use only under the direct supervision of an appropriately licensed health care professional.
Abuse of DILAUDID INJECTION and DILAUDID-HP INJECTION poses a hazard of overdose and death. This risk is increased with concurrent abuse of alcohol or other substances. Parenteral drug abuse is commonly associated with transmission of infectious diseases, such as hepatitis and HIV.
DILAUDID INJECTION and DILAUDID-HP INJECTION can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing, dispensing, ordering, or administering DILAUDID INJECTION or DILAUDID-HP INJECTION in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion. Prescribers should monitor all patients receiving opioids for signs of abuse, misuse, and addiction. Furthermore, patients should be assessed for their potential for opioid abuse prior to being prescribed opioid therapy. Persons at increased risk for opioid abuse include those with a personal or family history of substance abuse (including drug or alcohol abuse) or mental illness (e.g., depression). Opioids may still be appropriate for use in these patients, however, they will require intensive monitoring for indications of abuse.
Opioid drugs are sought by people with substance use disorders (abuse or addiction, the latter of which is also called “substance dependence”) and criminals who supply them by diverting medicines out of legitimate distribution channels. DILAUDID INJECTION and DILAUDID-HP INJECTION are targets for diversion.
“Drug-seeking” behavior is very common in persons with substance use disorders. Drug-seeking tactics include, but are not limited to, emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated “loss” of prescriptions, altering or forging of prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” to obtain additional prescriptions is common among people with untreated substance use disorders and criminals who divert controlled substances.
The risks of misuse and abuse should be considered when prescribing or dispensing DILAUDID INJECTION or DILAUDID-HP INJECTION. Concerns about abuse and addiction, should not prevent the proper management of pain, however. Treatment of pain should be individualized, balancing the potential benefits and risks for each patient.
Addiction is defined as a chronic, neurobiological disorder with genetic, psychosocial, and environmental aspects, characterized by one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances. Careful record keeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, proper dispensing and correct storage and handling are appropriate measures that help to limit misuse and abuse of opioid drugs. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised.
Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.
9.3 Dependence
Tolerance to opioids is demonstrated by the need for increasing doses to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance to different effects of opioids may develop to varying degrees and at varying rates in a given individual. There is also inter-patient variability in the rate and extent of tolerance that develops to various opioid effects, whether the effect is desirable (e.g., analgesia) or undesirable (e.g., nausea). In general, patients taking opioid analgesics that are appropriately titrated for pain control develop tolerance to the respiratory depressant effects fairly reliably. Conversely, tolerance to the constipating effects of opioids rarely develops, even when they are administered over long periods of time.
Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Physical dependence and tolerance are not unusual during chronic opioid therapy.
The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including: irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
In general, opioids used regularly should not be abruptly discontinued.
10 OVERDOSAGE
10.1 Signs and Symptoms
Signs and symptoms of acute overdosage with DILAUDID INJECTION or DILAUDID-HP INJECTION include: respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, apnea, circulatory collapse, cardiac arrest, and death.
Hydromorphone may cause miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis, rather than miosis, may be seen with hypoxia in overdose situations.
10.2 Treatment
In the treatment of overdosage, primary attention should be given to the reestablishment of a patent airway and institution of assisted or controlled ventilation. Supportive measures (including oxygen, vasopressors) should be employed in the management of circulatory shock and pulmonary edema accompanying overdose as indicated. Cardiac arrest or arrhythmias may require cardiac massage or defibrillation.
The opioid antagonist, naloxone, is a specific antidote against respiratory depression which may result from overdosage, or unusual sensitivity to DILAUDID INJECTION or DILAUDID-HP INJECTION. Therefore, an appropriate dose of this antagonist should be administered, preferably by the intravenous route, simultaneously with efforts at respiratory resuscitation. Naloxone should not be administered in the absence of clinically significant respiratory or circulatory depression. Naloxone should be administered cautiously to persons who are known, or suspected, to be physically dependent on DILAUDID INJECTION or DILAUDID-HP INJECTION. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute withdrawal syndrome.
Since the duration of action of DILAUDID INJECTION and DILAUDID-HP INJECTION may exceed that of the antagonist, the patient should be kept under continued surveillance; repeated doses of the antagonist may be required to maintain adequate respiration. Apply other supportive measures when indicated.
11 DESCRIPTION
DILAUDID (hydromorphone hydrochloride), a hydrogenated ketone of morphine, is an opioid analgesic. The chemical name of DILAUDID is 4,5α-epoxy-3-hydroxy-17-methylmorphinan-6-one hydrochloride. The structural formula is:
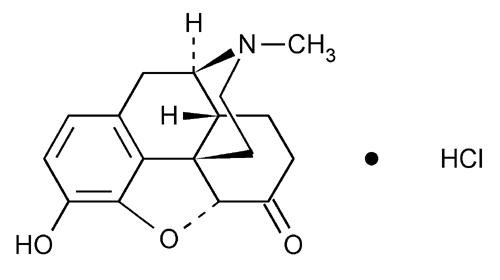
C17H19NO3•HCl 321.80
DILAUDID INJECTION is available as a sterile, aqueous solution in COLORLESS ampules for parenteral administration. Each 1 mL ampule contains 1 mg, 2 mg, or 4 mg of hydromorphone hydrochloride with 0.2% sodium citrate and 0.2% citric acid added as a buffer to maintain a pH between 3.5 and 5.5.
DILAUDID-HP INJECTION is available as a sterile, aqueous solution in AMBER ampules and in AMBER , single-dose vials for intravenous, subcutaneous, or intramuscular administration. Each ampule and single-dose vial contains 10 mg/mL of hydromorphone hydrochloride with 0.2% sodium citrate and 0.2% citric acid added as a buffer to maintain a pH of between 3.5 and 5.5. The single dose vials are capped with stoppers containing natural rubber latex.
DILAUDID-HP INJECTION is also available as sterile, lyophilized powder in an AMBER , single-dose vial for reconstitution for intravenous, subcutaneous, or intramuscular administration. Each single dose vial contains 250 mg sterile, lyophilized hydromorphone HCl with either hydrochloric acid or sodium hydroxide added to adjust the pH. Each vial is to be reconstituted with 25 mL of Sterile Water for Injection USP to provide a solution containing 10 mg/mL with a pH between 4.5 and 6.5. The single dose vials are capped with stoppers containing natural rubber latex.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mode of analgesic action of opioid analgesics is unknown. However, specific CNS opiate receptors have been identified. Opioids are believed to express their pharmacological effects by combining with these receptors.
Hydromorphone hydrochloride is a mu-opioid receptor agonist whose principal therapeutic action is analgesia. Other members of the class known as opioid agonists include substances such as morphine, oxycodone, fentanyl, codeine, hydrocodone, and oxymorphone.
Central Nervous System
Pharmacological effects of opioid agonists include anxiolysis, euphoria, feelings of relaxation, and cough suppression, as well as analgesia.
Hydromorphone produces respiratory depression by direct effect on brain stem respiratory centers. The mechanism of respiratory depression also involves a reduction in the responsiveness of the brain stem respiratory centers to increases in carbon dioxide tension.
Hydromorphone causes miosis. Pinpoint pupils are a common sign of opioid overdose but are not pathognomonic (pontine lesions of hemorrhagic or ischemic origin may produce similar findings).
Gastrointestinal Tract and Other Smooth Muscle
Gastric, biliary and pancreatic secretions are decreased by opioids such as hydromorphone. Hydromorphone causes a reduction in motility associated with an increase in tone in the gastric antrum and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, and tone may be increased to the point of spasm. The end result is constipation. Hydromorphone can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi.
Cardiovascular System
Hydromorphone may produce hypotension as a result of either peripheral vasodilation, release of histamine, or both. Other manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, and red eyes.
Effects on the myocardium after intravenous administration of opioids are not significant in normal persons, vary with different opioid analgesic agents and vary with the hemodynamic state of the patient, state of hydration and sympathetic drive.
Endocrine System
Opioids may influence the hypothalamic-pituitary-adrenal or -gonadal axes. Some changes that can be seen include an increase in serum prolactin, and decreases in plasma cortisol and testosterone. Clinical signs and symptoms may be manifest from these hormonal changes.
Immune System
In vitro and animal studies indicate that opioids have a variety of effects on immune functions. The clinical significance of these findings is unknown.
12.2 Pharmacokinetics
Distribution
At therapeutic plasma levels, hydromorphone is approximately 8-19% bound to plasma proteins. After an intravenous bolus dose, the steady state of volume of distribution [mean (%CV)] is 302.9 (32%) liters.
Metabolism
Hydromorphone is extensively metabolized via glucuronidation in the liver, with greater than 95% of the dose metabolized to hydromorphone-3-glucuronide along with minor amounts of 6-hydroxy reduction metabolites.
Elimination
Only a small amount of the hydromorphone dose is excreted unchanged in the urine. Most of the dose is excreted as hydromorphone-3-glucuronide along with minor amounts of 6-hydroxy reduction metabolites. The systemic clearance is approximately 1.96 (20%) liters/minute. The terminal elimination half-life of hydromorphone after an intravenous dose is about 2.3 hours.
Special Populations
Hepatic Impairment
After oral administration of hydromorphone at a single 4 mg dose (2 mg hydromorphone immediate-release tablets), mean exposure to hydromorphone (Cmax and AUC∞) is increased 4-fold in patients with moderate (Child-Pugh Group B) hepatic impairment compared with subjects with normal hepatic function. Patients with moderate hepatic impairment should be started at one-fourth to one-half the recommended starting dose and closely monitored during dose titration. The pharmacokinetics of hydromorphone in patients with severe hepatic impairment has not been studied. A further increase in Cmax and AUC of hydromorphone in this group is expected and should be taken into consideration when selecting a starting dose [see USE IN SPECIFIC POPULATIONS (8.7)] .
Renal Impairment
The pharmacokinetics of hydromorphone following an oral administration of hydromorphone at a single 4 mg dose (2 mg hydromorphone immediate-release tablets) are affected by renal impairment. Mean exposure to hydromorphone (Cmax and AUC0-∞) is increased by 2-fold in patients with moderate (CLcr = 40 - 60 mL/min) renal impairment and increased by 4-fold in patients with severe (CLcr < 30 mL/min) renal impairment compared with normal subjects (CLcr > 80 mL/min). In addition, in patients with severe renal impairment, hydromorphone appeared to be more slowly eliminated with a longer terminal elimination half-life (40 hr) compared to patients with normal renal function (15 hr). Start patients with renal impairment on one-fourth to one-half the usual starting dose depending on the degree of impairment. Patients with renal impairment should be closely monitored during dose titration [see USE IN SPECIFIC POPULATIONS (8.6)] .
Pediatrics
Pharmacokinetics of hydromorphone have not been evaluated in children.
Geriatric
In the geriatric population, age has no effect on the pharmacokinetics of hydromorphone.
Gender
Gender has little effect on the pharmacokinetics of hydromorphone. Females appear to have a higher Cmax (25%) than males with comparable AUC0-24 values. The difference observed in Cmax may not be clinically relevant.
Race
The effect of race on hydromorphone pharmacokinetics has not been studied.
Pregnancy and Nursing Mothers
Hydromorphone crosses the placenta. Hydromorphone is also found in low levels in breast milk, and may cause respiratory compromise in newborns when administered during labor or delivery.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long term studies in animals to evaluate the carcinogenic potential of hydromorphone have not been conducted.
Mutagenesis
Hydromorphone was not mutagenic in the in vitro bacterial reverse mutation assay (Ames assay). Hydromorphone was not clastogenic in either the in vitro human lymphocyte chromosome aberration assay or the in vivo mouse micronucleus assay.
Impairment of Fertility
No effects on fertility, reproductive performance, or reproductive organ morphology were observed in male or female rats given oral doses up to 7 mg/kg/day which is 3-fold higher than the human dose of 24 mg DILAUDID INJECTION (4 mg every 4 hours), on a body surface area basis.
14 CLINICAL STUDIES
Analgesic effects of single doses of DILAUDID ORAL LIQUID administered to patients with post-surgical pain have been studied in double-blind controlled trials. In one study, both 5 mg and 10 mg of DILAUDID ORAL LIQUID provided significantly more analgesia than placebo.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 Safety and Handling Instructions
DILAUDID INJECTION and DILAUDID-HP INJECTION pose little risk of direct exposure to health care personnel and should be handled and disposed of prudently in accordance with hospital or institutional policy. When DILAUDID INJECTION or DILAUDID-HP INJECTION is no longer needed, any unused liquid should be destroyed by flushing it down the toilet.
Access to drugs with a potential for abuse such as DILAUDID INJECTION and DILAUDID-HP INJECTION presents an occupational hazard for addiction in the health care industry. Routine procedures for handling controlled substances developed to protect the public may not be adequate to protect health care workers. Implementation of more effective accounting procedures and measures to restrict access to drugs of this class (appropriate to the practice setting) may minimize the risk of self-administration by health care providers.
16.2 How Supplied
DILAUDID INJECTION
DILAUDID INJECTION (hydromorphone hydrochloride) is supplied in COLORLESS ampules. Each 1 mL of sterile, aqueous solution contains 1 mg, 2 mg, or 4 mg hydromorphone hydrochloride with 0.2% sodium citrate and 0.2% citric acid solution. DILAUDID INJECTION contains no added preservative and is supplied as follows:
NDC
59011-441-10: Box of ten 1 mL (1 mg/mL) ampules
NDC
59011-442-10: Box of ten 1 mL (2 mg/mL) ampules
NDC
59011-442-25: Box of twenty-five 1 mL (2 mg/mL) ampules
NDC
59011-444-10: Box of ten 1 mL (4 mg/mL) ampules
DILAUDID-HP INJECTION
DILAUDID-HP INJECTION (hydromorphone hydrochloride) is supplied in AMBER ampules, and AMBER single-dose vials. Each ampule and single-dose vial of sterile aqueous solution contains 10 mg of hydromorphone hydrochloride with 0.2% sodium citrate and 0.2% citric acid solution.
DILAUDID-HP INJECTION Sterile Lyophilized Powder is supplied in an AMBER single-dose vial. Each vial contains 250 mg of sterile, lyophilized hydromorphone hydrochloride.
DILAUDID-HP INJECTION contains no added preservative and is supplied as follows:
NDC
59011-445-01: Box of ten 1 mL (10 mg/mL) ampules
NDC
59011-445-05: Box of ten 5 mL (10 mg/mL) ampules
†
NDC
59011-445-50: One 50 mL (10 mg/mL) single-dose vial with black rubber stopper and white flip-top/tear-off seal.
†
NDC
59011-446-25: One 250 mg single-dose vial with black rubber stopper and black flip-top seal.
†The Stoppers for These Products Contain Natural Rubber Latex
16.3 Storage
PROTECT FROM LIGHT.
Keep covered in carton until time of use. Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature].
Healthcare professionals can telephone Purdue Pharma L.P.’s Medical Services Department (1-888-726-7535) for information on this product.
CAUTION: DEA Order Form Required.
©2011 Purdue Pharma L.P.
Manufactured by
Hospira, Inc., Lake Forest, IL 60045, U.S.A.
For
Purdue Pharma L.P. Stamford, CT 06901-3431
U.S. Patent Number 6,589,960
302703-0A
Box of ten 1 mg/mL ampules
NDC 59011-441-10
Box of ten 2 mg/mL ampules
NDC 59011-442-10

Label for one 50mL Single Dose Vial
Box of ten 4 mg/mL ampules
NDC 59011-444-10
Box of ten 1mL (10 mg) ampules
NDC 59011-445-01

Dilaudid Injection 5 mg/mL
NDC 59011-445-50
Dilaudid Injection 250 mg/vial
NDC 59011-446-25
Dilaudidhydromorphone hydrochloride INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dilaudidhydromorphone hydrochloride INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dilaudidhydromorphone hydrochloride INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dilaudid HPhydromorphone hydrochloride INJECTION, SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Dilaudid HPhydromorphone hydrochloride INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||