Depo-SubQ Provera
depo-subQ provera 104 medroxyprogesterone acetate injectable suspension 104 mg/0.65 mL
FULL PRESCRIBING INFORMATION: CONTENTS*
- WARNING: LOSS OF BONE MINERAL DENSITY
- DEPO-SUBQ PROVERA DESCRIPTION
- CLINICAL PHARMACOLOGY
- DEPO-SUBQ PROVERA INDICATIONS AND USAGE
- DEPO-SUBQ PROVERA CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- 1. Physical Examination
- 2. Fluid Retention
- 3. Weight Gain
- 4. Return to Ovulation and Fertility
- 5. Depression
- 6. Injection Site Reactions
- 7. Carbohydrate/Metabolism
- 8. Liver Function
- 9. Drug Interactions
- 10. Laboratory Tests
- 11. Carcinogenesis, Mutagenesis, Impairment of Fertility
- 12. Pregnancy
- 13. Nursing Mothers
- 14. Pediatric Use
- 15. Geriatric Use
- INFORMATION FOR THE PATIENT
- DEPO-SUBQ PROVERA ADVERSE REACTIONS
- DEPO-SUBQ PROVERA DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- Patient Information About
- PRINCIPAL DISPLAY PANEL - 104 mg Syringe Label
- PRINCIPAL DISPLAY PANEL - 104 mg Syringe Carton
FULL PRESCRIBING INFORMATION
Physician Information
WARNING: LOSS OF BONE MINERAL DENSITY
Women who use depo-subQ provera 104 may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible.
It is unknown if use of depo-subQ provera 104 during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life.
depo-subQ provera 104 should not be used as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate (see WARNINGS, section 1).
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
DEPO-SUBQ PROVERA DESCRIPTION
depo-subQ provera 104 contains medroxyprogesterone acetate (MPA), a derivative of progesterone, as its active ingredient. Medroxyprogesterone acetate is active by the parenteral and oral routes of administration. It is a white to off-white, odorless crystalline powder that is stable in air and that melts between 205° and 209°C. It is freely soluble in chloroform, soluble in acetone and dioxane, sparingly soluble in alcohol and methanol, slightly soluble in ether, and insoluble in water.
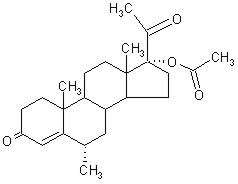
The chemical name for medroxyprogesterone acetate is 17-hydroxy-6α-methylpregn-4-ene-3,20-dione 17-acetate. The structural formula is as follows:
depo-subQ provera 104 for subcutaneous (SC) injection is available in pre-filled syringes (160 mg/mL), each containing 0.65 mL (104 mg) of medroxyprogesterone acetate sterile aqueous suspension.
Each 0.65 mL contains:
| Medroxyprogesterone acetate | 104 mg |
| Methylparaben | 1.040 mg |
| Propylparaben | 0.098 mg |
| Sodium Chloride | 5.200 mg |
| Polyethylene Glycol | 18.688 mg |
| Polysorbate 80 | 1.950 mg |
| Monobasic Sodium Phosphate ∙ H2O | 0.451 mg |
| Dibasic Sodium Phosphate ∙ 12H2O | 0.382 mg |
| Methionine | 0.975 mg |
| Povidone | 3.250 mg |
| Water for Injection | qs |
When necessary, the pH is adjusted with sodium hydroxide or hydrochloric acid, or both.
CLINICAL PHARMACOLOGY
depo-subQ provera 104 (medroxyprogesterone acetate injectable suspension), when administered at 104 mg/0.65 mL to women every 3 months (12 to 14 weeks), inhibits the secretion of gonadotropins, which prevents follicular maturation and ovulation and causes endometrial thinning. These actions produce its contraceptive effect.
Supression of serum estradiol concentrations and a possible direct action of depo-subQ provera 104 on the lesions of endometriosis are likely to be responsible for the therapeutic effect on endometriosis-associated pain.
Pharmacokinetics
The pharmacokinetic parameters of medroxyprogesterone acetate (MPA) following a single SC injection of depo-subQ provera 104 are shown in Table 1 and Figure 1.
| Cmax
(ng/mL) |
Tmax
(day) |
C91
(ng/mL) |
AUC0–91
(ng∙day/mL) |
AUC0–∞
(ng∙day/mL) |
t½ (day) |
|
|---|---|---|---|---|---|---|
| Cmax = peak serum concentration; Tmax = time when Cmax is observed; C91 = serum concentration at 91 days; AUC0–91 and AUC0–∞ = area under the concentration-time curve over 91 days or infinity, respectively; t½ = terminal half-life | ||||||
| Mean | 1.56 | 8.8 | 0.402 | 66.98 | 92.84 | 43 |
| Min | 0.53 | 2.0 | 0.133 | 20.63 | 31.36 | 16 |
| Max | 3.08 | 80.0 | 0.733 | 139.79 | 162.29 | 114 |
Absorption
Following a single SC injection of depo-subQ provera 104, serum MPA concentrations reach ≥ 0.2 ng/mL within 24 hours. The mean Tmax is attained approximately 1 week after injection.

In a study to assess accumulation and the achievement of steady state following multiple SC administrations, trough concentrations of MPA were determined after 6, 12, and 24 months, and in a subset of 8 subjects, bi-weekly concentrations were determined within one dosing interval in the second year of administration. The mean (SD) MPA trough concentrations were 0.67 (0.36) ng/mL (n=157), 0.79 (0.36) ng/mL (n=144), and 0.87 (0.33) ng/mL (n=106) at 6, 12 and 24 months, respectively.
Effect of Injection Site
depo-subQ provera 104 was administered into the anterior thigh or the abdomen to evaluate effects on the MPA concentration-time profile. MPA trough concentrations (Cmin; Day 91) were similar for the two injection locations.
Distribution
Plasma protein binding of MPA averages 86%. MPA binding occurs primarily to serum albumin. No binding of MPA occurs with sex-hormone-binding globulin (SHBG).
Metabolism
MPA is extensively metabolized in the liver by P450 enzymes. Its metabolism primarily involves ring A and/or side-chain reduction, loss of the acetyl group, hydroxylation in the 2-, 6-, and 21-positions or a combination of these positions, resulting in more than 10 metabolites.
Excretion
Residual MPA concentrations at the end of the first dosing interval (12 to 14 weeks) of depo-subQ provera 104 are generally below 0.5 ng/mL, consistent with its apparent terminal half-life of ~40 days after SC administration. Most MPA metabolites are excreted in the urine as glucuronide conjugates with only small amounts excreted as sulfates.
Linearity/Non-Linearity
Following a single SC administration of doses ranging from 50 to 150 mg, the AUC and Cmin (Day 91) increased with higher doses of depo-subQ provera 104, but there was considerable overlap across dose levels. Serum MPA concentrations at Day 91 increased in a dose proportional manner but Cmax did not appear to increase proportionally with increasing dose. The AUC data were suggestive of dose linearity.
Special Populations
Race
There were no significant differences in the pharmacokinetics and/or pharmacodynamics of MPA after SC administration of depo-subQ provera 104 in African-American and Caucasian women. The pharmacokinetics/pharmacodynamics of depo-subQ provera 104 were evaluated in Asian women in a separate study and also found to be similar to African-American and Caucasian women.
Effect of Body Weight
Although total MPA exposure was lower in obese women, no dosage adjustment of depo-subQ provera 104 is necessary based on body weight. The effect of body weight on the pharmacokinetics of MPA following a single dose was assessed in a subset of women (n = 42, body mass index [BMI] ranged from 18.2 to 46.7 kg/m2). The AUC0–91 values for MPA were 71.6, 67.9, and 46.3 ng·day/mL in women with BMI categories of ≤ 28 kg/m2, >28–38 kg/m2, and >38 kg/m2, respectively. The mean MPA Cmax was 1.74 ng/mL in women with BMI ≤ 28 kg/m2, 1.53 ng/mL in women with BMI >28–38 kg/m2, and 1.02 ng/mL in women with BMI > 38 kg/m2, respectively. The MPA trough (Cmin) concentrations had a tendency to be lower in women with BMI >38 kg/m2.
Hepatic Insufficiency
No clinical studies have evaluated the effect of hepatic disease on the disposition of depo-subQ provera 104. However, steroid hormones may be poorly metabolized in patients with severe liver dysfunction (see CONTRAINDICATIONS).
Renal Insufficiency
No clinical studies have evaluated the effect of renal disease on the pharmacokinetics of depo-subQ provera 104.
Drug-Drug Interactions
DEPO-SUBQ PROVERA INDICATIONS AND USAGE
depo-subQ provera 104 is indicated for the prevention of pregnancy in women of child bearing potential.
depo-subQ provera 104 also is indicated for management of endometriosis-associated pain.
In considering use for either indication, the loss of bone mineral density (BMD) in women of all ages and the impact on peak bone mass in adolescents should be considered, along with the decrease in BMD that occurs during pregnancy and/or lactation, in the risk/benefit assessment for women who use depo-subQ provera 104 long-term (see WARNINGS, section 1).
Contraception Studies
In three clinical studies, no pregnancies were detected among 2,042 women using depo-subQ provera 104 for up to 1 year. The Pearl Index pregnancy rate in women who were less than 36 years old at baseline, based on cycles in which they used no other contraceptive methods, was 0 pregnancies per 100 women-years of use (upper 95% confidence interval = 0.25).
Pregnancy rates for various contraceptive methods are typically reported for only the first year of use and are shown in Table 2.
| % of Women Experiencing an Unintended Pregnancy within the First Year of Use | % of Women Continuing Use at 1 Year |
|||
|---|---|---|---|---|
| Method | Typical Use |
Perfect Use |
||
| Source: Hatcher et al., 1998. i | ||||
| Chance |
85 | 85 | ||
| Spermicides |
26 | 6 | 40 | |
| Periodic Abstinence | 25 | 63 | ||
| Calendar | 9 | |||
| Ovulation Method | 3 | |||
| Symptothermal |
2 | |||
| Post-ovulation | 1 | |||
Cap |
||||
| Parous Women | 40 | 26 | 42 | |
| Nulliparous Women | 20 | 9 | 56 | |
| Sponge | ||||
| Parous Women | 40 | 20 | 42 | |
| Nulliparous Women | 20 | 9 | 56 | |
Diaphragm |
20 | 6 | 56 | |
| Withdrawal | 19 | 4 | ||
| Condom |
||||
| Female (Reality) | 21 | 5 | 56 | |
| Male | 14 | 3 | 61 | |
| Pill | 5 | 71 | ||
| Progestin only | 0.5 | |||
| Combined | 0.1 | |||
| IUD | ||||
| Progesterone T | 2.0 | 1.5 | 81 | |
| Copper T 380A | 0.8 | 0.6 | 78 | |
| LNg 20 | 0.1 | 0.1 | 81 | |
| Depo-Provera IM 150 mg | 0.3 | 0.3 | 70 | |
| Norplant and Norplant-2 | 0.05 | 0.05 | 88 | |
| Female Sterilization | 0.5 | 0.5 | 100 | |
| Male Sterilization | 0.15 | 0.10 | 100 | |
| Emergency Contraceptive Pills: Treatment initiated within 72 hours after unprotected intercourse reduces the risk of pregnancy by at least 75%. Lactational Amenorrhea Method: LAM is a highly effective, temporary method of contraception. |
||||
Endometriosis Studies
The efficacy of depo-subQ provera 104 in the reduction of endometriosis-associated pain in women with the signs and symptoms of endometriosis was demonstrated in two active comparator-controlled studies. Each study assessed reduction in endometriosis-associated pain over 6 months of treatment and recurrence of symptoms for 12-months post treatment. Subjects treated with depo-subQ provera 104 for 6 months received a 104 mg dose every 3 months (2 injections), while women treated with leuprolide microspheres for 6 months received a dose of 11.25 mg every 3 months (2 injections) or 3.75 mg every month (6 injections). Study 268 was conducted in the U.S. and Canada and enrolled 274 subjects (136 on depo-subQ provera 104 and 138 on leuprolide). Study 270 was conducted in South America, Europe and Asia, and enrolled 299 subjects (153 on depo-subQ provera 104 and 146 on leuprolide).
Reduction in pain was evaluated using a modified Biberoglu and Behrman scale that consisted of three patient-reported symptoms (dysmenorrhea, dyspareunia, and pelvic pain not related to menses) and two signs assessed during pelvic examination (pelvic tenderness and induration). For each category, a favorable response was defined as improvement of at least 1 unit (severity was assessed on a scale of 0 to 3) relative to baseline score (Figure 2).

Favorable Response = reduction in severity of symptom or sign of ≥ 1 point on a scale of 0 to 3, as compared to baseline
Additionally, scores from each of the five categories were combined, with the total (composite score) considered a global measurement of overall disease improvement. For subjects with baseline scores for each of the 5 categories, a mean decrease of 4 points relative to baseline was considered a clinically meaningful improvement. Across both studies, for both treatment groups, the mean changes in the composite score met the protocol-defined criterion for improvement.
In the clinical trials, treatment with depo-subQ provera 104 was limited to six months. Data on the persistence of benefit with longer treatment are not available.
Subjects recorded daily the occurrence and severity of hot flushes. Of the depo-subQ provera 104 users, 28.6% reported experiencing moderate or severe hot flushes at baseline, 36.2% at month 3, and 26.7% at month 6. Of the leuprolide users, 32.8% reported experiencing moderate or severe hot flushes at baseline, 74.2% at month 3, and 68.5% at month 6.
DEPO-SUBQ PROVERA CONTRAINDICATIONS
- Known or suspected pregnancy.
- Undiagnosed vaginal bleeding.
- Known or suspected malignancy of breast.
- Active thrombophlebitis, or current or past history of thromboembolic disorders, or cerebral vascular disease.
- Significant liver disease.
- Known hypersensitivity to medroxyprogesterone acetate or any of its other ingredients.
WARNINGS
1. Loss of Bone Mineral Density
Use of depo-subQ provera 104 reduces serum estrogen levels and is associated with significant loss of bone mineral density (BMD). This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. It is unknown if use of depo-subQ provera 104 by younger women will reduce peak bone mass and increase the risk for osteoporotic fracture in later life.
A study to assess the reversibility of loss of BMD in adolescents was conducted with Depo-Provera CI (150mg medroxyprogesterone acetate IM, DMPA). After discontinuing Depo-Provera CI in adolescents, mean BMD loss at total hip and femoral neck did not fully recover by 60 months (240 weeks) post-treatment. Similarly, in adults, there was only partial recovery of mean BMD at total hip, femoral neck and lumbar spine towards baseline by 24 months post-treatment.
depo-subQ provera 104 should not be used as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate. BMD should be evaluated when a woman needs to continue to use depo-subQ provera 104 long-term. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity.
Other birth control methods should be considered in the risk/benefit analysis for the use of depo-subQ provera 104 in women with osteoporosis risk factors. depo-subQ provera 104 can pose an additional risk in patients with risk factors for osteoporosis (e.g., metabolic bone disease, chronic alcohol and/or tobacco use, anorexia nervosa, strong family history of osteoporosis or chronic use of drugs that can reduce bone mass such as anticonvulsants or corticosteroids). Although there are no studies addressing whether calcium and Vitamin D lessen BMD loss in women using depo-subQ provera 104, all patients should have adequate calcium and Vitamin D intake.
BMD Changes in Adult Women after Long-Term Treatment for Contraception
A study comparing changes in BMD in women using depo-subQ provera 104 with women using Depo-Provera Contraceptive Injection (Depo-Provera CI, 150 mg) showed no significant differences in BMD loss between the two groups after two years of treatment. Mean percent changes in BMD in the depo-subQ provera 104 group are listed in Table 3.
| Lumbar Spine | Total Hip | Femoral Neck | ||||
|---|---|---|---|---|---|---|
| Time on Treatment | N | Mean % Change (95% CI) |
N | Mean % Change (95% CI) |
N | Mean % Change (95% CI) |
| 1 year | 166 | -2.7 (-3.1 to -2.3) |
166 | -1.7 (-2.1 to -1.3) |
166 | -1.9 (-2.5 to -1.4) |
| 2 year | 106 | - 4.1 (-4.6 to -3.5) |
106 | -3.5 (-4.2 to -2.7) |
106 | -3.5 (-4.3 to -2.6) |
In another controlled clinical study, adult women using Depo-Provera CI (150 mg) for up to 5 years showed spine and hip BMD mean decreases of 5–6%, compared to no significant change in BMD in the control group. The decline in BMD was more pronounced during the first two years of use, with smaller declines in subsequent years. Mean changes in lumbar spine BMD of –2.86%, -4.11%, -4.89%, -4.93% and –5.38% after 1, 2, 3, 4 and 5 years,-respectively, were observed. Mean decreases in BMD of the total hip and femoral neck were similar.
After stopping use of Depo-Provera CI (150 mg) there was partial recovery of BMD toward baseline values during the 2-year post-therapy period. Longer duration of treatment was associated with less complete recovery during this 2-year period following the last injection. Table 4 shows the change in BMD in women after 5 years of treatment with Depo-Provera CI and in women in a control group, as well as the extent of recovery of BMD for the subset of the women for whom 2-year post treatment data were available.
| Time in Study | Spine | Total Hip | Femoral Neck | |||
|---|---|---|---|---|---|---|
Depo-Provera  |
Control |
Depo-Provera  |
Control |
Depo-Provera  |
Control |
|
| 5 years | -5.38% n=33 |
0.43% n=105 |
-5.16% n=21 |
0.19% n=65 |
-6.12% n=34 |
-0.27% n=106 |
| 7 years | -3.13% n=12 |
0.53% n=60 |
-1.34% n=7 |
0.94% n=39 |
-5.38% n=13 |
-0.11% n=63 |
Bone Mineral Density Changes in Adolescent Females (12–18 years of age)
The impact of Depo-Provera CI (150 mg) use for up to 240 weeks (4.6 years) was evaluated in an open-label non-randomized clinical study in 389 adolescent females (12–18 years). Use of Depo-Provera CI was associated with a significant decline from baseline in BMD.
Partway through the trial, drug administration was stopped (at 120 weeks). The mean number of injections per Depo-Provera CI user was 9.3. The decline in BMD at total hip and femoral neck was greater with longer duration of use (see Table 5). The mean decrease in BMD at 240 weeks was more pronounced at total hip (-6.4%) and femoral neck (-5.4%) compared to lumbar spine (-2.1%).
In general, adolescents increase bone density during the period of growth following menarche, as seen in the untreated cohort. However, the two cohorts were not matched at baseline for age, gynecologic age, race, BMD and other factors that influence the rate of acquisition of bone mineral density.
| Duration of Treatment | Depo-Provera CI (150 mg IM) |
Unmatched, Untreated Cohort | ||
|---|---|---|---|---|
| N | Mean % Change | N | Mean % Change | |
| Total Hip BMD | ||||
| Week 60 (1.2 years) | 113 | -2.75 | 166 | 1.22 |
| Week 120 (2.3 years) | 73 | -5.40 | 109 | 2.19 |
| Week 240 (4.6 years) | 28 | -6.40 | 84 | 1.71 |
| Femoral Neck BMD | ||||
| Week 60 | 113 | -2.96 | 166 | 1.75 |
| Week 120 | 73 | -5.30 | 108 | 2.83 |
| Week 240 | 28 | -5.40 | 84 | 1.94 |
| Lumbar Spine BMD | ||||
| Week 60 | 114 | -2.47 | 167 | 3.39 |
| Week 120 | 73 | -2.74 | 109 | 5.28 |
| Week 240 | 27 | -2.11 | 84 | 6.40 |
BMD recovery post-treatment in adolescent women
Longer duration of treatment and smoking were associated with less recovery of BMD following the last injection of Depo-Provera CI. Table 6 shows the extent of recovery of BMD up to 60 months post-treatment for adolescent women who received Depo-Provera CI for two years or less compared to more than two years. Post-treatment follow-up showed that, in women treated for more than two years, only lumbar spine BMD recovered to baseline levels after treatment was discontinued. Subjects treated with Depo-Provera for more than two years did not recover to their baseline BMD level at femoral neck and total hip even up to 60 months post-treatment. Adolescent women in the untreated cohort gained BMD throughout the trial period (data not shown).
| Duration of Treatment | 2 years or less | More than 2 years | ||
|---|---|---|---|---|
| N | Mean % Change from baseline | N | Mean % Change from baseline | |
| Total Hip BMD | ||||
| End of Treatment | 49 | -1.5% | 49 | -6.2% |
| 12 M post-treatment | 33 | -1.4% | 24 | -4.6% |
| 24 M post-treatment | 18 | 0.3% | 17 | -3.6% |
| 36 M post-treatment | 12 | 2.1% | 11 | -4.6% |
| 48 M post-treatment | 10 | 1.3% | 9 | -2.5% |
| 60 M post-treatment | 3 | 0.2% | 2 | -1.0% |
| Femoral Neck BMD | ||||
| End of Treatment | 49 | -1.6% | 49 | -5.8% |
| 12 M post-treatment | 33 | -1.4% | 24 | -4.3% |
| 24 M post-treatment | 18 | 0.5% | 17 | -3.8% |
| 36 M post-treatment | 12 | 1.2% | 11 | -3.8% |
| 48 M post-treatment | 10 | 2.0% | 9 | -1.7% |
| 60 M post-treatment | 3 | 1.0% | 2 | -1.9% |
| Lumbar Spine BMD | ||||
| End of Treatment | 49 | -0.9% | 49 | -3.5% |
| 12 M post-treatment | 33 | 0.4% | 23 | -1.1% |
| 24 M post-treatment | 18 | 2.6% | 17 | 1.9% |
| 36 M post-treatment | 12 | 2.4% | 11 | 0.6% |
| 48 M post-treatment | 10 | 6.5% | 9 | 3.5% |
| 60 M post-treatment | 3 | 6.2% | 2 | 5.7% |
BMD Changes in Adult Women after Six Months of Treatment for Endometriosis
In two clinical studies of 573 adult women with endometriosis, the BMD effects of 6 months of depo-subQ provera 104 treatment were compared to 6 months of leuprolide treatment. Subjects were then observed, off therapy, for an additional 12 months (Table 7).
| Time of Measurement | Lumbar Spine | Total Hip | ||||||
|---|---|---|---|---|---|---|---|---|
| depo-subQ provera 104 | Leuprolide | depo-subQ provera 104 | Leuprolide | |||||
| N | Mean % change | N | Mean % change | N | Mean % change | N | Mean % change | |
| EOT = End of Treatment | ||||||||
| Month 6 of treatment (EOT) | 208 | -1.20 | 229 | -4.10 | 207 | -0.03 | 227 | -1.83 |
| 6 months off treatment | 168 | -1.06 | 180 | -2.75 | 169 | -0.05 | 181 | -1.59 |
| 12 months off treatment | 124 | -0.54 | 133 | -1.48 | 125 | 0.39 | 134 | -1.15 |
2. Bleeding Irregularities
Most women using depo-subQ provera 104 experienced changes in menstrual bleeding patterns, such as amenorrhea, irregular spotting or bleeding, prolonged spotting or bleeding, and heavy bleeding. As women continued using depo-subQ provera 104, fewer experienced irregular bleeding and more experienced amenorrhea. If abnormal bleeding is persistent or severe, appropriate investigation and treatment should be instituted.
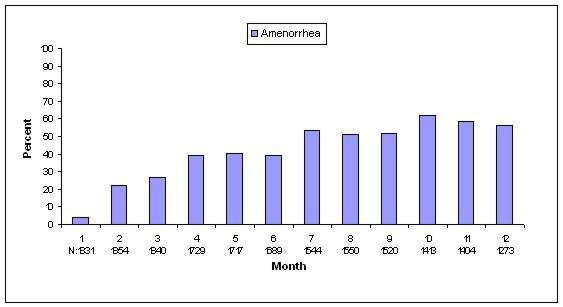
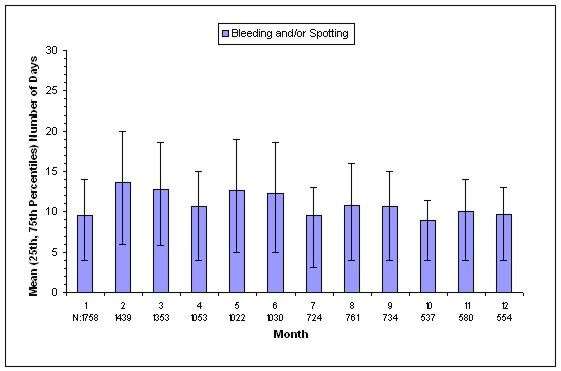
In three contraception trials, 39.0 % of women experienced amenorrhea during month six, and 56.5% experienced amenorrhea during month 12. The changes in menstrual bleeding patterns from the three contraception trials are presented in Figures 3 and 4.
| N = Number of subjects in analysis for indicated month |
| Figure 3. Percentages of depo-subQ provera 104 Treated Women with Amenorrhea per 30-Day Month in Contraception Studies (ITT Population, N=2053) |
|
| N = Number of subjects with bleeding and/or spotting during indicated month |
| Figure 4. Mean (25th, 75th Percentiles) Number of Bleeding and/or Spotting Days in the Subgroup of Women with Bleeding and/or Spotting by Month for Women Treated with depo-subQ provera 104 in Contraception Studies |
|
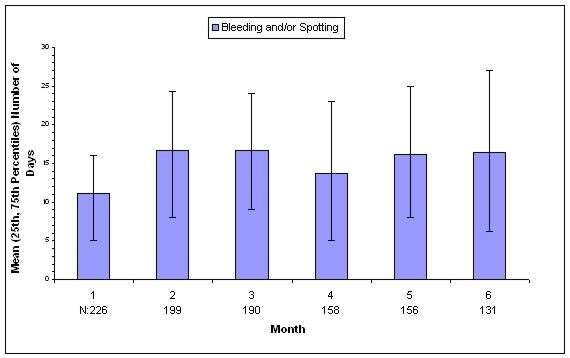
The changes in menstrual patterns in the two endometriosis trials are presented in Figures 5 and 6.
| N = Number of subjects in analysis for indicated month |
| Figure 5. Percentages of depo-subQ provera 104 Treated Women with Amenorrhea per 30-Day Month in Endometriosis Studies (Combined ITT Population, N=289) |

|
| N = Number of subjects with bleeding and/or spotting during indicated month |
| Figure 6. Mean (25th, 75th Percentiles) Number of Bleeding and/or Spotting Days in the Subgroup of Women with Bleeding and/or Spotting by Month for Women Treated with depo-subQ provera 104 in Endometriosis Studies Combined |
|
3. Cancer Risks
Long-term, case-controlled surveillance of users of depot medroxyprogesterone acetate IM 150 mg (Depo-Provera CI, 150 mg) found slight or no increased overall risk of breast cancer and no overall increased risk of ovarian, liver, or cervical cancer, and a prolonged, protective effect of reducing the risk of endometrial cancer.
A pooled analysisii from two case-control studiesiii iv reported the relative risk (RR) of breast cancer for women who had ever used Depo-Provera CI (150 mg) as 1.1 (95% confidence interval [CI] 0.97 to 1.4). Overall, there was no increase in risk with increasing duration of use of Depo-Provera CI (150 mg). The RR of breast cancer for women of all ages who had initiated use of Depo-Provera CI (150 mg) within the previous 5 years was estimated to be 2.0 (95% CI 1.5 to 2.8). A component of the pooled analysisiii described above, showed an increased RR of 2.19 (95% CI 1.23 to 3.89) of breast cancer associated with use of Depo-Provera CI (150 mg) in women whose first exposure to drug was within the previous 4 years and who were under 35 years of age. However, the overall RR for ever-users of Depo-Provera CI (150 mg) was only 1.21 (95% CI 0.96 to 1.52).
[NOTE: The value of 2.19 means that women whose first exposure to drug was within the previous 4 years and who were under 35 years of age had a 2.19-fold (95% CI 1.23 to 3.89-fold) increased risk of breast cancer relative to nonusers. The National Cancer Institutev reports an average annual incidence rate for breast cancer for US women, all races, age 30 to 34 years of 26.7 per 100,000. A RR of 2.19, thus, increases the possible risk from 26.7 to 58.5 cases per 100,000 women. The attributable risk, thus, is 31.8 per 100,000 women per year.]
The relative rate of invasive squamous-cell cervical cancer in women who ever used Depo-Provera CI (150 mg) was estimated to be 1.11 (95% CI 0.96 to 1.29). No trends in risk with duration of use or times since initial or most recent exposure were observed.
4. Thromboembolic Disorders
Although MPA has not been causally associated with the induction of thrombotic or thromboembolic disorders, there have been rare reports of serious thrombotic events in women using Depo-Provera CI (150 mg). Any patient who develops thrombosis while undergoing therapy with depo-subQ provera 104 should discontinue treatment unless she has no other acceptable options for birth control (see CONTRAINDICATIONS).
5. Ocular Disorders
Medication should not be re-administered pending examination if there is a sudden partial or complete loss of vision or if there is a sudden onset of proptosis, diplopia or migraine. If examination reveals papilledema or retinal vascular lesions, medication should not be re-administered.
6. Ectopic Pregnancy
Healthcare providers should be alert to the possibility of an ectopic pregnancy among women using depo-subQ provera 104 who become pregnant or complain of severe abdominal pain.
7. Anaphylaxis and Anaphylactoid Reaction
Serious anaphylactic reactions have been infrequently reported in women using Depo-Provera CI (150 mg). If an anaphylactic reaction occurs, appropriate emergency medical treatment should be instituted.
PRECAUTIONS
1. Physical Examination
It is good medical practice for all women to have annual history and physical examinations, including women using depo-subQ provera 104. The physical examination, however, may be deferred until after initiation of depo-subQ provera 104 if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
2. Fluid Retention
Because progestational drugs may cause some degree of fluid retention, conditions that might be influenced by this condition, such as epilepsy, migraine, asthma, and cardiac or renal dysfunction, require careful observation.
3. Weight Gain
Weight gain is a common occurrence in women using depo-subQ provera 104. In three large clinical trials using depo-subQ provera 104, the mean weight gain was 3.5 lb in the first year of use. In a small, two-year study comparing depo-subQ provera 104 to Depo-Provera CI (150 mg), the mean weight gain observed for women using depo-subQ provera 104 (7.5 lb) was similar to the mean weight gain for women using Depo-Provera CI, 150 mg (7.6 lb).
Although there are no data related to weight gain beyond 2 years for depo-subQ provera 104, the data on Depo-Provera CI (150 mg) may be relevant. In a clinical study, after five years, 41 women using Depo-Provera CI (150 mg) had a mean weight gain of 11.2 lb, while 114 women using non-hormonal contraception had a mean weight gain of 6.4 lb.
4. Return to Ovulation and Fertility
Return to ovulation is likely to be delayed after stopping therapy. Among 15 women who received multiple doses of depo-subQ provera 104:
- Median time to ovulation was 10 months after the last injection
- Earliest return to ovulation was 6 months after the last injection
- 12 women (80%) ovulated within 1 year of the last injection
However, ovulation has occurred as early as 14 weeks after a single dose of depo-subQ provera 104, and therefore it is important to follow the recommended dosing schedule.
Return to fertility also is likely to be delayed after stopping therapy. Among 28 women using depo-subQ provera 104 for contraception who stopped treatment to become pregnant, 1 became pregnant within 1 year of her last injection. A second woman became pregnant 443 days after her last injection. Seven women were lost to follow-up.
5. Depression
Patients with a history of treatment for clinical depression should be carefully monitored while receiving depo-subQ provera 104.
6. Injection Site Reactions
In 5 clinical studies of depo-subQ provera 104 involving 2,325 women (282 treated for up to 6 months, 1,780 treated for up to 1 year and 263 women treated for up to 2 years), 5% of women reported injection site reactions, and 1% had persistent skin changes, typically described as small areas of induration or atrophy.
7. Carbohydrate/Metabolism
Some patients receiving progestins may exhibit a decrease in glucose tolerance. Diabetic patients should be carefully observed while receiving such therapy.
8. Liver Function
If jaundice or any other liver abnormality develops in any woman receiving depo-subQ provera 104, treatment should be stopped while the cause is determined. Treatment may be resumed when liver function is acceptable and when the healthcare provider has determined that depo-subQ provera 104 did not cause the abnormality.
9. Drug Interactions
No drug-drug interaction studies have been conducted with depo-subQ provera 104. Aminoglutethimide administered concomitantly with depo-subQ provera 104 may significantly decrease the serum concentrations of MPA.
10. Laboratory Tests
The pathologist should be advised of progestin therapy when relevant specimens are submitted. The physician should be informed that certain endocrine and liver function tests, and blood components may be affected by progestin therapy:
-
(a) Plasma and urinary steroid levels are decreased (e.g., progesterone, estradiol, pregnanediol, testosterone, cortisol). -
(b) Plasma and urinary gonadotropin levels are decreased (e.g., LH, FSH). -
(c) SHBG concentrations are decreased. -
(d) T3-uptake values may decrease. -
(e) There may be small changes in coagulation factors. -
(f) Sulfobromophthalein and other liver function test values may be increased slightly. -
(g) There may be small changes in lipid profiles.
11. Carcinogenesis, Mutagenesis, Impairment of Fertility
See WARNINGS, section 3 and PRECAUTIONS, section 4
12. Pregnancy
Although depo-subQ provera 104 should not be used during pregnancy, there appears to be little or no increased risk of birth defects in women who have inadvertently been exposed to medroxyprogesterone acetate injections in early pregnancy. Neonates exposed to medroxyprogesterone acetate in-utero and followed to adolescence showed no evidence of any adverse effects on their health including their physical, intellectual, sexual or social development.
13. Nursing Mothers
Although the drug is detectable in the milk of mothers receiving Depo-Provera CI (150 mg), milk composition, quality, and amount are not adversely affected. Neonates and infants exposed to medroxyprogesterone acetate from breast milk have been studied for developmental and behavioral effects through puberty, and no adverse effects have been noted.
14. Pediatric Use
depo-subQ provera 104 is not indicated before menarche. Use of depo-subQ provera 104 is associated with significant loss of bone mineral density (BMD). This loss of BMD is of particular concern during adolescence and early adulthood, a critical period of bone accretion. In adolescents, interpretation of BMD results should take into account patient age and skeletal maturity. It is unknown if use of depo-subQ provera 104 by younger women will reduce peak bone mass and increase the risk for osteoporotic fractures in later life. Other than concerns about loss of BMD, the safety and effectiveness are expected to be the same for postmenarchal adolescents and adult women.
15. Geriatric Use
depo-subQ provera 104 is intended for use in women with childbearing potential. Studies with depo-subQ provera 104 in geriatric women have not been conducted.
INFORMATION FOR THE PATIENT
See PATIENT LABELING.
DEPO-SUBQ PROVERA ADVERSE REACTIONS
In five clinical studies of depo-subQ provera 104 involving 2,325 women (282 treated for up to 6 months, 1,780 treated for up to 1 year and 263 treated for up to 2 years), 9% of women discontinued treatment for adverse reactions. Among these 212 women, the most common reasons for discontinuation were:
- Uterine bleeding irregularities (35%, n=75)
- Increased weight (18%, n=39)
- Decreased libido (11%, n=23)
- Acne (10%, n=21)
- Injection site reactions (6%, n=12)
Adverse reactions reported by 5% or more of all women in these clinical trials included:
- Headache (9%)
- Intermenstrual bleeding (7%)
- Increased weight (6%)
- Amenorrhea (6%)
- Injection site reactions (5%)
Adverse reactions reported by 1% to <5% of all women in these clinical trials included:
General disorders: fatigue, injection site pain
Gastrointestinal disorders: abdominal distention, abdominal pain, diarrhea, nausea
Infections: bronchitis, influenza, nasopharyngitis, pharyngitis, sinusitis, upper respiratory tract infection, urinary tract infection, vaginal candidiasis, vaginitis, vaginitis bacterial
Investigations: abnormal cervix smear
Musculoskeletal, connective tissue, and bone disorders: arthralgia, back pain, limb pain
Nervous system disorders: dizziness, insomnia
Psychiatric disorders: anxiety, depression, irritability, decreased libido
Reproductive system and breast disorders: breast pain, breast tenderness, dysmenorrhea, menometrorrhagia, menorrhagia, menstruation irregular, uterine hemorrhage, vaginal hemorrhage
Skin disorders: acne
Vascular disorders: hot flushes
Postmarketing Experience
There have been rare cases of osteoporosis including osteoporotic fractures reported postmarketing in patients taking DEPO-PROVERA Contraceptive Injection. In addition, infrequent voluntary reports of anaphylaxis and anaphylactoid reaction have been received associated with use of Depo-Provera CI (150 mg).
The following additional reactions have been reported with Depo-Provera Contraceptive Injection and may occur with use of depo-subQ provera 104:
General disorders: asthenia, axillary swelling, chills, chest pain, fever, excessive thirst
Blood and lymphatic system disorders: anemia, blood dyscrasia
Cardiac disorders: tachycardia
Gastrointestinal disorders: gastrointestinal disturbances, rectal bleeding
Hepato-biliary disorders: jaundice
Immune system disorders: allergic reaction
Infections: genitourinary infections
Investigations: decreased glucose tolerance
Musculoskeletal, connective tissue, and bone disorders: loss of bone mineral density, scleroderma
Neoplasms: breast cancer, cervical cancer
Nervous system disorders: convulsions, facial palsy, fainting, paralysis, paresthesia, somnolence
Psychiatric disorders: increased libido, nervousness
Reproductive system and breast disorders: breast lumps, galactorrhea, nipple discharge or bleeding, oligomenorrhea, prevention of lactation, prolonged anovulation, unexpected pregnancy, uterine hyperplasia, vaginal cyst
Respiratory disorders: asthma, dyspnea, hoarseness
Skin disorders: angioedema, dry skin, increased body odor, melasma, pruritus, urticaria
Vascular disorders: deep vein thrombosis, pulmonary embolus, thrombophlebitis
DEPO-SUBQ PROVERA DOSAGE AND ADMINISTRATION
CONTRACEPTION AND ENDOMETRIOSIS INDICATIONS
Route of Administration
depo-subQ provera 104 must be given by subcutaneous injection into the anterior thigh or abdomen, once every 3 months (12 to 14 weeks). depo-subQ provera 104 is not formulated for intramuscular injection. Dosage does not need to be adjusted for body weight. The pre-filled syringe of depo-subQ provera 104 must be vigorously shaken just before use to create a uniform suspension.
First Injection
Ensure that the patient is not pregnant at the time of the first injection. For women who are sexually active and having regular menses, the first injection should be given only during the first 5 days of a normal menstrual period. Women who are breast-feeding may have their first injection during or after their sixth postpartum week.
Second and Subsequent Injections
Dosing is every 12 to 14 weeks. If more than 14 weeks elapse between injections, pregnancy should be ruled out before the next injection.
IF USING FOR CONTRACEPTION AND SWITCHING FROM ANOTHER METHOD
When switching from other contraceptive methods, depo-subQ provera 104 should be given in a manner that ensures continuous contraceptive coverage. For example, patients switching from combined (estrogen plus progestin) contraceptives should have their first injection of depo-subQ provera 104 within 7 days after the last day of using that method (7 days after taking the last active pill, removing the patch or ring). Similarly, contraceptive coverage will be maintained in switching from Depo-Provera CI (150 mg) to depo-subQ provera 104, provided the next injection is given within the prescribed dosing period for Depo-Provera CI (150 mg).
IF USING FOR TREATMENT OF ENDOMETRIOSIS
Treatment for longer than two years is not recommended, due to the impact of long-term depo-subQ provera 104 on bone mineral density. If symptoms return after discontinuation of treatment, bone mineral density should be evaluated prior to retreatment.
Instructions for Use of depo-subQ provera 104
FOR SUBCUTANEOUS ADMINISTRATION ONLY
Please read these instructions carefully. It is very important that the entire dose of depo-subQ provera 104 is given.
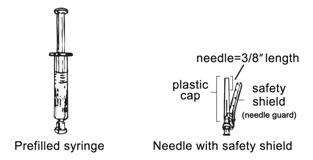
Getting ready
Do not refrigerate. Ensure that the medication is at room temperature prior to injection (to ensure appropriate viscosity of the suspension). Make sure the following components are available.
depo-subQ provera 104, as with other parenteral drug products, should be inspected visually for particulate matter and discoloration prior to administration.
Step 1: Choosing & preparing the injection Area
Choose the injection area.
|
Preferred injection areas:
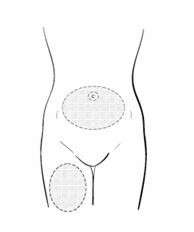
Upper thigh or abdomen |
Use an alcohol pad to wipe the skin in the injection area you have chosen.
|
Step 2: Syringe preparation
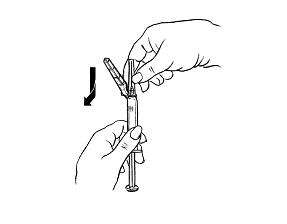
| Carefully remove the needle and syringe from the packaging. Hold the syringe firmly by the barrel, with the barrel pointing upward.
|
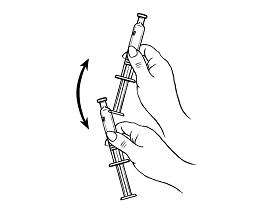
|
Hold the syringe barrel firmly.
|
Shake vigorously for 1 minute
|
Hold the syringe barrel firmly.
|
|
|
|
|
|
|
|
Step 3: Injecting the dose
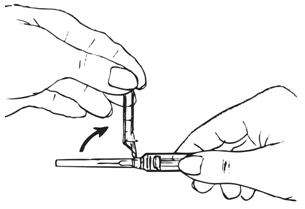
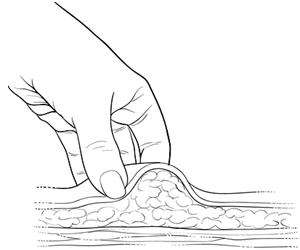
| Gently grasp and squeeze a large area of skin in the chosen injection area between the thumb and forefinger, pulling it away from the body. |
|
Insert the needle at a 45 degree angle so that most of the needle is in the fatty tissue.
|

|
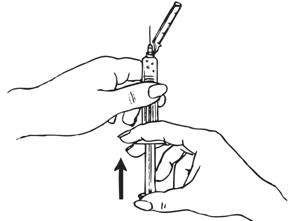
Inject the medication slowly until the syringe is empty.
|
Inject slowly (5–7 seconds) 
|
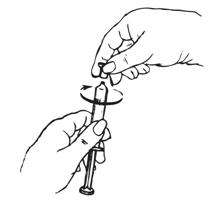
Step 4: Disposing the needle and syringe
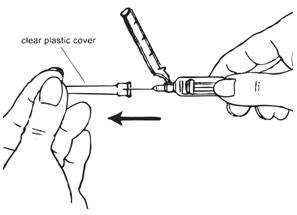
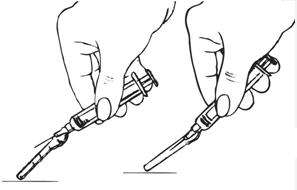
| After completing the injection, remove the needle from the skin and activate the safety shield. |
|
| Position shield about 40°– 45°. With a firm quick motion, press down against a flat surface until a click is heard or felt. | |
| If uncertain that the safety shield is fully engaged, repeat this step. | |
Use a clean cotton pad to press lightly on the injection area for a few seconds.
|

|
| Following the administration of each dose, the used syringe should be discarded in a safe and proper manner. | |
| Keep away from children. | |
HOW SUPPLIED
depo-subQ provera 104 for subcutaneous use (medroxyprogesterone acetate injectable suspension 104 mg/0.65 mL) is available as a pre-filled syringe, packaged with a 26-gauge × 3/8 inch Terumo® Surguard™ needle in the following presentation:
NDC 0009-4709-13 0.65 mL single-use, disposable syringe
Store at controlled room temperature 20° to 25° C (68° to 77°F) [see USP].
This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com
Rx only

LAB-0295-11.0
August 2013
-
i Trussell J. Contraceptive efficacy. In Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowel D, Guest F, Contraceptive Technology: 17th Revised Edition. New York, NY: Irvington Publishers, 1998. -
ii Skegg DCG, Noonan EA, Paul C, Spears GFS, Meirik O, Thomas DB. Depot Medroxyprogesterone Acetate and Breast Cancer: A Pooled Analysis from the World Health Organization and New Zealand Studies. JAMA. 1995; 273(10): 799–804. -
iii WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Breast cancer and depot-medroxyprogesterone acetate: a multi-national study. Lancet. 1991; 338:833–838. -
iv Paul C, Skegg DCG, Spears GFS. Depot medroxyprogesterone (Depo-Provera) and risk of breast cancer. Br Med J. 1989; 299:759–762. -
v Surveillance, Epidemiology, and End Results: Incidence and Mortality Data, 1973–1977. National Cancer Institute Monograph, 57: June 1981. (NIH publication No. 81-2330).
Patient Information About
depo-subQ provera 104™
medroxyprogesterone acetate injectable suspension
104 mg/0.65 mL
WHAT IS THE MOST IMPORTANT INFORMATION I SHOULD KNOW ABOUT depo-subQ provera 104?
Use of depo-subQ provera 104 may cause you to lose calcium stored in your bones. The longer you use depo-subQ provera 104 the more calcium you are likely to lose. The calcium may not return completely once you stop using depo-subQ provera 104.
Loss of calcium may cause weak, porous bones (osteoporosis) that could increase the risk that your bones might break, especially after menopause. It is not known whether your risk of developing osteoporosis may be greater if you are a teenager when you start to use depo-subQ provera 104.
You should use depo-subQ provera 104 long-term (for example, more than 2 years) only if other methods of birth control are not right for you.
depo-subQ provera 104 does not protect you from HIV (AIDS) and other diseases spread through sex (STDs).
WHAT IS depo-subQ provera 104?
depo-subQ provera 104 is a drug for birth control. It also helps relieve pain related to endometriosis (en-do-ME-tree-OH-sis). Symptoms of endometriosis arise when cells normally inside your uterus grow outside the uterus. The cells respond to menstrual cycle hormones, and may cause painful periods, pelvic pain, and painful sex.
depo-subQ provera 104 contains a hormone called medroxyprogesterone acetate (MPA). It is given as a shot (injection) every 3 months. Three months is the same as 12 to 14 weeks.
HOW WELL DOES depo-subQ provera 104 WORK FOR PREVENTING PREGNANCY?
When you use depo-subQ provera 104 correctly, the chance of getting pregnant is very low. In studies, no women became pregnant during the year they used depo-subQ provera 104 injection.
The list below estimates the chances of getting pregnant using different types of birth control. The numbers are based on typical use. Typical use includes people who use the method correctly and people who use the method incorrectly. The list shows the number of women out of 100 women who will likely get pregnant if they use the method for one year.
| Method |
Typical chance of getting pregnant in 1 year (No. of pregnancies in 100 women) |
|---|---|
| Shot | Less than 1 |
| Implant | |
| Female sterilization | |
| Male sterilization | |
| IUD (copper IUD and levonorgestrel IUD) | |
| Pill | 5 |
| Condom alone (male) | 14 |
| Withdrawal | 19 |
| Diaphragm with spermicides | 20 |
| Condom alone (female) | 21 |
| Periodic abstinence | 25 |
| Spermicides alone | 26 |
| Vaginal sponge or Cervical cap with spermicide | 20 to 40 |
HOW WILL I GET depo-subQ provera 104?
depo-subQ provera 104 is given as a shot just under the skin on your thigh or belly. You get it once every 3 months.
For Birth Control:
First Shot:
Your healthcare provider will want to be sure that you are not pregnant before you get your first shot. Normally, you get the shot by the 5th day from the START of your menstrual period. You get it whether or not you are still bleeding.
If you are breast-feeding, you may have your first shot as early as 6 weeks after you deliver your baby.
After the first shot:
It is very important to keep getting depo-subQ provera 104 every 3 months. If you wait more than 14 weeks between shots, you could become pregnant. Your healthcare provider must make sure you are not pregnant before you get your next shot.
When you get your shot, make an appointment for your next shot. Mark it on your calendar.
If you need a birth control method for more than two years, your healthcare provider may ask you to have a test of your bones or ask you to switch to another birth control method before continuing depo-subQ provera 104, especially if you have other risks for weak bones.
For Endometriosis:
If you have regular periods, you get depo-subQ provera 104 the same way as described above for birth control. If your periods have stopped or are not regular, your healthcare provider must test to make sure you are not pregnant before you get your first shot.
It is not recommended that you receive depo-subQ provera 104 for treatment of endometriosis for longer than two years. If your painful symptoms return after stopping treatment, your healthcare provider should ask you to have a test of your bones before restarting treatment.
WHAT IF I MISS A SHOT?
- If you miss a shot, or wait longer than 14 weeks between shots, you could get pregnant. The longer you wait, the greater the risk of getting pregnant.
- Talk with your healthcare provider to find out when to restart depo-subQ provera 104. You should be tested to be sure you are not pregnant.
- Use another kind of nonhormonal birth control, such as condoms, until you start depo-subQ provera 104 again.
DO NOT TAKE depo-subQ provera 104 IF YOU…
- Are pregnant or might be pregnant
- Have any unexplained vaginal bleeding
- Ever had breast cancer
- Ever had serious blood clots, such as blood clots in your legs (deep venous thrombophlebitis), lungs (pulmonary embolism), heart (heart attack), or head (stroke)
- Have liver disease
- Are allergic to anything in depo-subQ provera 104. (There is a list of what is in depo-subQ provera 104 at the end of this leaflet.)
BEFORE TAKING depo-subQ provera 104
Your healthcare provider may do a physical examination and check your blood and urine.
Tell your healthcare provider about all your medical conditions.
Most important, tell your healthcare provider if you:
- Are pregnant or might be pregnant. You should not get depo-subQ provera 104 if you are pregnant.
- Plan to become pregnant in the next year. After you stop getting depo-subQ provera 104, it takes time for your body to be able to get pregnant. It can be as early as 1 week after the last shot wears off. Most likely it will take up to 1 year or longer for you to get pregnant.
- Have breast cancer in your family
- Have an abnormal mammogram (breast X-ray), lumps in your breast, or bleeding from your nipples
- Have irregular, light, or heavy menstrual periods
- Have or had any of the following medical problems:
– Kidney problems
– High blood pressure
– Migraine headaches
– Asthma
– Seizures
– Diabetes, or if it runs in your family
– Depression
– Heart attack, stroke, or developed blood clots
– Bone disease
– Anorexia nervosa (an eating disorder)
– A strong family history of osteoporosis
– Drug use that can lower the amount of calcium in bones (drugs for epilepsy or steroids)
– Drinking a lot of alcohol or smoking a lot
It is important to see your healthcare provider regularly if you have any of these conditions.
Tell your healthcare provider about all the medicines you take. This includes prescription and over-the-counter medicines, vitamins, and herbal products.
WHAT ELSE SHOULD I KNOW ABOUT TAKING depo-subQ provera 104?
Other Birth Control. If you can't take birth control pills or can't use a birth control patch or ring, you may be able to use depo-subQ provera 104. Ask your healthcare provider.
Pregnancy. When you take depo-subQ provera 104 every 3 months, your chance of getting pregnant is very low. You could miss a period or have a light period and not be pregnant. If you miss 1 or 2 periods and think you might be pregnant, see your healthcare provider as soon as possible.
You should not use depo-subQ provera 104 if you are pregnant. However, depo-subQ provera 104 taken by accident during pregnancy does not seem to cause birth defects.
Pregnancy in your tubes (Ectopic Pregnancy). If you have severe pain low in your belly, tell your healthcare provider right away. Infrequently, a baby may start to grow outside the uterus, most often in the tubes.
Nursing a baby. Wait at least 6 weeks after your baby is born to start depo-subQ provera 104. You can use depo-subQ provera 104 if you are nursing.
- It does not lower the amount of milk you can make.
- It can pass through breast milk into your baby, but it is not harmful.
Blood or urine tests. depo-subQ provera 104 may affect blood or urine test results. Tell your healthcare provider you are taking depo-subQ provera 104 if you are going to have blood or urine tests.
Other medicines. depo-subQ provera 104 may not work as well if you are also taking Cytadren (aminoglutethimide), a cancer medicine. You may need to use another kind of birth control.
WHAT ARE THE MOST SERIOUS RISKS OF depo-subQ provera 104?
-
Losing calcium from your bones. depo-subQ provera 104 use may decrease the amount of calcium in your bones. The longer you use depo-subQ provera 104, the more calcium you are likely to lose. This increases the risk of your bones weakening if you use depo-subQ provera 104 continuously for a long time (for example, if you use depo-subQ provera 104 for more than two years). The loss of calcium may increase your risk of osteoporosis and broken bones, particularly after your menopause.
Calcium is generally added to the bones during teenage years. The decrease of calcium in your bones is of most concern if you are a teenager or have the following risk factors:
– Bone disease
– Anorexia nervosa (an eating disorder)
– A strong family history of osteoporosis
– Drug use that can lower the amount of calcium in bones (drugs for epilepsy or steroids), or
– Drinking a lot of alcohol or smoking a lot
If you need a birth control method for more than two years, your healthcare provider may ask you to have a test of your bones or ask you to switch to another birth control method before continuing depo-subQ provera 104, especially if you have other risks for weak bones. When depo-subQ provera 104 is stopped, the calcium in your bones begins to come back. The lost calcium may not return completely once you stop using depo-subQ provera 104. Your healthcare provider may tell you to take calcium and Vitamin D as this may lessen the loss of calcium from your bones.
- Abnormal or very heavy bleeding. If you start having very heavy or very long periods, tell your healthcare provider.
- Liver problems. Your healthcare provider may stop depo-subQ provera 104 if you have liver problems. Some signs of liver problems are yellow skin or eyes, feeling like you have the flu, feeling more tired than usual, and itching. Tell your healthcare provider if you have these symptoms.
- Allergic reaction. Allergic reactions to depo-subQ provera 104 are not common. If you have hives, problems breathing, or just do not feel right after your shot, call your healthcare provider or go to the Emergency Room right away.
-
Serious blood clots. Call your healthcare provider immediately if you:
– Have sharp chest pain, cough blood, or suddenly have trouble breathing
– Have a sudden severe headache with vomiting, blindness or trouble talking, weakness, or
numbness in an arm or leg, or get dizzy or faint– Have swelling or severe pain in your leg
WHAT ARE COMMON SIDE EFFECTS OF depo-subQ provera 104?
The most common side effects are:
- Changes in your monthly periods. You may not know when you will bleed, your periods may not be regular, you may have heavy bleeding, or you may have spotting. You may have more days of bleeding during the first 2 or 3 months after you start depo-subQ provera 104. Over time, you may have less and less bleeding. Many women stop having periods by the end of one year. Your periods will come back eventually after you stop using depo-subQ provera 104.
- Weight gain. In studies, women gained an average of 3 to 4 pounds during the first year they used depo-subQ provera 104. After 2 years of using depo-subQ provera 104, women gained an average of 7 to 8 pounds. Some women gained more, some gained less, some lost, and some stayed the same. Weight changes beyond 2 years of use with depo-subQ provera 104 have not been studied. Women who used a similar birth control product for 5 years gained on average 5 pounds more than women who did not use a hormone contraceptive product.
- Skin reaction where you got the shot. Lumps, skin dimpling, or pain are usually mild and usually don't last long. Scarring is unusual, but may happen. If there is swelling or your skin gets hot, has pus or looks bruised one or more days after your shot, call your healthcare provider.
- Headache.
Women using depo-subQ provera 104 for birth control or endometriosis had these less common side effects: abdominal pain, acne, breast tenderness, being irritable, depression, hot flushes, insomnia, joint pain, lack of energy, less sex drive, painful periods, nausea and sleepiness.
If you feel you are having other side effects, talk with your healthcare provider.
DOES depo-subQ provera 104 CAUSE CANCER?
- Birth control like depo-subQ provera 104 was studied in women for many years. In general, the risk of breast cancer slightly increased or stayed about the same as in women not using birth control like depo-subQ provera 104.
- The risk of cancer of the ovary, liver, or cervix did not change.
- There is a decreased risk of cancer of the uterus (endometrial cancer).
WHAT IF I WANT TO BECOME PREGNANT?
Plan ahead. The effect of depo-subQ provera 104 can last for a long time after you stop getting shots. Although you may be able to get pregnant quickly, it is more likely to take a year or longer after your last shot before you get pregnant.
It's best to see your healthcare provider for a pre-pregnancy check-up. Your healthcare provider may also tell you to take a vitamin called folic acid every day if you are planning to become pregnant.
GENERAL ADVICE ABOUT depo-subQ provera 104
For more information about depo-subQ provera 104, ask your healthcare provider or pharmacist. You can also visit www.depo-subQprovera104.com or call 1-866-554 DEPO (3376). A nurse can answer questions in Spanish or English 24 hours-a-day, 7 days a week.
WHAT IS IN depo-subQ provera 104?
Active ingredient: medroxyprogesterone acetate
Inactive ingredients: methylparaben, propylparaben, sodium chloride, polyethylene glycol, polysorbate 80, monobasic sodium phosphate∙H2O, dibasic sodium phosphate∙12H2O, methionine, povidone, water for shot. When necessary, the pH is adjusted with sodium hydroxide or hydrochloric acid, or both.
This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com
Rx only

LAB-0298-3.0
August 2013
PRINCIPAL DISPLAY PANEL - 104 mg Syringe Label
depo-subQ
provera 104™
medroxyprogesterone acetate injectable
suspension (104 mg/0.65 mL for subcutaneous use)
104 mg/0.65 mL
0.65 mL Single Use Syringe
Store at 20° to 25°C (68° to 77°F).
Shake vigorously before use.
Pfizer
Pharmacia & Upjohn Co
MADE IN USA (includes
foreign content)
LOT/EXP:
8Q2334

PRINCIPAL DISPLAY PANEL - 104 mg Syringe Carton
NDC 0009-4709-13
Single Use 0.65 mL Prefilled Syringe
Rx only
depo-subQ provera 104™
medroxyprogesterone acetate injectable suspension
(104 mg/0.65 mL for subcutaneous use)
104 mg/0.65 mL
Pfizer
Distributed by
Pharmacia & Upjohn Co
Division of Pfizer Inc, NY, NY 10017
MADE IN USA (includes foreign content)

Depo-SubQ Proveramedroxyprogesterone acetate INJECTION, SUSPENSION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||