DECAVAC
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use DECAVAC (Tetanus and Diphtheria Toxoids Adsorbed) safely and effectively. See full prescribing information for DECAVAC. DECAVAC (Tetanus and Diphtheria Toxoids Adsorbed) Suspension for Intramuscular Injection Initial U.S. Approval: 1955RECENT MAJOR CHANGES Warnings and Precautions ( 5.2 ) [01/2011] INDICATIONS AND USAGEDECAVAC is a vaccine indicated for active immunization for the prevention of tetanus and diphtheria. DECAVAC is approved for use in persons 7 years of age and older. (1)DOSAGE AND ADMINISTRATION Each 0.5 mL dose should be administered intramuscularly. (2.1) Primary immunization consists of 3 doses. The first two doses are administered at least 4 weeks apart and the third dose is administered at least 6 months after the second dose. (2.1) Routine booster immunization against tetanus and diphtheria is recommended at 11-12 years of age and every 10 years thereafter. (2.1) DOSAGE FORMS AND STRENGTHS Suspension for injection supplied in 0.5 mL single-dose vials or syringes. (3) CONTRAINDICATIONS Severe allergic reaction (eg, anaphylaxis) after a previous dose of DECAVAC or any other tetanus toxoid or diphtheria toxoid containing vaccine or any other component of this vaccine. (4.1) WARNINGS AND PRECAUTIONS The tip caps of the prefilled syringes may contain natural rubber latex which may cause allergic reactions in latex sensitive individuals. (5.2) More frequent administration of DECAVAC than described in Dosage and Administration may be associated with increased incidence and severity of adverse reactions. (5.3) Persons who experienced an Arthus-type hypersensitivity reaction following a prior dose of a tetanus toxoid-containing vaccine should not receive DECAVAC less than 10 years since the last dose of tetanus toxoid-containing vaccine, even for tetanus prophylaxis as part of wound management. (5.4) If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome may be increased following DECAVAC. (5.5) Side Effects The most frequent solicited injection site reaction following DECAVAC was pain, reported in 71% of adolescents 11-17 years of age and in 63% of adults 18-64 years of age. (6.1) The most frequent solicited systemic adverse event following DECAVAC was headache, reported in 40% of adolescents 11-17 years of age and in 34% of adults 18-64 years of age. (6.1) Injection site swelling, injection site erythema, body ache or muscle weakness, tiredness, and diarrhea also were reported commonly (≥10%) in both age groups; chills, nausea, and sore and swollen joints were reported commonly (≥ 10%) in adolescents. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Sanofi Pasteur Inc. at 1-800-822-2463 (1-800-VACCINE) or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.DRUG INTERACTIONS No safety and immunogenicity data are available on concomitant administration of DECAVAC with other US licensed vaccines. (7.1) Immunosuppressive therapies may reduce the immune response to DECAVAC. (7.2)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1. DECAVAC INDICATIONS AND USAGE
- 2. DECAVAC DOSAGE AND ADMINISTRATION
- 3. DOSAGE FORMS AND STRENGTHS
- 4. DECAVAC CONTRAINDICATIONS
- 5. WARNINGS AND PRECAUTIONS
- 6. DECAVAC ADVERSE REACTIONS
- 7. DRUG INTERACTIONS
- 8. USE IN SPECIFIC POPULATIONS
- 11. DECAVAC DESCRIPTION
- 12. CLINICAL PHARMACOLOGY
- 13. NON-CLINICAL TOXICOLOGY
- 14. CLINICAL STUDIES
- 15. REFERENCES
- 16. HOW SUPPLIED/STORAGE AND HANDLING
- 17. PATIENT COUNSELING INFORMATION
FULL PRESCRIBING INFORMATION
1. INDICATIONS AND USAGE
DECAVAC® is a vaccine indicated for active immunization for the prevention of tetanus and diphtheria. DECAVAC vaccine is approved for use in persons 7 years of age and older.
2. DOSAGE AND ADMINISTRATION
2.1. Dosage and Schedule
Primary Immunization
DECAVAC vaccine may be used in persons 7 years of age and older who have not been immunized previously against tetanus and diphtheria or who have begun a primary immunization series but did not complete it. The primary immunization series consists of three 0.5 mL doses. The first two doses are administered at least 4 weeks apart and the third dose is administered at least 6 months after the second dose.
DECAVAC vaccine may be used to complete the primary immunization series for tetanus and diphtheria in persons 7 years of age or older who have received one or two doses of Diphtheria and Tetanus Toxoids and Pertussis Vaccine Adsorbed (whole-cell DTP), Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and/or Diphtheria and Tetanus Toxoids Adsorbed (DT). However, the safety and efficacy of DECAVAC vaccine in such regimens have not been evaluated.
Routine Booster Immunization
DECAVAC vaccine may be used for routine booster immunization against tetanus and diphtheria in persons 7 years of age and older who have completed primary immunization against tetanus and diphtheria. Routine booster immunization against tetanus and diphtheria is recommended in children 11-12 years of age and every 10 years thereafter. (1)
Tetanus Prophylaxis in Wound Management
For active tetanus immunization in wound management of patients 7 years of age and older, a preparation containing tetanus and diphtheria toxoids is preferred instead of single-antigen tetanus toxoid to enhance diphtheria protection. (2) DECAVAC vaccine is approved for wound management of patients 7 years of age and older.
The need for active immunization with a tetanus toxoid-containing preparation, with or without Tetanus Immune Globulin (TIG) (Human) depends on both the condition of the wound and the patient's vaccination history (Table 1).
When indicated, TIG (Human) should be administered using a separate needle and syringe at a different anatomic site, according to the manufacturer's package insert. If a contraindication to using a tetanus toxoid-containing vaccine exists in a person who has not completed tetanus primary immunization and other than a clean, minor wound is sustained, only passive immunization with TIG (Human) should be given. (2)
| History of Adsorbed Tetanus Toxoid (doses) | Clean, Minor Wounds | All Other Wounds |
||
|---|---|---|---|---|
| Td | TIG | Td | TIG | |
|
Unknown or |
Yes | No | Yes | Yes |
≥three
 |
No |
No | No |
No |
Diphtheria Prophylaxis for Case Contacts
DECAVAC vaccine may be used for post-exposure diphtheria prophylaxis in persons 7 years of age and older who have not completed primary vaccination, whose vaccination status is unknown, or who have not been vaccinated with diphtheria toxoid within the previous 5 years. Consult ACIP recommendations for additional interventions for post-exposure diphtheria prophylaxis. (2)
2.2. Administration
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If these conditions exist, DECAVAC vaccine should not be administered.
DECAVAC vaccine, after shaking, is a turbid liquid, whitish-gray in color.
For DECAVAC vaccine supplied in vials, shake the vial well before withdrawing the dose. Discard vial if DECAVAC vaccine cannot be resuspended.
For DECAVAC vaccine supplied in syringes, shake the syringe well before administering the dose. Discard syringe if DECAVAC vaccine cannot be resuspended.
Inject 0.5 mL intramuscularly. The preferred site is the deltoid muscle. DECAVAC vaccine should not be injected into the gluteal area or areas where there may be a major nerve trunk.
Do not administer DECAVAC vaccine intravenously or subcutaneously.
DECAVAC vaccine should not be combined through reconstitution or mixed with any other vaccine.
3. DOSAGE FORMS AND STRENGTHS
DECAVAC vaccine is a sterile suspension for injection available in 0.5 mL single-dose vials or syringes.
4. CONTRAINDICATIONS
4.1. Hypersensitivity
A severe allergic reaction (eg, anaphylaxis) after a previous dose of DECAVAC vaccine or any other tetanus toxoid or diphtheria toxoid containing vaccine or any other component of this vaccine is a contraindication to administration of DECAVAC vaccine. [See Description (11).] Because of uncertainty as to which component of the vaccine may be responsible, no further vaccination with diphtheria or tetanus components should be carried out. Alternatively, such individuals may be referred to an allergist for evaluation if further immunizations are to be considered.
5. WARNINGS AND PRECAUTIONS
5.1. Management of Acute Allergic Reactions
Epinephrine injection (1:1000) and other appropriate agents and equipment must be immediately available should an acute anaphylactic reaction occur.
5.2. Latex
The tip caps of the DECAVAC prefilled syringes may contain natural rubber latex, which may cause allergic reactions in latex-sensitive individuals.
5.3. Frequency of Administration
More frequent administration of DECAVAC vaccine than described in Dosage and Administration [see Dosage and Administration (2.1) ] may be associated with increased incidence and severity of adverse reactions.
5.4. Arthus Reactions
Persons who experienced an Arthus-type hypersensitivity reaction following a prior dose of a tetanus-toxoid containing vaccine usually have high serum tetanus antitoxin levels and should not receive DECAVAC vaccine more frequently than every 10 years, even for tetanus prophylaxis as part of wound management [see Dosage and Administration (2.1) ].
5.5. Guillain-Barré Syndrome and Brachial Neuritis
A review by the Institute of Medicine found evidence for a causal relation between tetanus toxoid and both brachial neuritis and Guillain-Barré syndrome. (3) If Guillain-Barré syndrome occurred within 6 weeks after receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome may be increased following DECAVAC vaccine.
5.6. Limitations of Vaccine Effectiveness
Vaccination with DECAVAC vaccine may not protect all individuals.
5.7. Altered Immunocompetence
Immune responses to inactivated vaccines and toxoids when given to immunocompromised persons may be suboptimal. The immune response to DECAVAC vaccine administered to immunocompromised individuals (whether from disease or treatment) has not been studied.
6. ADVERSE REACTIONS
6.1. Data from Clinical Studies
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to vaccine use and for approximating rates.
6.2. Primary Immunization
In a clinical study, 42 persons 6-58 years of age underwent primary immunization against tetanus and diphtheria. Eight of these participants (19%) noted local reactions consisting of pain and tenderness, induration, and erythema at the injection site; none reported systemic symptoms. (4)
6.3. Booster Immunization
In a clinical study, 792 adolescents 11-17 years of age and 573 adults 18-64 years of age received a booster dose with DECAVAC vaccine. Study participants had not received tetanus or diphtheria toxoid-containing vaccines within the previous 5 years. Solicited local reactions and systemic adverse events were monitored daily for 14 days post-vaccination using subject diary cards. Serious adverse events were monitored through 6 months post-vaccination. Ninety-seven percent of participants who received DECAVAC vaccine completed the 6-month telephone follow-up.
Solicited Adverse Events
The frequency of selected solicited injection site reactions (pain, swelling, or erythema) occurring during Days 0-14 following booster vaccination with DECAVAC vaccine in adolescents 11 through 17 years of age, and adults 18 through 64 years of age are presented in Table 2. Pain at the injection site was the most common adverse reaction occurring in 71% of adolescents and 62.9% of adults.
| Adverse Event | Adolescents 11-17 years N  |
Adults 18-64 years N  |
|
|---|---|---|---|
| Injection Site Pain | Any | 71.0 | 62.9 |
Moderate |
15.6 | 10.2 | |
Severe |
0.6 | 0.9 | |
| Injection Site Swelling | Any | 18.3 | 17.3 |
| Moderate | |||
| 1.0 to 3.4 cm | 5.7 | 5.4 | |
| Severe | |||
| ≥3.5 cm | 5.5 | 5.5 | |
| ≥5 cm | 3.6 | 2.7 | |
| Injection Site Erythema | Any | 19.7 | 21.6 |
| Moderate | |||
| 1.0 to 3.4 cm | 4.6 | 8.4 | |
| Severe | |||
| ≥3.5 cm | 5.3 | 4.8 | |
| ≥5 cm | 2.9 | 3.0 | |
The frequency of solicited systemic adverse events occurring during Days 0-14 following booster vaccination with DECAVAC vaccine are presented in Table 3. Headache was the most frequent solicited systemic adverse event, and was usually of mild or moderate intensity.
| Adverse Event | Adolescents 11-17 years | Adults 18-64 years | ||
|---|---|---|---|---|
N |
N |
|||
| Headache | Any | 40.4 | 34.1 | |
Moderate
 |
11.1 | 10.5 | ||
Severe
 |
1.5 | 2.1 | ||
|
Body Ache or Muscle Weakness |
Any | 29.9 | 18.8 | |
Moderate
 |
6.9 | 5.7 | ||
Severe
 |
0.9 | 0.9 | ||
| Tiredness | Any | 27.3 | 20.7 | |
Moderate
 |
7.5 | 6.1 | ||
Severe
 |
1.0 | 0.5 | ||
| Chills | Any | 12.6 | 6.6 | |
Moderate
 |
2.5 | 1.6 | ||
Severe
 |
0.1 | 0.5 | ||
| Nausea | Any | 12.3 | 7.9 | |
Moderate
 |
3.2 | 1.8 | ||
Severe
 |
0.6 | 0.5 | ||
|
Sore and Swollen Joints |
Any | 11.7 | 7.0 | |
Moderate
 |
2.5 | 2.1 | ||
Severe
 |
0.1 | 0.5 | ||
| Diarrhea | Any | 10.2 | 11.3 | |
Moderate
 |
2.0 | 2.7 | ||
Severe
 |
0.0 | 0.5 | ||
|
Lymph Node Swelling |
Any | 5.3 | 4.1 | |
Moderate
 |
0.5 | 0.5 | ||
Severe
 |
0.0 | 0.0 | ||
| Vomiting | Any | 2.8 | 1.8 | |
Moderate
 |
1.1 | 0.9 | ||
Severe
 |
0.3 | 0.2 | ||
| Fever | Any ≥38.0°C (≥100.4°F) | 2.7 | 1.1 | |
|
≥38.8°C to ≤39.4°C (≥102.0°F to ≤103.0°F) |
0.6 | 0.2 | ||
| ≥39.5°C (≥103.1°F) | 0.1 | 0.2 | ||
| Rash | Any | 2.0 | 2.3 | |
Serious Adverse Events
Among 792 adolescents 11-17 years of age and 573 adults 18-64 years of age who received a booster dose with DECAVAC vaccine, 2 adolescents and 2 adults reported a serious adverse event that occurred within 30 days following vaccination. Events reported in adolescents were jaw fracture secondary to trauma and abdominal pain/appendectomy. Events reported in adults were atrial septal defect and elective surgical repair in one subject, and myocardial infarction in one subject with a history of coronary artery disease.
6.4. Post-Marketing Experience
The following adverse events have been spontaneously reported during the post-marketing use of Td manufactured by Sanofi Pasteur Inc. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccination. The following adverse events were included based on severity, frequency of reporting or the strength of causal association with DECAVAC vaccine.
-
Blood and Lymphatic System Disorders
Lymphadenopathy.
-
Immune System Disorders
Allergic reactions (such as rash, urticaria, pruritus, and angioedema), including anaphylactic reactions.
-
Nervous System Disorders
Headache, paresthesia, dizziness, syncope, and convulsions.
-
Gastrointestinal Disorders
Nausea, vomiting.
-
Musculoskeletal, Connective Tissue and Bone Disorders
Myalgia, arthralgia, pain in extremities, musculoskeletal stiffness.
-
General Disorders and Administration Site Conditions
Injection site reactions (including swelling, redness, warmth, induration, cellulitis, and nodules).
Pyrexia, chills, pain, malaise, asthenia, fatigue, edema peripheral.
7. DRUG INTERACTIONS
7.1. Concomitant Administration with Other Vaccines
No safety and immunogenicity data are available regarding concomitant administration of DECAVAC vaccine with other US licensed vaccines.
7.2. Immunosuppressive Treatments
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs and corticosteroids (used in greater than physiologic doses), may reduce the immune response to DECAVAC vaccine.
7.3. Tetanus Immune Globulin (Human)
If passive protection against tetanus is required, TIG (Human) may be administered according to its prescribing information, concomitantly with DECAVAC vaccine at a separate site with a separate needle and syringe. [See Dosage and Administration (2.1).]
8. USE IN SPECIFIC POPULATIONS
8.1. Pregnancy
Pregnancy Catergory C: Animal reproduction studies have not been conducted with DECAVAC vaccine. It is also not known whether DECAVAC vaccine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. DECAVAC vaccine should be given to a pregnant woman only if clearly needed.
8.3. Nursing Mothers
It is not known whether DECAVAC vaccine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when DECAVAC vaccine is administered to a nursing woman.
8.4. Pediatric Use
DECAVAC vaccine is not approved for use in infants and children younger than 7 years of age. Safety and effectiveness of DECAVAC vaccine in this age group have not been established.
8.5. Geriatric Use
Clinical studies of DECAVAC vaccine did not include subjects aged 65 years and over to determine whether they respond differently than younger subjects.
11. DESCRIPTION
DECAVAC vaccine, Tetanus and Diphtheria Toxoids Adsorbed, for intramuscular injection, is a sterile suspension of alum (aluminum potassium sulfate)-precipitated toxoids in an isotonic sodium chloride solution. The vaccine, after shaking, is a turbid liquid, whitish-gray in color.
Corynebacterium diphtheriae cultures are grown in a modified Mueller and Miller medium. (5) Clostridium tetani cultures are grown in a peptone-based medium containing an extract of bovine muscle tissue. The bovine muscle tissue used in this medium is US sourced. Tetanus and diphtheria toxins produced during the growth of the cultures are detoxified with formaldehyde. The detoxified materials are then separately purified by serial ammonium sulfate fractionation and diafiltration, and adsorbed onto alum.
Each 0.5 mL dose of DECAVAC vaccine is formulated to contain the following active ingredients: 5 Lf of tetanus toxoid and 2 Lf of diphtheria toxoid. The tetanus and diphtheria toxoids induce at least 2 units and 0.5 units of antitoxin per mL of serum, respectively, in the guinea pig potency test. Each 0.5 mL dose also contains a trace amount of thimerosal [mercury derivative, (≤0.3 mcg mercury/dose) not as a preservative] from the manufacturing process, aluminum potassium sulfate adjuvant (not more than 0.28 mg aluminum by assay), and not more than 100 mcg (0.02%) of residual formaldehyde.
The tip caps of the prefilled syringes may contain natural rubber latex. No other components of any presentation contain latex.
12. CLINICAL PHARMACOLOGY
12.1. Tetanus
Tetanus is an acute and often fatal disease caused by an extremely potent neurotoxin produced by C tetani. Protection against disease is due to the development of neutralizing antibodies to tetanus toxin. A serum tetanus antitoxin level of 0.01 IU/mL, measured by neutralization assays, is considered the minimum protective level. (6) (7) A tetanus antitoxoid level ≥0.1 IU/mL as measured by the enzyme-linked immunosorbent assay (ELISA) used in the booster immunization study of DECAVAC vaccine is considered protective [see Clinical Studies (14.2) ].
12.2. Diphtheria
Diphtheria is an acute toxin-mediated disease caused by toxigenic strains of C diphtheriae. Protection against disease is due to the development of neutralizing antibodies to diphtheria toxin. A serum diphtheria antitoxin level of 0.01 IU/mL is the lowest level giving some degree of protection. (7) (8) A diphtheria antitoxin level of 0.1 IU/mL is generally regarded as protective. (8) Diphtheria antitoxin levels of ≥1.0 IU/mL have been associated with long-term protection. (8) Antibodies to diphtheria toxin were measured by a microneutralization assay in the booster immunization study of DECAVAC vaccine [see Clinical Studies (14.2) ].
13. NON-CLINICAL TOXICOLOGY
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been performed with DECAVAC vaccine to evaluate carcinogenicity, mutagenic potential, or impact on fertility.
14. CLINICAL STUDIES
14.1. Primary Immunization
The effectiveness of primary immunization with tetanus toxoid and diphtheria toxoid used in DECAVAC vaccine was determined on the basis of an immunogenicity study, with a comparison to a serological correlate of protection (0.01 antitoxin units/mL) established by the Panel on Review of Bacterial Vaccines & Toxoids. (7) A clinical study to evaluate the serological responses was performed in 58 individuals 6-58 years of age. Of these, 46 persons had no evidence of prior immunity to tetanus toxin and 47 persons had no evidence of prior immunity to diphtheria toxin. The results indicated protective levels of antibody were achieved in greater than 90% of the study population after primary immunization with both components. (4)
14.2. Booster Immunization
In a clinical study, the immune response to booster immunization with DECAVAC vaccine was evaluated in 516 adolescents 11-17 years of age and 509 adults 18-64 years of age. Participants had not received a tetanus or diphtheria toxoid-containing vaccine within the previous 5 years. Sera were obtained before and approximately 35 days after vaccination. Antibodies to tetanus toxoid were measured by an ELISA. Antibodies to diphtheria toxin were measured by a microneutralization assay. Seroprotection rates and booster response rates for tetanus are provided in Table 4. Seroprotection rates and booster response rates for diphtheria are provided in Table 5.
| Tetanus Antitoxoid (IU/mL) | ||||||
|---|---|---|---|---|---|---|
| Pre-Vaccination | 1 Month Post-Vaccination | |||||
| Age Group (years) |
N |
% ≥0.1 (95% CI) |
% ≥1.0 (95% CI) |
% ≥0.1 (95% CI) |
% ≥1.0 (95% CI) |
% Booster (95% CI) |
| 11-17 | 516 | 99.2 (98.0, 99.8) |
43.8 (39.5, 48.2) |
100.0 (99.3, 100.0) |
99.4 (98.3, 99.9) |
91.3 (88.5, 93.6) |
| 18-64 | 509 | 95.9 (93.8, 97.4) |
70.3 (66.2, 74.3) |
99.8 (98.9, 100.0) |
98.2 (96.7, 99.2) |
66.8 (62.5, 70.9) |
| Diphtheria Antitoxin (IU/mL) | ||||||
|---|---|---|---|---|---|---|
| Pre-Vaccination | 1 Month Post-Vaccination | |||||
| Age Group (years) |
N |
% ≥0.1 (95% CI) |
% ≥1.0 (95% CI) |
% ≥0.1 (95% CI) |
% ≥1.0 (95% CI) |
% Booster (95% CI) |
| 11-17 | 515-516 | 70.7 (66.5, 74.6) |
17.3 (14.1, 20.8) |
99.8 (98.9, 100.0) |
98.4 (97.0, 99.3) |
95.0 (92.7, 96.7) |
| 18-64 | 506-507 | 63.3 (59.0, 67.5) |
16.0 (12.9, 19.5) |
95.1 (92.8, 96.8) |
79.9 (76.1, 83.3) |
83.4 (79.9, 86.5) |
15. REFERENCES
-
1 CDC. General Recommendations on Immunization: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2011;60(RR-02):1-60. -
2 CDC. Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991:40(No. RR-10):1-28. -
3 Institute of Medicine (US). Stratton KR, et al, eds. Adverse events associated with childhood vaccines: evidence bearing on causality. Washington (DC): National Academy Press. 1994:67-117. -
4 Myers MG, et al. Primary immunization with tetanus and diphtheria toxoids. JAMA 248:1982;2478-2480. -
5 Mueller JH, et al. Production of diphtheria toxin of high potency (100 Lf) on a reproducible medium. J Immunol 40:1941;21-32. -
6 Wassilak SGF, et al. Tetanus toxoid. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 5th ed. Philadelphia, PA: WB Saunders Company;2008:805-839. -
7 Department of Health and Human Services, Food and Drug Administration. Biological Products; Bacterial Vaccines and Toxoids; Implementation of Efficacy Review; Proposed Rule. Federal Register Vol 50 No 240:1985; 51002-51117. -
8 Vitek CR and Wharton M. Diphtheria toxoid. In: Plotkin SA, Orenstein WA, Offit PA, editors. Vaccines. 5th ed. Philadelphia, PA: WB Saunders Company;2008:139-156.
16. HOW SUPPLIED/STORAGE AND HANDLING
16.1. How Supplied
Vial, 1 Dose (10 per package) – NDC 49281-291-83. Contains no latex.
Syringe, 1 Dose (10 per package, without needle) – NDC 49281-291-10. The tip caps of the prefilled syringes may contain natural rubber latex. No other components contain latex.
16.2. Storage and Handling
Store at 2° to 8°C (35° to 46°F). Do not freeze.
Do not use vaccine after expiration date.
17. PATIENT COUNSELING INFORMATION
Prior to administration of DECAVAC vaccine, health-care providers should inform the patient, parent, or guardian of the benefits and risks of immunization and of the importance of completing the primary immunization series or receiving recommended booster doses, as appropriate.
The health-care provider should inform the patient, parent, or guardian about the potential for adverse reactions that have been temporally associated with the administration of DECAVAC vaccine or other vaccines containing similar ingredients. Patients, parents or guardians should be instructed to report any suspected adverse reactions to their health-care provider.
The health-care provider should provide the Vaccine Information Statements which are required by the National Childhood Vaccine Injury Act of 1986 to be given with each immunization.
Product information
as of March 2011.
Manufactured by:
Sanofi Pasteur Inc.
Swiftwater PA 18370 USA
5876-5877
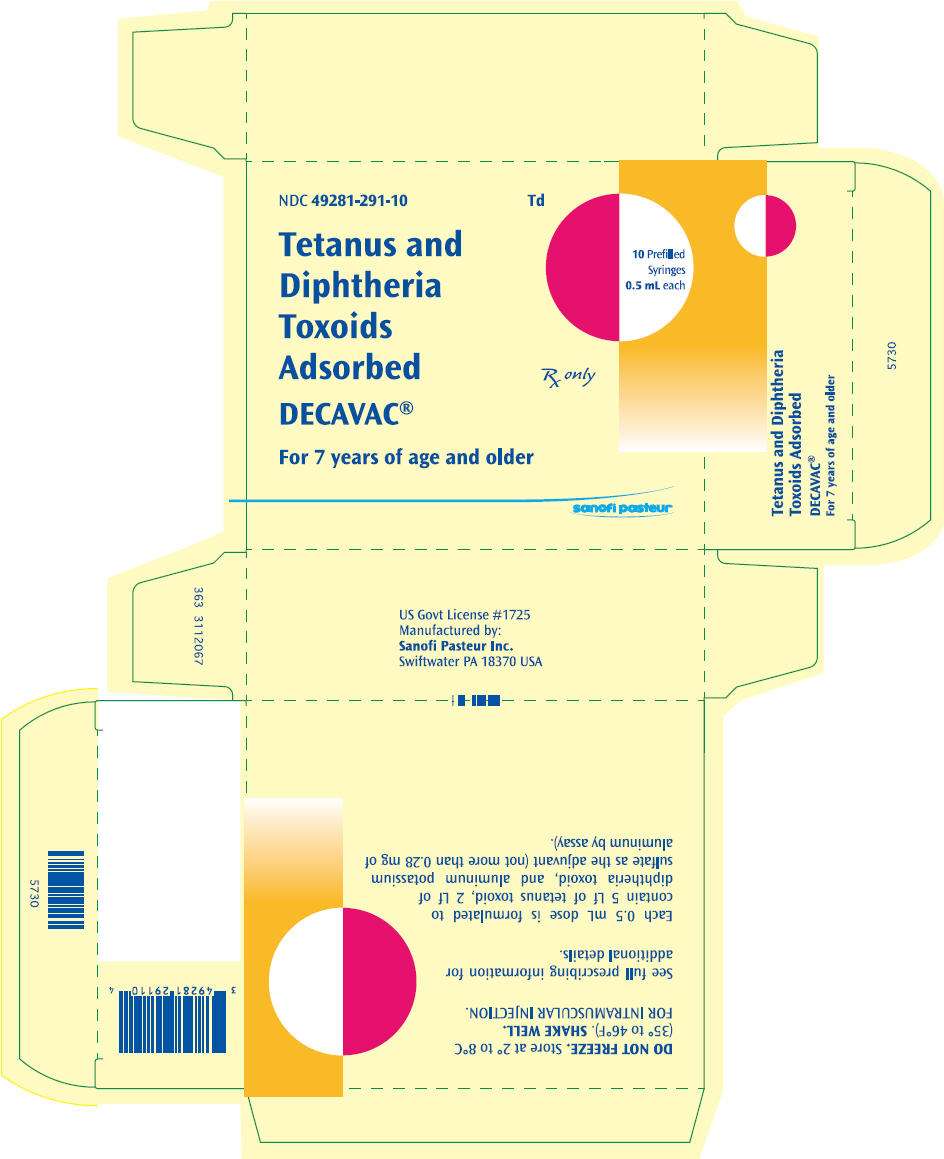
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Carton
NDC 49281-291-10
Tetanus and
Diphtheria
Toxoids
Adsorbed
DECAVAC®
For 7 years of age and older
Td
10 Prefilled
Syringes
0.5 mL each
Rx only
sanofi pasteur
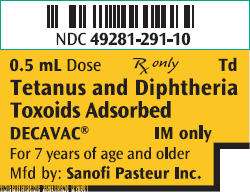
PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Label
NDC 49281-291-10
0.5 mL Dose
Rx only
Td
Tetanus and Diphtheria
Toxoids Absorbed
DECAVAC ®
IM only
For 7 years of age and older
Mfd by: Sanofi Pasteur Inc.
DECAVACCLOSTRIDIUM TETANI TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) and CORYNEBACTERIUM DIPHTHERIAE TOXOID ANTIGEN (FORMALDEHYDE INACTIVATED) SUSPENSION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||