Chenodal
Manchester Pharmaceuticals Inc.
Manchester Pharmaceuticals Inc.
Chenodal 250 mg (chenodiol tablets)
FULL PRESCRIBING INFORMATION: CONTENTS*
- SPECIAL NOTE
- CHENODAL DESCRIPTION
- CLINICAL PHARMACOLOGY
- PATIENT SELECTION
- Evaluation of Surgical Risk
- CHENODAL INDICATIONS AND USAGE
- CHENODAL CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- CHENODAL ADVERSE REACTIONS
- DRUG ABUSE AND DEPENDENCE
- CHENODAL DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
FULL PRESCRIBING INFORMATION

Rx only
NDC 45043-876-40
Chenodal 250 mg
(Chenodiol Tablets)
100 Tablets
Manchester Pharmaceuticals, Inc.
Each Film-Coated Tablet Contains: Chenodiol 250 mg
Usual Adult Dosage: Please see package insert for detailed prescribing information.
Store and Dispense: Store at 200 to 250C (680 to 770F). [see USP Controlled Room Temperature]. Dispense in a tight container as defined in the USP.
KEEP THIS AND ALL MEDICATION OUT OF THE REACH OF CHILDREN.
Manufactured for: Manchester Pharmaceuticals, Inc.
Fort Collins, CO 80525
866-758-7068
Bar code
45043 87640
Lot No.:
Exp. Date:
SPECIAL NOTE
CHENODAL DESCRIPTION
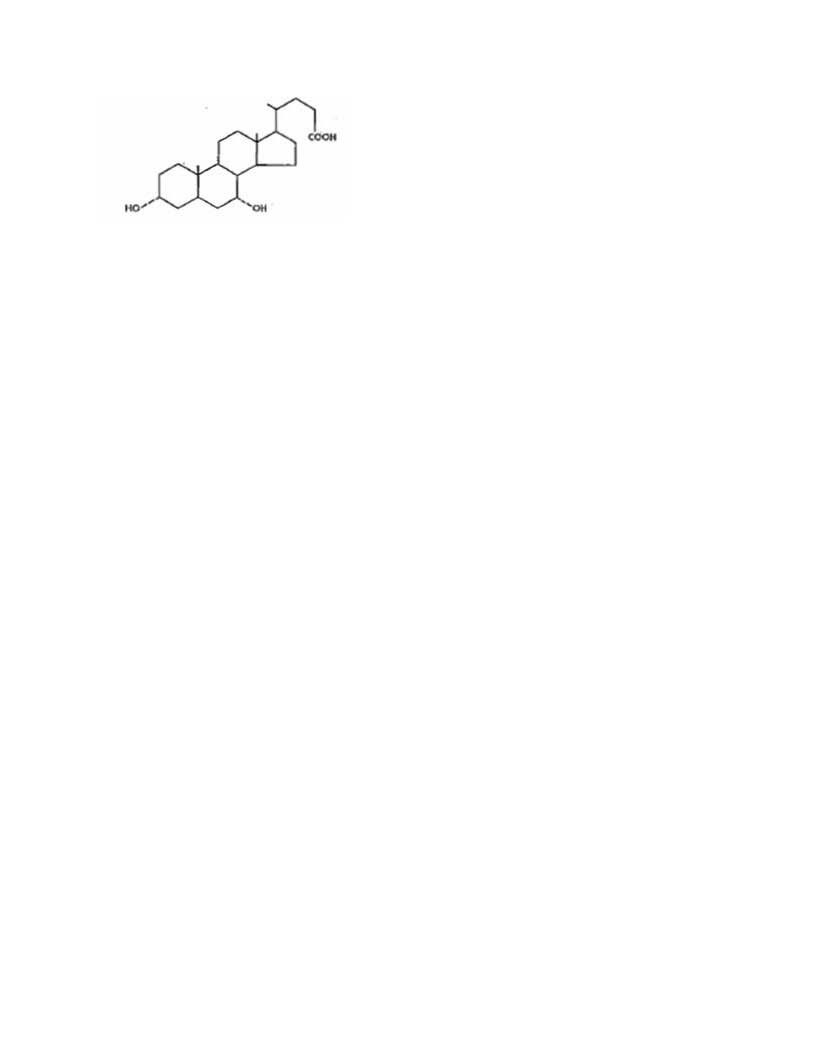
Chenodiol is the non-proprietary name for chenodeoxycholic acid,
a naturally occurring human bile acid. It is a bitter-tasting white powder
consisting of crystalline and amorphous particles freely soluble in methanol,
acetone and acetic acid and practically insoluble in water. Its chemical name is
3α, 7α-dihydroxy-5β-cholan-24-oic acid (C24H40O4), it has a molecular weight of
392.58, and its structure is shown below;
Chenodiol film-coated tablets for oral administration contain 250 mg of
chenodiol.
Inactive ingredients: pregelatinized starch; silicon dioxide;
microcrystalline cellulose, sodium starch glycollate; and magnesium stearate;
the thin-film coating contains: opadry YS-2-7035 [consisting of methylcellulose
and glycerin] and sodium lauryl sulfate
CLINICAL PHARMACOLOGY
At therapeutic doses, chenodiol suppresses hepatic synthesis of
both cholesterol and cholic acid, gradually replacing the latter and its
metabolite, deoxycholic acid in an expanded bile acid pool. These actions
contribute to biliary cholesterol desaturation and gradual dissolution of
radiolucent cholesterol gallstones in the presence of a gall-bladder visualized
by oral cholecystography. Chenodiol has no effect on radiopaque (calcified)
gallstones or on radiolucent bile pigment stones.
Chenodiol is well absorbed from the small intestine and taken up by the liver
where it is converted to its taurine and glycine conjugates and secreted in
bile. Owing to 60 % to 80% first-pass hepatic clearance, the body pool of
chenodiol resides mainly in the enterohepatic circulation; serum and urinary
bile acid levels are not significantly affected during chenodiol therapy.
At steady-state, an amount of chenodiol near the daily dose escapes to the
colon and is converted by bacterial action to lithocholic acid. About 80% of the
lithocholate is excreted in the feces; the remainder is absorbed and converted
in the liver to its poorly absorbed sulfolithocholyl conjugates. During
chenodiol therapy there is only a minor increase in biliary lithocholate, while
fecal bile acids are increased three- to fourfold.
Chenodiol is unequivocally hepatotoxic in many animal species, including
sub-human primates at doses close to the human dose. Although the theoretical
cause is the metabolite, lithocholic acid, an established hepatotoxin, and man
has an efficient mechanism for sulfating and eliminating this substance, there
is some evidence that the demonstrated hepatotoxicity is partly due to chenodiol
per se. The hepatotoxicity of
lithocholic acid is characterized biochemically and morphologically as
cholestatic.
Man has the capacity to form sulfate conjugates of lithocholic acid.
Variation in this capacity among individuals has not been well established and a
recent published report suggests that patients who develop chenodiol-induced
serum aminotransferase elevations are poor sulfators of lithocholic acid (see ADVERSE
REACTIONS and WARNINGS).
General Clinical Results
Floatable versus Nonfloatable Stones
A major finding in clinical trials was a difference between floatable and nonfloatable stones,
with respect to both natural history and response to chenodiol. Over the
two-year course of the National Cooperative Gallstone Study (NCGS), placebo –
treated patients with floatable stones (n = 47) had significantly higher rates
of biliary pain and cholecystectomy than patients with nonfloatable stones (n =
258) (47% versus 27% and 19%versus 4%, respectively). Chenodiol treatment (750
mg/day) compared to placebo was associated with a significant reduction in both
biliary pain and the cholecystectomy rates in the group with floatable stones
(27% versus 47% and 1.5% versus 19%, respectively). In an uncontrolled clinical
trial using 15 mg/kg/day, 70% of the patients with small (less than 15 mm)
floatable stones (n = 10) had complete confirmed dissolution.
In the NCGS in patients with nonfloatable stones, chenodiol produced no
reduction in biliary pain and showed a tendency to increase the cholecystectomy
rate (8% versus 4%). This finding was more pronounced with doses of chenodiol
below 10 mg/kg. The subgroup of patients with nonfloatable stones and a history
of biliary pain had the highest rates of cholecystectomy and aminotransferase
elevations during chenodiol treatment. Except for the NCGS subgroup with
pretreatment biliary pain, dose-related aminotransferase elevations and diarrhea
have occurred with equal frequency in patients with floatable or nonfloatable
stones. In the uncontrolled clinical trial mentioned above, 27% of the patients
with nonfloatable stones (n = 59) had complete confirmed dissolutions, including
35% with small (less than 15 mm)(n= 40) and only 11% with large, nonfloatable
stones (n= 19).
Of 916 patients enrolled NCGS, 17.6% had stones seen in upright form
(horizontal X-ray beam) to float in the dye-laden bile during oral
cholecystography using iopanoic acid. Other investigators report similar
findings. Floatable stones are not detected by ultrasonography in the absence
for dye. Chemical analysis has shown floatable stones to be essentially pure
cholesterol).
Other Radiographic and Laboratory Features
Radiolucent stones may have rims or centers of opacity representing
calcification. Pigment stones and partially calcified radiolucent stones do not
respond to chenodiol. Subtle calcification can sometimes be detected in flat
film X-rays, if not obvious in the oral cholecystogram. Among nonfloatable
stones, cholesterol stones are more apt than pigment stones to be smooth
surfaced, less than 0.5 cm in diameter, and to occur in numbers less than 10. As
stone size number and volume increase, the probability of dissolution within 24
months decreases. Hemolytic disorders, chronic alcoholism, biliary cirrhosis and
bacterial invasion of the biliary system predispose to pigment gallstone
formation. Pigment stones of primary biliary cirrhosis should be suspected in
patients with elevated alkaline phosphates, especially if positive
anti-mitochondrial antibodies are present. The presence of microscopic
cholesterol crystals in aspirated gallbladder bile, and demonstration of
cholesterol super saturation by bile lipid analysis increase the likelihood that
the stones are cholesterol stones.
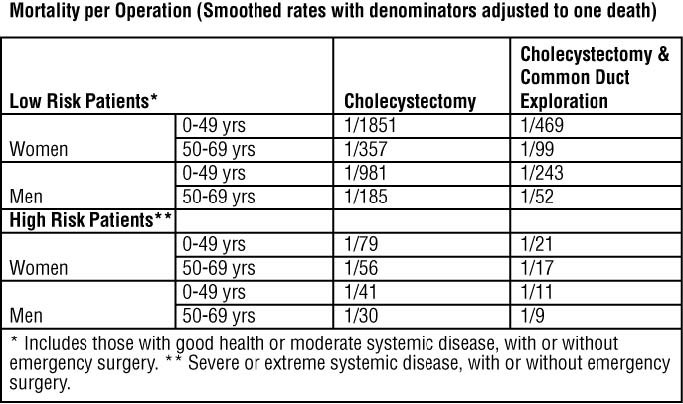
PATIENT SELECTION
Evaluation of Surgical Risk
CHENODAL INDICATIONS AND USAGE
Chenodal (chenodiol tablets) is indicated for patients with radiolucent stones in well-opacifying gallbladders, in whom selective surgery would be undertaken except for the presence of increased surgical risk due to systemic disease or age. The likelihood of successful dissolution is far greater if the stones are floatable or small. For patients with nonfloatable stones, dissolution is less likely and added weight should be given to the risk that more emergent surgery might result form a delay due to unsuccessful treatment. Safety of use beyond 24 months is not established. Chenodiol will not dissolve calcified (radiopaque) or radiolucent bile pigment stones.
CHENODAL CONTRAINDICATIONS
Pregnancy Category X
WARNINGS
PRECAUTIONS
Information for patients
Patients should be counseled on the importance of periodic visits
for liver function tests and oral cholecystograms (or ultrasonograms) for
monitoring stone dissolution; they should be made aware of the symptoms of
gallstone complications and be warned to report immediately such symptoms to the
physician. Patients should be instructed on ways to facilitate faithful
compliance with the dosage regimen throughout the usual long term of therapy,
and on temporary doses reduction if episodes of diarrhea occur.
Drug interactions
Carcinogenesis, mutagenesis, impairment of fertility
A two-year oral study of chenodiol in rats failed to show a
carcinogenic potential at the tested levels of 15 to 60 mg/kg/day (1 to 4 times
the maximum recommended human dose, MRHD). It has been reported that chenodiol
given in long-term studies at oral doses up to 600 mg/kg/day (40 times the MRHD)
to rats and 1000 mg/kg/day (65 times the MRHD) to mice induced benign and
malignant liver cell tumors in female rats and cholangiomata in female rats and
male mice. Two-year studies of lithocholic acid ( a major metabolite of
chenodiol) in mice (125 to 250 mg/kg/day) and rats (250 and 500 mg/kg/day) found
it not to be carcinogenic. The dietary administration of Lithocholic acid to
chickens is reported to cause hepatic adenomatous hyperplasia.
Pregnancy
Pregnancy Category X: See CONTRAINDICATIONS
Nursing mothers
Pediatric use
The safety and effectiveness of chenodiol in children have not been established.
CHENODAL ADVERSE REACTIONS
Hepatobiliary
Dose-related serum aminotransferase (mainly SGPT) elevations, usually not accompanied by rises in
alkaline phosphatase or bilirubin, occurred in 30% or more of patients treated with the recommended dose of Chenodiol. In most cases, these elevations were
minor (1 ½ to 3 times the upper limit of laboratory normal) and transient, returning to within the normal range within six months despite continued
administration of the drug. In 2% to 3% of patients, SGPT levels rose to over three times the upper limit of laboratory normal, recurred on rechallenge with
the drug, and required discontinuation of chenodiol treatment. Enzyme levels have returned to normal following withdrawal of chenodiol (see WARNINGS).
Morphologic studies of liver biopsies taken before and after 9 and 24 months of treatment with chenodiol have shown that 63% of the patients prior to
chenodiol treatment had evidence of intrahepatic cholestasis. Almost all pretreatment patients had electron microscopic abnormalities. By the ninth month
of treatment, reexamination of two-thirds of the patients showed an 89% incidence of the signs of intrahepatic cholestasis. Two of 89 patients at the
ninth month had lithocholate-like lesions in the canalicular membrane, although there were not clinical enzyme abnormalities in the face of continued treatment
and no change in Type 2 light microscopic parameters.
Increased Cholecystectomy Rate
NCGS patients with a history of biliary pain prior to treatment had higher cholecystectomy rates
during the study if assigned to low dosage chenodiol (375 mg/day) than if
assigned to either placebo or high dosage chenodiol (750 mg/day). The
association with low dosage chenodiol though not clearly a causal one, suggests
that patients unable to take higher doses of chenodiol may be at greater risk of
cholecystectomy.
Gastrointestinal
Serum Lipids
Hematologic
DRUG ABUSE AND DEPENDENCE
Overdosage
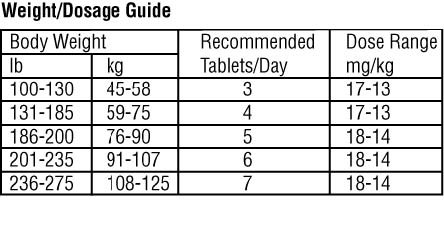
CHENODAL DOSAGE AND ADMINISTRATION
HOW SUPPLIED
ChenodalChenodiol TABLET, FILM COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||