Betaxolol Hydrochloride
Falcon Pharmaceuticals, Ltd.
Alcon Laboratories, Inc.
Sterile
FULL PRESCRIBING INFORMATION: CONTENTS*
- BETAXOLOL HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- BETAXOLOL HYDROCHLORIDE INDICATIONS AND USAGE
- BETAXOLOL HYDROCHLORIDE CONTRAINDICATIONS
- WARNING
- PRECAUTIONS
- Nursing Mothers
- Pediatric Use
- Geriatric Use
- BETAXOLOL HYDROCHLORIDE ADVERSE REACTIONS
- OVERDOSAGE
- BETAXOLOL HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- PRINCIPAL DISPLAY PANEL
FULL PRESCRIBING INFORMATION
DESCRIPTION
Betaxolol Hydrochloride Ophthalmic Solution contains betaxolol hydrochloride, a cardioselective beta-adrenergic receptor blocking agent, in a sterile isotonic solution. Betaxolol hydrochloride is a white, crystalline powder, soluble in water, with a molecular weight of 343.89. The chemical structure is presented below:
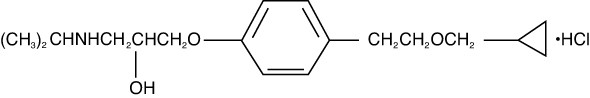
Empirical Formula:
C18H29NO3•HCl
Chemical Name:
(±)-1-[p-[2-(Cyclopropylmethoxy)ethyl]phenoxy]-3-(isopropylamino)-2-propanol hydrochloride.
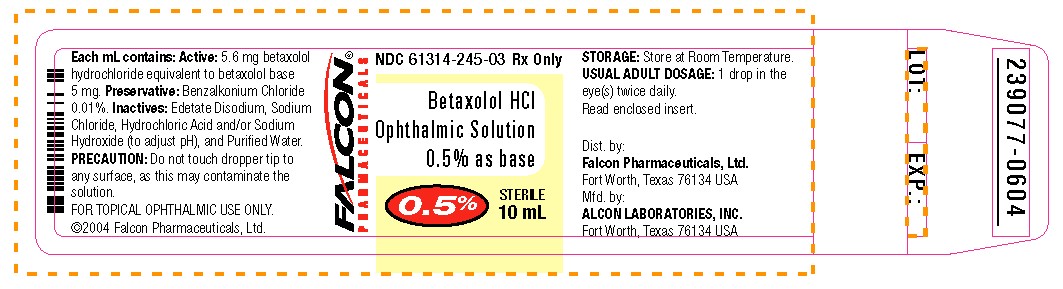
Each mL of Betaxolol Hydrochloride Ophthalmic Solution (0.5%) contains: Active: 5.6 mg betaxolol hydrochloride equivalent to betaxolol base 5 mg. Preservative: Benzalkonium Chloride 0.01%. Inactives: Edetate Disodium, Sodium Chloride, Hydrochloric Acid and/or Sodium Hydroxide (to adjust pH), and Purified Water.
CLINICAL PHARMACOLOGY
Betaxolol Hydrochloride, a cardioselective (beta-1-adrenergic) receptor blocking agent, does not have significant membrane-stabilizing (local anesthetic) activity and is devoid of intrinsic sympathomimetic action. Orally administered beta-adrenergic blocking agents reduce cardiac output in healthy subjects and patients with heart disease. In patients with severe impairment of myocardial function, beta-adrenergic receptor antagonists may inhibit the sympathetic stimulatory effect necessary to maintain adequate cardiac function.
When instilled in the eye, Betaxolol Hydrochloride Ophthalmic Solution has the action of reducing elevated as well as normal intraocular pressure, whether or not accompanied by glaucoma. Ophthalmic betaxolol has minimal effect on pulmonary and cardiovascular parameters.
Ophthalmic betaxolol (one drop in each eye) was compared to timolol and placebo in a three-way crossover study challenging nine patients with reactive airway disease who were selected on the basis of having at least a 15% reduction in the forced expiratory volume in one second (FEV1) after administration of ophthalmic timolol. Betaxolol HCl had no significant effect on pulmonary function as measured by FEV1, Forced Vital Capacity (FVC) and FEV1/VC. Additionally, the action of isoproterenol, a beta stimulant, administered at the end of the study was not inhibited by ophthalmic betaxolol. In contrast, ophthalmic timolol significantly decreased these pulmonary functions.
FEV1 - Percent Change from Baseline1
| Means | |||
|---|---|---|---|
| Betaxolol 1.0%a | Timolol 0.5% | Placebo | |
| Baseline | 1.6 | 1.4 | 1.4 |
| 60 Minutes | 2.3 | -25.7* | 5.8 |
| 120 Minutes | 1.6 | -27.4* | 7.5 |
| 240 Minutes | -6.4 | -26.9* | 6.9 |
| Isoproterenolb | 36.1 | -12.4* | 42.8 |
1Schoene, R. B. et al., Am. J. Ophthal. 97:86, 1984.
aTwice the clinical concentration.
bInhaled at 240 minutes; measurement at 270 minutes.
*Timolol statistically different from betaxolol and placebo (p < 0.05).
No evidence of cardiovascular beta-adrenergic blockade during exercise was observed with betaxolol in a double-masked, three-way crossover study in 24 normal subjects comparing ophthalmic betaxolol, timolol and placebo for effect on blood pressure and heart rate. Mean arterial blood pressure was not affected by any treatment; however, ophthalmic timolol produced a significant decrease in the mean heart rate.
Mean Heart Rates1
| TREATMENT | |||
|---|---|---|---|
| Bruce Stress Exercise Test | |||
| Minutes | Betaxolol 1%a | Timolol 0.5% | Placebo |
| 0 | 79.2 | 79.3 | 81.2 |
| 2 | 130.2 | 126.0 | 130.4 |
| 4 | 133.4 | 128.0* | 134.3 |
| 6 | 136.4 | 129.2* | 137.9 |
| 8 | 139.8 | 131.8* | 139.4 |
| 10 | 140.8 | 131.8* | 141.3 |
1Atkins, J. M. et al., Am. J. Oph. 99:173-175, Feb., 1985.
aTwice the clinical concentration.
*Mean pulse rate significantly lower for timolol than betaxolol or placebo (p < 0.05).
Clinical Studies: Optic nerve head damage and visual field loss are the result of a sustained elevated intraocular pressure and poor ocular perfusion. Betaxolol Hydrochloride Ophthalmic Solution has the action of reducing elevated as well as normal intraocular pressure, and the mechanism of ocular hypotensive action appears to be a reduction of aqueous production as demonstrated by tonography and aqueous fluorophotometry. The onset of action with Betaxolol Hydrochloride Ophthalmic Solution can generally be noted within 30 minutes and the maximal effect can usually be detected 2 hours after topical administration. A single dose provides a 12-hour reduction in intraocular pressure. Clinical observation of glaucoma patients treated with Betaxolol Hydrochloride Ophthalmic Solution for up to three years shows that the intraocular pressure lowering effect is well maintained.
Clinical studies show that topical Betaxolol Hydrochloride Ophthalmic Solution reduces mean intraocular pressure 25% from baseline. In trials using 22 mmHg as a generally accepted index of intraocular pressure control, Betaxolol Hydrochloride Ophthalmic Solution was effective in more than 94% of the population studied, of which 73% were treated with the beta blocker alone. In controlled, double-masked studies, the magnitude and duration of the ocular hypotensive effect of Betaxolol Hydrochloride Ophthalmic Solution and ophthalmic timolol solution were clinically equivalent.
Betaxolol Hydrochloride Ophthalmic Solution has also been used successfully in glaucoma patients who have undergone a laser trabeculoplasty and have needed additional long-term ocular hypotensive therapy.
Betaxolol Hydrochloride Ophthalmic Solution has been well tolerated in glaucoma patients wearing hard or soft contact lenses and in aphakic patients.
Betaxolol Hydrochloride Ophthalmic Solution does not produce miosis or accommodative spasm which are frequently seen with miotic agents. The blurred vision and night blindness often associated with standard miotic therapy are not associated with Betaxolol Hydrochloride Ophthalmic Solution. Thus, patients with central lenticular opacities avoid the visual impairment caused by a constricted pupil.
INDICATIONS AND USAGE
Betaxolol Hydrochloride Ophthalmic Solution has been shown to be effective in lowering intraocular pressure and is indicated in the treatment of ocular hypertension and chronic open-angle glaucoma. It may be used alone or in
combination with other anti-glaucoma drugs.
In clinical studies, Betaxolol Hydrochloride Ophthalmic Solution was safely used to lower intraocular pressure in 47 patients with both glaucoma and reactive airway disease who were followed for a mean period of 15 months. However, caution should be used in treating patients with severe reactive airway disease or a history of asthma.
CONTRAINDICATIONS
Hypersensitivity to any component of this product. Betaxolol Hydrochloride Ophthalmic Solution is contraindicated in patients with sinus bradycardia, greater than a first degree atrioventricular block, cardiogenic shock, or patients with overt cardiac failure.
WARNING
Topically applied beta-adrenergic blocking agents may be absorbed systemically. The same adverse reactions found with systemic administration of beta-adrenergic blocking agents may occur with topical administration. For example, severe respiratory reactions and cardiac reactions, including death due to bronchospasm in patients with asthma, and rarely death in association with cardiac failure, have been reported with topical application of beta-adrenergic blocking agents.
Betaxolol Hydrochloride Ophthalmic Solution has been shown to have a minor effect on heart rate and blood pressure in clinical studies. Caution should be used in treating patients with a history of cardiac failure or heart block. Treatment with Betaxolol Hydrochloride Ophthalmic Solution should be discontinued at the first signs of cardiac failure.
PRECAUTIONS
General
Information for Patients
Do not touch dropper tip to any surface as this may contaminate the solution.
Diabetes Mellitus
Beta-adrenergic blocking agents should be administered with caution in patients subject to spontaneous hypoglycemia or to diabetic patients (especially those with labile diabetes) who are receiving insulin or oral hypoglycemic agents.
Beta-adrenergic receptor blocking agents may mask the signs and symptoms of acute hypoglycemia.
Thyrotoxicosis
Beta-adrenergic blocking agents may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-adrenergic blocking agents, which might precipitate a thyroid storm.
Muscle Weakness
Beta-adrenergic blockade has been reported to potentiate muscle weakness consistent with certain myasthenic symptoms (e.g., diplopia, ptosis, and generalized weakness).
Major Surgery
Consideration should be given to the gradual withdrawal of beta-adrenergic blocking agents prior to general anesthesia because of the reduced ability of the heart to respond to beta-adrenergically mediated sympathetic reflex stimuli.
Pulmonary
Caution should be exercised in the treatment of glaucoma patients with excessive restriction of pulmonary function. There have been reports of asthmatic attacks and pulmonary distress during betaxolol treatment. Although rechallenges of some such patients with ophthalmic betaxolol has not adversely affected pulmonary function test results, the possibility of adverse pulmonary effects in patients sensitive to beta-blockers cannot be ruled out.
Risk from Anaphylactic Reaction
While taking beta-blockers, patients with a history of atopy or a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated accidental, diagnostic, or therapeutic challenge with such allergens. Such patients may be unresponsive to the usual doses of epinephrine used to treat anaphylactic reactions.
Drug Interactions
Patients who are receiving a beta-adrenergic blocking agent orally and Betaxolol Hydrochloride Ophthalmic Solution should be observed for a potential additive effect either on the intraocular pressure or on the known systemic effects of beta blockade.
Close observation of the patient is recommended when a beta blocker is administered to patients receiving catecholamine-depleting drugs such as reserpine, because of possible additive effects and the production of hypotension and/or bradycardia.
Betaxolol is an adrenergic blocking agent; therefore, caution should be exercised in patients using concomitant adrenergic psychotropic drugs.
Ocular
In patients with angle-closure glaucoma, the immediate treatment objective is to reopen the angle by constriction of the pupil with a miotic agent. Betaxolol has little or no effect on the pupil. When Betaxolol Hydrochloride Ophthalmic Solution is used to reduce elevated intraocular pressure in angle-closure glaucoma, it should be used with a miotic and not alone.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime studies with betaxolol HCl have been completed in mice at oral doses of 6, 20 or 60 mg/kg/day and in rats at 3, 12 or 48 mg/kg/day; betaxolol HCl demonstrated no carcinogenic effect. Higher dose levels were not tested.
In a variety of in vitro and in vivo bacterial and mammalian cell assays, betaxolol HCl was nonmutagenic.
Pregnancy
Pregnancy Category C. Reproduction, teratology, and peri- and postnatal studies have been conducted with orally administered betaxolol HCl in rats and rabbits. There was evidence of drug related postimplantation loss in rabbits and rats at dose levels above 12 mg/kg and 128 mg/kg, respectively. Betaxolol HCl was not shown to be teratogenic, however, and there were no other adverse effects on reproduction at subtoxic dose levels. There are no adequate and well-controlled studies in pregnant women. Betaxolol Hydrochloride Ophthalmic Solution should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
It is not known whether betaxolol HCl is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Betaxolol Hydrochloride Ophthalmic Solution is administered to nursing women.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
No overall differences in safety or effectiveness have been observed between elderly and younger patients.
ADVERSE REACTIONS
The following adverse reactions have been reported in clinical trials with Betaxolol Hydrochloride Ophthalmic Solution.
Ocular: Discomfort of short duration was experienced by one in four patients, but none discontinued therapy; occasional tearing has been reported. Rare instances of decreased corneal sensitivity, erythema, itching sensation, corneal punctate staining, keratitis, anisocoria, edema, and photophobia have been reported.
Additional medical events reported with other formulations of betaxolol include blurred vision, foreign body sensation, dryness of the eyes, inflammation, discharge, ocular pain, decreased visual acuity, and crusty lashes.
Systemic: Systemic reactions following administration of Betaxolol Hydrochloride Ophthalmic Solution 0.5% or Betaxolol Hydrochloride Ophthalmic Suspension 0.25% have been rarely reported. These include:
Cardiovascular: Bradycardia, heart block and congestive failure.
Pulmonary: Pulmonary distress characterized by dyspnea, bronchospasm, thickened bronchial secretions, asthma and respiratory failure.
Central Nervous System: Insomnia, dizziness, vertigo, headaches, depression, lethargy, and increase in signs and symptoms of myasthenia gravis.
Other: Hives, toxic epidermal necrolysis, hair loss and glossitis.
OVERDOSAGE
No information is available on overdosage of humans. The oral LD50 of the drug ranged from 350-920 mg/kg in mice and 860-1050 mg/kg in rats. The symptoms which might be expected with an overdose of a systemically administered beta-1-adrenergic receptor blocker agent are bradycardia, hypotension and acute cardiac failure. A topical overdose of Betaxolol Hydrochloride Ophthalmic Solution may be flushed from the eye(s) with warm tap water.
DOSAGE AND ADMINISTRATION
The recommended dose is one to two drops of Betaxolol Hydrochloride Ophthalmic Solution in the affected eye(s) twice daily. In some patients, the intraocular pressure lowering responses to Betaxolol Hydrochloride Ophthalmic Solution may require a few weeks to stabilize. As with any new medication, careful monitoring of patients is advised.
If the intraocular pressure of the patient is not adequately controlled on this regimen, concomitant therapy with pilocarpine and other miotics, and/or epinephrine and/or carbonic anhydrase inhibitors can be instituted.
HOW SUPPLIED
Betaxolol Hydrochloride Ophthalmic Solution is a sterile, isotonic, aqueous solution of betaxolol hydrochloride. Supplied as follows: 5, 10 and 15 mL in plastic ophthalmic DROP-TAINER* dispensers.
5 mL: NDC 61314-245-01 15 mL: NDC 61314-245-02
10 mL: NDC 61314-245-03
STORAGE: Store at room temperature.
Rx Only
*DROP-TAINER is a registered trademark of Alcon Manufacturing, Ltd.
9001563-0306
Dist. by:
FALCON Pharmaceuticals, Ltd.
Fort Worth, Texas 76134
Mfd. by:
ALCON LABORATORIES, INC.
Fort Worth, Texas 76134 USA
Printed in USA
PRINCIPAL DISPLAY PANEL
NDC 61314-4245-03 Rx Only
FALCON Pharmaceuticals®
Betaxolol HCl
Ophthalmic
Solution,
0.5% as base
0.5%
10 mL Sterile
AFFILATE OF QUALITY RX
ALCON
LABORATORIES, INC.

Betaxolol HydrochlorideBetaxolol Hydrochloride SOLUTION/ DROPS
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||