Aminophylline
General Injectables & Vaccines, Inc
Aminophylline 250 mg 25 mg/mL Injection, USP 10 mL Single Dose Vial
FULL PRESCRIBING INFORMATION: CONTENTS*
- Description
- Clinical Pharmacology
- Clinical Studies
- Aminophylline Indications and Usage
- Contraindications
- Warnings
- Precautions
- Side Effects
- Overdosage
- Dosage and Administration
- How Supplied
- Sample Package Label
FULL PRESCRIBING INFORMATION
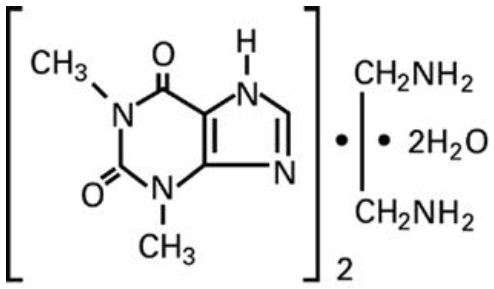
Description
25 mg/mL Aminophylline, Dihydrate
(Equivalent to 19.7 mg/mL of Anhydrous
Theophylline)
Ampul
Fliptop Vial
Rx only
Clinical Pharmacology
Mechanism of Action:
Theophylline has two distinct actions in the airways of patients with reversible obstruction; smooth muscle relaxation (i.e., bronchodilation) and suppression of the response of the airways to stimuli (i.e., nonbronchodilator prophylactic effects). While the mechanisms of action of theophylline are not known with certainty, studies in animals suggest that bronchodilation is mediated by the inhibition of two isozymes of phosphodiesterase (PDE III and, to a lesser extent, PDE IV), while nonbronchodilator prophylactic actions are probably mediated through one or more different molecular mechanisms, that do not involve inhibition of PDE III or antagonism of adenosine receptors. Some of the adverse effects associated with theophylline appear to be mediated by inhibition of PDE III (e.g., hypotension, tachycardia, headache, and emesis) and adenosine receptor antagonism (e.g., alterations in cerebral blood flow).
Theophylline increases the force of contraction of diaphragmatic muscles. This action appears to be due to enhancement of calcium uptake through an adenosine-mediated channel.
Serum Concentration-Effect Relationship:
Bronchodilation occurs over the serum theophylline concentration range of 5 - 20 mcg/mL. Clinically important improvement in symptom control and pulmonary function has been found in most studies to require serum theophylline concentrations greater than 10 mcg/ mL. At serum theophylline concentrations greater than 20 mcg/mL, both the frequency and severity of adverse reactions increase. In general, maintaining the average serum theophylline concentration between 10 and 15 mcg/mL will achieve most of the drug’s potential therapeutic benefit while minimizing the risk of serious adverse events.
Pharmacokinetics:
Overview The pharmacokinetics of theophylline vary widely among similar patients and cannot be predicted by age, sex, body weight or other demographic characteristics. In addition, certain concurrent illnesses and alterations in normal physiology (see Table I) and co-administration of other drugs (see Table II) can significantly alter the pharmacokinetic characteristics of theophylline. Within subject variability in metabolism has also been reported in some studies, especially in acutely ill patients. It is, therefore, recommended that serum theophylline concentrations be measured frequently in acutely ill patients receiving intravenous theophylline (e.g., at 24-hr. intervals). More frequent measurements should be made during the initiation of therapy and in the presence of any condition that may significantly alter theophylline clearance (see PRECAUTIONS, Effects on Laboratory Tests).
| Popular Characteristics Age |
Total Body Clearance * mean (range)†† (mL/kg/min) |
Half-Life mean (range)†† (hr) |
| Premature Neonates |
|
|
| postnatal age 3-15 days |
0.29 (0.09 - 0.49) |
30 (17 - 43) |
| postnatal age 25-57 days |
0.64 (0.04 -1.2) |
20 (9.4 - 30.6) |
| Term Infants |
|
|
| postnatal age 1 - 2 days |
NR † |
25.7 (25 - 26.5) |
| postnatal age 3 - 30 days |
NR † |
11 (6-19) |
| Children |
|
|
| 1 - 4 years | 1.7 (0.5 - 2.9) |
3.4 (1.2 - 5.6) |
| 4 - 12 years |
1.6 (0.8 - 2.4) |
NR † |
| 13 - 15 years |
0.9 (0.48 - 1.3) |
NR † |
| 16-17 years |
1.4 (0.2 - 2.6) | 3.7 |
| Adults (16 - 60) |
|
|
| otherwise healthy nonsmoking asthmatics |
0.65 (0.27 - 1.03) |
8.7 (6.1 - 12.8) |
| Elderly (more than 60 years) nonsmokers with normal cardiac, liver, and renal function |
0.41 (0.21 - 0.61) |
9.8 (1.6 - 18) |
| Concurrent Illness or Altered Physiological State |
|
|
| Acute pulmonary edema |
0.33 ** (0.07 - 2.45) | 19 ** (3.1 - 8.2) |
| COPD- more than 60 years, stable nonsmoker more than 1 year. |
0.54 (0.44 - 0.64) |
11 (9.4 -12.6) |
| COPD with cor pulmonale |
0.48 (0.08 - 0.88) |
NR † |
| Cystic Fibrosis (14 - 28 years) |
1.25 (0.31 - 2.2) |
6 (1.8 - 10.2) |
| Fever associated with acute viral respiratory illness (children 9 - 15 years) |
NR † | 7 (1.0 - 13) |
| Liver disease-cirrhosis |
0.31** (0.1 - 0.7) |
32** (10 - 56) |
| acute hepatitis |
0.35 (0.25 - 0.45) |
19.2 (16.6 - 21.8) |
| cholestasis |
0.65 (0.25 - 1.45) |
14.4 (5.7 - 31.8) |
| Pregnancey - 1st trimester |
NR † | 8.5 (3.1 - 13.9) |
| 2nd trimester |
NR † | 8.8 (3.8 - 13.8) |
| 3rd trimester |
NR † | 13 (8.4 - 17.6) |
| Sepsis with multi-organ failure |
0.47 (0.19-1.9) |
18.8 (6.3 - 24.1) |
| Thyroid disease - hypothyroid |
0.38 (0.13 - 0.57) |
11.6 (8.2 - 25) |
| hyperthyroid |
0.8 (0.68 - 0.97) |
4.56 (3.7 - 5.6) |
Note
Distribution
Metabolism
Excretion
Serum Concentrations at Steady State
Special Populations
Geriatric
Pediatrics
Gender
Race
Renal Insufficiency
Hepatic Insufficiency
Congestive Heart Failure
Smokers
Fever
Miscellaneous
Clinical Studies
Inhaled beta-2 selective agonists and systemically administered corticosteroids are the treatments of first choice for management of acute exacerbations of asthma. The results of controlled clinical trials on the efficacy of adding intravenous theophylline to inhaled beta-2 selective agonists and systemically administered corticosteroids in the management of acute exacerbations of asthma have been conflicting. Most studies in patients treated for acute asthma exacerbations in an emergency department have shown that addition of intravenous theophylline does not produce greater bronchodilation and increases the risk of adverse effects. In contrast, other studies have shown that addition of intravenous theophylline is beneficial in the treatment of acute asthma exacerbations in patients requiring hospitalization, particularly in patients who are not responding adequately to inhaled beta-2 selective agonists. In patients with chronic obstructive pulmonary disease (COPD), clinical studies have shown that theophylline decreases dyspnea, air trapping, the work of breathing, and improves contractility of diaphragmatic muscles with little or no improvement in pulmonary function measurements.
Aminophylline Indications and Usage
Intravenous theophylline is indicated as an adjunct to inhaled beta-2 selective agonists and systemically administered corticosteroids for the treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with asthma and other chronic lung diseases, e.g., emphysema and chronic bronchitis.
Contraindications
Aminophylline is contraindicated in patients with a history of hypersensitivity to theophylline or other components in the product including ethylenediamine.
Warnings
Concurrent Illness:
Theophylline should be used with extreme caution in patients with the following clinical conditions due to the increased risk of exacerbation of the concurrent condition:
Active peptic ulcer disease
Seizure disorders
Cardiac arrhythmias (not including bradyarrhythmias)
Conditions That Reduce Theophylline Clearance:
There are several readily identifiable causes of reduced theophylline clearance. If the infusion rate is not appropriately reduced in the presence of these risk factors, severe and potentially fatal theophylline toxicity can occur. Careful consideration must be given to the benefits and risks of theophylline use and the need for more intensive monitoring of serum theophylline concentrations in patients with the following risk factors:
Age
Neonates (term and premature)
Children less than 1 year
Elderly (greater than 60 years)
Concurrent Diseases
Acute pulmonary edema
Congestive heart failure
Cor pulmonale
Fever; greater than or equal to 102° for 24 hours or more; or lesser temperature elevations for longer periods
Hypothyroidism
Liver disease; cirrhosis, acute hepatitis
Reduced renal function in infants less than 3 months of age
Sepsis with multi-organ failure
Shock
Cessation of Smoking
Drug Interactions
Adding a drug that inhibits theophylline metabolism (e.g., cimetidine, erythromycin, tacrine) or stopping a concurrently administered drug that enhances theophylline metabolism (e.g., carbamazepine, rifampin). (See PRECAUTIONS, Drug Interactions, Table II.)
When Signs or Symptoms of Theophylline Toxicity Are Present:
Whenever a patient receiving theophylline develops nausea or vomiting, particularly repetitive vomiting, or other signs or symptoms consistent with theophylline toxicity (even if another cause may be suspected), the intravenous infusion should be stopped and a serum theophylline concentration measured immediately.
Dosage Increases
Increases in the dose of intravenous theophylline should not be made in response to an acute exacerbation of symptoms unless the steady-state serum theophylline concentration is less than 10 mcg/mL. As the rate of theophylline clearance may be dose-dependent (i.e., steady-state serum concentrations may increase disproportionately to the increase in dose), an increase in dose based upon a sub-therapeutic serum concentration measurement should be conservative. In general, limiting infusion rate increases to about 25% of the previous infusion rate will reduce the risk of unintended excessive increases in serum theophylline concentration (see DOSAGE AND ADMINISTRATION, TABLE VI).
Precautions
General
Careful consideration of the various interacting drugs and physiologic conditions that can alter theophylline clearance and require dosage adjustment should occur prior to initiation of theophylline therapy and prior to increases in theophylline dose (see WARNINGS).
Monitoring Serum Theophylline Concentrations:
Serum theophylline concentration measurements are readily available and should be used to determine whether the dosage is appropriate. Specifically, the serum theophylline concentration should be measured as follows:
1. Before making a dose increase to determine whether the serum concentration is sub-therapeutic in a patient who continues to be symptomatic.
2. Whenever signs or symptoms of theophylline toxicity are present.
3. Whenever there is a new illness, worsening of an existing concurrent illness or a change in the patient’s treatment regimen that may alter theophylline clearance (e.g., fever greater than 102°F sustained for greater than or equal to 24 hours, hepatitis, or drugs listed in Table II are added or discontinued).
In patients who have received no theophylline in the previous 24 hours, a serum concentration should be measured 30 minutes after completion of the intravenous loading dose to determine whether the serum concentration is less than 10 mcg/mL indicating the need for an additional loading dose or greater than 20 mcg/mL indicating the need to delay starting the constant I.V. infusion. Once the infusion is begun, a second measurement should be obtained after one expected half-life (e.g., approximately 4 hours in children 1 to 9 years and 8 hours in non-smoking adults; See Table I for the expected half-life in additional patient populations). The second measurement should be compared to the first to determine the direction in which the serum concentration has changed. The infusion rate can then be adjusted before steady state is reached in an attempt to prevent an excessive or sub-therapeutic theophylline concentration from being achieved. If a patient has received theophylline in the previous 24 hours, the serum concentration should be measured before administering an intravenous loading dose to make sure that it is safe to do so. If a loading dose is not indicated (i.e., the serum theophylline concentration is greater than or equal to 10 mcg/mL), a second measurement should be obtained as above at the appropriate time after starting the intravenous infusion. If, on the other hand, a loading dose is indicated (See DOSAGE AND ADMINISTRATION for guidance on selection of the appropriate loading dose), a second blood sample should be obtained after the loading dose and a third sample should be obtained one expected half-life after starting the constant infusion to determine the direction in which the serum concentration has changed. Once the above procedures related to initiation of intravenous theophylline infusion have been completed, subsequent serum samples for determination of theophylline concentration should be obtained at 24-hour intervals for the duration of the infusion. The theophylline infusion rate should be increased or decreased as appropriate based on the serum theophylline levels. When signs or symptoms of theophylline toxicity are present, the intravenous infusion should be stopped and a serum sample for theophylline concentration should be obtained as soon as possible, analyzed immediately, and the result reported to the clinician without delay. In patients in whom decreased serum protein binding is suspected (e.g., cirrhosis, women during the third trimester of pregnancy), the concentration of unbound theophylline should be measured and the dosage adjusted to achieve an unbound concentration of 6-12 mcg/mL. Saliva concentrations of theophylline cannot be used reliably to adjust dosage without special techniques.
Effects on Laboratory Tests:
As a result of its pharmacological effects, theophylline at serum concentrations within the 10 - 20 mcg/mL range modestly increases plasma glucose (from a mean of 88 mg% to 98 mg%), uric acid (from a mean of 4 mg/dl to 6 mg/dl), free fatty acids (from a mean of 451 mEq/L to 800 mEq/L), total cholesterol (from a mean of 140 vs 160 mg/dl), HDL (from a mean of 36 to 50 mg/dl), HDL/LDL ratio (from a mean of 0.5 to 0.7), and urinary free cortisol excretion (from a mean of 44 to 63 mcg/24 hr). Theophylline at serum concentrations within the 10 - 20 mcg/mL range may also transiently decrease serum concentrations of triiodothyronine (144 before, 131 after one week and 142 ng/dl after 4 weeks of theophylline). The clinical importance of these changes should be weighed against the potential therapeutic benefit of theophylline in individual patients.
Drug Interactions:
Theophylline interacts with a wide variety of drugs. The interaction may be pharmacodynamic, i.e., alterations in the therapeutic response to theophylline or another drug or occurrence of adverse effects without a change in serum theophylline concentration. More frequently, however, the interaction is pharmacokinetic, i.e., the rate of theophylline clearance is altered by another drug resulting in increased or decreased serum theophylline concentrations. Theophylline only rarely alters the pharmacokinetics of other drugs. The drugs listed in Table II have the potential to produce clinically significant pharmacodynamic or pharmacokinetic interactions with theophylline. The information in the “Effect” column of Table II assumes that the interacting drug is being added to a steadystate theophylline regimen. If theophylline is being initiated in a patient who is already taking a drug that inhibits theophylline clearance (e.g., cimetidine, erythromycin), the dose of theophylline required to achieve a therapeutic serum theophylline concentration will be smaller. Conversely, if theophylline is being initiated in a patient who is already taking a drug that enhances theophylline clearance (e.g., rifampin), the dose of theophylline required to achieve a therapeutic serum theophylline concentration will be larger. Discontinuation of a concomitant drug that increases theophylline clearance will result in accumulation of theophylline to potentially toxic levels, unless the theophylline dose is appropriately reduced. Discontinuation of a concomitant drug that inhibits theophylline clearance will result in decreased serum theophylline concentrations, unless the theophylline dose is appropriately increased. The drugs listed in Table III have either been documented not to interact with theophylline or do not produce a clinically significant interaction (i.e.,less than 15% change in theophylline clearance). The listing of drugs in Tables II and III are current as of September 1, 1995. New interactions are continuously being reported for theophylline, especially with new chemical entities. The clinician should not assume that a drug does not interact with theophylline if it is not listed in Table II. Before addition of a newly available drug in a patient receiving theophylline, the package insert of the new drug and/or the medical literature should be consulted to determine if an interaction between the new drug and theophylline has been reported.
| Drug |
Type of Interaction |
Effect ** |
| Adenosine |
Theophylline blocks adenosine receptors. |
Higher doses of adenosine may be required to achieve desired effect. |
| Alcohol |
A single large dose of alcohol (3 mL/kg of whiskey) decreases theophylline clearance for up to 24 hours. |
30% increase |
| Allopurinol |
Decreases theophylline clearance at allopurinol doses greater than or equal to 600 mg/day. |
25% increase |
| Aminoglutethimide |
Increases theophylline clearance by induction of microsomal enzyme activity |
25% decrease |
| Carbamazepine |
Similar to aminoglutethimide. |
30% decrease |
| Cimetidine |
Decreases theophylline clearance by inhibiting cytochrome P450 1A2. |
70% increase |
| Ciproflaxin |
Similar to cimetidine. |
40% increase |
| Clarithromycin |
Similar to erythromycin. |
25% increase |
| Diazepam |
Benzodiazepines increase CNS concentrations of adenosine, a potent CNS depressant, while theophylline blocks adenosine receptors. |
Larger diazepam doses may be required to produce desired level of sedation. Discontinuation of theophylline without reduction of diazepam dose may result in respiratory depression. |
| Disulfiram |
Decreases theophylline clearance by inhibiting hydroxylation and demethylation. |
50% increase |
| Enoxacin |
Similar to cimetidine. |
300% increase |
| Ephedrine |
Synergistic CNS effects. |
Increased frequency of nausea, nervousness, and insomnia. |
| Erythromycin |
Erythromycin metabolite decreases theophylline clearance by inhibiting cytochrome P450 3A3. |
35% increase. Erythromycin steady-state serum concentrations decrease by a similar amount. |
| Estrogen |
Estrogen containing oral contraceptives decrease theophylline clearance in a dose-dependent fashion. The effect of progesterone on theophylline clearance is unknown. |
30% increase |
| Flurazepam |
Similar to diazepam. |
Similar to diazepam. |
| Fluvoxamine |
Similar to cimetidine. |
Similar to cimetidine. |
| Halothane |
Halothane sensitizes the myocardium to catecholamines, theophylline increases release of endogenous catecholamines. |
Increased risk of ventricular arrhythmias. |
| Interferon, human recombinant alpha -A |
Decreases theophylline clearance. |
100% increase |
| Isoproterenol (I.V.) |
Increases theophylline clearance |
20% decrease |
| Ketamine |
Pharmacologic |
May lower theophylline seizure threshold. |
| Lithium |
Theophylline increases renal lithium clearance. |
Lithium dose required to achieve a therapeutic serum concentration increased an average of 60%. |
| Lorazepam |
Similar to diazepam. |
Similar to diazepam. |
| Methotrexate (MTX) |
Decreases theophylline clearance. |
20% increase after low dose MTX, higher dose MTX may have a greater effect. |
| Mexiletine |
Similar to disulfiram. |
80% increase |
| Midazolam |
Similar to diazepam. |
Similar to diazepam. |
| Moricizine |
Increases theophylline clearance. 25 |
25% decease |
| Pancuronium |
Theophylline may antagonize nondepolarizing neuromuscular blocking effects; possibly due to phosphodiesterase inhibition. |
Larger dose of pancuronium may be required to achieve neuromuscular blockade. |
| Pentoxifylline |
Decreases theophylline clearance |
30% increase |
| Phenobarbital (PB) |
Similar to aminoglutethimide. |
25% decrease after two weeks of concurrent Phenobarbital. |
| Phenytoin |
Phenytoin increases theophylline clearance by increasing microsomal enzyme activity. Theophylline decreases phenytoin absorption. |
Serum theophylline and phenytoin concentrations decrease about 40%. |
| Propafenone |
Decreases theophylline clearance and pharmacologic interaction. |
40% increase. Beta-2 blocking effect may decrease efficacy of theophylline. |
| Propranolol |
Similar to cimetidine and pharmacologic interaction. |
100% increase. Beta-2 blocking effect may decrease efficacy of theophylline. |
| Rifampin |
Increases theophylline clearance by increasing cytochrome P450 1A2 and 3A3 activity. |
20 - 40% decrease |
| Sulfinpyrazone |
Increases theophylline clearance by increasing demethylation and hydroxylation. Decreases renal clearance of theophylline. |
20% decrease |
| Tacrine |
Similar to cimetidine, also increases renal clearance of theophylline. |
90% increase |
| Thibendazole |
Decreases theophylline clearance. |
190% increase |
| Ticlopidine |
Decreases theophylline clearance. |
60% increase |
| Troleandomycin |
Similar to erythromycin. |
33 - 100% increase depending on troleandomycin dose. |
| Verapamil |
Similar to disulfiram. |
20% increase |
| alubeterol, systemic and inhaled |
lomefloxacin |
| amoxicillin |
mebendazole |
| ampicillin with or without sulbactam |
medroxyprogesterone |
| atenolol |
methylprednisolone |
| azithromycin |
metronidaozole |
| caffeine, dietary ingestion |
metroprolol |
| cefaclor |
nadolol |
| co-trimoxazole (trimethoprim and sulfamethoxazole) |
nifedipine |
| diltiazem |
nizatidine |
| dirithromycin |
norfloxacin |
| enflurane |
ofloxacin |
| famotidine |
omeprazole |
| felodipine |
prednisone, prednisolone |
| finasteride |
ranitidine |
| hydrocortisone |
rifabutin |
| isoflurane |
roxithromycin |
| isradipine |
sorbitolj (purgative doses do not inhibit theophylline absorption) |
| influenza vaccine |
sucralfate |
| ketoconazole |
terbutaline, systemic |
|
|
terfenadine |
|
|
tetracycline |
|
|
tocainide |
The Effect of Other Drugs on Theophylline Serum Concentration Measurements:
Carcinogenesis, Mutagenesis, and Impairment of Fertility:
Pregnancy
Nursing Mothers:
Pediatric Use:
Geriatric Use
Side Effects
Adverse reactions associated with theophylline are generally mild when peak serum theophylline concentrations are less than 20 mcg/mL and mainly consist of transient caffeine-like adverse effects such as nausea, vomiting, headache, and insomnia. When peak serum theophylline concentrations exceed 20 mcg/mL, however, theophylline produces a wide range of adverse reactions including persistent vomiting, cardiac arrhythmias, and intractable seizures which can be lethal (see OVERDOSAGE). Other adverse reactions that have been reported at serum theophylline concentrations less than 20 mcg/mL include diarrhea, irritability, restlessness, fine skeletal muscle tremors, and transient diuresis. In patients with hypoxia secondary to COPD, multifocal atrial tachycardia and flutter have been reported at serum theophylline concentrations greater than or equal to 15 mcg/mL. There have been a few isolated reports
of seizures at serum theophylline concentrations less than 20 mcg/mL in patients with an underlying neurological disease or in elderly patients. The occurrence of seizures in elderly patients with serum theophylline concentrations less than 20 mcg/mL may be secondary to decreased protein binding resulting in a larger proportion of the total serum theophylline concentration in the pharmacologically active unbound form. The clinical characteristics of the seizures reported in patients with serum theophylline concentrations less than 20 mcg/mL
have generally been milder than seizures associated with excessive serum theophylline concentrations resulting from an overdose (i.e., they have generally been transient, often stopped without anticonvulsant therapy, and did not result in neurological residua). Products containing aminophylline may rarely produce severe allergic reactions of the skin, including exfoliative dermatitis, after systemic administration in a patient who has been previously sensitized by topical application of a substance containing ethylenediamine. In such patients skin patch tests are positive for ethylenediamine, a component of aminophylline, and negative for theophylline. Pharmacists and other individuals who experience repeated skin exposure while physically handling aminophylline may develop a contact dermatitis due to the ethylenediamine component.
|
|
Acute Overdose (Large Single Ingestion) |
|
Chronic Overdosage (Multiple Excessive Doses) |
|
| Sign/Symptom |
Study 1 (n=157) |
Study 2 (n=14) |
Study 1 (n=92) |
Study 2 (n=102) |
| Asymptomatic | NR** |
0 |
NR** |
6 |
| Gastrointestinal |
|
|
|
|
| Vomiting |
73 |
93 |
30 |
61 |
| Abdominal Pain |
NR** |
21 |
NR** |
12 |
| Diarrhea |
NR** |
0 |
NR** |
14 |
| Hematemesis |
NR** |
0 |
NR** |
2 |
| Metabolic/Other |
|
|
|
|
| Hypokalemia |
85 |
79 |
44 |
43 |
| Hyperglycemia |
98 |
NR** |
18 |
NR** |
| Acid/base disturbance |
34 |
21 |
9 |
5 |
| Rhabdomyolysis |
NR** |
7 |
NR** |
0 |
| Cardiovascular |
|
|
|
|
| Sinus tachycardia |
100 |
86 |
100 |
62 |
| Other supraventricular tachycardias |
2 |
21 |
12 |
14 |
| Ventricular premature beats |
3 |
21 |
10 |
19 |
| Atrial fibrillation of flutter |
1 |
NR** |
12 |
NR** |
| Cardiovascular |
|
|
|
|
| Multifocal atrial tachycardia |
0 |
NR** |
2 |
NR** |
| Ventricular arrhythmias with hemodynamic instability |
7 |
14 |
40 |
0 |
| Hypotension/shock |
NR** |
21 |
NR** |
8 |
| Neurologic |
|
|
|
|
| Nervousness |
NR** |
64 |
NR** |
21 |
| Tremors |
38 |
29 |
16 |
14 |
| Disorientation |
NR** |
7 |
NR** |
11 |
| Seisures |
5 |
14 |
14 |
5 |
| Death | 3 |
21 |
10 |
4 |
Overdosage
General:
The chronicity and pattern of theophylline overdosage significantly influences clinical manifestations of toxicity, management and outcome. There are two common presentations: 1) acute overdose, i.e., infusion of an excessive loading dose or excessive maintenance infusion rate for less than 24 hours, and 2) chronic overdosage , i.e., excessive maintenance infusion rate for greater than 24 hours. The most common causes of chronic theophylline overdosage include clinician prescribing of an excessive dose or a normal dose in the presence of factors known to decrease the rate of theophylline clearance and increasing the dose in response to an exacerbation of symptoms without first measuring the serum theophylline concentration to determine whether a dose increase is safe. Several studies have described the clinical manifestations of theophylline overdose following oral administration and attempted to determine the factors that predict life-threatening toxicity. In general, patients who experience an acute overdose are less likely to experience seizures than patients who have experienced a chronic overdosage, unless the peak serum theophylline concentration is greater than 100 mcg/mL. After a chronic overdosage, generalized seizures, life-threatening cardiac arrhythmias, and death may occur at serum theophylline concentrations greater than 30 mcg/mL. The severity of toxicity after chronic overdosage is more strongly correlated with the patient’s age than the peak serum theophylline concentration; patients greater than 60 years are at the greatest risk for severe toxicity and mortality after a chronic overdosage. Pre-existing or concurrent disease may also significantly increase the susceptibility of a patient to a particular toxic manifestation, e.g., patients with neurologic disorders have an increased risk of seizures and patients with cardiac disease have an increased risk of cardiac arrhythmias for a given serum theophylline concentration compared to patients without the underlying disease. The frequency of various reported manifestations of oral theophylline overdose according to the mode of overdose are listed in Table IV. Other manifestations of theophylline toxicity include increases in serum calcium, creatine kinase, myoglobin and leukocyte count, decreases in serum phosphate and magnesium, acute myocardial infarction, and urinary retention in men with obstructive uropathy. Seizures associated with serum theophylline concentrations greater than 30 mcg/mL are often resistant to anticonvulsant therapy and may result in irreversible brain injury if not rapidly controlled. Death from theophylline toxicity is most often secondary to cardiorespiratory arrest and/or hypoxic encephalopathy following prolonged generalized seizures or intractable cardiac arrhythmias causing hemodynamic compromise.
Overdose Management:
General Recommendations for Patients with Symptoms of Theophylline Overdose or Serum Theophylline Concentrations greater than 30 mcg/mL While Receiving Intravenous Theophylline.
1. Stop the theophylline infusion.
2. While simultaneously instituting treatment, contact a regional poison center to obtain updated information and advice on individualizing the recommendations that follow.
3. Institute supportive care, including establishment of intravenous access, maintenance of the airway, and electrocardiographic monitoring.
4. Treatment of seizures Because of the high morbidity and mortality associated with theophylline-induced seizures, treatment should be rapid and aggressive. Anticonvulsant therapy should be initiated with an intravenous benzodiazepine, e.g., diazepam, in increments of 0.1 - 0.2 mg/kg every 1 - 3 minutes until seizures are terminated. Repetitive seizures should be treated with a loading dose of phenobarbital (20 mg/kg infused over 30 - 60 minutes). Case reports of theophylline overdose in humans and animal studies suggest that phenytoin is ineffective in terminating theophylline-induced seizures. The doses of benzodiazepines and phenobarbital required to terminate theophylline-induced seizures are close to the doses that may cause severe respiratory depression or respiratory arrest; the clinician should therefore be prepared to provide assisted ventilation. Elderly patients and patients with COPD may be more susceptible to the respiratory depressant effects of anticonvulsants. Barbiturate-induced coma or administration of general anesthesia may be required to terminate repetitive seizures or status epilepticus. General anesthesia should be used with caution in patients with theophylline overdose because fluorinated volatile anesthetics may sensitize the myocardium to endogenous catecholamines released by theophylline. Enflurane appears less likely to be associated with this effect than halothane and may, therefore, be safer. Neuromuscular blocking agents alone should not be used to terminate seizures since they abolish the musculoskeletal manifestations without terminating seizure activity in the brain.
5. Anticipate Need for Anticonvulsants In patients with theophylline overdose who are at high risk for theophylline-induced seizures, e.g., patients with acute overdoses and serum theophylline concentrations greater than 100 mcg/mL or chronic overdosage in patients greater than 60 years of age with serum theophylline concentrations greater than 30 mcg/mL, the need for anticonvulsant therapy should be anticipated. A benzodiazepine such as diazepam should be drawn into a syringe and kept at the patient’s bedside and medical personnel qualified to treat seizures should be immediately available. In selected patients at high risk for theophylline-induced seizures, consideration should be given to the administration of prophylactic anticonvulsant therapy. Situations where prophylactic anticonvulsant therapy should be considered in high risk patients include anticipated delays in instituting methods for extracorporeal removal of theophylline (e.g., transfer of a high risk patient from one health care facility to another for extracorporeal removal) and clinical circumstances that significantly interfere with efforts to enhance theophylline clearance (e.g., a neonate where dialysis may not be technically feasible or a patient with vomiting unresponsive to antiemetics who is unable to tolerate multiple-dose oral activated charcoal). In animal studies, prophylactic administration of phenobarbital, but not phenytoin, has been shown to delay the onset of theophylline-induced generalized seizures and to increase the dose of theophylline required to induce seizures (i.e., markedly increases the LD50). Although there are no controlled studies in humans, a loading dose of intravenous phenobarbital (20 mg/kg infused over 60 minutes) may delay or prevent life-threatening seizures in high risk patients while efforts to enhance theophylline clearance are continued. Phenobarbital may cause respiratory depression, particularly in elderly patients and patients with COPD.
6. Treatment of cardiac arrhythmias Sinus tachycardia and simple ventricular premature beats are not harbingers of life-threatening arrhythmias, they do not require treatment in the absence of hemodynamic compromise, and they resolve with declining serum theophylline concentrations. Other arrhythmias, especially those associated with hemodynamic compromise, should be treated with antiarrhythmic therapy appropriate for the type of arrhythmia.
7. Serum Theophylline Concentration Monitoring The serum theophylline concentration should be measured immediately upon presentation, 2 - 4 hours later, and then at sufficient
intervals, e.g., every 4 hours, to guide treatment decisions and to assess the effectiveness of therapy. Serum theophylline concentrations may continue to increase after presentation of the patient for medical care as a result of continued absorption of theophylline from the gastrointestinal tract. Serial monitoring of serum theophylline serum concentrations should be continued until it is clear that the concentration is no longer rising and has returned to nontoxic levels.
8. General Monitoring Procedures Electrocardiographic monitoring should be initiated on presentation and continued until the serum theophylline level has returned to a nontoxic level. Serum electrolytes and glucose should be measured on presentation and at appropriate intervals indicated by clinical circumstances. Fluid and electrolyte abnormalities should be promptly corrected. Monitoring and treatment should be continued until the serum concentration decreases below 20 mcg/mL.
9. Enhance clearance of theophylline Multiple-dose oral activated charcoal (e.g., 0.5 mg/kg up to 20 g, every two hours) increases the clearance of theophylline at least twofold by adsorption of theophylline secreted into gastrointestinal fluids. Charcoal must be retained in, and pass through, the gastrointestinal tract to be effective; emesis should therefore be controlled by administration of appropriate antiemetics. Alternatively, the charcoal can be administered continuously through a nasogastric tube in conjunction with appropriate antiemetics. A single dose of sorbitol may be administered with the activated charcoal to promote stooling to facilitate clearance of the adsorbed theophylline from the gastrointestinal tract. Sorbitol alone does not enhance clearance of theophylline and should be dosed with caution to prevent excessive stooling which can result in severe fluid and electrolyte imbalances. Commercially available fixed combinations of liquid charcoal and sorbitol should be avoided in young children and after the first dose in adolescents and adults since they do not allow for individualization of charcoal and sorbitol dosing. In patients with intractable vomiting, extracorporeal methods of theophylline removal should be instituted (see OVERDOSAGE, Extracorporeal Removal).
Specific Recommendations:
Acute Overdose (e.g., excessive loading dose or excessive infusion rate less than 24 hours
A. Serum Concentration greater than 20 less than 30 mcg/mL
1. Stop the theophylline infusion.
2. Monitor the patient and obtain a serum theophylline concentration in 2 - 4 hours to insure that the concentration is decreasing.
B. Serum Concentration greater than 30 less than 100 mcg/mL
1. Stop the theophylline infusion.
2. Administer multiple dose oral activated charcoal and measures to control emesis.
3. Monitor the patient and obtain serial theophylline concentrations every 2 - 4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
4. Institute extracorporeal removal if emesis, seizures, or cardiac arrhythmias cannot be adequately controlled (see OVERDOSAGE, Extracorporeal Removal).
C. Serum Concentration greater than 100 mcg/mL
1. Stop the theophylline infusion.
2. Consider prophylactic anticonvulsant therapy.
3. Administer multiple-dose oral activated charcoal and measures to control emesis.
4. Consider extracorporeal removal, even if the patient has not experienced a seizure (see OVERDOSAGE, Extracorporeal Removal).
5. Monitor the patient and obtain serial theophylline concentrations every 2 - 4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
Chronic Overdosage (e.g., excessive infusion rate for greater than 24 hours)
A. Serum Concentration greater than 20 less than 30 mcg/mL (with manifestations of theophylline toxicity)
1. Stop the theophylline infusion.
2. Monitor the patient and obtain a serum theophylline concentration in 2 - 4 hours to insure that the concentration is decreasing.
B. Serum Concentration greater than 30 mcg/mL in patients less than 60 years of age
1. Stop the theophylline infusion.
2. Administer multiple-dose oral activated charcoal and measures to control emesis.
3. Monitor the patient and obtain serial theophylline concentrations every 2 - 4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
4. Institute extracorporeal removal if emesis, seizures, or cardiac arrhythmias cannot be adequately controlled (see OVERDOSAGE, Extracorporeal Removal).
C. Serum Concentration greater than 30 mcg/mL in patients greater than or equal to 60 years of age
1. Stop the theophylline infusion.
2. Consider prophylactic anticonvulsant therapy.
3. Administer multiple-dose oral activated charcoal and measures to control emesis.
4. Consider extracorporeal removal even if the patient has not experienced a seizure (see OVERDOSAGE, Extracorporeal Removal).
5. Monitor the patient and obtain serial theophylline concentrations every 2 - 4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
Extracorporeal Removal:
Increasing the rate of theophylline clearance by extracorporeal methods may rapidly decrease serum concentrations, but the risks ofthe procedure must be weighed against the potential benefit. Charcoal hemoperfusion is the most effective method of extracorporeal removal, increasing theophylline clearance up to six fold, but serious complications, including hypotension, hypocalcemia, platelet consumption and bleeding diatheses may occur. Hemodialysis is about as efficient as multiple-dose oral activated charcoal and has a lower risk of serious complications than charcoal hemoperfusion. Hemodialysis should be considered as an alternative when charcoal hemoperfusion is not feasible and multiple-dose oral charcoal is ineffective because of intractable emesis. Serum theophylline concentrations may rebound 5 - 10 mcg/mL after discontinuation of charcoal hemoperfusion or hemodialysis due to redistribution
of theophylline from the tissue compartment. Peritoneal dialysis is ineffective for theophylline removal; exchange transfusions in neonates have been minimally effective.
Dosage and Administration
General Considerations:
The steady-state serum theophylline concentration is a function of the infusion rate and the rate of theophylline clearance in the individual patient. Because of marked individual differences in the rate of theophylline clearance, the dose required to achieve a serum theophylline concentration in the 10-20 mcg/mL range varies fourfold among otherwise similar patients in the absence of factors known to alter theophylline clearance. For a given population there is no single theophylline dose that will provide both safe and effective serum concentrations for all patients. Administration of the median theophylline dose required to achieve a therapeutic serum theophylline concentration in a given population may result in either sub-therapeutic or potentially toxic serum theophylline concentrations in individual patients. The dose of theophylline must be individualized on the basis of serum theophylline concentration measurements in order to achieve a dose that will provide maximum potential benefit with minimal risk of adverse effects. When theophylline is used as an acute bronchodilator, the goal of obtaining a therapeutic serum concentration is best accomplished with an intravenous loading dose. Because of rapid distribution into body fluids, the serum concentration (C) obtained from an initial
loading dose (LD) is related primarily to the volume of distribution (V), the apparent space into which the drug diffuses:
C = LD/V
If a mean volume of distribution of about 0.5 L/kg is assumed (actual range is 0.3 to 0.7 L/kg), each mg/kg (ideal body weight) of theophylline administered as a loading dose over 30 minutes results in an average 2 mcg/mL increase in serum theophylline concentration. Therefore, in a patient who has received no theophylline in the previous 24 hours, a loading dose of intravenous theophylline of 4.6 mg/kg (5.7 mg/kg as aminophylline), calculated on the basis of ideal body weight and administered over 30 minutes, on average, will produce a maximum post-distribution serum concentration of 10 mcg/mL with a range of 6-16 mcg/mL. When a loading dose becomes necessary in the patient who has already received theophylline, estimation of the serum concentration based upon the history is unreliable, and an immediate serum level determination is indicated. The loading dose can then be determined as follows:
D = (Desired C - Measured C) (V)
where D is the loading dose, C is the serum theophylline concentration, and V is the volume of distribution. The mean volume of distribution can be assumed to be 0.5 L/kg and the desired serum concentration should be conservative (e.g., 10 mcg/mL) to allow for the variability in the volume of distribution. A loading dose should not be given before obtaining a serum theophylline concentration if the patient has received any theophylline in the previous 24 hours. A serum concentration obtained 30 minutes after an intravenous loading dose, when distribution is complete, can be used to assess the need for and size of subsequent loading doses, if clinically indicated, and for guidance of continuing therapy. Once a serum
concentration of 10 to 15 mcg/mL has been achieved with the use of a loading dose(s), a constant intravenous infusion is started. The rate of administration is based upon mean pharmacokinetic parameters for the population and calculated to achieve a target serum concentration of 10 mcg/mL (see Table V). For example, in non-smoking adults, initiation of a constant intravenous theophylline infusion of 0.4 mg/kg/hr (0.5 mg/kg/hr as aminophylline) at the completion of the loading dose, on average, will result in a steadystate concentration of 10 mcg/mL with a range of 7-26 mcg/mL. The mean and range of steady-state serum concentrations are similar when the average child (age 1 to 9 years) is given a loading dose of 4.6 mg/kg theophylline (5.7 mg/kg as aminophylline) followed by a constant intravenous infusion of 0.8 mg/kg/hr (1.0 mg/kg/hr as aminophylline). Since there is large interpatient variability in
theophylline clearance, serum concentrations will rise or fall when the patient’s clearance is significantly different from the mean population value used to calculate the initial infusion rate. Therefore, a second serum concentration should be obtained one expected half-life after starting the constant infusion (e.g., approximately 4 hours for children age 1 to 9 and 8 hours for nonsmoking adults; See Table I for the expected half-life in additional patient populations) to determine if the concentration is accumulating or declining from the post loading dose level. If the level is declining as a result of a higher than average clearance, an additional loading dose can be administered and/or the infusion rate increased. In contrast, if the second sample demonstrates a higher level, accumulation of the drug can be assumed, and the infusion rate should be decreased before the concentration exceeds 20 mcg/mL. An additional sample
is obtained 12 to 24 hours later to determine if further adjustments are required and then at 24-hour intervals to adjust for changes, if they occur. This empiric method, based upon mean pharmacokinetic parameters, will prevent large fluctuations in serum concentration during the most critical period of the patient’s course. In patients with cor pulmonale, cardiac decompensation, or liver dysfunction, or in those taking drugs that markedly reduce theophylline clearance (e.g., cimetidine), the initial theophylline infusion rate should not exceed 17 mg/hr (21 mg/hr as aminophylline) unless serum concentrations can be monitored at 24-hour intervals. In these patients, 5 days may be required before steady-state is reached.
Theophylline distributes poorly into body fat, therefore, mg/kg dose should be calculated on the basis of ideal body weight. Table V contains initial theophylline infusion rates following an appropriate loading dose recommended for patients in various age groups and clinical circumstances. Table VI contains recommendations for final theophylline dosage adjustment based upon serum theophylline concentrations. Application of these general dosing recommendations to individual patients must take into account the unique clinical characteristics of each patient. In general, these recommendations should serve as the upper limit for dosage adjustments in order to decrease the risk of potentially serious adverse events associated with unexpected large increases in serum theophylline concentration.
| Patient population | Age | Theophylline infusion rate (mg/kg/hr)*† |
| Neonates |
Postnatal age up to 24 days Postnatal age beyond 24 days |
1 mg/kg q 12h/‡ 1.5 mg/kg q12 h/‡ |
| Infants |
6-52 weeks old |
mg/kg/hr=(0.008) (age in weeks) + 0.21 |
| Young children |
1-9 years |
0.8 |
| Older children |
9-12 years |
0.7 |
| Adolescents (cigarette or marijuana smokers) |
12-16 years |
0.7 |
| Adolescents (nonsmokers) |
12-16 years |
0.5 § |
| Adults (otherwise healthy nonsmokers) |
16-60 years |
0.4§ |
| Elderly |
greater than 60 years |
0.3# |
| Cardiac decompensation, cor pulmonale, liver dysfunction, sepsis with multiorgan failure, or shock |
|
0.2# |
|
Peak Serum Concentration |
Dosage Adjustment |
| less than 9.9 mdg/mL |
If symptoms are not controlled and current dosage is tolerated, increase infusion rate about 25%. Recheck serum concentration after 12 hours in children and 24 hours in adults for further dosage adjustment. |
| 10 to 14.9 mcg/mL |
If symptoms are controlled and current dosage is tolerated, maintain infusion rate and recheck serum concentration at 24 hour intervals.¶ If symptoms are not controlled and current dosage is tolerated consider adding additional medication(s) to treatment regimen. |
| 15 - 19.9 mcg/mL |
Consider 10% decrease in infusion rate to provide greater margin of safety even if current dosage is tolerated.¶ |
| 20 - 24.9 mcg/mL |
Decrease infusion rate by 25% even if no adverse effects are present. Recheck serum concentration after 12 hours in children and 24 hours in adults to guide further dosage adjustment. |
| 25 - 3- mcg/mL |
Stop infusion for 12 hours in children and 24 hours in adults and decrease subsequent infusion rate at least 25% even if no adverse effects are present. Recheck serum concentration after 12 hours in children and 24 hours in adults to guide further dosage adjustment. If symptomatic, stop infusion and consider whether overdose treatment is indicated (see recommendations for chronic overdosage). |
| greater than 30 mcg/mL |
Stop the infusion and treat overdose as indicated (see recommendations for chronic overdosage). If theophylline is subsequently resumed, decrease infusion rate by at least 50% and recheck serum concentration after 12 hours in children and 24 hours in adults to guide further dosage adjustment. |
Intravenous Admixture Incompatibility:
How Supplied
Aminophylline Injection, USP 25 mg/mL is supplied in single-dose containers as follows:
| List No. | Container | Volume | Total Content |
| 0409-7385-01 |
Ampul |
10 mL |
250 mg |
| 0409-7386-01 |
Ampul |
20 mL |
500 mg |
| 0409-5921-01 |
Partial-fill Fliptop Vial |
10 mL |
250 mg |
| 0409-5922-01 |
Partial-fill Fliptop Vial | 20 mL |
500 mg |
Sample Package Label
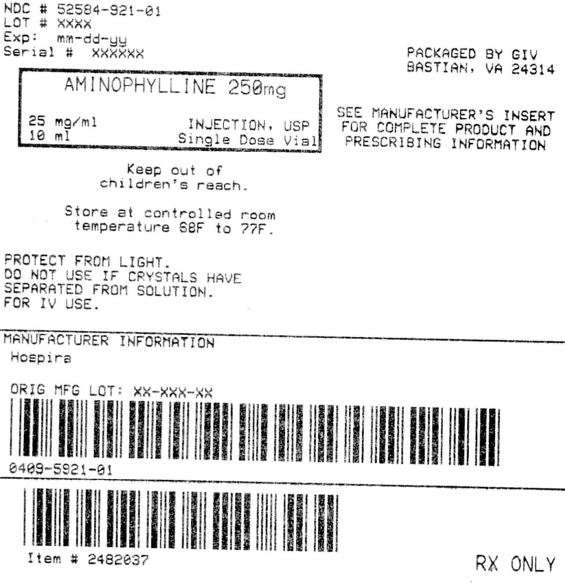
AminophyllineAminophylline INJECTION, SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||